Anterior Cruciate Ligament (ACL) Reconstruction
This article requires a page merger with a similar article of a similar name or containing repeated information. (9 May 2024)
Original Editors - Dorien Scheirs
Top Contributors - Aarti Sareen, Laura Ritchie, Admin, Kim Jackson, Scott Cornish, Tony Lowe, Beverly Klinger, Dorien Scheirs, Evan Thomas, Tarina van der Stockt, WikiSysop, Simisola Ajeyalemi, Rachael Lowe, William Jones, Mariam Hashem, Claire Knott, Wanda van Niekerk, Olajumoke Ogunleye, Scott Buxton, Venus Pagare and George Prudden
Definition/Description[edit | edit source]
The anterior cruciate ligament (ACL) is important for maintaining the stability in the knee, particularly in activities involving cutting, pivoting or kicking. People with ruptured ACLs have unstable knees that generally become more damaged over time. ACL reconstruction is the surgical treatment of choice which is done in certain conditions and stage.
NONOPERATIVE TREATMENT IS PREFERED
- Older than 35 years age
- No or minimal anterior tibialy sublaxation
- No additional intraarticular injury
- Minimal athletic participation.
OPERATIVE TREATMENT IS PREFERRED
- Younger than 25 years
- Marked anterior tibial subluxation
- Additional intraarticular damage
- Active in sports.
Majority of patients fall between these two extremes, and treatment should always be indiviualized.
General principles of ACL reconstrution[edit | edit source]
- Restore stability
- Maintaence of full range of motion
- Isometric ligament function
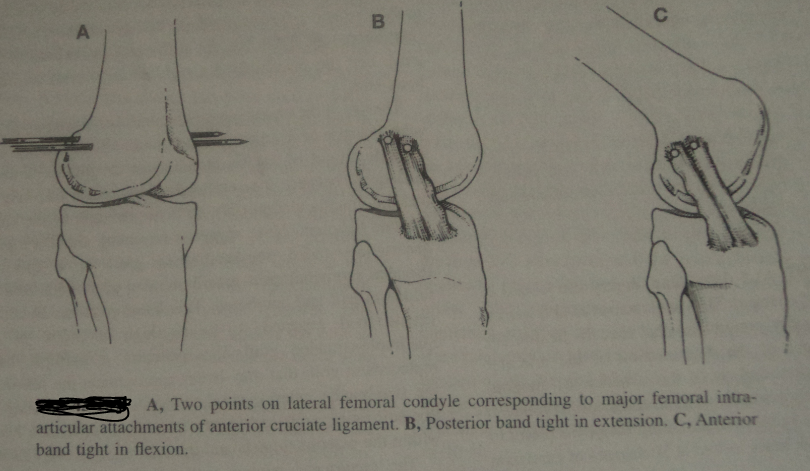
The gols of reconstructive surgery are to restore stability and still maintain the full ROM. For this goal it is essential that all ligaments and capsular restraits are isometric within a full ROM.[1] The isometric function of ACL is achieved by its configuration of fiber bundles and their attachments.[2]ACL is not a single cord and have bundle of indiviual fibers which assume spiral configuration and fan out over broad attachment areas. Due to its complex structure,liagment attachment sites should not be altered during reconstruction.[3].
Techniques for ACL reconstruction[edit | edit source]
There are basically two different techniques used for ACL reconstruction.
- Extraarticular
- Intraarticular
EXTRAARTICULAR PROCEDURE
In 1970s and 1980s the extraarticular procedures were performed commanly for anterior tibial sublaxation to eliminate mainly the pivot shift bye creating a static restraint to anterior tibial sublaxation which was usually accompained by connecting the lateral femoral epicondyle to Gerdy's tubercle with the collageous restraint lying parallel to the intraarticular course of ACL. This also avoid the problem of lack of blood supply to the intraarticular reconstructions. Most of these procedures use the iliotibial band or tract connecting the lateral femoral epicondyle to the gerdy tubercle,Krackow and Brooks. The optimal attachment point for the extraarticular reconstructions for anterolateral rotatory instability is found to be the Gerdy tubercle. This procedure is also used primarily in conjunction with an intraarticular reconstruction when severe anterior instability is due to injury or late stretching of the secondary stabilizing capsular structures or the lateral side of the knee.[4]
PROCEDURES
- Maclntosh method(iliotibial band tenodesis)
- Maclntosh, modified by Loseen method
- Andrews method
DISADVANTAGES
- Diminsh the anterolateral rotatory sublaxation but do not recreate the normal anatomy and function of the ACL.
- When used alone have high rate of failure.
INTRAARTICULAR PROCEDURE
The advances made in arthoscopy procedure lead to intraarticular reconstruction of ACL and better results in ACL injury rehabilitation. This procedure may involve a small arthrotomy incision also which preserve the vastus medialis obliquus muscle to the patella. This procedure can be performed with both endoscopic technique or double incision arthoscopic technique.
Various tissues/graft have been used to anatomically recontruct the tore ACL which include portions of the extensor mechanism[5][6], patellar tendon,iliotibial tract[7][8], semitendinousus tendon[9][10], gracilis tendon[11] and menisci[12]. These all are included in allografts i.e grafts taken from the person undergoing surgery. Other methods include the use of allografts and synthetic ligaments.[13][14]. This procedure have the following steps:
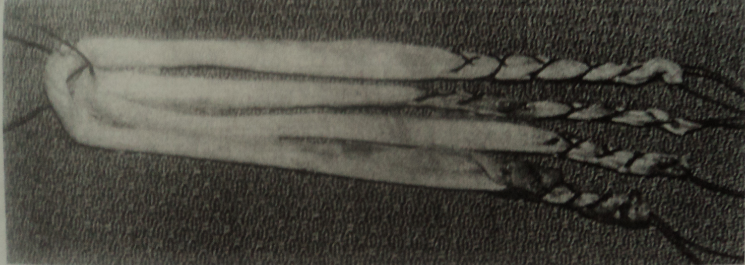
- Graft selection: Which graft can be use is decided while taking the decision of timing of surgery for ACL reconstrution. The most commanly used autograft is patellar bone graft and hamstring tendon graft (semitendinosus and gracilis).
- General considerations: In this the patient positioning before beginning the procedure is important.Knee flexion is more important with the endoscopic technique than the double incision arthoscopic technique. Routinely, 1g first generation of cephalosporin is administered before surgery.
- Diagnostic arthroscopy: It is preformed along with any necessary meniscal debridement or repair. Attention toward partial thickness tear, displaced bucket handle tears and the status of the articular surfaces, including the patellofemoral joint. Surgeon confirm that the cannula is placed intra articularly at the beginning fo the procedure,because the marked soft tissue fluid extravasation can quickly occur with the pump inflow system. Following diagnostic arthoscopy,graft procurement if done.
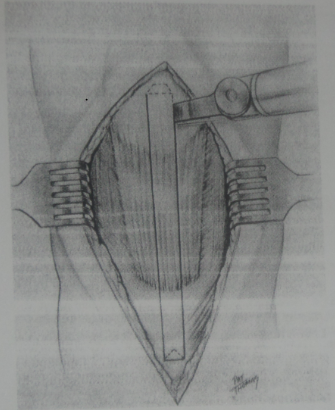
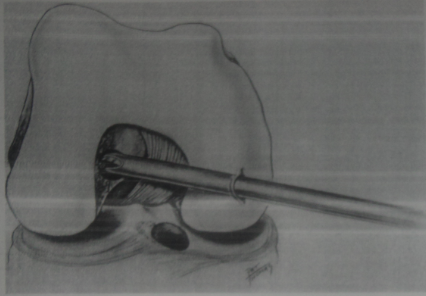
- Graft Harvest: Mini incision extending from distal pole of patella to 2.5cm below the tibial tubercle is made to procure the graft. After retracting the other strutures the graft to be taken is sharpely outlined and micro oscillating saw blade is used to harvest the graft/bone plug. Usually a triangle bone plug profile is obtained.
- Graft preparation: Graft is shaped in generally 10mm tube size for the femoral drill hole and 11mm tube for the tibial tunnel.
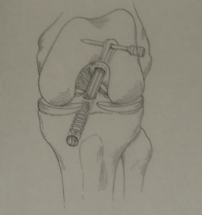
- Intercondylar notch preparation and notchplasty: Notchplasty is performed with 5.5mm burr from the anterior aspect of the intercondylar notch posteriorly and from distal to proximal. In this the residual tissue is also peeled off. Tissue is aggressively debrided with and arthroscopic shaver. If in the small intercondylar or notch area then further modifications are done.
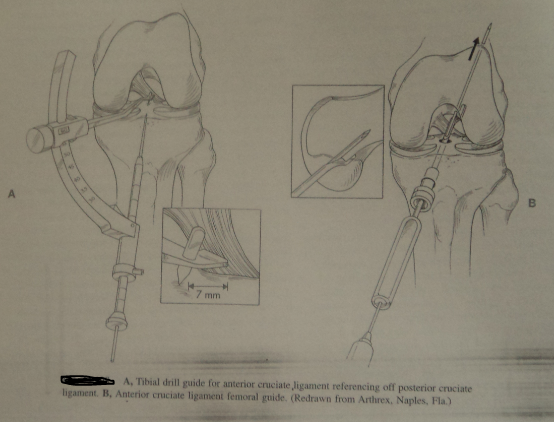
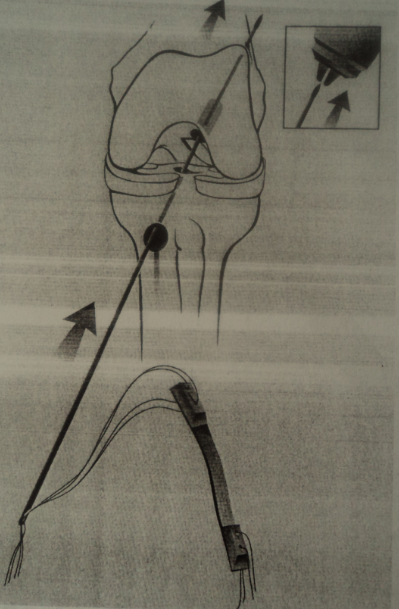
- Tibial tunnel placement: Tibial tunnel should be placed so that the graft is not impinged by the roof fo the intercondylar notch and should residue within the middle third of teh former ACL insertion site.
- Femoral Tunnel placement: after the tibial tunnel placement the femoral tunnel placement is done so as to make normal ACL like graft placement.
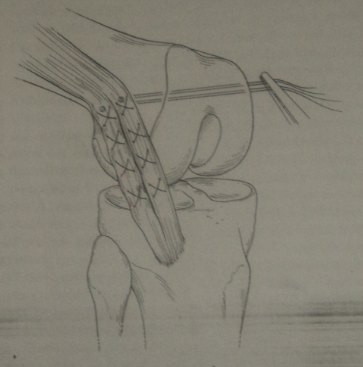
- Graft placement: The graft after the tunnel placement is slided along with arthroscopic grasper througth the tunnel.Graft may be rotated before tibial fixation.
- Graft fixatio: A Nitinol pin is then used to fix the graft with the bone and tunnel.Graft may be rotated before tibial fixationas normal ACL has been shown to have and external rotation within its fibers of app.90 degree. Also the amount of graft tension created during fixation have direct effect on ACL rehabilitation.
- Wound closure: Before closing, the graft harvest site is copiously injected with 0.25% Marcaine. the 0.25% Marcaine is also injected intra-articularly. The wound is closed with interruped abosorble sutures with the knee in flexion.
The reconstruction of the anterior cruciate ligament is one of the most common orthopedic surgery, at commonly there is a articular cartilage degeneration.
- A total collateral ligament rupture and a full-thickness cartilage lesion would be visualized by an MRI.
- There is a patella tendon procedure: involves the central third of the ipsilateral patellar tendon. There is a fixation of the bone blocks within the tibia and femur
- There is a hamstring-tendon procedure: four-layer, fold-up M. gracilis en M. semitendinosus tendons.
- This means that the take a part of the patella tendon or M. gracilis or M. semitendinosus for the reconstruction of the anterior cruciate ligament.
- The surgery takes places at 10 weeks after the injury.
The reconstruction of the Anterior Cruciate ligament is compared with other treatments. A central aspect of the treatment is a physical therapist. But it’s not always offered.
Double-bundle reconstruction:
The semitendinosus is used with the autograft trough 2 tunnels in both tibia and femur. The autograft method: bone-to-bone ( BTB) and hamstrings/ semitendinosus grafts. They also can use 3 tunnels: 2 tunnels through the tibia and 1 tunnel through the femur.
There are 2 important procedures for the reconstruction.
The first procedure is the autologous bone-patella tendon-bone graft and the autologous four-strand hamstrings graft. These are the 2 most popular procedures.
By the bone-patella tendon-bone graft, they take a couple of bone blocks from the patella and the tibial tubercle. This procedure causes more anterior knee pain than the semitendinosus graft. By the second procedure, they take the distal end of the semitendinosus and the gracilis tendon.
Other procedures are: the LARS artificial ligament,( Ligament Advanced Reinforcement System )iliotibial tract allografts, cadaveric allografts, synthetic materials and grafts from living related donor people. But all materials have their drawbacks: cross-infections, breakage, immunological responses, chronic effusions, recurrent instability[15]
Clinically Relevant Anatomy[edit | edit source]
The anatomy of the femoral and the tibial tunnel:
Femoral tunnel:
The tunnel at the sagittal side of the knee goes to the cortex of the femur and the roof of the intercondylar notch.
Tibial Tunnel:
First the tibial tunnel has to be created at the correct way, to prevent impingement of the grafts against the roof of the intercondylar notch. The tibial tunnel should be oriented at the Blumensaat line. This line goes from the tibial tuberosity and the posterior side should be oriented to the line of Blumensaat
Which Graft?
[edit | edit source]
Various tissues/graft have been used to anatomically recontruct the tore ACL.
These grafts are of 4 types
- Autografts which are taken from the patient's his/her own body and include portions of the extensor mechanism [16][17], patellar tendon,iliotibial tract [18][19], semitendinousus tendon[20][21], gracilis tendon [22] and menisci [23].
- Allografts: i.e grafts taken from cadavers.[24][25].
- Xenografts: grafts taken from animals. Bovine xenografts in particular have been associated with high complication rate [26].
- Synthetics: These can be further classified into 3 categories, biogradable (carbon fibers),permanent prostheses(Gore-Tex and Dacron) and ligament augmentation devices.
But the most comman used are the autografts (patellar bone & hamstring) and sometimes the allografts.There is no concensus in the literature as to which provides the most stability [27] Each of these choices has advantages and disadvantages.
Patellar Tendon[edit | edit source]
When a patellar tendon graft is taken, the central 1/3 of the patellar tendon is removed (about 9 or 10 mm) along with a block of bone at the sites of attachment on the kneecap and tibia.
Advantages:
- Closely resembles what needs reconstruction. The length of the patellar tendon is about the same as the ACL, and the bone ends of the graft can be placed in to the bone where the ACL attaches.
- Early bone to bone healing at 6 weeks. Bone to bone healing is considered to be stronger than soft tissue to bone healing as with a hamstring graft.
- Possibility of more aggressive rehabilitation and earleir return to sport.
Disadvantages:
- Harvest site morbidity of Patellar_Tendinitis and anterior knee pain.
- Patellofemoral joint tightness with late chondromalacia.
- Late patella fracture
- Late patellar tendon rupture
- Loss of range of motion
- Injury to the infra-patellar branch of the saphenous nerve.
Hamstring Tendon[edit | edit source]
With the improvement in the technique of the preparation of the multiple bundle graft, this graft choice has become more popular.
Advantages:
- 4 bundle graft is stronger and stiffer than the patellar tendon.
- No risk on anterior knee pain as with the patellar tendon.
- Smaller incision.
- Pain in the immediate post-operative period is less.
Disadvantages:
- Graft harvest can be difficult expecially in those with small muscles.
- Graft fixation to bone requires additional 'hardware' i.e. screws, endobutton.
- Graft healing of soft tissue to bone takes longer to heal, 10-12 weeks.
- Donor site morbidity. Patients may struggle to regain full strength of the hamstrings from which the donor was taken.[28]
Allograft (Donor Tissue)[edit | edit source]
Allograft is most commonly used in lower demand patients, or patients who are undergoing revision ACL surgery. Biomechanical studies show that allograft (donor tissue from a cadaver) is not as strong as a patient's own tissue (autograft). For many patients, however, the strength of the reconstructed ACL using an allograft is sufficient for their demands. Therefore this may be an excellent option for patients not planning to participate in high-demand sports (e.g. soccer, basketball, etc.).
Advantages:
Decreased operative time
- No need to remove other tissue to use for the graft
- Smaller incisions
- Less post-operative pain.
Disadvantages:
- Risk of disease transmission.
- Graft preparation to kill the living cells decreases the strength of the tissue.
- Longer graft to bone incorporation time.
- Not readily available
- Expensive
Autograft vs allograft reconstruction of the anterior cruciate ligament
Autograft: patellar tendon grafts and Achilles tendon grafts. Standard anterolateral and anteromedial portals were created. A 3-4 cm incision was made into the tibial tunnel over the proximal part of the tibia. Then the ACL beath pin was drilled into the cortex of the femur and proximally out of the skin. At last the ACL reamer is placed over the pin trough the tibial tunnel.
The allograft method: When they used this method, they’ve taken materials from cadavers. But this method isn’t that reliable as the autograft method. And it needs a longer time to revascularize.
Summary[edit | edit source]
Many surgeons have a preferred technique for different reasons. The strength of patellar tendon and hamstring grafts is essentially equal. There is no right answer as to which is best, at least not one that has been proven in orthopedic studies. The strength of allograft tissue is less than the other grafts, but the strength of both the patellar tendon and hamstring tendon grafts exceed the strength of a normal ACL.
Successful anterior cruciate ligament reconstruction is dependent on a number of factors including: patient selection, surgical technique, postoperative rehabilitation, and associated secondary restraint ligamentous instability. Errors in graft selection, tunnel placement, tensioning, or fixation methods chosen may also lead to graft failure. The comparison studies in the literature show that the outcome is almost the same irregardless of the graft choice. The most important aspect of the operation is to place the tunnels in the correct position. The choice of graft is really incidental.[29]
A Cochrane review in 2011[30] described the following:
- All tests for knee stability favoured patellar tendon grafts.
- Conversely, people had more anterior knee pain and discomfort with kneeling after patellar tendon reconstruction.
- After patellar tendon reconstruction, more people had some loss in their ability to straighten out their leg at the knee.
- In contrast, more people had some loss in their ability to bend their leg at the knee after hamstring tendon reconstruction.
A more recent study concluded that "ipsilateral autograft continues to show excellent results in terms of patient satisfaction, symptoms, function, activity level, and stability. The use of HT autograft does, however, show better outcomes than the PT autograft in all of these outcome measures. Additionally, at 15 years, the HT graft–reconstructed ACLs have shown a lower rate of radiological osteoarthritis"[31].
Outcome Measures[edit | edit source]
- International Knee Documentation Committee Subjective Knee Form (IKDC)
- Knee injury Osteoarthritis Outcome Score (KOOS)
- Tegner Lysholm Knee Scoring Scale
Examination and classification
[edit | edit source]
Grading and examining the anterior tibial sublaxation post ACL injury
|
SEVERITY |
AMOUNT OF ABNORMAL TIBIAL ROTATION |
POSITIVE TEST |
COMMENT |
| Mild (Grade 1) |
1+ (< 5 mm) |
Lashman and FRD |
May be present with generalized joint laxity (physiological) |
| Moderate (Grade II) |
2+ (5-10 mm) |
Lashman,FRD,Losee,ALRI,pivot 'slide" but not "jerk' |
no obvious jump with jerk and PS |
| Severe (Grade III) |
3+ (11-15 mm) |
Lachman,FRD, Losee,ALRI,jerk and PS |
Obvious jump with jerk and PS and gross subluxation-reduction with test |
| Gross (Grade IV) |
4+ (> 15mm) |
Lachman,FRD,Losee,ALRI,jerk and PS |
Impingment of lateral tibial plateau in sublaxation position, which requires examiner to backoff during pivot shift test to effect reduction |
(FRD- flexion rotation drawer, ALRI- anterolateral rotatory instability, PS- pivot shift)
KINEMATICS[32]
The kinematics of the single- bundle ACL reconstruction: the kinematics showed that the standard single-bundle ACL reconstruction doesn’t create the same kinematics as the intact ACL in normal activities. Only the anteroposterior stability seems to be reconstructed . When the knee turns, there is an abnormal tibial rotation in the knee. So the single-bundle ACl reconstruction does not recreate a normal rotation in the knee.
The kinematics of the double-bundle ACL recontstruction: the kinematics of the double-bundle ACL reconstruction are better than the kinematics of the single-bundle ACL reconstruction. The anterior translation is comparable with the intact ACL at 0° flexion. But the most stable position of the knee is 15° and 75°.
Physiotherapy Management[edit | edit source]
Pre Op[edit | edit source]
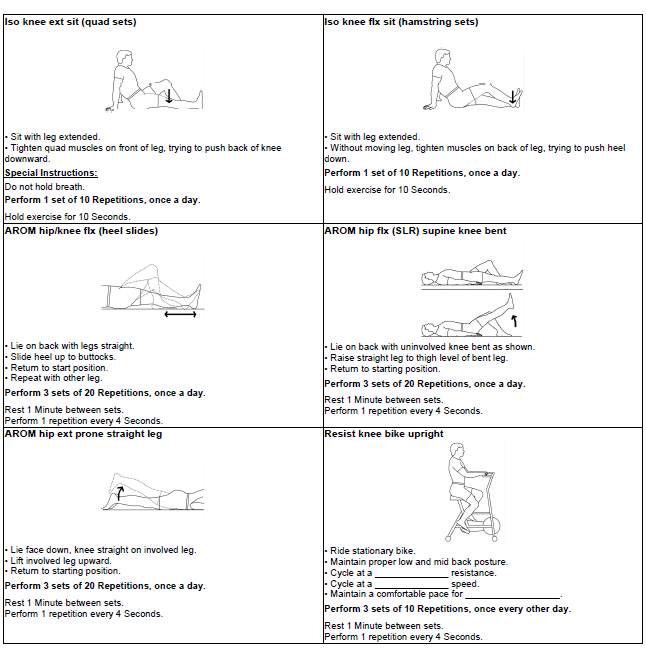
Following are the exercises which should be performed before ACL reconstrution surgery. Major concern are the strengthening exercises.
Post Op[edit | edit source]
Postoperative treatment and rehabilitation:[33]
Anti-inflammatory medication, a treatment for the sw elling for 5 days after the surgery. After 3 days the patient can do
straight leg raising exercises for about 200 times a day. This is necessary for strengthen the Quadriceps and to prevent
other muscles to shorten.
- After 2 – 3 w eeks: active flexion and extension and plantair flexion
- After 4 w eeks: exercises for proprioception
- After 2 -3 months: exercises for proprioception and anti-resistance training.
To be done:
- Toes, ankles, quads.
- Passive terminal extension (heel on towel).
- Knee flexion.
- Patella mobilisation.
- Mobilised partial weight bearing with a canvas splint and elbow crutches –
- patient may be non-weight bearing if they have had:
- Microfracture.
- PCL repair.
- Collateral repair.
- High tibial osteotomy.
Detailed ACL surgery rehabilitation can be read from this page
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
1) R. B. FROBELL, Ph. D. E.V. ROOS, … “A randomized trial of treatment for acute anterior cruciate ligament tears” , The new England journal of medicine, july 2010 http://www.nejm.org/doi/full/10.1056/NEJMoa0907797#t=article
2) D.L SHI, “Effect of anterior cruciate ligament reconstruction on biomechanical features of knee in level walking: a meta-analysis” , Chinese medical journal,2010
http://www.cmj.org/Periodical/paperlist.asp?id=LW2010113338438408321&linkintype=pubmed
3) A.B. MEYERS, A.H. HAIMS, ‘Imaging of anterior cruciate ligament repair and its complications’, American Journal of roentgen logy. Febuary 2010 http://www.ajronline.org/cgi/reprint/194/2/476
4) C. LEGNANI, A. VENTURA, ‘Anterior cruciate ligament reconstruction with synthetic grats. A review of literature’, January 2010, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2903133/?tool=pubmed
5) J.M. HUAN, ‘Cruciate ligament reconstruction using LARS artificial ligament under arthroscopy: 81 cases report’, Chinese medical journal, 2010 http://www.cmj.org/Periodical/paperlist.asp?id=LW2010120595905909751&linkintype=pubmed
6) E. TSUDA , I. YASUYUKI, “Comparable results between lateralized single- and double- bundle ACL reconstructions”, Hirosaki university graduate school of medicine, october 2008http://www.cmj.org/Periodical/paperlist.asp?id=LW2010120595905909751&linkintype=pubmed
7) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2650066/?tool=pubmed level of evidence is II, therapeutic study
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1-IhdOtu689PDq3353ICKCZ__AtralGYs_ebbGDbvcGOJ0fQmO|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ Warren RF,Marshell JL,Girgis F: The prime static stabilizer of the medial side of the knee,J Bone Joint Surg 56A:665,1974.
- ↑ Arms S et al:Strain measurement in the medial collateral ligament of the human knee: an autopsy study,J Biomech 16:491,1983.
- ↑ Warren RF,Marshell JL,Girgis F: The prime static stabilizer of the medial side of the knee,J Bone Joint Surg 56A:665,1974
- ↑ Campbell's operative orthopaedics; vol.3: tenth edition. Mosby publication.
- ↑ Clacy WG:Anterior cruciate ligament functional instability:a static intraarticular and dynamic extra articular procedure, Clin Orthop 172: 102,1983.
- ↑ Clancy WG et al: Anterior cruciate ligament reconstruction using one third of the patellar ligament, augmented by extraarticualar tendon transfers,J Bone Joint Surg 64A:352,1982.
- ↑ Galway HR,Maclntosh DL:The lateral pivot shift:a symptom and sign of anterior cruciate ligament insufficiency,Clinc Orthop 147:45,1980.
- ↑ Hey-Groves EW: The crucial ligaments of the knee joint:their function,rupture and the operative treatment of the same,Br J Surg 7:505,1920.
- ↑ Cho KO:Reconstruction of the anterior cruciate ligament bye semitendinousus tenodesis,J Bone Joint Surg 57A:608,1975.
- ↑ Horne JG,Parsons CJ:The anterior cruciate ligament:its anatomy and a new method of reconstruction,Can J Surg 20:214,1977.
- ↑ McMaster JH,Weinert CR,Scranton P:Diagnosis and managment of isolated anterior cruciate ligament tears:a preliminary report on reconstruction with the gracillis tendon,J Trauma 14:230,1974.
- ↑ Collins HR et al:The meniscus as a cruciate ligament substitude,J Sports Med 2:11,1974.
- ↑ Chick RR,Jackson DW:Tears of the anterior cruciate ligament in young athletes,J Bone Joint Surg 60A:970,1978.
- ↑ Indeicato PA.Linton RC,Huegel M: The results of fresh frozen patella tendon allografts for chronic anterior cruciate ligament deficiency of the knee,Am J Sports Med 20:118,1992.
- ↑ R. B. FROBELL, Ph. D. E.V. ROOS, … “A randomized trial of treatment for acute anterior cruciate ligament tears” , The new England journal of medicine, july 2010
- ↑ Clacy WG:Anterior cruciate ligament functional instability:a static intraarticular and dynamic extra articular procedure, Clin Orthop 172: 102,1983.
- ↑ Clancy WG et al: Anterior cruciate ligament reconstruction using one third of the patellar ligament, augmented by extraarticualar tendon transfers,J Bone Joint Surg 64A:352,1982.
- ↑ Galway HR,Maclntosh DL:The lateral pivot shift:a symptom and sign of anterior cruciate ligament insufficiency,Clinc Orthop 147:45,1980.
- ↑ Hey-Groves EW: The crucial ligaments of the knee joint:their function,rupture and the operative treatment of the same,Br J Surg 7:505,1920.
- ↑ Cho KO:Reconstruction of the anterior cruciate ligament bye semitendinousus tenodesis,J Bone Joint Surg 57A:608,1975.
- ↑ Horne JG,Parsons CJ:The anterior cruciate ligament:its anatomy and a new method of reconstruction,Can J Surg 20:214,1977.
- ↑ Horne JG,Parsons CJ:The anterior cruciate ligament:its anatomy and a new method of reconstruction,Can J Surg 20:214,1977.
- ↑ Collins HR et al:The meniscus as a cruciate ligament substitude,J Sports Med 2:11,1974.
- ↑ Chick RR,Jackson DW:Tears of the anterior cruciate ligament in young athletes,J Bone Joint Surg 60A:970,1978.
- ↑ Indeicato PA.Linton RC,Huegel M: The results of fresh frozen patella tendon allografts for chronic anterior cruciate ligament deficiency of the knee,Am J Sports Med 20:118,1992.
- ↑ Van Steenel CJ et al:Failure of anterior cruciate ligament reconstruction using tendon xenografts,J Bone Joint Surg 69A:860,1987.
- ↑ Nicholas GH Mohtadi, Denise S Chan1, Katie N Dainty, Daniel B Whelan. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Bone, Joint and Muscle Trauma Group, The Cochrane Library, Sept 2011
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedHeijine - ↑ Johnson. Graft Choice for ACL Reconstruction. International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine.
- ↑ Mohtadi NGH, Chan DS, Dainty KN, Whelan DB. Patellar or hamstring tendon grafts for ACL reconstruction in adults. Cochrane Summaries.
- ↑ Toby Leys, Lucy Salmon, Alison Waller, James Linklater and Leo Pinczewski. Clinical Results and Risk Factors for Reinjury 15 Years After Anterior Cruciate Ligament Reconstruction: A Prospective Study of Hamstring and Patellar Tendon Grafts. Am J Sports Med December 19, 2011
- ↑ A.B. MEYERS, A.H. HAIMS, ‘Imaging of anterior cruciate ligament repair and its complications’, American Journal of roentgen logy. Febuary 2010
- ↑ D.L SHI, “Effect of anterior cruciate ligament reconstruction on biomechanical features of knee in level walking: a meta-analysis” , Chinese medical journal,2010