Atherosclerosis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 19: | Line 19: | ||
Atherosclerotic cardiovascular disease mainly involves the heart and brain: [[Coronary Artery Disease (CAD)|coronary arterial disease]] and ischemic [[stroke]]. CAD and stroke are the world's first and fifth causes of death respectively.<ref name=":1" /> | Atherosclerotic cardiovascular disease mainly involves the heart and brain: [[Coronary Artery Disease (CAD)|coronary arterial disease]] and ischemic [[stroke]]. CAD and stroke are the world's first and fifth causes of death respectively.<ref name=":1" /> | ||
<div class="row"> | |||
<div class="col-md-6"> {{#ev:youtube|VmWj-Rl4-7w |400}} <div class="text-right"><ref>Dr. Matt and Dr. Mike. Atherosclerosis in 2 minutes. Available from: https://www.youtube.com/watch?v=VmWj-Rl4-7w [last accessed 29/6/2022]</ref></div></div> | |||
<div class="col-md-6"> {{#ev:youtube|jwL4lkSlvSA|400}} <div class="text-right"><ref>Dr. Matt and Dr. Mike. Atherosclerosis - Pathogenesis, risk factors and complications. Available from: https://www.youtube.com/watch?v=jwL4lkSlvSA [last accessed 29/6/2022]</ref></div></div> | |||
</div> | |||
== Pathophysiology == | == Pathophysiology == | ||
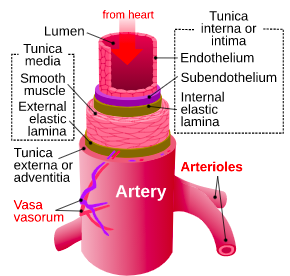
[[File:Artery layers.png|right|frameless|290x290px]] | [[File:Artery layers.png|right|frameless|290x290px]] | ||
Atherosclerosis mainly develops through the continuous process of arterial wall lesions due to lipid retention by trapping in the intima by a matrix (eg proteoglycans) resulting in a modification which then aggravates [[Inflammation Acute and Chronic|chronic inflammation]] | Atherosclerosis mainly develops through the continuous process of arterial wall lesions due to lipid retention by trapping in the intima by a matrix (eg proteoglycans) resulting in a modification which then aggravates [[Inflammation Acute and Chronic|chronic inflammation]] vulnerable sites in the arteries. This plays an important role in all phases of atherogenic progression (see stages below). | ||
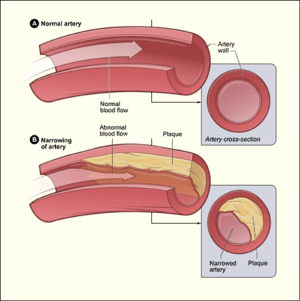
The systemic changes detected in atherosclerosis are closely similar in the [[aorta]] and the [[Coronary Artery|coronary]] and the [[Common Carotid Artery|carotid]] arteries. The continuous process of atherosclerosis is typically comprehended as an extended sequence of histologic developments or a series of different classes of lesions that may be visible to the unaided eye.<ref name=":1" />[[File:Atherosclerosis diagram.png|right|frameless]]The Three Stages of Atherosclerosis | The systemic changes detected in atherosclerosis are closely similar in the [[aorta]] and the [[Coronary Artery|coronary]] and the [[Common Carotid Artery|carotid]] arteries. The continuous process of atherosclerosis is typically comprehended as an extended sequence of histologic developments or a series of different classes of lesions that may be visible to the unaided eye.<ref name=":1" />[[File:Atherosclerosis diagram.png|right|frameless]]The Three Stages of Atherosclerosis | ||
# The fatty streak: This first stage of atherosclerosis can sometimes be found in children as young as 10 years of age. In this stage, a yellow streak appears along major arteries, such as the aorta and carotid artery. This streak is made up of smooth [[muscle]] cells, cholesterol, and macrophages (a type of [[Leukocytes|white blood cell]]). The fatty streak phase alone does not cause any noticeable symptoms but can progress into a more dangerous phase of atherosclerosis called a fibrous plaque. | # The fatty streak: This first stage of atherosclerosis can sometimes be found in children as young as 10 years of age. In this stage, a yellow streak appears along major arteries, such as the aorta and carotid artery. This streak is made up of smooth [[muscle]] cells, cholesterol, and macrophages (a type of [[Leukocytes|white blood cell]]). The fatty streak phase alone does not cause any noticeable symptoms but can progress into a more dangerous phase of atherosclerosis called a fibrous plaque. | ||
# Fibrous plaque: A fibrous plaque develops within the inner layer of the vessel. This plaque is made up of smooth muscle cells, macrophages, and [[lymphocytes]] (a more aggressive type of white blood cell). These cells have cholesterol inside of them. As the fibrous plaque grows, it begins to protrude into the vessel where the blood is flowing. | # Fibrous plaque: A fibrous plaque develops within the inner layer of the vessel. This plaque is made up of smooth muscle cells, macrophages, and [[lymphocytes]] (a more aggressive type of white blood cell). These cells have cholesterol inside of them. As the fibrous plaque grows, it begins to protrude into the vessel where the blood is flowing. | ||
# Complicated lesion: The final stage of atherosclerosis is defined when a dangerous series of events occur. When the fibrous plaque breaks apart, it exposes the cholesterol and [[Connective Tissue Disorders|connective]] tissue underneath it. This event is recognized by the body as an injury, and a team of [[blood]] clotting cells | # Complicated lesion: The final stage of atherosclerosis is defined when a dangerous series of events occur. When the fibrous plaque breaks apart, it exposes the cholesterol and [[Connective Tissue Disorders|connective]] tissue underneath it. This event is recognized by the body as an injury, and a team of [[blood]] clotting cells is sent to the scene. This becomes particularly dangerous because now the blood flow is being restricted by the initial blockage as well as the clot that has formed. The ruptured plaque in combination with the blood clot is called a complicated lesion<ref>Study.com Atherosclerosis: Stages & Prognosis Available from:https://study.com/academy/lesson/atherosclerosis-stages-prognosis.html (accessed 12.2.2021)</ref>. | ||
== Treatment == | == Treatment == | ||
The best management of ASCVD is to treat the risk factors such as elevated LDL-C, blood pressure (BP), diabetes, among others. Also, all patients should be encouraged to exercise for 90 to 150 minutes and eat a healthy diet low in saturated (red and processed meat, organ meats, and the like) | The best management of ASCVD is to treat the risk factors such as elevated LDL-C, blood pressure (BP), and diabetes, among others. Also, all patients should be encouraged to exercise for 90 to 150 minutes and eat a healthy diet low in saturated (red and processed meat, organ meats, and the like), trans fats (baked goods), and salt intake of less than 5 grams per day with enrichment in fiber, monounsaturated fats, fatty fish, fruits, and vegetables. Smokers should be encouraged to stop and be referred to a smoking cessation program.<ref name=":1" /> | ||
== Physiotherapy == | == Physiotherapy == | ||
[[File:Exercise photo.jpg|right|frameless]] | [[File:Exercise photo.jpg|right|frameless]] | ||
We can help our clients manage their condition through education regarding heart-healthy eating, aiming for a healthy weight, managing stress, physical activity and quitting smoking. | We can help our clients manage their condition through education regarding heart-healthy eating, aiming for a healthy weight, managing stress, physical activity, and quitting smoking. | ||
Patient education plays a significant role in maintaining a healthy lifestyle. American Heart Association has Provided a [https://www.heart.org/-/media/Files/Health-Topics/Cholesterol/My-Cholesterol-Guide-English.pdf 'My Cholesterol Guide: Taken Action. Live Healthy!'] Understanding the cholesterol in depth will help the patient to reduce the risk factors and live a healthy | Patient education plays a significant role in maintaining a healthy lifestyle. American Heart Association has Provided a [https://www.heart.org/-/media/Files/Health-Topics/Cholesterol/My-Cholesterol-Guide-English.pdf 'My Cholesterol Guide: Taken Action. Live Healthy!'] Understanding the cholesterol in depth will help the patient to reduce the risk factors and live a healthy lifestyle. This can include the role of cholesterol medication, what to eat and what to not, and how to improve and maintain levels of cholesterol. | ||
We are instrumental in providing exercise | We are instrumental in providing exercise prescriptions and monitoring. See the below links as examples | ||
* [[Cardiac Rehabilitation|Cardiac rehabilitation]] | * [[Cardiac Rehabilitation|Cardiac rehabilitation]] | ||
* [[Physical Activity and Exercise Prescription|Physical Activity and Exercise Presciption]] | * [[Physical Activity and Exercise Prescription|Physical Activity and Exercise Presciption]] | ||
| Line 46: | Line 49: | ||
== Lifestyle Factors: Future Directions == | == Lifestyle Factors: Future Directions == | ||
[[File:Healthy food.jpg|right|frameless]] | [[File:Healthy food.jpg|right|frameless]] | ||
Despite major efforts to reduce atherosclerotic cardiovascular disease (ASCVD) burden with conventional risk factor control, significant residual risk remains. Recent evidence on non-traditional determinants of cardiometabolic health has advanced our understanding of lifestyle–disease interactions. Of particular relevance is the potential of low-risk lifestyle factors to impact | Despite major efforts to reduce the atherosclerotic cardiovascular disease (ASCVD) burden with conventional risk factor control, significant residual risk remains. Recent evidence on non-traditional determinants of cardiometabolic health has advanced our understanding of lifestyle–disease interactions. Of particular relevance is the potential of low-risk lifestyle factors to impact plaque vulnerability (through altered adipose tissue and skeletal muscle phenotype and secretome) and collectively cause a set of phenotypic adaptations resulting in an anti-atherosclerotic milieu.<ref name=":0" /> | ||
Lifestyle factors include ( | Lifestyle factors include (not limited to) the following: | ||
* Chronic exposure to environmental stressors eg. poor diet quality, [[Physical Inactivity|sedentarism]], ambient air pollution and noise, [[Sleep Deprivation and Sleep Disorders|sleep deprivation]] and psychosocial [[Stress and Health|stress]]. | * Chronic exposure to environmental stressors eg. poor diet quality, [[Physical Inactivity|sedentarism]], ambient air pollution and noise, [[Sleep Deprivation and Sleep Disorders|sleep deprivation]] and psychosocial [[Stress and Health|stress]]. | ||
* [[Body Composition|Body composition]] versus body weight. The effects of diet on health seem to be more closely related to body composition than to body weight and total fat mass per se, suggesting that body mass index ([[Obesity|BMI]]) can be an inadequate measure for assessing the effects of diet on health | * [[Body Composition|Body composition]] versus body weight. The effects of diet on health seem to be more closely related to body composition than to body weight and total fat mass per se, suggesting that body mass index ([[Obesity|BMI]]) can be an inadequate measure for assessing the effects of diet on health | ||
| Line 59: | Line 62: | ||
== Complications == | == Complications == | ||
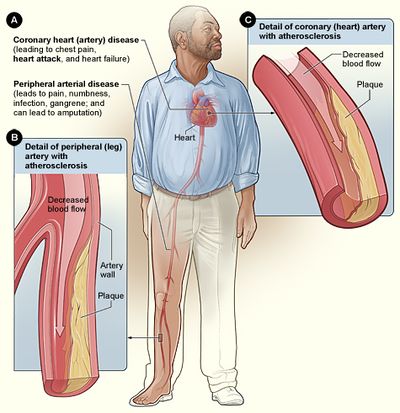
ASCVD can present as coronary artery disease (CAD), cerebrovascular disease (CVA), transient ischemic attack (TIA), peripheral artery disease (PAD), | ASCVD can present as coronary artery disease (CAD), cerebrovascular disease (CVA), transient ischemic attack (TIA), peripheral artery disease (PAD), abdominal aneurysms, and renal artery stenosis in males<ref name=":1" />. | ||
== References == | == References == | ||
Revision as of 12:02, 28 June 2022
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Kim Jackson, Shreya Trivedi and Uchechukwu Chukwuemeka
Introduction[edit | edit source]
Atherosclerosis is caused by plaque (fatty deposits) build up in the arteries. These deposits are made up of cholesterol, fatty substances, cellular waste products, calcium and fibrin.
- It is a chronic inflammatory disease of the arteries and is the underlying cause of about 50% of all deaths in westernized society.
- Despite major efforts to reduce atherosclerotic cardiovascular disease (ASCVD) burden with conventional risk factor control, significant residual risk remains. Recent evidence on non-traditional determinants of cardiometabolic health has advanced our understanding of lifestyle-disease interactions.[1]
Etiology[edit | edit source]
ASCVD is of multifactorial etiology. The most common risk factors include:
Hypercholesterolemia (LDL-cholesterol); Hypertension; Diabetes Mellitus; Cigarette smoking; Age (male older than 45 years and female older than 55 years); Male gender; and strong family history (male relative younger than 55 years and female relative younger than 65 years); Sedentary lifestyle; Obesity; Diets high in saturated and trans-fatty acids; and certain Genetic mutations.[2]
Epidemiology[edit | edit source]
Since atherosclerosis is a predominantly asymptomatic condition, it is difficult to determine the incidence accurately. Atherosclerosis is considered the major cause of cardiovascular diseases.
Atherosclerotic cardiovascular disease mainly involves the heart and brain: coronary arterial disease and ischemic stroke. CAD and stroke are the world's first and fifth causes of death respectively.[2]
Pathophysiology[edit | edit source]
Atherosclerosis mainly develops through the continuous process of arterial wall lesions due to lipid retention by trapping in the intima by a matrix (eg proteoglycans) resulting in a modification which then aggravates chronic inflammation vulnerable sites in the arteries. This plays an important role in all phases of atherogenic progression (see stages below).
The systemic changes detected in atherosclerosis are closely similar in the aorta and the coronary and the carotid arteries. The continuous process of atherosclerosis is typically comprehended as an extended sequence of histologic developments or a series of different classes of lesions that may be visible to the unaided eye.[2]
The Three Stages of Atherosclerosis
- The fatty streak: This first stage of atherosclerosis can sometimes be found in children as young as 10 years of age. In this stage, a yellow streak appears along major arteries, such as the aorta and carotid artery. This streak is made up of smooth muscle cells, cholesterol, and macrophages (a type of white blood cell). The fatty streak phase alone does not cause any noticeable symptoms but can progress into a more dangerous phase of atherosclerosis called a fibrous plaque.
- Fibrous plaque: A fibrous plaque develops within the inner layer of the vessel. This plaque is made up of smooth muscle cells, macrophages, and lymphocytes (a more aggressive type of white blood cell). These cells have cholesterol inside of them. As the fibrous plaque grows, it begins to protrude into the vessel where the blood is flowing.
- Complicated lesion: The final stage of atherosclerosis is defined when a dangerous series of events occur. When the fibrous plaque breaks apart, it exposes the cholesterol and connective tissue underneath it. This event is recognized by the body as an injury, and a team of blood clotting cells is sent to the scene. This becomes particularly dangerous because now the blood flow is being restricted by the initial blockage as well as the clot that has formed. The ruptured plaque in combination with the blood clot is called a complicated lesion[5].
Treatment[edit | edit source]
The best management of ASCVD is to treat the risk factors such as elevated LDL-C, blood pressure (BP), and diabetes, among others. Also, all patients should be encouraged to exercise for 90 to 150 minutes and eat a healthy diet low in saturated (red and processed meat, organ meats, and the like), trans fats (baked goods), and salt intake of less than 5 grams per day with enrichment in fiber, monounsaturated fats, fatty fish, fruits, and vegetables. Smokers should be encouraged to stop and be referred to a smoking cessation program.[2]
Physiotherapy[edit | edit source]
We can help our clients manage their condition through education regarding heart-healthy eating, aiming for a healthy weight, managing stress, physical activity, and quitting smoking. Patient education plays a significant role in maintaining a healthy lifestyle. American Heart Association has Provided a 'My Cholesterol Guide: Taken Action. Live Healthy!' Understanding the cholesterol in depth will help the patient to reduce the risk factors and live a healthy lifestyle. This can include the role of cholesterol medication, what to eat and what to not, and how to improve and maintain levels of cholesterol.
We are instrumental in providing exercise prescriptions and monitoring. See the below links as examples
- Cardiac rehabilitation
- Physical Activity and Exercise Presciption
- Physical Activity
- Home Exercise Plan
- Aerobic Activity
Lifestyle Factors: Future Directions[edit | edit source]
Despite major efforts to reduce the atherosclerotic cardiovascular disease (ASCVD) burden with conventional risk factor control, significant residual risk remains. Recent evidence on non-traditional determinants of cardiometabolic health has advanced our understanding of lifestyle–disease interactions. Of particular relevance is the potential of low-risk lifestyle factors to impact plaque vulnerability (through altered adipose tissue and skeletal muscle phenotype and secretome) and collectively cause a set of phenotypic adaptations resulting in an anti-atherosclerotic milieu.[1]
Lifestyle factors include (not limited to) the following:
- Chronic exposure to environmental stressors eg. poor diet quality, sedentarism, ambient air pollution and noise, sleep deprivation and psychosocial stress.
- Body composition versus body weight. The effects of diet on health seem to be more closely related to body composition than to body weight and total fat mass per se, suggesting that body mass index (BMI) can be an inadequate measure for assessing the effects of diet on health
- Cardiorespiratory fitness: Physical inactivity and low cardiorespiratory fitness (CRF) are under-recognized cardiometabolic risk factors and are strong independent predictors of outcomes in primary and secondary prevention of ASCVD across different BMI groups. Encouragingly, high levels of physical activity and CRF largely neutralize the adverse effects of adiposity and other traditional cardiovascular disease risk factors, including the metabolic syndrome
- Physical Activity: Particularly resistance training, affects body composition in a way that promotes an overall anti-inflammatory and anti-atherogenic milieu Of particular current interest is skeletal muscle maintenance as a way of attenuating immunosenescence and inflammation, a hallmark of chronic, age-related diseases
- Diet: Collectively, for maintaining cardiovascular and overall health, strong evidence and broad consensus speak to minimizing consumption of added sugars and refined grains and avoiding industrial trans-fatty acids, while replacing them with plant- and animal-based whole foods
- Muscle strength and functionality
- Intestinal microbiome: In recent years, microbiome–health interactions have been found to play a fundamental role in cardiovascular health. One major link between the intestinal microbiome and high-risk atherosclerosis is gut dysbiosis-related inflammation. Gut dysbiosis has been linked to increased mucosal barrier permeability, which allows the penetration of bacteria and their products into the circulatory system. This elicits a systemic, chronic, pro-inflammatory condition and provides a mechanistic basis for the observed association of ASCVD and a wide array of non-communicable diseases with gut dysbiosis.
All the above are increasingly recognized as major determinants of cardiovascular health.[1]
Complications[edit | edit source]
ASCVD can present as coronary artery disease (CAD), cerebrovascular disease (CVA), transient ischemic attack (TIA), peripheral artery disease (PAD), abdominal aneurysms, and renal artery stenosis in males[2].
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Lechner K, von Schacky C, McKenzie AL, Worm N, Nixdorff U, Lechner B, Kränkel N, Halle M, Krauss RM, Scherr J. Lifestyle factors and high-risk atherosclerosis: Pathways and mechanisms beyond traditional risk factors. European journal of preventive cardiology. 2020 Mar 1;27(4):394-406.Available from:https://pubmed.ncbi.nlm.nih.gov/31408370/ (accessed 11.2.2021)
- ↑ 2.0 2.1 2.2 2.3 2.4 Pahwa R, Jialal I. Atherosclerosis. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507799/ (accessed 12.2.2021)
- ↑ Dr. Matt and Dr. Mike. Atherosclerosis in 2 minutes. Available from: https://www.youtube.com/watch?v=VmWj-Rl4-7w [last accessed 29/6/2022]
- ↑ Dr. Matt and Dr. Mike. Atherosclerosis - Pathogenesis, risk factors and complications. Available from: https://www.youtube.com/watch?v=jwL4lkSlvSA [last accessed 29/6/2022]
- ↑ Study.com Atherosclerosis: Stages & Prognosis Available from:https://study.com/academy/lesson/atherosclerosis-stages-prognosis.html (accessed 12.2.2021)