Breast Cancer Related Lymphedema: Difference between revisions
No edit summary |
Claire Knott (talk | contribs) No edit summary |
||
| Line 23: | Line 23: | ||
== The Impact of Surgery, Radiation and Chemotherapy Therapy on Lymphedema Risk == | == The Impact of Surgery, Radiation and Chemotherapy Therapy on Lymphedema Risk == | ||
#[[File:Sentinel group1.png|right|frameless|308x308px]]Surgery implications: All of the lymph fluid from one side of the upper body (the chest, the ribcage, the arm and hand) drain to the axillary lymph nodes. The more lymph nodes and vessels removed, the greater the likelihood that this flow is going to be disrupted and potentially cause Lymphoedma.The dissection and assessment of the axillary lymph nodes | #[[File:Sentinel group1.png|right|frameless|308x308px]]Surgery implications: All of the lymph fluid from one side of the upper body (the chest, the ribcage, the arm and hand) drain to the axillary lymph nodes. The more lymph nodes and vessels removed, the greater the likelihood that this flow is going to be disrupted and potentially cause Lymphoedma.The dissection and assessment of the axillary lymph nodes is an essential and routine component in the process of staging and determination of adjuvant therapy modalities. Axillary lymph node dissection (ALND) may result in significant postoperative morbidity (60%) and severe complications, including lymphedema of the arm, seroma, sensory numbness, paresthesia, pain and infection. | ||
* Lymphedema is of particular concern, as it occurs in 6–30% of patients, and no curative therapy is available. | * Lymphedema is of particular concern, as it occurs in 6–30% of patients, and no curative therapy is available. | ||
* With the advent of improved screening modalities, breast cancer is now being diagnosed and treated at an early stage, prior to lymph node metastasis.<ref>Rahman M, Mohammed S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4533217/ Breast cancer metastasis and the lymphatic system.] Oncology letters. 2015 Sep 1;10(3):1233-9.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4533217/ (accessed 27.1.2021)</ref> | * With the advent of improved screening modalities, breast cancer is now being diagnosed and treated at an early stage, prior to lymph node metastasis.<ref>Rahman M, Mohammed S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4533217/ Breast cancer metastasis and the lymphatic system.] Oncology letters. 2015 Sep 1;10(3):1233-9.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4533217/ (accessed 27.1.2021)</ref> | ||
| Line 33: | Line 33: | ||
== Physiotherapy == | == Physiotherapy == | ||
More than one in five patients who undergo treatment for breast cancer will develop breast cancer-related lymphedema (BCRL). Lymphedema can develop at any stage following cancer treatment with most diagnoses being made between three months and 20 years. Identifying and treating lymphedema early leads to best outcomes. | |||
The physical therapist works closely with the client and other members of the health care team to optimise function, enhance participation and manage the symptoms, namely swelling, caused by lymphedema. Therapy generally consists of: | |||
* Quality patient education that begins early in the post-operative period and is followed by evidence-based physiotherapy can be effective in reducing the risk of lymphedema in women who undergo breast cancer surgery with ALND<ref>Lu SR, Hong RB, Chou W, Hsiao PC. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4348127/ Role of physiotherapy and patient education in lymphedema control following breast cancer surgery]. Therapeutics and clinical risk management. 2015;11:319.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4348127/<nowiki/>(accessed 28.1.2021)</ref>. | |||
* [[Manual Lymphatic Drainage|Manual lymphatic drainage]] (MLD), a type of hands-on therapy, is frequently used for BCRL and often as part of complex decongestive therapy (CDT). | * [[Manual Lymphatic Drainage|Manual lymphatic drainage]] (MLD), a type of hands-on therapy, is frequently used for BCRL and often as part of complex decongestive therapy (CDT). | ||
* [[Complete Decongestive Therapy (CDT)|CDT]] is a fourfold conservative treatment which includes MLD, compression therapy (consisting of compression bandages, compression sleeves, or other types of compression garments), skin care, and lymph-reducing exercises (LREs)<ref name=":1">Ezzo J, Manheimer E, McNeely ML, Howell DM, Weiss R, Johansson KI, Bao T, Bily L, Tuppo CM, Williams AF, Karadibak D. [https://pubmed.ncbi.nlm.nih.gov/25994425/ Manual lymphatic drainage for lymphedema following breast cancer treatment.] Cochrane Database of Systematic Reviews. 2015(5).Available from:https://pubmed.ncbi.nlm.nih.gov/25994425/ (accessed 27.1.2021)</ref>. | * [[Complete Decongestive Therapy (CDT)|CDT]] is a fourfold conservative treatment which includes MLD, compression therapy (consisting of compression bandages, compression sleeves, or other types of compression garments), skin care, and lymph-reducing exercises (LREs)<ref name=":1">Ezzo J, Manheimer E, McNeely ML, Howell DM, Weiss R, Johansson KI, Bao T, Bily L, Tuppo CM, Williams AF, Karadibak D. [https://pubmed.ncbi.nlm.nih.gov/25994425/ Manual lymphatic drainage for lymphedema following breast cancer treatment.] Cochrane Database of Systematic Reviews. 2015(5).Available from:https://pubmed.ncbi.nlm.nih.gov/25994425/ (accessed 27.1.2021)</ref>. | ||
Physiotherapists should encourage clients to keep doing all of the activities that they enjoy. Research has shown that no activity level, occupation, or hobby is related to developing lymphedema. | Physiotherapists should encourage clients to keep doing all of the activities that they enjoy. Research has shown that no activity level, occupation, or hobby is related to developing lymphedema. Resistance training has been shown to be safe and may assist in preventing lymphedema<ref>Schmitz KH, Ahmed RL, Troxel A, Cheville A, Smith R, Lewis-Grant L, Bryan CJ, Williams-Smith CT, Greene QP. [https://www.nejm.org/doi/full/10.1056/NEJMoa0810118 Weight lifting in women with breast-cancer–related lymphedema.] New England Journal of Medicine. 2009 Aug 13;361(7):664-73.Available from:https://www.nejm.org/doi/full/10.1056/NEJMoa0810118 (accessed 28.1.2021)</ref>. [[File:Lymphedema Compression sleeve.jpg|right|frameless]] | ||
Image: Lymphoedma compression sleeve | Image: Lymphoedma compression sleeve | ||
For | For further physiotherapy specific information, see [[Lymphoedema]] and/or [[Breast Cancer]] | ||
== References == | == References == | ||
Revision as of 05:10, 31 January 2021
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Claire Knott and Temitope Olowoyeye
Introduction[edit | edit source]
Breast cancer–related lymphedema (BCRL) is a potentially debilitating and often irreversible complication of breast cancer treatment. Risk of BCRL is proportional to the extent of axillary surgery and radiation. Other risk factors include obesity and infections. Minimizing axillary surgery and radiation has been proven to reduce the risk of BCRL.
Comprehensive multidisciplinary assessment at the time of initial diagnosis; early referral to physical therapy after surgery; and patient education regarding weight loss, skin, and nail care are cornerstones of the management of early-stage lymphedema.
End-stage lymphedema may benefit from referral to a plastic surgeon specializing in lymphedema surgery[1].
Lymphatic Involvement[edit | edit source]
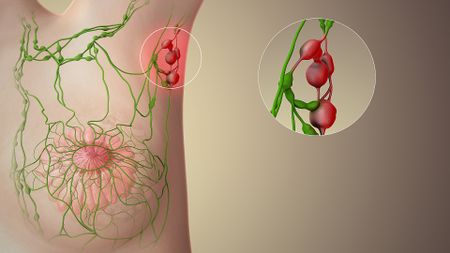
The inherent characteristics of the lymphatic physiology serve as the primary route for tumor cell metastasis. Image illustrating sentinel lymph nodes. The axillary lymph nodes drain 75% of the lymph from the breasts and so may swell in cancer.
- The increasing size of the tumor triggers a rise in the intratumoral interstitial fluid pressure, and interstitial fluid is released as the system attempts to achieve homeostasis.
- Unlike the vascular vessels, the lymphatic vessels are highly permeable; the flow rate is approximately 100–500x slower, and coupled with lesser shearing stresses due to vasodilation.
- The lymphatic route is superior in facilitating tumor cell dissemination.
- Breast tumors, in particular, preferentially utilize the lymphatic system for tumor cell dissemination.
- Lymph nodes act as a reservoir for tumor cells to take root and form metastatic tumors. The extent of lymph node involvement and regional lymph node status is considered to be crucial in patient prognosis.
The Impact of Surgery, Radiation and Chemotherapy Therapy on Lymphedema Risk[edit | edit source]
- Surgery implications: All of the lymph fluid from one side of the upper body (the chest, the ribcage, the arm and hand) drain to the axillary lymph nodes. The more lymph nodes and vessels removed, the greater the likelihood that this flow is going to be disrupted and potentially cause Lymphoedma.The dissection and assessment of the axillary lymph nodes is an essential and routine component in the process of staging and determination of adjuvant therapy modalities. Axillary lymph node dissection (ALND) may result in significant postoperative morbidity (60%) and severe complications, including lymphedema of the arm, seroma, sensory numbness, paresthesia, pain and infection.
- Lymphedema is of particular concern, as it occurs in 6–30% of patients, and no curative therapy is available.
- With the advent of improved screening modalities, breast cancer is now being diagnosed and treated at an early stage, prior to lymph node metastasis.[2]
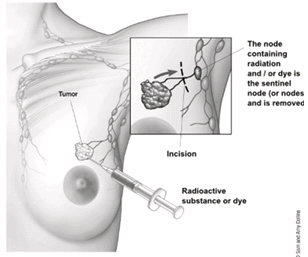
- Now, when possible, surgeon favour sentinel lymph node biopsy (SLNB). This surgery removes just the first few lymph nodes, the “sentinel nodes”, that drain fluid away from the breast. Identification of the sentinel nodes is done by mapping the flow of lymph with a radioactive substance or blue dye. If the sentinel nodes are free of cancer cells, then no additional nodes need to be removed (lowering risk of Lymphoedema).[3]
2. Radiation treatments also can affect the lymphatic system.
- Radiation therapy can cause the formation of scar tissue that presses on or narrows the remaining lymph vessels and nodes. This interferes even further with the flow of lymph out of the arm and upper body.
- Radiation directly to the underarm carries the most risk for radiation-related lymphedema, since this is where most of the nodes are, but radiation to the breast or chest areas also increases risk[3].
3. Adjuvant chemotherapy, especially docetaxel, is a risk factors for breast cancer-related lymphedema.[4][5] Docetaxel use results in the hyperstabilization of microtubule assembly. Treatment of cells with docetaxel causes the inhibition of major cellular events, such as mitotic cell division, endosomal uptake, secretion, and transport[6].
Physiotherapy[edit | edit source]
More than one in five patients who undergo treatment for breast cancer will develop breast cancer-related lymphedema (BCRL). Lymphedema can develop at any stage following cancer treatment with most diagnoses being made between three months and 20 years. Identifying and treating lymphedema early leads to best outcomes.
The physical therapist works closely with the client and other members of the health care team to optimise function, enhance participation and manage the symptoms, namely swelling, caused by lymphedema. Therapy generally consists of:
- Quality patient education that begins early in the post-operative period and is followed by evidence-based physiotherapy can be effective in reducing the risk of lymphedema in women who undergo breast cancer surgery with ALND[7].
- Manual lymphatic drainage (MLD), a type of hands-on therapy, is frequently used for BCRL and often as part of complex decongestive therapy (CDT).
- CDT is a fourfold conservative treatment which includes MLD, compression therapy (consisting of compression bandages, compression sleeves, or other types of compression garments), skin care, and lymph-reducing exercises (LREs)[8].
Physiotherapists should encourage clients to keep doing all of the activities that they enjoy. Research has shown that no activity level, occupation, or hobby is related to developing lymphedema. Resistance training has been shown to be safe and may assist in preventing lymphedema[9].
Image: Lymphoedma compression sleeve
For further physiotherapy specific information, see Lymphoedema and/or Breast Cancer
References[edit | edit source]
- ↑ Tandra P, Kallam A, Krishnamurthy J. Identification and management of lymphedema in patients with breast cancer. Journal of oncology practice. 2019 May;15(5):255-62.Available from:https://ascopubs.org/doi/10.1200/JOP.18.00141 (accessed 27.1.2021)
- ↑ Rahman M, Mohammed S. Breast cancer metastasis and the lymphatic system. Oncology letters. 2015 Sep 1;10(3):1233-9.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4533217/ (accessed 27.1.2021)
- ↑ 3.0 3.1 Breast cancer org. Lymphoedema Available from:https://www.breastcancer.org/treatment/lymphedema/how/treat_impact (accessed 27.1.2021)
- ↑ https://lymphoedemaeducation.com.au/resources/risk-factors-for-breast-cancer%E2%80%91related-lymphedema-correlation-with-docetaxel-administration/ (accessed 27.1.2021)
- ↑ Aoishi Y, Oura S, Nishiguchi H, Hirai Y, Miyasaka M, Kawaji M, Shima A, Nishimura Y. Risk factors for breast cancer-related lymphedema: correlation with docetaxel administration. Breast Cancer. 2020 Sep;27(5):929-37.Available from:https://pubmed.ncbi.nlm.nih.gov/32270417/ (accessed 27.1.2021)
- ↑ Morse DL, Gray H, Payne CM, Gillies RJ. Docetaxel induces cell death through mitotic catastrophe in human breast cancer cells. Molecular cancer therapeutics. 2005 Oct 1;4(10):1495-504.Available from: https://mct.aacrjournals.org/content/4/10/1495(accessed 27.1.2021)
- ↑ Lu SR, Hong RB, Chou W, Hsiao PC. Role of physiotherapy and patient education in lymphedema control following breast cancer surgery. Therapeutics and clinical risk management. 2015;11:319.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4348127/(accessed 28.1.2021)
- ↑ Ezzo J, Manheimer E, McNeely ML, Howell DM, Weiss R, Johansson KI, Bao T, Bily L, Tuppo CM, Williams AF, Karadibak D. Manual lymphatic drainage for lymphedema following breast cancer treatment. Cochrane Database of Systematic Reviews. 2015(5).Available from:https://pubmed.ncbi.nlm.nih.gov/25994425/ (accessed 27.1.2021)
- ↑ Schmitz KH, Ahmed RL, Troxel A, Cheville A, Smith R, Lewis-Grant L, Bryan CJ, Williams-Smith CT, Greene QP. Weight lifting in women with breast-cancer–related lymphedema. New England Journal of Medicine. 2009 Aug 13;361(7):664-73.Available from:https://www.nejm.org/doi/full/10.1056/NEJMoa0810118 (accessed 28.1.2021)