Cervical Cancer: Difference between revisions
Anna Usery (talk | contribs) No edit summary |
Anna Usery (talk | contribs) No edit summary |
||
| Line 36: | Line 36: | ||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
Cervical cancer is associated with and may be the manifestation of HPV.<ref name="Five" /><br> | |||
== Medications == | == Medications == | ||
Revision as of 03:04, 20 March 2014
Original Editors - Anna Marie Usery & Stephanie Wilton from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Anna Usery, Stephanie Wilton, Kim Jackson, Nupur Smit Shah, WikiSysop, Rewan Elsayed Elkanafany, Elaine Lonnemann, Vidya Acharya, Manisha Shrestha, Lucinda hampton and Wendy Walker
Definition/Description[edit | edit source]
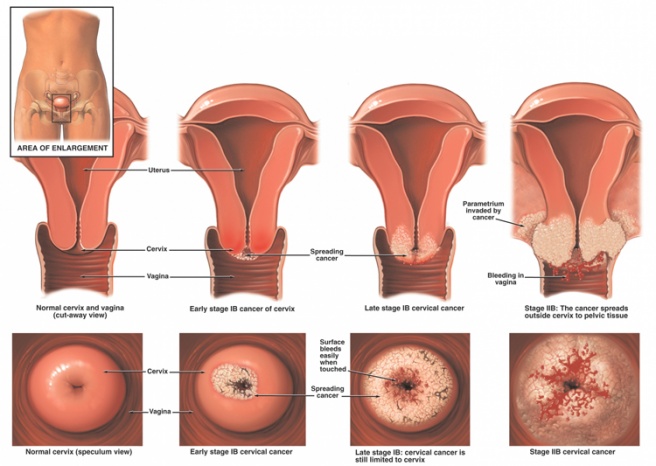
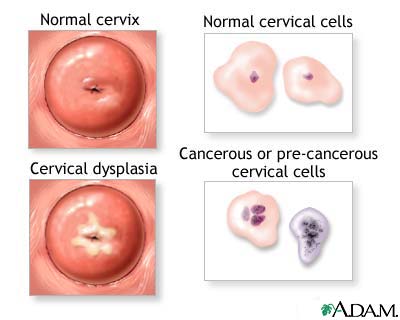
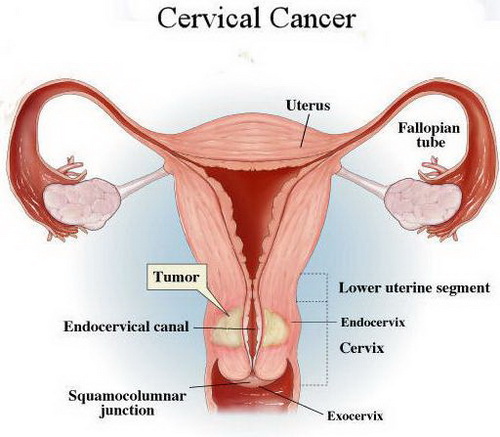
Cervical cancer is a type of cancer that forms within the tissues of the cervix.[1]The cervix connects the uterus with the vagina (birth cancal).[1], [2]The endocervix is the portion of the cervix closest to the uterus whereas the exocervix or ectocervix is closest to the vagina.[2] The cervix is covered in two main types of cells: squamous cells found on the exocervix, and glandular cells on the endocervix.[2] Squamous and glandular cells come together at the area known as the transformation zone. It is here where most cervical cancers originate.[2] Gradually, the normal cells lining this area develop pre-cancerous changes that change into cancer.[2] Cervical cancer typically grows at a slow rate and presents asymptomatically.[1] Therefore, it is recommended to receive routine Papanicolaou smears to test for changes in the lining of the cervix and/or the development of cancerous cells.[1]
Prevalence[edit | edit source]
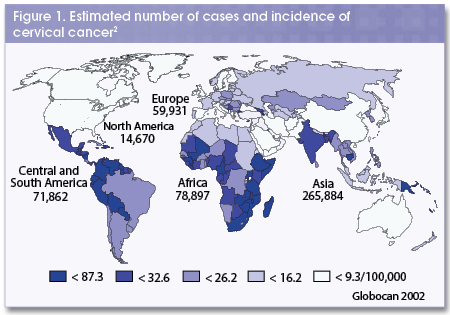
In the United States, cervical cancer is the fourteenth most common type of cancer found in women, and the third most common gynecological malignancy.[3],[4] However worldwide, cervical cancer is the most commonly found type of cancer in women.[3] In the United States, diagnosis of invasive stage cervical cancer has declined (75% decline since the 1960s) steadily.[3],[4]Screening for cervical cancer has become more common due to the introduction of the Pap smear in the 1930’s which made early detection possible.[5] Although cervical cancer is the most common cause of gynecological cancer-related death worldwide, mortality rates have decreased significantly in the United States (more than 45% since the early 1970s).[4],[5]
In the United States, approximately 11,000 women are diagnosed with cervical cancer and 3,700 women die due to the disease each year.[5] Worldwide,nearly 500,000 women are diagnosed with cervical cancer annually.[6] The disease accounts for 288,000 deaths per year.[5]
80% to 85% of cervical cancer realted deaths occur in developing countries.[6]
Pre-invasive carcinoma in situ (no invasion of surrounding tissues) is more common in women 30-40 years of age.[4] Invasive carcinoma is more frequent in women over 40 years of age.[4] Women ages 65 and over account for 25% of new cases of cervical cancer.[5]
Characteristics/Clinical Presentation[edit | edit source]
- May be asymptomatic (early stages)[4]
- Painful intercourse or pain after intercourse[4]
- Unexplained or unexpected bleeding (after intercourse or between menstrual periods)[3],[4]
- Watery, foul-smelling vaginal discharge (serosanguineous or yellowish color)[3],[4]
- Pelvic, epigastric, or low back pain (with large lesions)[3],[5]
- Hemiparesis, headache (cancer recurrence with brain metastases)[4]
- Bowel and bladder problems (later stages)[5]
Associated Co-morbidities[edit | edit source]
Cervical cancer is associated with and may be the manifestation of HPV.[5]
Medications[edit | edit source]
Drugs Approved to Prevent Cervical Cancer[1]
- Cervarix (Recombinant HPV Bivalent Vaccine)
- Gardasil (Recombinant HPV Quadrivalent Vaccine)
- Recombinant Human Papillomavirus (HPV) Bivalent Vaccine
- Recombinant Human Papillomavirus (HPV) Quadrivalent Vaccine
Drugs Approved to Treat Cervical Cancer[1],[7]
*Systemic Chemotherapy involves injecting or orally administering cancer-treating drugs.[7] These drugs then enter the bloodstream, and travel throughout the body, reaching areas of cancerous growth.[7]Chemotherapy can work in the following ways:[1][8]
-Cure the cancer
-Shrink the cancer
-Relieve symptoms
-Prolong life span by controlling cancer or putting it into remission
Chemotherapy is often delivered in cycles.[7] Periods of treatment are followed by periods of recovery.[7]
- Blenoxane (Bleomycin)-mixture of cytotoxic glycopeptide antibiotics; Side effects- Pulmonary fibrosis, hypotension, mental confusion, fever, chills and wheezing.[9]
- Cisplatin*-sterile aqueous solution that contains sodium chloride in water for injection; Side effects- Renal toxicity, nausea and vomitting, myelo-suppression, ototoxicity, facial edema, bronchoconstriction, tachycardia, hypotension[9]
- Hycamtin (Topotecan Hydrochloride)- anti-tumor drug with topoisomerase 1-inhibitory activity[9]
- Platinol (Cisplatin)
- Platinol-AQ (Cisplatin)
- Topotecan Hydrochloride (Hycamtin)
- Carboplatin
- Paclitaxel* (Taxol)- nonaqueous solution with antitumor activity; Side effects- anaphylaxis, dypsnea, hypotension, angioedema, urticaria (hives)[9]
- Gemcitabine (Gemzar)-nucleoside metabolic inhibitor that exhibits antitumor activity; Side effects- pallor, easy bruising or bleeding, unusual weakness, decreased urination, nausea, upper stomach pain, dark urine, clay-colored stools, jaundice, chest pain, pain spreading to arm or shoulder, diaphoresis, signs of allergic reaction[9]
*Currently, Cisplatin is the most effective single chemotherapy drug for recurrent disease.[10] When administered with paclitaxel, the combination is more effective than cisplatin alone (in terms of response rate and survival).[10]
Drug Combinations Used in Cervical Cancer[1]
- Gemcitabine-Cisplatin
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Medical professionals who are able to diagnose cervical cancer include:[11]
- Gynecologists
- Obstetricians
- Family physicians
- Nurse practitoner
- Physican assistants
- Internists
Screening Tests:
- Pap smear
A Pap smear, also referred to as a Pap test, tests cervical cells for abnormal changes.[12] It is these abnormal cellular changes that can lead to cervical cancer if left untreated.[12] Cervical cancer is highly preventable, given that regular Pap smears are performed.[12] It is recommended that women receive annual Pap smears beginning three years after the onset of vaginal intercourse but no later than 21 years of age.[5] Women aged 70 and older, with an intact cervix, are no longer required to recevie Pap smears if they have had no positive test results within the last 10 years.[5] Women who do not have a cervix (ex. hysterectomy) as well as no history of abnormal Pap results or cervical cancer can discontinue annual Pap smears.[12] However, some medical professionals support routine Pap smears regardless of age, presence of cervix, or past negative test results.[5] Even if not currently sexually active, or protected sex is being practiced, regular Pap smears should still be performed.[12]
Diagnostic Tests:
-Imaging:[13]
*Tumor must be at least stage 1b or greater to be seen on a radiograph.
- Magnetic resonance imaging (MRI)- imaging modality of choice for depicting primary tumor
- Ultrasound- tumor appears as a hypoechoic (dark) cervical mass; should not be used as primary diagnositc tool
- Computed tomography (CT)-used to assess disease in more advanced stages and/or monitor distant metastasis
- Positron emission tomography (PET)-CT- imaging modality of choice for staging cervical cancer
-Biopsy:[2]
- Colposcopic
- Endocervical curetttage (scraping)
- Cone
Etiology/Causes[edit | edit source]
The presence of human papillomavirus (HPV) is a common feature in the majority of individuals diagnosed with cervical cancer.[5] The disease normally spreads through local extension and through the lymphatic system to the retroperitoneal lymph nodes.
- Early age at first sexual intercourse (17 years or younger)
- Early age at first pregnancy
- Tobacco use, including exposure to passive smoke
- Low socioeconomic status (lack of screening)
- History of any sexually transmitted disease (STD), especially HPV and human immunodeficiency virus (HIV)
- History of multiple sex partners (five or more)
- History of childhood sexual abuse
- Intimate partner abuse
- Women whose mothers used the drug diethylstilbestrol (DES) during pregnancy
- Hormonal contraceptive use
- Ethnic background- African-American women experience a 72% higher incident compared with Caucasian women
- High parity (number of births)
- Alcohol and drug use (impaired decision making)
Systemic Involvement[edit | edit source]
627
Medical Management (current best evidence)[edit | edit source]
add text here
Physical Therapy Management (current best evidence)[edit | edit source]
add text here
Alternative/Holistic Management (current best evidence)[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
Infections
- Polyps
- Cervical conditions (infections, polyps, myomas)
- Iatrogenic (birth control pills, HRT, IUD)
- Cervical ectopic pregnancy (consider with women of childbearing age)
- Endometrial cancer with cervical invasion
- Other cervical malignant condition (sarcoma, lymphoma, metastasis)
- Invasion of cervix from other organ in proximty:
-bladder cancer
-rectal cancer
-vaginal cancer
-uterine cancer
Case Reports/ Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: addfeedhere|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Available at: http://www.cancer.gov/cancertopics/types/cervical. Accessed March 18, 2014.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Available at: http://www.cancer.org/cancer/cervicalcancer/detailedguide/cervical-cancer-what-is-cervical-cancer. Accessed March 18, 2014.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Ph.d. SE, Ph.d. KL. Understanding Pathophysiology. Mosby Incorporated; 2011.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 Goodman CC, Snyder TE. Differential Diagnosis for Physical Therapists, Screening for Referral. W B Saunders Company; 2012.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 Reviews CT. e-Study Guide for: Pathology: Implications for the Physical Therapist by Catherine C. Goodman, ISBN 9781416031185. Cram101 Textbook Reviews; 2012.
- ↑ 6.0 6.1 Available at: http://www.rho.org/about-cervical-cancer.htm. Accessed March 18, 2014.
- ↑ 7.0 7.1 7.2 7.3 7.4 Available at: http://www.cancer.org/treatment/treatmentsandsideeffects/treatmenttypes/chemotherapy/chemotherapyprinciplesanin-depthdiscussionofthetechniquesanditsroleintreatment/chemotherapy-principles-types-of-chemo-drugs. Accessed March 19, 2014.
- ↑ Available at: http://www.cancerresearchuk.org/cancer-help/about-cancer/treatment/chemotherapy/about/how-chemotherapy-works. Accessed March 18, 2014.
- ↑ 9.0 9.1 9.2 9.3 9.4 Available at: http://www.rxlist.com/script/main/hp.asp. Accessed March 19, 2014.
- ↑ 10.0 10.1 Cervical cancer. The Lancet. 2003;361(9376):2217.
- ↑ Available at: http://www.webmd.com/cancer/cervical-cancer/cervical-cancer-when-to-call-a-doctor. Accessed March 19, 2014.
- ↑ 12.0 12.1 12.2 12.3 12.4 Available at: http://www.womenshealth.gov/publications/our-publications/fact-sheet/pap-test.html. Accessed March 20, 2014.
- ↑ 13.0 13.1 13.2 Available at: http://radiopaedia.org/articles/carcinoma-of-the-cervix. Accessed March 19, 2014.
- ↑ 14.0 14.1 Available at: http://oncolex.org/en/Gynecological-cancer/Diagnoses/Cervical-cancer/Background/DifferentialDiagnoses. Accessed March 19, 2014.