Olecranon Fracture: Difference between revisions
Rachael Lowe (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) (Removed resource section as links were broken or needed a sign up to access) |
||
| (69 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editor''' - [[User:Andries Derycker|Andries Derycker]] | |||
{ | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | |||
== Definition/Description == | |||
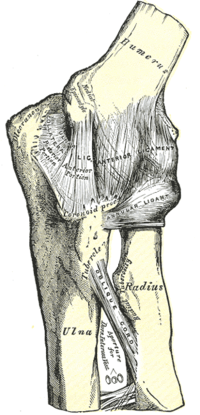
Olecranon fractures frequently occurs with elbow disorders. These fractures are regarded as one of the simplest articular lesions and its operative and physiotherapeutic treatment are straightforward. These fractures are mostly intra-articular and are generally associated with joint effusions and hematomas. Extra-articular fractures include avulsion fractures and are most commonly seen in the elderly.<ref name="Ryan">Donegan RP, Bell J. Operative Techniques in Orthopaedics: Olecranon Fractures. Elsevier, 2010. p.17 -23.</ref><ref name="Stan">Hoppenfeld S, Murthy VL. Treatment and Rehabilitation of Fractures. Lippincot, Williams & Wilkons, 2000.</ref><ref name=":5">Walters J, editor. Orthopaedics - A guide for practitioners. 4th Edition. Cape Town: University of Cape Town, 2010.</ref>[[File:Elbow joint.png|thumb|415x415px]] | |||
== Clinical relevant anatomy == | |||
The [[Elbow|elbow joint]] are made up of the following joints:<ref name=":5" /> | |||
* Ulna-humeral joint: | |||
** Function: Stability; elbow flexion/extention | |||
* Radio-humeral joint | |||
** Function: Lateral stability; forearm pronation/supination | |||
* Proximal radio-ulnar joint | |||
** Function: Forearm pronation/supination | |||
Olecranon function:<ref name=":5" /> | |||
* Insertion point for triceps, thus plays important role in extensor mechanism of the elbow.<ref name="Medical">Meeusen R. Elleboogletsels in Sportrevalidatie. Kluwer, 2009. p.11-15,47.</ref> | |||
* Major articulation for elbow joint | |||
== Epidemiology/Etiology == | |||
=== Mechanism of injury === | |||
* '''Direct''': | |||
** Fall on the forearm | |||
*** The olecranon is forced into the distal humerus by hyper-extending the elbow on an outstretched hand | |||
** Penetrating injuries affecting the articular surface (e.g. panga wounds) | |||
* '''Indirect''': Through triceps contraction | |||
** The contraction of the triceps avulses the olecranon and tears the distal triceps expansion | |||
** Sportsmen (e,g. wrestlers and gymnasts) that generate a lot of isometric arm power (e.g. wrestlers and gymnasts) are at risk | |||
<ref name="Ryan" /><ref name=":5" /><ref name=":0">Lavigne G, Baratz M. [https://www.sciencedirect.com/science/article/pii/S1531091404000439 Fractures of the olecranon.] Journal of the American Society for Surgery of the Hand, 2004;4(2):94-102.</ref> | |||
== Characteristics/Clinical presentation == | |||
=== Clinical presentation === | |||
Patients with a broken olecranon are unable to extend their arm.<ref name="Ryan" /><ref name=":0" /> | |||
== | === Classification === | ||
The Mayo classification system of olecranon fractures are based on the displacement of the olecranon, comminution and elbow stability. There are 3 types of fractures, each with two subtypes.<ref name=":1">Hutchinson DT, Horwitz DS, Ha G, Thomas CW, Bachus KN. [https://journals.lww.com/jbjsjournal/subjects/Elbow/Abstract/2003/05000/Cyclic_Loading_of_Olecranon_Fracture_Fixation.10.aspx Cyclic loading of olecranon fracture fixation constructs.] Journal of Bone and Joint Surgery 2003;85(5):831-7.</ref><ref name=":2">Koslowsky TC, Mader K, Dargel J, Schadt R, Koebke J, Pennig D. [https://www.researchgate.net/profile/Konrad_Mader/publication/24359729_Olecranon_fracture_fixation_with_a_new_implant_Biomechanical_and_clinical_considerations/links/59e88d53a6fdccfe7f8e8a07/Olecranon-fracture-fixation-with-a-new-implant-Biomechanical-and Olecranon fracture fixation with a new implant: biomechanical and clinical considerations.] Injury, 2009;40(6):618-24.</ref><ref name=":3">Kozin SH, Berglund LJ, Cooney WP, Morrey BF, An KN. [https://www.sciencedirect.com/science/article/pii/S1058274696800164 Biomechanical analysis of tension band fixation for olecranon fracture treatment.] Journal of shoulder and elbow surgery, 1996;5(6):442-8.</ref> | |||
* '''Type I:''' Non-comminuted and minimally comminuted fractures | |||
* '''Type II''': Displaced fracture with intact ulnar collateral ligaments | |||
** Displaced vs non-displaced | |||
** Stable fracture | |||
* '''Type III''': Fracture with disruption between the forearm and the humerus | |||
** Displaced vs non-displaced | |||
** Unstable as a result of the disruption of the medial collateral ligament | |||
== Diagnostic procedures == | |||
== | === Physical examination === | ||
* Subjective interview: | |||
** Mechanism of injury: Direct blow to the elbow | |||
** Complaints: | |||
*** Pain over elbow | |||
*** Inability to extend elbow | |||
* Observation: | |||
** Deformity: | |||
*** Obvious around elbow | |||
*** Forearm appears shorter | |||
*** Distortion of bony landmarks of elbow | |||
** Swelling | |||
** Bruising | |||
* Palpation: | |||
** Tender over tip of olecranon and proximal ulna | |||
** Palpable gap at fracture site | |||
* Range of motion: Limited elbow extension | |||
* Neuromuscular examination of the hand to rule out concomitant | |||
<ref name=":5" /> | |||
=== Special investigations === | |||
* [[X-Rays|X-rays]]: AP and lateral views<ref name=":5" /> | |||
{| border="0" cellspacing="1" cellpadding="1" | |||
|- | |||
|[[File:Olecranon Fracture.jpg|center|thumb]] | |||
|[[File:Olecranon Fracture X-Ray.jpg|center|thumb]] | |||
|} | |||
=== Outcome measures === | |||
* [[DASH Outcome Measure|Disabilities of the Arm, Shoulder and Hand (DASH)]] | |||
== | == Medical management == | ||
Management of olecranon fractures depends on displacement, comminution , and elbow stability. Primary elbow instability and fracture morphology are prognostic factors for elbow function and development of arthrosis after operative treatment. The aim of this management is to restore the extensor mechanism of the elbow, and reconstruct the articular surface. | |||
* '''Type I''': 2 weeks immobilization and symptomatic treatment | |||
** Risk of displacement as a result of triceps pull | |||
* '''Type II + III''': Require surgical fixation. | |||
== | <ref name="Ryan" /><ref name="Stan" /><ref name=":1" /><ref name=":2" /><ref name=":3" /><ref name=":4">Rommens PM, Küchle R, Schneider RU, Reuter M. [https://www.sciencedirect.com/science/article/pii/S0020138303005254 Olecranon fractures in adults: factors influencing outcome.] Injury, 2004;35(11):1149-57.</ref> | ||
=== Surgical intervention === | |||
* '''Tension band wiring fixation''': | |||
** Indication: Non-comminuted transverse fractures involving less than half the articular olecranon surface | |||
** Complications: | |||
*** Loss of fixation | |||
*** Non-union | |||
*** Skin breakdown | |||
*** Infection | |||
*** [[Olecranon Bursitis|Olecranon bursitis]] | |||
*** Radial head subluxation | |||
*** Prominent hardware | |||
[[File:Olecranon surgery.jpg|center|thumb]] | |||
* '''Plate fixation''' (more stable): | |||
** Indication: Comminuted fractures | |||
** Good outcomes with regards to union and the prevalence of hardware complications | |||
* '''Intramedullary screw fixation''': | |||
** Indication: Simple, non-comminuted transverse fractures: Intramedullary screw fixation | |||
** Improved pain, function, and range of motion when compared to tension band wiring | |||
* '''Olecranon exision and/or the triceps advancement-technique''': | |||
** Indication: Articular surface is too comminuted or osteoporotic for fixation (elderly/low-demand patients). | |||
** To decrease the risk of instability, the following criteria also applies - Intact: | |||
*** Medial collateral ligament | |||
*** Interosseous membrane | |||
*** Distal radioulnar joint | |||
*** Method: The triceps tendon is reattached to the proximal edge of the articular surface. | |||
<ref name="Ryan" /><ref name="Stan" /><ref name=":1" /><ref name=":2" /><ref name=":3" /><ref name=":4" /> | |||
== | === Complications === | ||
Possible complications with olecranon fractures and surgery thereof, include: | |||
* Permanent extension loss | |||
* [[Heterotopic Ossification|Heterotophic ossification]]<ref name="Stan" /> | |||
* Non-union | |||
* Malunion | |||
== Physiotherapy management == | |||
Precise post-operative care is very important for maximum healing. The functional goal of the physiotherapist is to restore and normalize activities of daily living. Rehabilitation and bone healing will take approximately 12 weeks: | |||
=== Week 1 === | |||
Inflammation phase: | |||
* A splint or cast is applied for fixation, in 60° [[elbow]] flexion to minimize tension on the skin | |||
* Assess capillary refill, [[sensation]], active and passive range of motion of the digits, excessive swelling | |||
* Commence active range of motion of the [[shoulder]], hand and digits (splint to be kept on) | |||
* Oedema management | |||
* After 3 to 4 days: | |||
** Isometric exercises of the wrist | |||
** Gentle active elbow flexion (without splint). | |||
** Active range of motion of the wrist | |||
** Teach patient functional adaptions, e.g. to use the uninvolved extremity for self-care activities | |||
<ref name="Stan" /><ref name="Medical" /> | |||
== | === Week 2 === | ||
Reparative phase: None to minimal stability in the elbow. | |||
* Extension to the elbow < 90° is not permitted in a cast or splint | |||
* Splint or cast removed in most cases | |||
* Gentle isometric exercises of the biceps | |||
* Isotonic exercises to the digits | |||
<ref name="Stan" /><ref name="Medical" /> | |||
=== Week 4-6 === | |||
Fracture now partially stable: | |||
* Active and active-assistive range of motion to the shoulder, elbow and wrist | |||
* Avoid passive range of motion at the elbow | |||
* Isometric exercises to the elbow and wrist in flexion and extension | |||
* Activities of daily living: Uses the affected extremity for stability and light self-care | |||
<ref name="Stan" /><ref name="Medical" /> | |||
== | === Week 8-12 === | ||
If fracture is clinically and radiographically healed: | |||
* Progressively weight bearing through affected limb | |||
* Resistive exercises to elbow flexors and extensors | |||
* Active and active-assistive range of motion to the elbow and wrist in all planes (until satisfactory range is achieved) | |||
* There may be some limitations in elbow extension: | |||
** Gentle passive stretching may be necessary | |||
** Dynamic splint may be used for passive elbow stretch | |||
<ref name="Stan" /><ref name="Medical" /> | |||
== Clinical bottom line == | |||
<div class="researchbox"> | |||
Olecranon fractures are typically caused by a direct blow to the elbow, but an avulsion fracture can also be caused with excessive triceps contraction. Surgical management is the treatment of choice, with specific guidelines for physiotherapy going with it. Even with the best rehabilitation, permanent loss of some elbow extension is a common side-effect of this fracture. | |||
</div> | |||
== References == | == References == | ||
<references /> | |||
<references /> | |||
[[Category:Vrije_Universiteit_Brussel_Project]] | |||
[[Category:Primary Contact]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Sports Injuries]] | |||
[[Category:Elbow]] | |||
[[Category:Conditions]] | |||
[[Category:Elbow - Conditions]] | |||
[[Category:Fractures]] | |||
Latest revision as of 14:35, 7 December 2023
Original Editor - Andries Derycker
Top Contributors - Derycker Andries, Marlies Verbruggen, Leana Louw, Admin, Rachael Lowe, Kim Jackson, Claire Knott, Wanda van Niekerk, Lucinda hampton, WikiSysop and Simisola Ajeyalemi
Definition/Description[edit | edit source]
Olecranon fractures frequently occurs with elbow disorders. These fractures are regarded as one of the simplest articular lesions and its operative and physiotherapeutic treatment are straightforward. These fractures are mostly intra-articular and are generally associated with joint effusions and hematomas. Extra-articular fractures include avulsion fractures and are most commonly seen in the elderly.[1][2][3]
Clinical relevant anatomy[edit | edit source]
The elbow joint are made up of the following joints:[3]
- Ulna-humeral joint:
- Function: Stability; elbow flexion/extention
- Radio-humeral joint
- Function: Lateral stability; forearm pronation/supination
- Proximal radio-ulnar joint
- Function: Forearm pronation/supination
Olecranon function:[3]
- Insertion point for triceps, thus plays important role in extensor mechanism of the elbow.[4]
- Major articulation for elbow joint
Epidemiology/Etiology[edit | edit source]
Mechanism of injury[edit | edit source]
- Direct:
- Fall on the forearm
- The olecranon is forced into the distal humerus by hyper-extending the elbow on an outstretched hand
- Penetrating injuries affecting the articular surface (e.g. panga wounds)
- Fall on the forearm
- Indirect: Through triceps contraction
- The contraction of the triceps avulses the olecranon and tears the distal triceps expansion
- Sportsmen (e,g. wrestlers and gymnasts) that generate a lot of isometric arm power (e.g. wrestlers and gymnasts) are at risk
Characteristics/Clinical presentation[edit | edit source]
Clinical presentation[edit | edit source]
Patients with a broken olecranon are unable to extend their arm.[1][5]
Classification[edit | edit source]
The Mayo classification system of olecranon fractures are based on the displacement of the olecranon, comminution and elbow stability. There are 3 types of fractures, each with two subtypes.[6][7][8]
- Type I: Non-comminuted and minimally comminuted fractures
- Type II: Displaced fracture with intact ulnar collateral ligaments
- Displaced vs non-displaced
- Stable fracture
- Type III: Fracture with disruption between the forearm and the humerus
- Displaced vs non-displaced
- Unstable as a result of the disruption of the medial collateral ligament
Diagnostic procedures[edit | edit source]
Physical examination[edit | edit source]
- Subjective interview:
- Mechanism of injury: Direct blow to the elbow
- Complaints:
- Pain over elbow
- Inability to extend elbow
- Observation:
- Deformity:
- Obvious around elbow
- Forearm appears shorter
- Distortion of bony landmarks of elbow
- Swelling
- Bruising
- Deformity:
- Palpation:
- Tender over tip of olecranon and proximal ulna
- Palpable gap at fracture site
- Range of motion: Limited elbow extension
- Neuromuscular examination of the hand to rule out concomitant
Special investigations[edit | edit source]
Outcome measures[edit | edit source]
Medical management[edit | edit source]
Management of olecranon fractures depends on displacement, comminution , and elbow stability. Primary elbow instability and fracture morphology are prognostic factors for elbow function and development of arthrosis after operative treatment. The aim of this management is to restore the extensor mechanism of the elbow, and reconstruct the articular surface.
- Type I: 2 weeks immobilization and symptomatic treatment
- Risk of displacement as a result of triceps pull
- Type II + III: Require surgical fixation.
Surgical intervention[edit | edit source]
- Tension band wiring fixation:
- Indication: Non-comminuted transverse fractures involving less than half the articular olecranon surface
- Complications:
- Loss of fixation
- Non-union
- Skin breakdown
- Infection
- Olecranon bursitis
- Radial head subluxation
- Prominent hardware
- Plate fixation (more stable):
- Indication: Comminuted fractures
- Good outcomes with regards to union and the prevalence of hardware complications
- Intramedullary screw fixation:
- Indication: Simple, non-comminuted transverse fractures: Intramedullary screw fixation
- Improved pain, function, and range of motion when compared to tension band wiring
- Olecranon exision and/or the triceps advancement-technique:
- Indication: Articular surface is too comminuted or osteoporotic for fixation (elderly/low-demand patients).
- To decrease the risk of instability, the following criteria also applies - Intact:
- Medial collateral ligament
- Interosseous membrane
- Distal radioulnar joint
- Method: The triceps tendon is reattached to the proximal edge of the articular surface.
Complications[edit | edit source]
Possible complications with olecranon fractures and surgery thereof, include:
- Permanent extension loss
- Heterotophic ossification[2]
- Non-union
- Malunion
Physiotherapy management[edit | edit source]
Precise post-operative care is very important for maximum healing. The functional goal of the physiotherapist is to restore and normalize activities of daily living. Rehabilitation and bone healing will take approximately 12 weeks:
Week 1[edit | edit source]
Inflammation phase:
- A splint or cast is applied for fixation, in 60° elbow flexion to minimize tension on the skin
- Assess capillary refill, sensation, active and passive range of motion of the digits, excessive swelling
- Commence active range of motion of the shoulder, hand and digits (splint to be kept on)
- Oedema management
- After 3 to 4 days:
- Isometric exercises of the wrist
- Gentle active elbow flexion (without splint).
- Active range of motion of the wrist
- Teach patient functional adaptions, e.g. to use the uninvolved extremity for self-care activities
Week 2[edit | edit source]
Reparative phase: None to minimal stability in the elbow.
- Extension to the elbow < 90° is not permitted in a cast or splint
- Splint or cast removed in most cases
- Gentle isometric exercises of the biceps
- Isotonic exercises to the digits
Week 4-6[edit | edit source]
Fracture now partially stable:
- Active and active-assistive range of motion to the shoulder, elbow and wrist
- Avoid passive range of motion at the elbow
- Isometric exercises to the elbow and wrist in flexion and extension
- Activities of daily living: Uses the affected extremity for stability and light self-care
Week 8-12[edit | edit source]
If fracture is clinically and radiographically healed:
- Progressively weight bearing through affected limb
- Resistive exercises to elbow flexors and extensors
- Active and active-assistive range of motion to the elbow and wrist in all planes (until satisfactory range is achieved)
- There may be some limitations in elbow extension:
- Gentle passive stretching may be necessary
- Dynamic splint may be used for passive elbow stretch
Clinical bottom line[edit | edit source]
Olecranon fractures are typically caused by a direct blow to the elbow, but an avulsion fracture can also be caused with excessive triceps contraction. Surgical management is the treatment of choice, with specific guidelines for physiotherapy going with it. Even with the best rehabilitation, permanent loss of some elbow extension is a common side-effect of this fracture.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Donegan RP, Bell J. Operative Techniques in Orthopaedics: Olecranon Fractures. Elsevier, 2010. p.17 -23.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Hoppenfeld S, Murthy VL. Treatment and Rehabilitation of Fractures. Lippincot, Williams & Wilkons, 2000.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Walters J, editor. Orthopaedics - A guide for practitioners. 4th Edition. Cape Town: University of Cape Town, 2010.
- ↑ 4.0 4.1 4.2 4.3 4.4 Meeusen R. Elleboogletsels in Sportrevalidatie. Kluwer, 2009. p.11-15,47.
- ↑ 5.0 5.1 Lavigne G, Baratz M. Fractures of the olecranon. Journal of the American Society for Surgery of the Hand, 2004;4(2):94-102.
- ↑ 6.0 6.1 6.2 Hutchinson DT, Horwitz DS, Ha G, Thomas CW, Bachus KN. Cyclic loading of olecranon fracture fixation constructs. Journal of Bone and Joint Surgery 2003;85(5):831-7.
- ↑ 7.0 7.1 7.2 Koslowsky TC, Mader K, Dargel J, Schadt R, Koebke J, Pennig D. Olecranon fracture fixation with a new implant: biomechanical and clinical considerations. Injury, 2009;40(6):618-24.
- ↑ 8.0 8.1 8.2 Kozin SH, Berglund LJ, Cooney WP, Morrey BF, An KN. Biomechanical analysis of tension band fixation for olecranon fracture treatment. Journal of shoulder and elbow surgery, 1996;5(6):442-8.
- ↑ 9.0 9.1 Rommens PM, Küchle R, Schneider RU, Reuter M. Olecranon fractures in adults: factors influencing outcome. Injury, 2004;35(11):1149-57.