Heterotopic Ossification: Difference between revisions
No edit summary |
No edit summary |
||
| Line 87: | Line 87: | ||
• Diagnostic and therapeutic follow-up purposes<br>• Phases 1 and 2 are indicative of hyperemia and blood pooling (precursors to process of HO)<br>• Usually positive after 2-4 weeks<br>• Serial bone scans used to monitor metabolic activity of HO to determine optimal timing for surgical resection and to predict postoperative occurrence <br><br> | • Diagnostic and therapeutic follow-up purposes<br>• Phases 1 and 2 are indicative of hyperemia and blood pooling (precursors to process of HO)<br>• Usually positive after 2-4 weeks<br>• Serial bone scans used to monitor metabolic activity of HO to determine optimal timing for surgical resection and to predict postoperative occurrence <br><br> | ||
'''Radiography<sup></sup>'''<sup>[1]</sup><br>• Soft tissue mass is the earliest radiographic finding<br>• HO seen on radiographs 4-6 weeks post-injury Typical appearance is circumferential ossification with a lucent center<br>• Cannot detect the mineralization of HO during first weeks after trauma/onset<br>• Frequently used to classify HO following THA <br>• Differential diagnosis: avulsion fracture fragments, osteochondral bodies, nonosseous soft tissue calcification and osteosarcoma<br><br> | '''Radiography<sup></sup>'''<sup>[1]</sup><br>• Soft tissue mass is the earliest radiographic finding<br>• HO seen on radiographs 4-6 weeks post-injury Typical appearance is circumferential ossification with a lucent center<br>• Cannot detect the mineralization of HO during first weeks after trauma/onset<br>• Frequently used to classify HO following THA <br>• Differential diagnosis: avulsion fracture fragments, osteochondral bodies, nonosseous soft tissue calcification and osteosarcoma<br><br> | ||
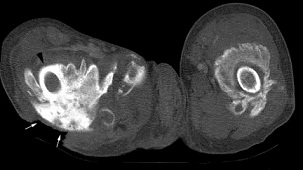
'''MRI and CT Scan'''<sup>[1]</sup>[[Image:HO MRI.jpg|frame|right|MRI showing heterotopic ossification (arrows)]]<br>• MRI not routinely used for evaluation of HO<br>• CT may detect soft tissue ossification at earlier stages than standard radiograph<br><br> | '''MRI and CT Scan'''<sup>[1]</sup>[[Image:HO MRI.jpg|frame|right|MRI showing heterotopic ossification (arrows)]]<br>• MRI not routinely used for evaluation of HO<br>• CT may detect soft tissue ossification at earlier stages than standard radiograph<br><br> | ||
<br> | <br> | ||
| Line 109: | Line 109: | ||
<br> | <br> | ||
<br> | |||
<br> | |||
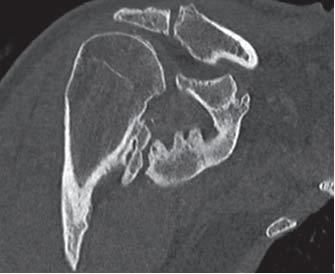
[[Image:HO CT scan.jpg|frame|left|CT scan showing heterotopic ossification of proximal femur]] | [[Image:HO CT scan.jpg|frame|left|CT scan showing heterotopic ossification of proximal femur]] | ||
<br> | |||
<br> | |||
<br> | <br> | ||
| Line 141: | Line 141: | ||
*high sensitivity and specificity for early detection of HO 1-week post-THR. | *high sensitivity and specificity for early detection of HO 1-week post-THR. | ||
''<u>'''Clinical Note:'''</u>''<u></u> the lack of simple objective measures in detecting heterotopic bone formation causes HO to be misdiagnosed in the early stages, leading to delayed treatment.<ref name="Hsu" / | ''<u>'''Clinical Note:'''</u>''<u></u> the lack of simple objective measures in detecting heterotopic bone formation causes HO to be misdiagnosed in the early stages, leading to delayed treatment.<ref name="Hsu" /> | ||
== Systemic Involvement == | == Systemic Involvement == | ||
Revision as of 23:14, 2 April 2017
Original Editors - Bruce Tan as part of the from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Bruce Tan, Morgan Yoder, Hannah McCabe, Naomi O'Reilly, Lucinda hampton, Admin, Elaine Lonnemann, 127.0.0.1, Wendy Walker, WikiSysop and Kim JacksonDefinition/Description[edit | edit source]
Heterotopic Ossification (HO) refers to the formation of lamellar bone inside soft tissue structures where bone does not normally exist. This process can occur in structures such as the skin, subcutaneous tissue, skeletal muscle, and fibrous tissue adjacent to bone. In more rare forms, HO has also been described in the walls of blood vessels and intra-abdominal sites such as the mesentery.[1]
Research suggests four factors which contribute to formation of heterotopic bone: 1) inciting event (usually trauma), 2) a signal from the site of injury, 3) a supply of mesenchymal cells whose genetic machinery is not fully committed, 4) an environment which is conducive to the continued formation of new bone.[1] These factors are discussed more indepth in the Etiology/Causes section.
HO was fisrt described by by Patin in 1692 while working with children diagnosed with myositis ossificans progressiva.[2] In 1918, Dejerine & Ceillier detailed the anatomical, clinical, and histological features of ectopic bone formation in soldiers who sustained spinal injuries during World War I.[3]
Following the work of Dejerine & Ceillier, Marshall Urist described the osteoinducive properties of bone morphogenic protein in ectopic areas such as muscle. This was and still is considered a "landmark discovery" in orthopedic research.[4] Two of the original reasearch articles by Urist can be found below:
Etiology/Causes
[edit | edit source]
The exact pathophysiology of HO is unknown. The transformation of primitive mesenchymal cells in connective tissue into osteoblastic tissue and osteoid involve diverse and poorly understood triggers.[1] These triggers include genetic, post-traumatic, neurogenic, post-surgical, and reactive lesions of hands and feet.
Genetic forms include two types: Fibrodysplasia Ossificans Progressive (FOP) and Progressive Osseous Heteroplasia(POH). These types are described as massive deposits of heterotopic bone around multiple joints in the absence of an inciting event (i.e. trauma).[2] This is the most severe type of HO, progressively forming throughout the life and severely effecting health, life expectancy, and quality of life. (B
MP)
Post-traumatic HO begins with spindle cell proliferation within the first week of the traumatic event. Within 1-2 weeks, primitive osteoid develops. After the second week, primitive cartilage and woven bone can be seen. Trabecular bone forms 2-5 weeks after the trauma. Amorphous calcium phosphate is gradually replaced by hydroxyapatite crystals as the mineralization progresses. After about 6 months, there is an appearance of true bone in the connective tissue between the muscle planes.[1]
Neurogenic heterotopic ossification occurs after sickle cell anemia, hemophilia, tetanus, poliomyelitis, multiple sclerosis, and toxic epidermal necrolysis. Neurogenic HO develops only in sites distal to the level of the spinal cord injury. The areas affected by HO are almost always on the affected side of brain injury or stroke.[1]
Post-surgical HO most commonly develops after procedures which require open reduction, internal fixation and joint replacement surgeries, with THA being the most common.[2]
Reactive lesions of the hands and feet are usually associated with the periosteum or periarticular fibrous tissue, which differentiates the category from myositis ossificans. These lesions occur in three clinico-radiologic settings: 1) bizzare parosteal osteochondromatous, 2) florid reactive periositis, and 3) subungual exostoses.[2]
Prevalence[edit | edit source]
• Following lower extremity amputation: 7%[6]
• Following TBI: 11% (ranges reported from 10-20%)[6]
Hip most common, followed by elbow[1][7]
• Following SCI: 20% (ranges reported from 20-40%)[6]
• Following THA: 55%[1]
• 83% if open reduction and internal fixation is performed following TKA: 15% (ranges reported from 1-42%)[8]
• Following elbow fracture and/or dislocation: 90%[1]
Following forearm fracture: 20%
In a recent study, Foruria et al. looked at the prevalence of heterotopic ossification in all elbow pathologies entering an emergency room over a 5 year period. They found the highest prevalence of HO occurred in terrible triad injuries, transolecranon fracture-dislocations, and an associated distal humeral fracture. The location of the ossification was most commonly found on the posterior aspect of the ulna. Risk factors for HO include dislocation or subluxation at the time of injury, open injury, and severe chest injury. When a pathology was treated surgically, 37% of participants developed an ossification.[7]
Clinical Diagnosis
[edit | edit source]
Clinical signs and symptoms of HO may appear as soon as 3 weeks or up to 12 weeks after initial musculoskeletal trauma, spinal cord injury, or other precipitating event.[9] The first sign of HO is generally loss of joint mobility and subsequently loss of function. Other findings that may suggest the presence of HO include swelling, erythema, heat, local pain, palpable mass, and contracture formation. In some cases, a fever may be present.[1]
Differential Diagnoses: The initial inflammatory phase of HO may mimic other pathologies such as cellulitis, thrombophlebitis, osteomyelitis, or a tumorous process.[4][3] Other differential diagnoses include DVT, septic arthritis, hematoma, or fracture. DVT and HO have been positively associated. This is thought to be due to the mass effect and local inflammation of the HO, encouraging thrombus formation. The thrombus formation is caused by venous compression and phlebitis.[1]
Classification Systems
[edit | edit source]
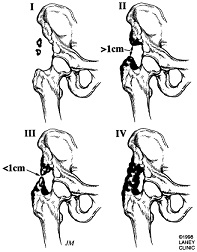
Brooker Classification of Heterotopic Ossification (Following THA)[10]
Class 1: Island of bone within a soft tissue about the hip
Class 2: Bone spurs originating from the pelvis of proximal end of femur leaving at least 1 cm between opposing bone surfaces
Class 3: Bone spurs originating from pelvis or proximal femur leaving <1 cm between opposing bone surfaces
Class 4: Ankyloses of the hip
Brooker did not describe a class 0 but subsequent studies using the Brooker classification have defined Class 0 as the absence of radiographic HO.
Schmidt and Hackenbrock Classification of Heterotopic Ossification (Following THA)[1]
Region 1: Heterotopic ossification strictly below the tip of the greater trochanter
Region 2: Heterotopic ossification below and above the tip of the greater trochanter
Region 3: Heterotopic ossification strictly above the tip of the greater trochanter
Grade A: Single or multiple heterotopic ossification <10 mm in maximal extent without contact with pelvis or femur
Grade B: Heterotopic ossification >10 mm without contact with the pelvis but with possible contact with the femur; no bridging from the femur to the proximal part of the greater trochanter; no evidence of ankyloses
Grade C: Ankylosis by means of firm bridging from femur to pelvis
McAfee’s Classification of Heterotopic Ossification (Following Total Disc Arthroplasty)[11]
0: No HO
1: Islands of bone not within the margins of the disc and not interfering with motion
2: Bone within the margins of the disc but not blocking motion
3: Bone within the margins of the disc and interfering with motion of the prosthesis
4: Bone ankylosis
Stages of Development
[edit | edit source]
Chronology of Development of Heterotopic Ossification[12]
- 0 days: +/- erythema, swelling, tenderness
- 7 days: clinically palpable mass
- 7-14 days: poorly defined shadow on radiograph
- 14-21 days: osteoid deposition, radiographic shadows
- 21-35 days: fluffy radiodensities; the “dotted veil” effect
- 24 days: definite radiographic evidence
- 30 days: mineralization shows a zonal pattern (best seen on CT scan)
- 45 days: histologic “zonal” pattern evident, reflecting well-formed mineralization at the periphery
- 180-365 days: development of mature bone
Diagnostic Tests and Lab Tests[edit | edit source]
Ultrasonography[13]
• Detection of HO 2 weeks earlier than by x-ray
• More accurate than any laboratory tests
• Help clinicians advocate for prompt/aggressive physical therapy
• Eliminates high false-positive rate of physical exam alone
Three-phase bone scintigraphy[4]
• Diagnostic and therapeutic follow-up purposes
• Phases 1 and 2 are indicative of hyperemia and blood pooling (precursors to process of HO)
• Usually positive after 2-4 weeks
• Serial bone scans used to monitor metabolic activity of HO to determine optimal timing for surgical resection and to predict postoperative occurrence
Radiography[1]
• Soft tissue mass is the earliest radiographic finding
• HO seen on radiographs 4-6 weeks post-injury Typical appearance is circumferential ossification with a lucent center
• Cannot detect the mineralization of HO during first weeks after trauma/onset
• Frequently used to classify HO following THA
• Differential diagnosis: avulsion fracture fragments, osteochondral bodies, nonosseous soft tissue calcification and osteosarcoma
MRI and CT Scan[1]
• MRI not routinely used for evaluation of HO
• CT may detect soft tissue ossification at earlier stages than standard radiograph
Prostoglandin E2: (PGE2)
- monitior PGE2 excretion in 24-hour urinalysis
- PGE2 felt to be reliable bone marker for early detection and determining treatment efficacy
- A sudden increase is an indication for bone scintigraphy
Alkaline Phosphatase: (ALP)[4]
- frequently used in early detection of HO
- High sensitivity, low specificity
- Serum ALP levels can be dependent on renal and hepatic function, so they are not always useful.
Ultrasonography:
- earlier detection than conventional ragiograph
- local signs of inflammation in SCI patients are suggestive of HO
- high sensitivity and specificity for early detection of HO 1-week post-THR.
Clinical Note: the lack of simple objective measures in detecting heterotopic bone formation causes HO to be misdiagnosed in the early stages, leading to delayed treatment.[4]
Systemic Involvement[edit | edit source]
Evidence shows that there are no systemic effects secondary to the formation of heterotopic ossification. The most common sites where this condition presents are the hips, knees, spine, elbow, wrists, hands, and any site which is involved in a traumatic event.
Medical Management (current best evidence)[edit | edit source]
The treatment of heterotopic ossification is largely dependent on the amount of ectopic bone formation, the location and the associated functional limitations of the patient.
The first goal of medical management is to identify those patients at risk for developing HO and treating them prophylactically (see medications section). Research supports two other approaches for the medical management of HO: 1)surgical excision and 2) radiation therapy.
Sugical intervention:
The two main goals of sugical intervention are to alter the position of the affected joint or improve its range of motion (ROM).[3]. Through his work, Garland has created a recommended timetable for surgical intervention:[5]
- 6 months following traumatic development of HO
- 1-year following development of HO secondary to a spinal cord injury
- 18 months following development of HO secondary to head injury
The above timetables were established to determine the most optimal timing of surgical intervention. Clinicians must determine if the lesion has reached maturation before surgical excision to decrease the risk of intraoperative complcations such as hemorrhage, and the reoccurance of the ectopic lesion.[6] The use of bone scans to determine metabolic activity of the lesion and serum ALP levels are common aids in this decision making process.
Shehab et al. also describe a criteria for recommending surgical removal of heterotopic ossification. The criteria are as follows:[6]
- significantly limited ROM of involved joint (e.g., hip should have < 50o ROM); for most patients, progression to joint ankylosis is the most serious complication of heterotopic ossification.File:Shoulder HO CT3D 2.JPG3D CT reconstruction of same shoulder (Chao et al.)
- Absence of local fever, swelling, erythema, or other clinical findings of actue heterotopic ossification.
- Normal serum alkaline phosphate levels.
- Return of bone scan findings to normal or near normal; if serial quantitative bone scans are obtained, there should be a sharply decreasing trend followed by a steady state for 2-3 months.
Radiotherapy:
- The use of radiotherapy as a prophylactic treatment comes mainly from the literature concerning total hip arthroplasty.[4]
- Radiating pluripotential mesenchymal cells may effectively prevent the development of HO.[7]
- A dose of 700-800 cGy of local radiation in the first four post-operative days has shown to prevent HO formation in patients who are at high risk.[4]
<span id="fck_dom_range_temp_1301766677195_863" /><span id="fck_dom_range_temp_1301766677195_498" />
<span id="fck_dom_range_temp_1301766773393_61" /><span id="fck_dom_range_temp_1301766773393_201" />
Physical Therapy Management (current best evidence)[edit | edit source]
Physical therapy has been shown to benefit patients suffering from heterotopic ossification. Pre-operative PT can be used to help preseve the structures around the lesion. ROM exercises (PROM, AAROM, AROM) and strengthening will help prevent muscle atrophy and preserve joint motion.
Clinical note: caution must be taken when working with patients with known heterotopic lesions. Therapy which is too aggressive can aggrevate the condition and lead to inflammation, erythema, hemorrhage, and increased pain.
Post-operative rehabilitation has also shown benefit patients with recent surgical resection of heterotopic ossification. The post-op management of HO is similar to pre-op treatment but much more emphasis is placed on edema control, scar management, and infection prevention. Calandruccio et al. outlined a rehabilitation protocol for patients who underwent surgical excision of heterotopic ossification of the elbow. The phases of rehab and goals for each phase are as follows:[8]
Phase I (Week 1)
- Goals
- Prevent infection
- Protect and decrease stress on surgical site
- Decrease pain
- Control and decrease edema
- ROM to 80% of affected joint
- Maintain ROM of joint proximal and distal to surgical site
Phase II (2-8 weeks)
- Goals
- Reduce pain
- Manage edema
- Encourage limited ADL performances
- Promote scar mobility and proper remodeling
- Promote full ROM of affected joint
- Encourage quality muscle contractions
Phase III (9-24 weeks)
- Goals
- Self-manage pain
- Prevent flare-up with functional activities
- Improve strength
- Improve ROM (if still limited)
- Return to previous levels of activity
Casavant and Hastings also provide great insight into the evaluation and management of heterotopic ossification in their article titled Heterotopic Ossification about the Elbow: A Therapist’s Guide to Evaluation and Management.[9]
Clinical Note: The two studies used above were primarily focused on rehabiliatation of the elbow secondary to heterotopic ossification. However, the goals and stages of the rehabilitation process can be used as a guide when treating at other sites.
Differential Diagnosis[edit | edit source]
Since radiography is the most common form of imaging used to diganose heterotopic ossification, the presence of an opaque lesion can mislead the clinician initially. Important categories to consider when contemplating a differential diagnosis for HO include the following:[2],[6]
- Tumors→ osteosarcoma, osteochondroma
K. Liu et al. discuss a variety of tumorous processes which have been assosiated with sites developing HO.[10]
- Infection→osteomyelitis
- Inflammation→ cellulitis
- Circulatory complications→ deep vein thrombosis, thrombophlebitis
Case Reports/ Case Studies[edit | edit source]
Tibiofibular Syndesmosis and Ossification. Case Report: Sequelae of Ankle Sprains in an Adolescent Football Player.
Heterotopic Mesenteric Ossification ("intraabdominal myositis ossificans): A Case Report.
A Case of Psoas Ossification from the use of BMP-2 for Posterolateral Fusion at L4-L5.
- Brower RS, Vickroy NM. A case of psoas ossification from the use of BMP-2
for posterolateral fusion at L4–L5.Spine 2008; 18: 653-655.<span id="fck_dom_range_temp_1299789628126_629" />
Infrapatellar Heterotopic Ossification after Anterior Cruciate Ligament Reconstruction.
- Valencia H, Gavín C. Infrapatellar heterotopic ossification after anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy: Official Journal Of The ESSKA [serial on the Internet. (2007, Jan), [cited March 31, 2011]; 15(1): 39-42. Available from: MEDLINE.]
Heterotopic Ossification of the Ulnar Collateral Ligament: A Description of a Case in a Top Level Weightlifting Athlete.
- A Giombini, L Innocenzi, G Massazza, F Fagnani, et al. Heterotopic ossification of the ulnar collateral ligament: a description of a case in a top level weightlifting athlete. Journal of Sports Medicine and Physical Fitness. 2005 Sep 1;45(3): 370-80. In: ProQuest Medical Library [database on the Internet [cited 2011 Mar 31]. Available from: ProQuest; Document ID: 942792311]
Resources
[edit | edit source]
The Mystery of Heterotopic Ossification and How it Affected My Life
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1NOY_AEF8gNY3HRCwoXdtFZj9G-OSG0TNDAFjiqNOh_xvySEXY|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ 1.0 1.1 McCarthy EF, Sundaram M. Heterotopic ossification: a review. Skeletal Radiol 2005; 34: 609-619.
- ↑ 2.0 2.1 Bossche LV, Vanderstraeten G. Heterotopic ossification: a review. J Rehabil Med 2005; 37: 129-136.
- ↑ 3.0 3.1 Pape HC et al. Current concepts in the development of hetetrotopic ossification. Journ Bone and Joint Surg 2004; 86: 783-787.
- ↑ 4.0 4.1 4.2 4.3 4.4 Cite error: Invalid
<ref>tag; no text was provided for refs namedHsu - ↑ Garland DE. A clinical perspective on common forms of acquired heterotopic ossification. Clin Orthop 1991; 263: 13-29.
- ↑ 6.0 6.1 6.2 Cite error: Invalid
<ref>tag; no text was provided for refs namedShehab et al. - ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedChao - ↑ Pho C, Godges J. Heterotopic ossification about the elbow: repair and rehabilitation. KPSoCal Ortho PT Residency.
- ↑ Casavant AM and Hasting H. Heterotopic ossification about the elbow: a therapist’s guide to evaluation and management. Journal of Hand Therapy 2006; 19: 255-267.
- ↑ Liu K, Tripp S, Layfield LJ. Heterotopic ossification: review of histological findings and tissue distribution in a 10-year experience. Research and Practice 2007; 203: 633-640.