Uterine Prolapse: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (180 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox">'''Original Editors '''- [[User:Amanda Mattingly|Amanda Mattingly]] from [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project]]. '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} </div> | |||
'''Original Editors '''- [[Pathophysiology of Complex Patient Problems| | |||
''' | |||
</div> | |||
== Definition/Description == | == Definition/Description == | ||
[[File:Uterine Prolapse diagram.png|right|frameless|400x400px]] | |||
Uterine prolapse is the herniation of the uterus from its natural anatomical location into the vaginal canal, through the hymen, or through the introitus of the vagina. This is due to the weakening of its surrounding support structures. Uterine prolapse is one of the multiple conditions that are classified under the broader term of [[Pelvic Organ Prolapse|pelvic organ prolapse]]. | |||
* In its usual state, the uterus rests in the apical compartment of pelvic organs. The [[Female Genital Tract|uterus and vagina]] are suspended from the [[sacrum]] and lateral pelvic sidewall via the [[The Uterine And Cervical Ligaments|uterosacral and cardinal ligament complexes]]. The weakening of these ligaments allows for the prolapse of the uterus into the vaginal vault. | |||
* Although uterine prolapse is not inherently life-threatening, it can lead to sexual dysfunction, poor body image, and lower quality of life due to associated bowel or bladder incontinence.<ref name=":0">Chen CJ, Thompson H. [https://www.statpearls.com/ArticleLibrary/viewarticle/30897 Uterine Prolapse]. StatPearls [Internet]. 2020 Nov 19.Available from:https://www.statpearls.com/ArticleLibrary/viewarticle/30897 (accessed 4.4.2021)</ref>.<ref name="three">Bordman R, Telner D, Jackson B, Little D. Step-by-step approach to managing pelvic organ prolapse. Canadian Family Physician; 2007; 53: 485-487.</ref> <ref name="twentyone">Mater Mothers' Hospital. Prolapse. http://brochures.mater.org.au/Home/Brochures/Mater-Mothers--Hospitals/Prolapse (accessed 5 April 2010).</ref> | |||
* Upon diagnosis, patients should be reassured that uterine prolapse is a common and well-known condition. Additionally, educating patients regarding potential sequelae and available treatments will allow them to know what to expect and make them active participants in their own care<ref name=":0" />. | |||
[[File:Uterus and nearby organs.jpeg|right|frameless|350x350px]] | |||
== Etiology == | |||
The risk factors for uterine prolapse are the same as for other pelvic organ prolapses. | |||
* The Oxford Family Planning Association study found that pelvic organ prolapse became more likely with successive births. | |||
* Women with [[Obesity|BMI >25]] were more likely to experience uterine prolapse than women with BMI in the normal range. | |||
* [[Older People - An Introduction|Advancing age]] has been shown to correlate markedly with rates of prolapse. | |||
* Additional risk factors include [[Connective Tissue Disorders|connective tissue disorder]]<nowiki/>s such as [[Marfan Syndrome|Marfan]] syndrome and [[Ehlers-Danlos Syndrome|Ehler’s Danlos]] syndrome<ref name=":0" /> | |||
* | |||
== | == Epidemiology == | ||
It is difficult to distinguish rates of uterine prolapse from pelvic organ prolapse as most studies cohort them together. | |||
* Approximately 50% of women in the US can be expected to have some degree of pelvic organ prolapse in advanced age ( affects 9.7% of women between ages 20-39 and 49.7% of women >80 years old). | |||
* In less developed countries such as Nepal, greater than 1 million women out of approximately 15 million women have been found to have uterine prolapse, equating to approximately 7% of the Nepalese female population<ref name=":0" /> | |||
== | == Clinical Presentation == | ||
Image 3: Uterosacral ligament | |||
[[File:Uterosacral ligament.png|right|frameless]] | |||
The symptoms of uterine prolapse include: | |||
* a sensation of heaviness and pressure in the vagina | |||
* a distinct lump or bulge within the vagina | |||
* a bulge protruding out of the vagina | |||
* painful sexual intercourse. | |||
Uterine prolapse is described in 4 stages, indicating how far it has descended. Other pelvic organs (such as the bladder or bowel) may also be prolapsed into the vagina. | |||
* Stage I – the uterus is in the upper half of the vagina | |||
* Stage II – the uterus has descended nearly to the opening of the vagina | |||
* Stage III – the uterus protrudes out of the vagina | |||
* Stage IV – the uterus is completely out of the vagina<ref name=":1">Vic Health [https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/prolapsed-uterus#treatments-for-uterine-prolapse Uterus Prolapse] Available from:https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/prolapsed-uterus#treatments-for-uterine-prolapse (accessed 4.4.2021)</ref>. | |||
== Treatment/Management == | |||
[[File:Pelvic-floor-muscles hammock.jpg|right|frameless|500x500px]] | |||
Treatment of uterine prolapse is largely dependent on the extent to which a patient is experiencing symptoms. Treatments include surgical and non-surgical options, the choice of which will depend on general health, the severity of the condition and plans for a future pregnancy. | |||
= | Proper diagnosis and management of uterine prolapse can majorly impact a patient’s quality of life and can have long-term physical and mental health effects. Healthcare practitioners should thoroughly counsel patients with uterine prolapse so they can make informed decisions and choose the treatment that is right for them<ref name=":0" />. | ||
Options include: | |||
< | * Pelvic floor exercises | ||
* Vaginal pessary | |||
</ | * Vaginal surgery.<ref name=":1" /> | ||
# Pelvic floor muscle training: | |||
* Typically taught to patients in association with a physiotherapist. They have been shown to result in subjective improvement in symptoms by patients as well as objective improvement in the The Pelvic Organ Prolapse Quantification (POP-Q) system score by examiners. | |||
[[File:Pessary.png|right|frameless|696x696px]] | |||
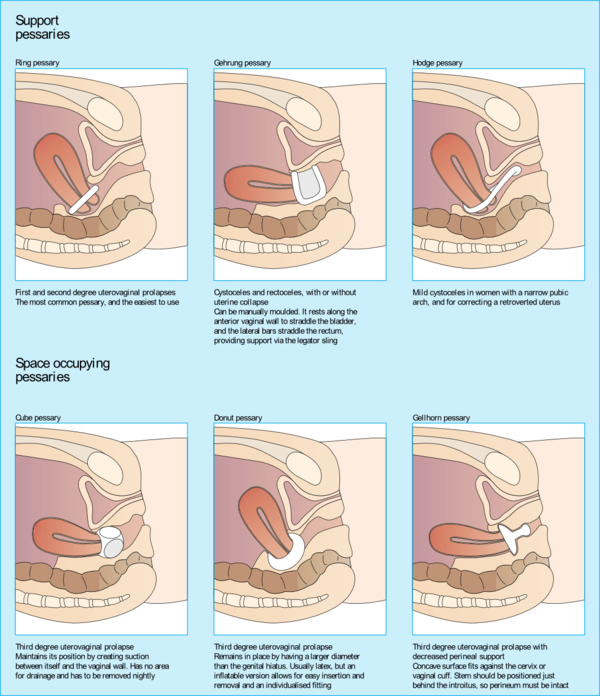
2. Vaginal pessaries: | |||
* Objects often made of silicone that are inserted into the vagina to provide support for the prolapsed pelvic organs. | |||
* Vaginal pessaries can be an effective way of reducing the symptoms of a prolapse, but they will not be appropriate for everyone. Together with pelvic floor exercises, they may provide a non-surgical solution to manage a uterine prolapse. | |||
* Vaginal pessaries provide a solution in 84% of cases of advanced pelvic organ prolapse with mild adverse events in 31% of cases. | |||
* Patients must be fitted for a pessary and commonly try several pessaries before finding the appropriate one. The examiner should be able to sweep a single finger between the pessary and vaginal walls. The patient should be able to walk, bend, and urinate comfortably without shifting the pessary. Complications of pessary placement include vaginal irritation/ulceration, discharge, pain, bleeding, and odor. | |||
* Regular reassessments of pessary fit should be performed to ensure that the pessary is not rubbing against the walls of the vagina, as this can lead to irritation of the vaginal mucosa and predispose patients to infection. Patients with dementia or poor follow up are not good candidates for pessary placement as they require frequent cleaning and regular reassessment of position to prevent complications. | |||
3. Surgical management | |||
* Decision should be made after a detailed discussion with the patient regarding the desire for future vaginal intercourse, effects on body image, cultural views, alternative treatments, and potential complications. | |||
* In moderate to severe cases, the prolapse may have to be surgically repaired. In laparoscopic surgery, instruments are inserted through the navel. The uterus is pulled back into its correct position and reattached to its supporting ligaments. The operation can also be performed with an abdominal incision. | |||
* Surgery may fail and the prolapse can recur if the original cause of the prolapse, such as obesity, coughing or straining, is not addressed<ref name=":1" /><ref name=":0" />. | |||
== | == Physiotherapy == | ||
Physical therapists play a major role in the nonsurgical management of Uterine prolapse. Along with pessary support, pelvic-floor muscle training (PFMT) is cited in highly credible reviews as a main nonsurgical option for women with Uterine prolapse.<ref>Saunders K. [https://academic.oup.com/ptj/article/97/4/455/3057463 Recent advances in understanding pelvic-floor tissue of women with and without pelvic organ prolapse: considerations for physical therapists.] Physical therapy. 2017 Feb 28;97(4):455-63. Available from:https://academic.oup.com/ptj/article/97/4/455/3057463 (last accessed 11.1.2020)</ref> | |||
See the great physiotherapy section in [[Pelvic Organ Prolapse]] | |||
<references /> | == Complications == | ||
The weakness of pelvic floor attachments allowing for prolapse of the apical compartment can additionally allow for prolapse of the anterior and posterior compartments resulting in a compounded cystocele, rectocele, and/or enterocele. These often concomitant conditions can result in urinary incontinence, fecal incontinence, and long term morbidity<ref name=":0" />.<article> | |||
In addition to physical discomfort, it is common for patients to experience anxiety, depression, and poor self-esteem as a result of their condition thus, referral for psychotherapy should be offered<ref name=":0" />. | |||
==References == | |||
<references /> | |||
[[Category:Womens_Health]] | |||
[[Category:Pelvic Health]] | |||
[[Category:Pelvis]] | |||
[[Category:Pelvis - Conditions]] | |||
[[Category:Conditions]] | |||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
Latest revision as of 19:12, 4 April 2021
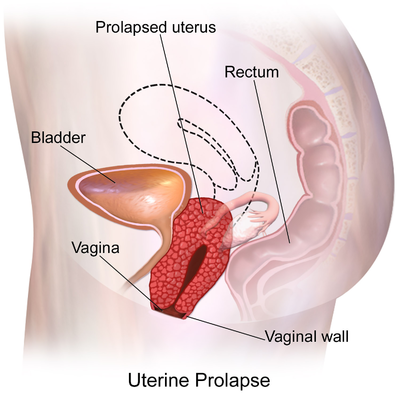
Definition/Description[edit | edit source]
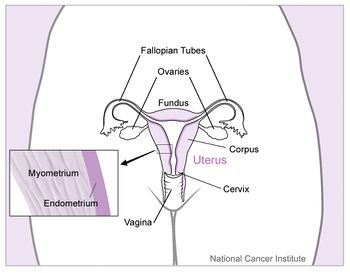
Uterine prolapse is the herniation of the uterus from its natural anatomical location into the vaginal canal, through the hymen, or through the introitus of the vagina. This is due to the weakening of its surrounding support structures. Uterine prolapse is one of the multiple conditions that are classified under the broader term of pelvic organ prolapse.
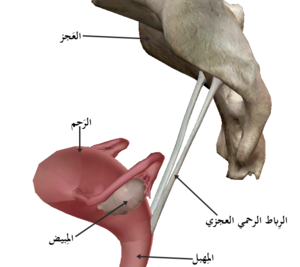
- In its usual state, the uterus rests in the apical compartment of pelvic organs. The uterus and vagina are suspended from the sacrum and lateral pelvic sidewall via the uterosacral and cardinal ligament complexes. The weakening of these ligaments allows for the prolapse of the uterus into the vaginal vault.
- Although uterine prolapse is not inherently life-threatening, it can lead to sexual dysfunction, poor body image, and lower quality of life due to associated bowel or bladder incontinence.[1].[2] [3]
- Upon diagnosis, patients should be reassured that uterine prolapse is a common and well-known condition. Additionally, educating patients regarding potential sequelae and available treatments will allow them to know what to expect and make them active participants in their own care[1].
Etiology[edit | edit source]
The risk factors for uterine prolapse are the same as for other pelvic organ prolapses.
- The Oxford Family Planning Association study found that pelvic organ prolapse became more likely with successive births.
- Women with BMI >25 were more likely to experience uterine prolapse than women with BMI in the normal range.
- Advancing age has been shown to correlate markedly with rates of prolapse.
- Additional risk factors include connective tissue disorders such as Marfan syndrome and Ehler’s Danlos syndrome[1]
Epidemiology[edit | edit source]
It is difficult to distinguish rates of uterine prolapse from pelvic organ prolapse as most studies cohort them together.
- Approximately 50% of women in the US can be expected to have some degree of pelvic organ prolapse in advanced age ( affects 9.7% of women between ages 20-39 and 49.7% of women >80 years old).
- In less developed countries such as Nepal, greater than 1 million women out of approximately 15 million women have been found to have uterine prolapse, equating to approximately 7% of the Nepalese female population[1]
Clinical Presentation[edit | edit source]
Image 3: Uterosacral ligament
The symptoms of uterine prolapse include:
- a sensation of heaviness and pressure in the vagina
- a distinct lump or bulge within the vagina
- a bulge protruding out of the vagina
- painful sexual intercourse.
Uterine prolapse is described in 4 stages, indicating how far it has descended. Other pelvic organs (such as the bladder or bowel) may also be prolapsed into the vagina.
- Stage I – the uterus is in the upper half of the vagina
- Stage II – the uterus has descended nearly to the opening of the vagina
- Stage III – the uterus protrudes out of the vagina
- Stage IV – the uterus is completely out of the vagina[4].
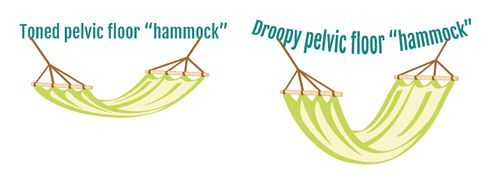
Treatment/Management[edit | edit source]
Treatment of uterine prolapse is largely dependent on the extent to which a patient is experiencing symptoms. Treatments include surgical and non-surgical options, the choice of which will depend on general health, the severity of the condition and plans for a future pregnancy.
Proper diagnosis and management of uterine prolapse can majorly impact a patient’s quality of life and can have long-term physical and mental health effects. Healthcare practitioners should thoroughly counsel patients with uterine prolapse so they can make informed decisions and choose the treatment that is right for them[1].
Options include:
- Pelvic floor exercises
- Vaginal pessary
- Vaginal surgery.[4]
- Pelvic floor muscle training:
- Typically taught to patients in association with a physiotherapist. They have been shown to result in subjective improvement in symptoms by patients as well as objective improvement in the The Pelvic Organ Prolapse Quantification (POP-Q) system score by examiners.
2. Vaginal pessaries:
- Objects often made of silicone that are inserted into the vagina to provide support for the prolapsed pelvic organs.
- Vaginal pessaries can be an effective way of reducing the symptoms of a prolapse, but they will not be appropriate for everyone. Together with pelvic floor exercises, they may provide a non-surgical solution to manage a uterine prolapse.
- Vaginal pessaries provide a solution in 84% of cases of advanced pelvic organ prolapse with mild adverse events in 31% of cases.
- Patients must be fitted for a pessary and commonly try several pessaries before finding the appropriate one. The examiner should be able to sweep a single finger between the pessary and vaginal walls. The patient should be able to walk, bend, and urinate comfortably without shifting the pessary. Complications of pessary placement include vaginal irritation/ulceration, discharge, pain, bleeding, and odor.
- Regular reassessments of pessary fit should be performed to ensure that the pessary is not rubbing against the walls of the vagina, as this can lead to irritation of the vaginal mucosa and predispose patients to infection. Patients with dementia or poor follow up are not good candidates for pessary placement as they require frequent cleaning and regular reassessment of position to prevent complications.
3. Surgical management
- Decision should be made after a detailed discussion with the patient regarding the desire for future vaginal intercourse, effects on body image, cultural views, alternative treatments, and potential complications.
- In moderate to severe cases, the prolapse may have to be surgically repaired. In laparoscopic surgery, instruments are inserted through the navel. The uterus is pulled back into its correct position and reattached to its supporting ligaments. The operation can also be performed with an abdominal incision.
- Surgery may fail and the prolapse can recur if the original cause of the prolapse, such as obesity, coughing or straining, is not addressed[4][1].
Physiotherapy[edit | edit source]
Physical therapists play a major role in the nonsurgical management of Uterine prolapse. Along with pessary support, pelvic-floor muscle training (PFMT) is cited in highly credible reviews as a main nonsurgical option for women with Uterine prolapse.[5]
See the great physiotherapy section in Pelvic Organ Prolapse
Complications[edit | edit source]
The weakness of pelvic floor attachments allowing for prolapse of the apical compartment can additionally allow for prolapse of the anterior and posterior compartments resulting in a compounded cystocele, rectocele, and/or enterocele. These often concomitant conditions can result in urinary incontinence, fecal incontinence, and long term morbidity[1].<article> In addition to physical discomfort, it is common for patients to experience anxiety, depression, and poor self-esteem as a result of their condition thus, referral for psychotherapy should be offered[1].
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Chen CJ, Thompson H. Uterine Prolapse. StatPearls [Internet]. 2020 Nov 19.Available from:https://www.statpearls.com/ArticleLibrary/viewarticle/30897 (accessed 4.4.2021)
- ↑ Bordman R, Telner D, Jackson B, Little D. Step-by-step approach to managing pelvic organ prolapse. Canadian Family Physician; 2007; 53: 485-487.
- ↑ Mater Mothers' Hospital. Prolapse. http://brochures.mater.org.au/Home/Brochures/Mater-Mothers--Hospitals/Prolapse (accessed 5 April 2010).
- ↑ 4.0 4.1 4.2 Vic Health Uterus Prolapse Available from:https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/prolapsed-uterus#treatments-for-uterine-prolapse (accessed 4.4.2021)
- ↑ Saunders K. Recent advances in understanding pelvic-floor tissue of women with and without pelvic organ prolapse: considerations for physical therapists. Physical therapy. 2017 Feb 28;97(4):455-63. Available from:https://academic.oup.com/ptj/article/97/4/455/3057463 (last accessed 11.1.2020)