Bone: Difference between revisions
(added original editor) |
(Undo revision 230372 by Lucinda hampton (talk)) |
||
| Line 1: | Line 1: | ||
#<div class="editorbox"> | #<div class="editorbox"> | ||
'''Original Editors ''' - | '''Original Editors ''' - | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | |||
== Introduction == | == Introduction == | ||
| Line 10: | Line 9: | ||
* Bone is a metabolically active connective tissue that provides structural support, facilitates movement, and protects vital organs. | * Bone is a metabolically active connective tissue that provides structural support, facilitates movement, and protects vital organs. | ||
* It plays an important role in regulating mineral and acid-base balance homeostasis. It also provides the environment for hematopoiesis (blood cells production) within the bone marrow. | * It plays an important role in regulating mineral and acid-base balance homeostasis. It also provides the environment for hematopoiesis (blood cells production) within the bone marrow. | ||
* Bone is composed of an extracellular matrix and bone cells (osteocytes)<ref | * Bone is composed of an extracellular matrix and bone cells (osteocytes)<ref>El Sayed SA, Nezwek TA, Varacallo M. [https://www.ncbi.nlm.nih.gov/books/NBK441968/ Physiology, Bone.] InStatPearls [Internet] 2019 Jul 29. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK441968/ (last accessed 10.2.2020) | ||
</ref>. Under the right conditions, bone tissue undergoes a process of mineralization, formed by collagen matrix and hardened by deposited calcium. Bone tissue (osseous tissue) differs greatly from other tissues in the body. Bone is hard and many of its functions depend on that characteristic hardness.<ref name=":0">Opentextbc.ca. (2018). ''6.3 Bone Structure – Anatomy and Physiology''. [online] Available at: <nowiki>https://opentextbc.ca/anatomyandphysiology/chapter/6-3-bone-structure/</nowiki> </ref>The skeleton is composed of around 80% cortical bone and 20% trabecular bone.<ref name=":1">Singh S, Bray TJ, Hall-Craggs MA. Quantifying bone structure, micro-architecture, and pathophysiology with MRI. Clinical radiology. 2018 Mar 1;73(3):221-30.</ref> | </ref>. Under the right conditions, bone tissue undergoes a process of mineralization, formed by collagen matrix and hardened by deposited calcium. Bone tissue (osseous tissue) differs greatly from other tissues in the body. Bone is hard and many of its functions depend on that characteristic hardness.<ref name=":0">Opentextbc.ca. (2018). ''6.3 Bone Structure – Anatomy and Physiology''. [online] Available at: <nowiki>https://opentextbc.ca/anatomyandphysiology/chapter/6-3-bone-structure/</nowiki> </ref>The skeleton is composed of around 80% cortical bone and 20% trabecular bone.<ref name=":1">Singh S, Bray TJ, Hall-Craggs MA. Quantifying bone structure, micro-architecture, and pathophysiology with MRI. Clinical radiology. 2018 Mar 1;73(3):221-30.</ref> | ||
* Much of the cellular activity in a bone consists of removal and replacement at the same site, a process called remodelling. The remodelling process occurs throughout life and becomes dominant by the time that bone reaches its peak mass (typically by the early 20s). Remodelling continues throughout life so that most of the adult skeleton is replaced about every 10 years.<ref>Office of the Surgeon General (US. [https://www.ncbi.nlm.nih.gov/books/NBK45504/ The Basics of Bone in Health and Disease.] InBone Health and Osteoporosis: A Report of the Surgeon General 2004. Office of the Surgeon General (US). Available from:https://www.ncbi.nlm.nih.gov/books/NBK45504/ (last accessed 10.2.2020)</ref> | * Much of the cellular activity in a bone consists of removal and replacement at the same site, a process called remodelling. The remodelling process occurs throughout life and becomes dominant by the time that bone reaches its peak mass (typically by the early 20s). Remodelling continues throughout life so that most of the adult skeleton is replaced about every 10 years.<ref>Office of the Surgeon General (US. [https://www.ncbi.nlm.nih.gov/books/NBK45504/ The Basics of Bone in Health and Disease.] InBone Health and Osteoporosis: A Report of the Surgeon General 2004. Office of the Surgeon General (US). Available from:https://www.ncbi.nlm.nih.gov/books/NBK45504/ (last accessed 10.2.2020)</ref> | ||
| Line 41: | Line 40: | ||
Type 1 collagen is a non-calcified matrix (osteoid) designed to resist the tension experienced by the weight-bearing functions of bone. It forms from osteoblasts, the main cellular component of bone. | Type 1 collagen is a non-calcified matrix (osteoid) designed to resist the tension experienced by the weight-bearing functions of bone. It forms from osteoblasts, the main cellular component of bone. | ||
'''Osteoblasts''' produce matrix, build up bone tissue. They function in the production, transport, and arrangement of the osteoid matrix. Furthermore, they initiate and regulate matrix mineralization and control the neighboring bone cells activities. | '''Osteoblasts''' produce matrix, build up bone tissue. They function in the production, transport, and arrangement of the osteoid matrix. Furthermore, they initiate and regulate matrix mineralization and control the neighboring bone cells activities. | ||
| Line 63: | Line 58: | ||
* Bones provide a frame for other soft tissues of the musculoskeletal system to attach to such as muscles, tendons, and ligaments. These allow for support as well as the movement by contracting and relaxing of the muscles which then, in turn, result in flexion, extension, abduction, adduction, and other forms of movement. | * Bones provide a frame for other soft tissues of the musculoskeletal system to attach to such as muscles, tendons, and ligaments. These allow for support as well as the movement by contracting and relaxing of the muscles which then, in turn, result in flexion, extension, abduction, adduction, and other forms of movement. | ||
* Form a mechanical barrier to different structures within the human body. For example, the rib cage and the skull help shield our vital organs, the heart/lungs, and the brain, respectively, from trauma.<ref name=":3" /> | * Form a mechanical barrier to different structures within the human body. For example, the rib cage and the skull help shield our vital organs, the heart/lungs, and the brain, respectively, from trauma.<ref name=":3" /> | ||
# | |||
==== Synthetic ==== | ==== Synthetic ==== | ||
The marrow is found in the trabecular portions of bones and is responsible for hematopoiesis, or the production of red blood cells, white blood cells, and platelets.<ref name=":3" />{{#ev:youtube|v2u-k40uVvU}} | The marrow is found in the trabecular portions of bones and is responsible for hematopoiesis, or the production of red blood cells, white blood cells, and platelets.<ref name=":3" />{{#ev:youtube|v2u-k40uVvU}} | ||
| Line 75: | Line 72: | ||
== Remodelling: == | == Remodelling: == | ||
=== Clinical Significance | ==== Purpose: ==== | ||
* To allow bone to ordinarily adjust strength in proportion to the degree of bone stress. When subjected to heavy loads, bones will consequently thicken. | |||
* To rearrange shape of bone for proper support of mechanical forces in accordance with stress patterns. | |||
* To replace old bone which may be brittle/weak in order to maintain toughness of bone. New organic matrix is needed as the old organic matrix degenerates<ref>Kobayashi S, Takahashi HE, Ito A, Saito N, Nawata M, Horiuchi H, Ohta H, Iorio R, Yamamoto N, Takaoka K. Trabecular minimodeling in human iliac bone. Bone. 2003 Feb 1;32(2):163-9.</ref>. | |||
==== Calcium homeostasis/balance must exist between osteoclasts and osteoblasts activity ==== | |||
* If too much new tissue is formed, the bones become abnormally large and thick (acromegaly) | |||
* Excessive loss of calcium weakens the bones, as occurs in osteoporosis | |||
==== Repair: ==== | |||
* The osteoclasts function to remove fragments of dead or damaged bone by dissolving and reabsorbing calcium salts of bone matrix. Like a building that has just collapsed, the rubble must be removed before reconstruction can take place. Osteoblasts are activated to knit the broken ends of bone together.<ref name=":2" /> | |||
== Clinical Significance == | |||
Bone tissue is susceptible to a myriad of pathologies that may range from etiologies of embryological, metabolic, autoimmune, neoplastic, or idiopathic origins. These include, but are not limited to, the conditions discussed below. | Bone tissue is susceptible to a myriad of pathologies that may range from etiologies of embryological, metabolic, autoimmune, neoplastic, or idiopathic origins. These include, but are not limited to, the conditions discussed below. | ||
* [[Achondroplasia]] is a genetic disorder commonly associated as a cause of dwarfism. Individuals affected may present with short extremities due to decreased development of endochondral bone. | * [[Achondroplasia]] is a genetic disorder commonly associated as a cause of dwarfism. Individuals affected may present with short extremities due to decreased development of endochondral bone. | ||
| Line 90: | Line 93: | ||
* Skeletal [[Oncology|neoplasm]] begins in the metaphysis of long bones with patients complaining of bone pain with swelling or as a pathologic fracture (a break in the bone caused by weakness of the bone through disease rather than trauma). Much more common in teenagers than in the elderly.<ref name=":3">Baig MA, Bacha D. [https://www.ncbi.nlm.nih.gov/books/NBK541132/ Histology, Bone]. InStatPearls [Internet] 2019 May 5. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK541132/ (last accessed 10.2.2020)</ref> | * Skeletal [[Oncology|neoplasm]] begins in the metaphysis of long bones with patients complaining of bone pain with swelling or as a pathologic fracture (a break in the bone caused by weakness of the bone through disease rather than trauma). Much more common in teenagers than in the elderly.<ref name=":3">Baig MA, Bacha D. [https://www.ncbi.nlm.nih.gov/books/NBK541132/ Histology, Bone]. InStatPearls [Internet] 2019 May 5. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK541132/ (last accessed 10.2.2020)</ref> | ||
* Bone [[fracture]]<nowiki/>s | * Bone [[fracture]]<nowiki/>s | ||
*[[Osteoporosis|Osteoporosis]] | *[[Osteoporosis|Osteoporosis]] | ||
*[[Osteoarthritis|Osteoarthritis]] | *[[Osteoarthritis|Osteoarthritis]] | ||
*[[Osteomalacia]] | *[[Osteomalacia]] | ||
Revision as of 08:40, 10 February 2020
Original Editors -
Top Contributors - Lucinda hampton, Candace Goh, Admin, Shaimaa Eldib, Kim Jackson, Jess Bell, Wataru Okuyama, Khloud Shreif, Robin Tacchetti, George Prudden, Claire Knott, Manisha Shrestha, Sai Kripa, Tony Lowe, Stephanie Geeurickx, WikiSysop and Joao Costa
Introduction[edit | edit source]
The adult human skeleton is composed of 206 bones. At birth, there are approximately 270 bones, with the final adult count decreasing as a portion of these bones fuse during phases of skeletal growth and maturation.
- Bone is a metabolically active connective tissue that provides structural support, facilitates movement, and protects vital organs.
- It plays an important role in regulating mineral and acid-base balance homeostasis. It also provides the environment for hematopoiesis (blood cells production) within the bone marrow.
- Bone is composed of an extracellular matrix and bone cells (osteocytes)[1]. Under the right conditions, bone tissue undergoes a process of mineralization, formed by collagen matrix and hardened by deposited calcium. Bone tissue (osseous tissue) differs greatly from other tissues in the body. Bone is hard and many of its functions depend on that characteristic hardness.[2]The skeleton is composed of around 80% cortical bone and 20% trabecular bone.[3]
- Much of the cellular activity in a bone consists of removal and replacement at the same site, a process called remodelling. The remodelling process occurs throughout life and becomes dominant by the time that bone reaches its peak mass (typically by the early 20s). Remodelling continues throughout life so that most of the adult skeleton is replaced about every 10 years.[4]
Structure[edit | edit source]
The four general categories of bones are:
- long bones : include the clavicles, humeri, radii, ulnae, metacarpals, femurs, tibiae, fibulae, metatarsals, and phalanges
- short bones: include the carpal and tarsal bones, patellae, and sesamoid bones.
- flat bones: include the skull, mandible, scapulae, sternum, and ribs.
- irregular bones. include the vertebrae, sacrum, coccyx, and hyoid bone.
Flat bones form by membranous bone formation, whereas long bones are formed by a combination of endochondral and membranous bone formation.[5]
Gross anatomy:[edit | edit source]
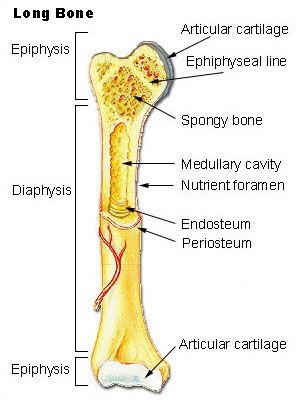
A long bone has two parts: the diaphysis and the epiphysis. The diaphysis is the tubular shaft that runs between the proximal and distal ends of the bone. The hollow region in the diaphysis is called the medullary cavity, which is filled with yellow marrow. The walls of the diaphysis are composed of dense and hard compact bone.[6]
Individual bone structure[edit | edit source]
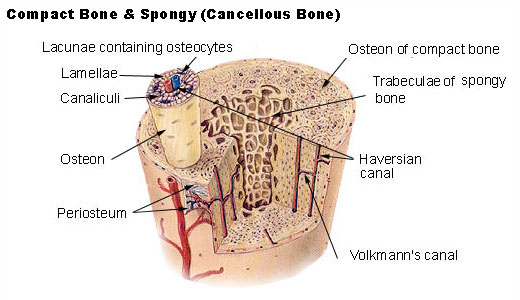
Architecturally, bone categorizes into two subtypes: cortical and trabecular bones.
- Cortical Bone: consists of about 80% of the total bone in the body and is much stronger than trabecular bone. It is very resistant to bending, torsion, and compression and is much more dense with a minimal role in metabolism. It is seen mostly in the shaft of long bones like the femur and the tibia as well as in the outer shell of trabecular bone.
- Trabecular Bone (spongy bone): consists of only 20% of the total bone but has ten times the surface/volume ratio of cortical bone. It responds eight times faster to changes in load making it far more dynamic. It occurs in areas that more subject to compression such as the vertebral body, pelvis, and the metaphyses.[7]
Cellular structure[edit | edit source]
As a specialized connective tissue, bone is comprised of mainly type 1 collagen fibers and inorganic salts.
Type 1 collagen is a non-calcified matrix (osteoid) designed to resist the tension experienced by the weight-bearing functions of bone. It forms from osteoblasts, the main cellular component of bone.
Osteoblasts produce matrix, build up bone tissue. They function in the production, transport, and arrangement of the osteoid matrix. Furthermore, they initiate and regulate matrix mineralization and control the neighboring bone cells activities.
Once the osteoid is mineralized, the precursor cells get surrounded by organic intracellular substances called lacunae to become fully developed and matured into osteocytes. The mineral content is chiefly hydroxyapatite crystals composed of mainly calcium and phosphate ions but can occasionally have sodium and carbonite as well.
Osteocytes maintain bone tissue by mineralising osteoid. They have a widespread distribution. Their cell processes are fundamental to allows osseous tissue to be responsive to the mechanical and metabolic organism constraints.
Osteoclasts, maintain bone tissue by mineralising osteoid. They are the large, multinucleated cells on the surface of bones in pits called Howship lacunae responsible for removing calcium from bone by secreting proteolytic enzymes and hydrogen ions to dissolve the calcium hydroxyapatite crystals. On average, osteoclasts have 12 nuclei, though the number may range from 2 to as many as 100. In their cytoplasm, interconnecting actin filaments produce a clear area between the cell membrane and the nuclei
Osteons represents a single functional unit of bone tissue. It is arranged with concentric lamellae of collagen fiber orientations around a central canal consisting of osteocyte’s arterial, venous, and nerve supply, is known as the Haversian canal. This system also consists of the canaliculi and Volkmann canal which allow for communication between neighboring osteocytes and communication between neighboring osteons, respectively.[7]
Molecular structure
Approximately 20% of in vivo bone is water. Of the dry bone mass, 60-70% of is bone mineral in the form of small crystals and the rest is collagen. The composition of the mineral component is hydroxyapatite Ca10(PO4)6(OH)2 and collagen is the main fibrous protein of the human body.
Functions:[edit | edit source]
Mechanical[edit | edit source]
- Bones provide a frame for other soft tissues of the musculoskeletal system to attach to such as muscles, tendons, and ligaments. These allow for support as well as the movement by contracting and relaxing of the muscles which then, in turn, result in flexion, extension, abduction, adduction, and other forms of movement.
- Form a mechanical barrier to different structures within the human body. For example, the rib cage and the skull help shield our vital organs, the heart/lungs, and the brain, respectively, from trauma.[7]
Synthetic[edit | edit source]
The marrow is found in the trabecular portions of bones and is responsible for hematopoiesis, or the production of red blood cells, white blood cells, and platelets.[7]
Metabolic;[5][edit | edit source]
- The bone matrix can store several minerals, chiefly calcium and phosphorus as well as iron in the form of ferritin.
- Chondroitin sulfate, a carbohydrate moiety, is also a commonly found element in the matrices.
- Specific growth factors, including insulin-like growth factor or IGF-1, are housed in bone and then released periodically.
- pH balance is also regulated as bones may alter the composition of alkaline salts in the serum to maintain the optimal pH level.
- Osteocytes can engulf toxic molecules and heavy metals from the serum as a means of detoxification
- Fat storage[7]
Remodelling:[edit | edit source]
Purpose:[edit | edit source]
- To allow bone to ordinarily adjust strength in proportion to the degree of bone stress. When subjected to heavy loads, bones will consequently thicken.
- To rearrange shape of bone for proper support of mechanical forces in accordance with stress patterns.
- To replace old bone which may be brittle/weak in order to maintain toughness of bone. New organic matrix is needed as the old organic matrix degenerates[8].
Calcium homeostasis/balance must exist between osteoclasts and osteoblasts activity[edit | edit source]
- If too much new tissue is formed, the bones become abnormally large and thick (acromegaly)
- Excessive loss of calcium weakens the bones, as occurs in osteoporosis
Repair:[edit | edit source]
- The osteoclasts function to remove fragments of dead or damaged bone by dissolving and reabsorbing calcium salts of bone matrix. Like a building that has just collapsed, the rubble must be removed before reconstruction can take place. Osteoblasts are activated to knit the broken ends of bone together.[5]
Clinical Significance[edit | edit source]
Bone tissue is susceptible to a myriad of pathologies that may range from etiologies of embryological, metabolic, autoimmune, neoplastic, or idiopathic origins. These include, but are not limited to, the conditions discussed below.
- Achondroplasia is a genetic disorder commonly associated as a cause of dwarfism. Individuals affected may present with short extremities due to decreased development of endochondral bone.
- Paget disease of the bone is characterized to be an imbalance amongst the activities of osteoblasts and osteoclasts. Of unknown etiology, the condition only affects localized portions of the skeletal tissue, generally involving one or more neighboring bones rather than the diffuse skeletal system.
- If untreated, Paget disease of the bone can act as a risk factor for osteosarcoma, a malignant proliferation of osteoblasts.
- Skeletal neoplasm begins in the metaphysis of long bones with patients complaining of bone pain with swelling or as a pathologic fracture (a break in the bone caused by weakness of the bone through disease rather than trauma). Much more common in teenagers than in the elderly.[7]
- Bone fractures
- Osteoporosis
- Osteoarthritis
- Osteomalacia
- Rickets
- Epiphyseal plate disorders
References[edit | edit source]
- ↑ El Sayed SA, Nezwek TA, Varacallo M. Physiology, Bone. InStatPearls [Internet] 2019 Jul 29. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK441968/ (last accessed 10.2.2020)
- ↑ Opentextbc.ca. (2018). 6.3 Bone Structure – Anatomy and Physiology. [online] Available at: https://opentextbc.ca/anatomyandphysiology/chapter/6-3-bone-structure/
- ↑ Singh S, Bray TJ, Hall-Craggs MA. Quantifying bone structure, micro-architecture, and pathophysiology with MRI. Clinical radiology. 2018 Mar 1;73(3):221-30.
- ↑ Office of the Surgeon General (US. The Basics of Bone in Health and Disease. InBone Health and Osteoporosis: A Report of the Surgeon General 2004. Office of the Surgeon General (US). Available from:https://www.ncbi.nlm.nih.gov/books/NBK45504/ (last accessed 10.2.2020)
- ↑ 5.0 5.1 5.2 Clarke B. Normal bone anatomy and physiology. Clinical journal of the American Society of Nephrology. 2008 Nov 1;3(Supplement 3):S131-9.
- ↑ Hall JE. Guyton and Hall textbook of medical physiology e-Book. Elsevier Health Sciences; 2015 May 31.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 Baig MA, Bacha D. Histology, Bone. InStatPearls [Internet] 2019 May 5. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK541132/ (last accessed 10.2.2020)
- ↑ Kobayashi S, Takahashi HE, Ito A, Saito N, Nawata M, Horiuchi H, Ohta H, Iorio R, Yamamoto N, Takaoka K. Trabecular minimodeling in human iliac bone. Bone. 2003 Feb 1;32(2):163-9.