Muscle Function: Effects of Aging: Difference between revisions
(linked pages) |
(linked pages, reference edit and minor grammar edit) |
||
| Line 10: | Line 10: | ||
As we age our muscles undergo progressive changes, primarily involving loss of [[muscle]] mass and [[Muscle Strength|strength]]. | As we age our muscles undergo progressive changes, primarily involving loss of [[muscle]] mass and [[Muscle Strength|strength]]. | ||
The age-related loss of muscle function is known as '''Sarcopenia'''<ref>Rosenberg IH | The age-related loss of muscle function is known as '''Sarcopenia'''<ref>Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr. 1997;127(suppl 5):990S-991S.</ref>, derived from the Greek words for flesh (sarcos) and loss (penia) and its definition includes loss of muscle strength and power, as well as reduced function<ref>Rolland Y, Czerwinski S, Abellan Van Kan G, Morley JE, Cesari M, Onder G et al: Sarcopenia: its assessment, etiology, pathogenesis, consequences and future perspectives. J Nutr Health Aging. 2008;12(7):433-450. | ||
</ref>. It occurs with increasing age, and is a major component in the development of frailty. | |||
The loss of muscle mass during the aging process is important clinically as it reduces strength and exercise capacity, both which are needed to perform activities of daily living. | The loss of muscle mass during the aging process is important clinically as it reduces strength and exercise capacity, both which are needed to perform activities of daily living. | ||
The video below gives a good summary of the changes and effects on performance and health. | The video below gives a good summary of the changes and effects on performance and health. | ||
{{#ev:youtube|https://www.youtube.com/watch?v=ymcFS1tQrsk|width}}<ref>Mayo clinic. Muscle loss and aging. Available from: https://www.youtube.com/watch?v=ymcFS1tQrsk | {{#ev:youtube|https://www.youtube.com/watch?v=ymcFS1tQrsk|width}}<ref>Mayo clinic. Muscle loss and aging. Available from: https://www.youtube.com/watch?v=ymcFS1tQrsk [last accessed 11.5.2019]</ref> | ||
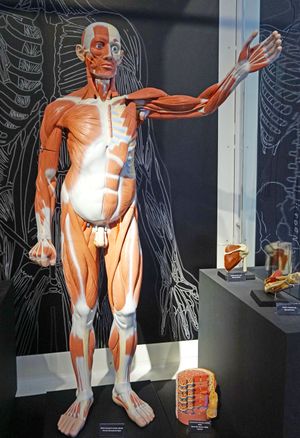
== Age-related changes in muscle structure == | == Age-related changes in muscle structure == | ||
<div>With increasing age, we lose muscle mass: lean muscle mass contributes up to 50% of total body weight in young adults, but this decreases to 25% by 75 to 80 years<ref>Short KR, Nair KS | <div>With increasing age, we lose muscle mass: lean muscle mass contributes up to 50% of total body weight in young adults, but this decreases to 25% by 75 to 80 years<ref>Short KR, Nair KS. The effect of age on protein metabolism. Curr Opin Clin Nutr Metab Care.2000; 3(1):39-44</ref>. </div><div></div><div>Typical muscle changes with age:</div> | ||
==== Gross Muscle changes: ==== | ==== Gross Muscle changes: ==== | ||
===== Reduced muscle mass (replaced by increased fat mass) ===== | ===== Reduced muscle mass (replaced by increased fat mass) ===== | ||
Reduction in lower limb muscle cross-sectional area have been observed to begin in early adulthood and accelerate beyond 50 years of age.This reduction in muscle cross-sectional area associated with decreases in contractile structures accompanied by increases in non contractile structures such as fat and connective tissue.<ref>Henwood TR, Riek S, Taaffe DR | Reduction in lower limb muscle cross-sectional area have been observed to begin in early adulthood and accelerate beyond 50 years of age.This reduction in muscle cross-sectional area associated with decreases in contractile structures accompanied by increases in non contractile structures such as fat and connective tissue.<ref name=":0">Henwood TR, Riek S, Taaffe DR. Strength versus muscle power-specific resistance training in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2008; 63(1):83-91.</ref> | ||
===== Reduced muscle strength ===== | ===== Reduced muscle strength ===== | ||
The total number of muscle fibers is significantly reduced with age, beginning at about 25 years and progressing at an accelerated rate thereafter The decline in muscle cross-sectional area is most likely due to decreases in total fiber number, especially type II fast-twitch glycolytic fibers. This results in reduced muscle power.<ref | The total number of muscle fibers is significantly reduced with age, beginning at about 25 years and progressing at an accelerated rate thereafter The decline in muscle cross-sectional area is most likely due to decreases in total fiber number, especially type II fast-twitch glycolytic fibers. This results in reduced muscle power.<ref name=":0" /> | ||
==== Muscle Fibre changes: ==== | ==== Muscle Fibre changes: ==== | ||
| Line 31: | Line 32: | ||
===== Changes in Muscle Fiber Size ===== | ===== Changes in Muscle Fiber Size ===== | ||
Elderly individuals often [[Falls in elderly|fall]] because of poor [[Muscle Strength|muscle strength]] and reduced [[Balance|balancing ability]] related to muscle aging. Types IIA and IIB muscle fibers decrease with age in the area percentage, fiber number percentage, and mean fiber area, whereas Type I fibers increase in area and number but not in size. Morphologically, Type II fibers appeared smaller and flatter. Investigations suggest deterioration in muscle quality and balancing coordination in elderly patients. | Elderly individuals often [[Falls in elderly|fall]] because of poor [[Muscle Strength|muscle strength]] and reduced [[Balance|balancing ability]] related to muscle aging. Types IIA and IIB muscle fibers decrease with age in the area percentage, fiber number percentage, and mean fiber area, whereas Type I fibers increase in area and number but not in size. Morphologically, Type II fibers appeared smaller and flatter. Investigations suggest deterioration in muscle quality and balancing coordination in elderly patients. A research done provided data to help determine treatments for reversing muscle fiber changes and reducing the number of falls and related fractures in patients.<ref>Lee WS, Cheung WH, Qin L, Tang N, Leung KS. Age-associated decrease of type IIA/B human skeletal muscle fibers. Clin Orthop Relat Res. 2006;450:231-7. | ||
</ref>The reduction in number of muscle fibers contributes more to the decrease of whole muscle cross-sectional area than does the reduction in area of individual fibers. The individual fast-twitch type II fibers decrease in cross-sectional area suggest that the relative contribution of fast-twitch type II fibers to force generation is less in the older adult.<br> | |||
===== Motor Unit Number and Size ===== | ===== Motor Unit Number and Size ===== | ||
The majority of the literature indicates that muscle fiber loss is due to a loss in motor neurons. There is consistent denervation and reinervation of the muscle fiber throughout one’s lifespan, but in the aged, denervation appears to outpace reinveration. Data indicate that a 60 year-old has approximately 25-50% fewer motor neurons than a 20 year-old, with the greatest losses in distal fast twitch motor neurons With the loss of the motor neuron, the deinervated fast twitch muscle fibers that were attached to it are either permanently deinervated and undergo apoptosis, or are reinverated with a different motor neuron most likely that of a slow twitch neuron, potentially making the fiber take on slow twitch characteristics<ref> | The majority of the literature indicates that muscle fiber loss is due to a loss in motor neurons. There is consistent denervation and reinervation of the muscle fiber throughout one’s lifespan, but in the aged, denervation appears to outpace reinveration. Data indicate that a 60 year-old has approximately 25-50% fewer motor neurons than a 20 year-old, with the greatest losses in distal fast twitch motor neurons With the loss of the motor neuron, the deinervated fast twitch muscle fibers that were attached to it are either permanently deinervated and undergo apoptosis, or are reinverated with a different motor neuron most likely that of a slow twitch neuron, potentially making the fiber take on slow twitch characteristics<ref>Bunn JA. Aging and the Motor Unit. J Sport Medic Doping Studie. 2012; S1:e001. doi:10.4172/2161-0673.S1-e001</ref> | ||
== Effects of endocrine changes on muscle == | == Effects of endocrine changes on muscle == | ||
| Line 41: | Line 43: | ||
With increased age, the following changes in endocrine function result in sarcopenia: | With increased age, the following changes in endocrine function result in sarcopenia: | ||
*Increased insulin resistance<ref>Refaie MR, Sayed-Ahmed NA, Bakr AM, Aziz MY, El Kannishi MH, Abdel-Gawad SS. Aging is an inevitable risk factor for insulin resistance. Journal of Taibah University Medical Sciences. 2006 | *Increased insulin resistance<ref>Refaie MR, Sayed-Ahmed NA, Bakr AM, Aziz MY, El Kannishi MH, Abdel-Gawad SS. Aging is an inevitable risk factor for insulin resistance. Journal of Taibah University Medical Sciences. 2006;1(1):30-41.</ref> | ||
*Decreased growth hormone<ref>Toogood AA | *Decreased growth hormone<ref>Toogood AA. Growth hormone (GH) status and body composition in normal ageing and in elderly adults with GH deficiency. Horm Res. 2003; 60(Suppl 1):105-111.</ref> | ||
*Reduction in oestrogen and testosterone<ref>Gower BA, Nyman L | *Reduction in oestrogen and testosterone<ref>Gower BA, Nyman L. Associations among oral estrogen use, free testosterone concentration, and lean body mass among postmenopausal women. J Clin Endocrinol Metab. 2000; 85(12):4476-4480.</ref> | ||
*Vitamin D deficiency<ref>Wicherts IS, van Schoor NM, Boeke AJ, et al | *Vitamin D deficiency<ref>Wicherts IS, van Schoor NM, Boeke AJ, Visser M, Deeg DJ, Smit J, et al. Vitamin D status predicts physical performance and its decline in older persons. J Clin Endocrinol Metab. 2007; 92(6):2058-2065.</ref> | ||
*Increased parathyroid hormone<ref>Visser M, Deeg DJ, Lips P | *Increased parathyroid hormone<ref>Visser M, Deeg DJ, Lips P. Low vitamin D and high parathyroid hormone levels as determinants of loss of muscle strength and muscle mass (sarcopenia): the Longitudinal Aging Study Amsterdam. J Clin Endocrinol Metab. 2003;88(12):5766-5772.</ref> | ||
== Conditions associated with impairment of skeletal function == | == Conditions associated with impairment of skeletal function == | ||
| Line 78: | Line 80: | ||
Resistance or weight training has been demonstrated to produce increases in muscle strength and power, and also mobility function, in older people living in the following settings: | Resistance or weight training has been demonstrated to produce increases in muscle strength and power, and also mobility function, in older people living in the following settings: | ||
#independently in the community<ref>Beneka A, Malliou P, Fatouros I, et al: Resistance training effects on muscular strength of elderly are related to intensity and gender. J Sci Med Sport 8:274-283 | #independently in the community<ref>Beneka A, Malliou P, Fatouros I, Jamurtas A, Gioftsidou A, Godolias G, et al: Resistance training effects on muscular strength of elderly are related to intensity and gender. J Sci Med Sport. 2005;8(3):274-283.</ref><ref name=":0" /><ref name=":1">Taaffe DR, Duret C, Wheeler S, Marcus R. Once-weekly resistance exercise improves muscle strength and neuromuscular performance in older adults. J Am Geriatr Soc. 1999; 47(10):1208-1214, 1999</ref> | ||
#in nursing homes<ref>Beyer N, Simonsen L, Bulow J, | #in nursing homes<ref>Beyer N, Simonsen L, Bulow J, Lorenzen T, Jensen DV, Larsen L, et al. Old women with a recent fall history show improved muscle strength and function sustained for six months after finishing training. Aging Clin Exp Res. 2007;19(4):300-309.</ref><ref>Harridge SD, Kryger A, Stensgaard A. Knee extensor strength, activation, and size in very elderly people following strength training. Muscle Nerve. 1999; 22(7):831-839.</ref> | ||
#hospitalised elderly people<ref>Hauer K, Specht N, Schuler M, | #hospitalised elderly people<ref>Hauer K, Specht N, Schuler M, Bärtsch P, Oster P. Intensive physical training in geriatric patients after severe falls and hip surgery. Age Ageing. 2002; 31(1):49-57</ref><ref>Suetta C, Magnusson SP, Rosted A, Aagaard P, Jakobsen AK, Larsen LH, et al. Resistance training in the early postoperative phase reduces hospitalization and leads to muscle hypertrophy in elderly hip surgery patients—a controlled, randomized study. J Am Geriatr Soc. 2004;52(12):2016-2022</ref> | ||
==== Gender differences ==== | ==== Gender differences ==== | ||
Increased muscle quality from resistance training is a common finding in older adults, and in men there appears to be no difference in young versus old<ref>Ivey FM, Tracy BL, Lemmer JT, et al | Increased muscle quality from resistance training is a common finding in older adults, and in men there appears to be no difference in young versus old<ref>Ivey FM, Tracy BL, Lemmer JT, NessAiver M, Metter EJ, Fozard JL, et al Effects of strength training and detraining on muscle quality: age and gender comparisons. J Gerontol A Biol Sci Med Sci. 2000; 55(3):B152-B157; discussion B8-B9</ref>, but there is a study which suggests that older women have a blunted response relative to younger women<ref>Hakkinen K, Alen M, Kallinen M, Newton RU, Kraemer WJ. Neuromuscular adaptation during prolonged strength training, detraining and re-strength-training in middle-aged and elderly people. Eur J Appl Physiol. 2000;83(1):51-62</ref>. | ||
==== Frequency of resistance training ==== | ==== Frequency of resistance training ==== | ||
Studies have demonstrated that resistance training regimes performed once, twice or even three times a week all result in strength improvements<ref | Studies have demonstrated that resistance training regimes performed once, twice or even three times a week all result in strength improvements<ref name=":1" />. | ||
==== Length of training programme ==== | ==== Length of training programme ==== | ||
Revision as of 11:13, 15 May 2019
Original Editor - Wendy Walker
Top Contributors - Wendy Walker, Lucinda hampton, Andeela Hafeez, Vidya Acharya, Kim Jackson, Tony Lowe, Uchechukwu Chukwuemeka, Tarina van der Stockt, WikiSysop, Simisola Ajeyalemi, Claire Knott, Rucha Gadgil, Amrita Patro, Lauren Lopez, Admin, Aminat Abolade, Evan Thomas and Lizzie Cotton
Introduction[edit | edit source]
As we age our muscles undergo progressive changes, primarily involving loss of muscle mass and strength.
The age-related loss of muscle function is known as Sarcopenia[1], derived from the Greek words for flesh (sarcos) and loss (penia) and its definition includes loss of muscle strength and power, as well as reduced function[2]. It occurs with increasing age, and is a major component in the development of frailty.
The loss of muscle mass during the aging process is important clinically as it reduces strength and exercise capacity, both which are needed to perform activities of daily living. The video below gives a good summary of the changes and effects on performance and health.
[edit | edit source]
Gross Muscle changes:[edit | edit source]
Reduced muscle mass (replaced by increased fat mass)[edit | edit source]
Reduction in lower limb muscle cross-sectional area have been observed to begin in early adulthood and accelerate beyond 50 years of age.This reduction in muscle cross-sectional area associated with decreases in contractile structures accompanied by increases in non contractile structures such as fat and connective tissue.[5]
Reduced muscle strength[edit | edit source]
The total number of muscle fibers is significantly reduced with age, beginning at about 25 years and progressing at an accelerated rate thereafter The decline in muscle cross-sectional area is most likely due to decreases in total fiber number, especially type II fast-twitch glycolytic fibers. This results in reduced muscle power.[5]
Muscle Fibre changes:[edit | edit source]
Changes in Muscle Fiber Size[edit | edit source]
Elderly individuals often fall because of poor muscle strength and reduced balancing ability related to muscle aging. Types IIA and IIB muscle fibers decrease with age in the area percentage, fiber number percentage, and mean fiber area, whereas Type I fibers increase in area and number but not in size. Morphologically, Type II fibers appeared smaller and flatter. Investigations suggest deterioration in muscle quality and balancing coordination in elderly patients. A research done provided data to help determine treatments for reversing muscle fiber changes and reducing the number of falls and related fractures in patients.[6]The reduction in number of muscle fibers contributes more to the decrease of whole muscle cross-sectional area than does the reduction in area of individual fibers. The individual fast-twitch type II fibers decrease in cross-sectional area suggest that the relative contribution of fast-twitch type II fibers to force generation is less in the older adult.
Motor Unit Number and Size[edit | edit source]
The majority of the literature indicates that muscle fiber loss is due to a loss in motor neurons. There is consistent denervation and reinervation of the muscle fiber throughout one’s lifespan, but in the aged, denervation appears to outpace reinveration. Data indicate that a 60 year-old has approximately 25-50% fewer motor neurons than a 20 year-old, with the greatest losses in distal fast twitch motor neurons With the loss of the motor neuron, the deinervated fast twitch muscle fibers that were attached to it are either permanently deinervated and undergo apoptosis, or are reinverated with a different motor neuron most likely that of a slow twitch neuron, potentially making the fiber take on slow twitch characteristics[7]
Effects of endocrine changes on muscle[edit | edit source]
With increased age, the following changes in endocrine function result in sarcopenia:
- Increased insulin resistance[8]
- Decreased growth hormone[9]
- Reduction in oestrogen and testosterone[10]
- Vitamin D deficiency[11]
- Increased parathyroid hormone[12]
Conditions associated with impairment of skeletal function[edit | edit source]
- Diabetes
- Metabolic syndrome
- Chronic Obstructive Airways Disease (COPD)
- Congestive Cardiac Failure
- Osteoarthritis
- Parkinsons
- Cancer
- Stroke
Functional Effects of Sarcopenia[edit | edit source]
Sarcopenia has a marked effect on function in all activities of daily living, contributing (along with reduction in balance) to reduced gait speed, falls, and fractures. The combination of osteoporosis and sarcopenia results in the frailty which frequently occurs in the elderly population.
Physiotherapy Interventions to minimise or reverse sarcopenia[edit | edit source]
Resistance exercise training :[edit | edit source]
The effects of resisted exercise on ageing muscles is the same as for young muscles:
- improved muscle strength
- increased muscle power - power is a product of both strength and speed. Optimal power reflects how quickly you can exert force to produce the desired movement
- improved muscle composition
Evidence:[edit | edit source]
Population studies[edit | edit source]
Resistance or weight training has been demonstrated to produce increases in muscle strength and power, and also mobility function, in older people living in the following settings:
- independently in the community[13][5][14]
- in nursing homes[15][16]
- hospitalised elderly people[17][18]
Gender differences[edit | edit source]
Increased muscle quality from resistance training is a common finding in older adults, and in men there appears to be no difference in young versus old[19], but there is a study which suggests that older women have a blunted response relative to younger women[20].
Frequency of resistance training[edit | edit source]
Studies have demonstrated that resistance training regimes performed once, twice or even three times a week all result in strength improvements[14].
Length of training programme[edit | edit source]
There are many studies which clearly demonstrate that older people who participate in resistance training programs lasting at least 6 to 12 weeks will show increase in both strength and mobility function[21][22][23].
Cochrane Review[edit | edit source]
The authors collated the results from 121 RCTs examing the effects of resistance strength training exercises, and came to the following conclusions:
"This review provides evidence that PRT (Progressive resistance strength training) is an effective intervention for improving physical functioning in older people, including improving strength and the performance of some simple and complex activities. However, some caution is needed with transferring these exercises for use with clinical populations because adverse events are not adequately reported."[24]
Dietary Advice[edit | edit source]
The Society for Sarcopenia, Cachexia, and Wasting convened an expert panel to develop nutritional recommendations for sarcopenia prevention and management.This panel concluded that for preventing and treating this condition, protein and energy intake are key components, along with both resistance and aerobic exercise.
Is there a role for supplements?[edit | edit source]
There is some evidence suggesting that additional supplementation with the amino acid Leucine (or its metabolite HMB) could potentially increase the effects of resistance training to combat sarcopenia[25][26].
Resources[edit | edit source]
- Aging in Motion (AIM) is a coalition of organizations working to advance research and treatment of sarcopenia and age-related functional decline: aginginmotion.org/
- The American Physical Therapy Association, APTA, www.apta.org/ have a useful document Physical Therapist's Guide to Sarcopenia and Frailty: www.moveforwardpt.com/symptomsconditionsdetail.aspx
References[edit | edit source]
- ↑ Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr. 1997;127(suppl 5):990S-991S.
- ↑ Rolland Y, Czerwinski S, Abellan Van Kan G, Morley JE, Cesari M, Onder G et al: Sarcopenia: its assessment, etiology, pathogenesis, consequences and future perspectives. J Nutr Health Aging. 2008;12(7):433-450.
- ↑ Mayo clinic. Muscle loss and aging. Available from: https://www.youtube.com/watch?v=ymcFS1tQrsk [last accessed 11.5.2019]
- ↑ Short KR, Nair KS. The effect of age on protein metabolism. Curr Opin Clin Nutr Metab Care.2000; 3(1):39-44
- ↑ 5.0 5.1 5.2 Henwood TR, Riek S, Taaffe DR. Strength versus muscle power-specific resistance training in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2008; 63(1):83-91.
- ↑ Lee WS, Cheung WH, Qin L, Tang N, Leung KS. Age-associated decrease of type IIA/B human skeletal muscle fibers. Clin Orthop Relat Res. 2006;450:231-7.
- ↑ Bunn JA. Aging and the Motor Unit. J Sport Medic Doping Studie. 2012; S1:e001. doi:10.4172/2161-0673.S1-e001
- ↑ Refaie MR, Sayed-Ahmed NA, Bakr AM, Aziz MY, El Kannishi MH, Abdel-Gawad SS. Aging is an inevitable risk factor for insulin resistance. Journal of Taibah University Medical Sciences. 2006;1(1):30-41.
- ↑ Toogood AA. Growth hormone (GH) status and body composition in normal ageing and in elderly adults with GH deficiency. Horm Res. 2003; 60(Suppl 1):105-111.
- ↑ Gower BA, Nyman L. Associations among oral estrogen use, free testosterone concentration, and lean body mass among postmenopausal women. J Clin Endocrinol Metab. 2000; 85(12):4476-4480.
- ↑ Wicherts IS, van Schoor NM, Boeke AJ, Visser M, Deeg DJ, Smit J, et al. Vitamin D status predicts physical performance and its decline in older persons. J Clin Endocrinol Metab. 2007; 92(6):2058-2065.
- ↑ Visser M, Deeg DJ, Lips P. Low vitamin D and high parathyroid hormone levels as determinants of loss of muscle strength and muscle mass (sarcopenia): the Longitudinal Aging Study Amsterdam. J Clin Endocrinol Metab. 2003;88(12):5766-5772.
- ↑ Beneka A, Malliou P, Fatouros I, Jamurtas A, Gioftsidou A, Godolias G, et al: Resistance training effects on muscular strength of elderly are related to intensity and gender. J Sci Med Sport. 2005;8(3):274-283.
- ↑ 14.0 14.1 Taaffe DR, Duret C, Wheeler S, Marcus R. Once-weekly resistance exercise improves muscle strength and neuromuscular performance in older adults. J Am Geriatr Soc. 1999; 47(10):1208-1214, 1999
- ↑ Beyer N, Simonsen L, Bulow J, Lorenzen T, Jensen DV, Larsen L, et al. Old women with a recent fall history show improved muscle strength and function sustained for six months after finishing training. Aging Clin Exp Res. 2007;19(4):300-309.
- ↑ Harridge SD, Kryger A, Stensgaard A. Knee extensor strength, activation, and size in very elderly people following strength training. Muscle Nerve. 1999; 22(7):831-839.
- ↑ Hauer K, Specht N, Schuler M, Bärtsch P, Oster P. Intensive physical training in geriatric patients after severe falls and hip surgery. Age Ageing. 2002; 31(1):49-57
- ↑ Suetta C, Magnusson SP, Rosted A, Aagaard P, Jakobsen AK, Larsen LH, et al. Resistance training in the early postoperative phase reduces hospitalization and leads to muscle hypertrophy in elderly hip surgery patients—a controlled, randomized study. J Am Geriatr Soc. 2004;52(12):2016-2022
- ↑ Ivey FM, Tracy BL, Lemmer JT, NessAiver M, Metter EJ, Fozard JL, et al Effects of strength training and detraining on muscle quality: age and gender comparisons. J Gerontol A Biol Sci Med Sci. 2000; 55(3):B152-B157; discussion B8-B9
- ↑ Hakkinen K, Alen M, Kallinen M, Newton RU, Kraemer WJ. Neuromuscular adaptation during prolonged strength training, detraining and re-strength-training in middle-aged and elderly people. Eur J Appl Physiol. 2000;83(1):51-62
- ↑ Galvao DA, Newton RU, Taaffe DR: Anabolic responses to resistance training in older men and women: a brief review. J Aging Phys Act 13:343-358, 200
- ↑ Hunter GR, McCarthy JP, Bamman MM: Effects of resistance training on older adults. Sports Med 34:329-348, 2004
- ↑ Phillips SM: Resistance exercise: good for more than just Grandma and Grandpa’s muscles. Appl Physiol Nutr Metab 32:1198-1205, 200
- ↑ Liu CJ, Latham NK: Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev 3:CD002759, 200
- ↑ Anthony JC, Anthony TG, Kimball SR, Vary TC, Jefferson LS. Orally administered leucine stimulates protein synthesis in skeletal muscle of postabsorptive rats in association with increased elF4F formation. J Nutr. 2000;130:139–145
- ↑ Vukovich MD, Stubbs NB, Bohlken RM. Body composition in 70-year-old adults responds to dietary beta-hydroxy-beta-methylbutyrate similarly to that of young adults. J Nutr. 2001;131:2049–2052