Distal Radial Fractures: Difference between revisions
(reformatting references) |
(reformatting references) |
||
| Line 6: | Line 6: | ||
== Definition/Description == | == Definition/Description == | ||
The radius is the larger of the two bones of the forearm, located radially. The distal end of the radius is considered as the three centimeters proximal to the radiocarpal joint, where the radius interfaces with the lunate and scaphoid bone of the wrist. A fracture of the distal radius can be caused by falling on the outstretched arm. <ref name=":5">American Academy of Orthopaedic Surgeons. Distal Radius Fractures [Internet]. Rosemont Illinois: American Academy of Orthopaedic Surgeons; 2013 [cited 2017 Oct 19]. Available from: <nowiki>http://orthoinfo.aaos.org/topic.cfm?topic=a00412</nowiki></ref> | The radius is the larger of the two bones of the forearm, located radially. The distal end of the radius is considered as the three centimeters proximal to the radiocarpal joint, where the radius interfaces with the lunate and scaphoid bone of the wrist. A fracture of the distal radius can be caused by falling on the outstretched arm. <ref name=":5">American Academy of Orthopaedic Surgeons. Distal Radius Fractures [Internet]. Rosemont Illinois: American Academy of Orthopaedic Surgeons; 2013 [cited 2017 Oct 19]. Available from: <nowiki>http://orthoinfo.aaos.org/topic.cfm?topic=a00412</nowiki></ref> The majority of distal radial fractures are closed injuries in which the overlying skin remains intact.<ref name=":0">Handoll HHG, Huntley JS, Madhok R. External Fixation versus conservative treatment for distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-78.</ref> <ref name=":1">Handoll HHG, Huntley JS, Madhok R. Different methods of external fixation for treating distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-67.</ref> The radius is the most commonly broken bone in the arm.<br> | ||
For centuries they called this fracture a dislocation of the wrist but this description remains obscure. It was redefined by an Irish surgeon and anatomist, Abraham Colles, in 1814. Subsequently, the name of this injury was changed to a Colles fracture and the name continues to be used by surgeons.<ref>Benjamin JA. 1965. Abraham Colles (1773–1843) Distinguished surgeon from Ireland. Invest Urol 3:321–323</ref> | For centuries they called this fracture a dislocation of the wrist but this description remains obscure. It was redefined by an Irish surgeon and anatomist, Abraham Colles, in 1814. Subsequently, the name of this injury was changed to a Colles fracture and the name continues to be used by surgeons.<ref>Benjamin JA. 1965. Abraham Colles (1773–1843) Distinguished surgeon from Ireland. Invest Urol 3:321–323</ref> <br> | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
| Line 28: | Line 28: | ||
The ulna is not part of the wrist joint – it articulates with the radius in two locations, the superior and the inferior radio-ulnar joint. Eighty percent of axial load is supported by the distal radius and 20% by the ulna. It is prevented from articulating with the carpal bones by a fibrocartilginous ligament, called the articular disk, which lies over the superior surface of the ulna.<br>Together, the carpal bones form a convex surface which articulates with the concave surface of the radius and articular disk. All the carpal joints are art sellaris (the concave part) and the radius the convex part of the joint is seen as an art sphaeroidea. | The ulna is not part of the wrist joint – it articulates with the radius in two locations, the superior and the inferior radio-ulnar joint. Eighty percent of axial load is supported by the distal radius and 20% by the ulna. It is prevented from articulating with the carpal bones by a fibrocartilginous ligament, called the articular disk, which lies over the superior surface of the ulna.<br>Together, the carpal bones form a convex surface which articulates with the concave surface of the radius and articular disk. All the carpal joints are art sellaris (the concave part) and the radius the convex part of the joint is seen as an art sphaeroidea. | ||
<br>There are several known ligamentous attachments to the distal radius. These often remain intact during distal radius fractures. The volar ligaments are stronger and give more stability to the radiocarpal articulation than the dorsal ligaments.<ref>Kenneth J. Koval, Joseph D. Zuckerman, Handbook of fractures, Philadelphia, second edition, 1994, pg 134.</ref> | <br>There are several known ligamentous attachments to the distal radius. These often remain intact during distal radius fractures. The volar ligaments are stronger and give more stability to the radiocarpal articulation than the dorsal ligaments.<ref>Kenneth J. Koval, Joseph D. Zuckerman, Handbook of fractures, Philadelphia, second edition, 1994, pg 134.</ref> | ||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
Distal radial fractures is one of the most common fractures of the upper extremity in adults, accounting for one-sixth of all fractures in the emergency department. It is seen predominantly in the older caucasian population.<ref name=":0" /> <ref name=":1" /> <ref>Abramo A, Kopylov P, Tagil M. Evaluation of a treatment protocol in distal radius fractures: a prospective study in 581 patients using DASH as outcome. Acta Orthopaedica. 2008;79(3):376-385</ref> <ref name=":2">Bienek T, Kusz D, Cielinski L. Peripheral nerve compression neuropathy after fractures of the distal radius. J Hand Surg. (British and European Volume). 2006;31B(3):256-260.</ref> <ref name=":11">Kay S, McMahon M, Stiller K. An advice and exercise program has some benefits over natural recovery after distal radius fracture: a randomized trial. Aust J Physiother. 2008;54:253-259. | Distal radial fractures is one of the most common fractures of the upper extremity in adults, accounting for one-sixth of all fractures in the emergency department. It is seen predominantly in the older caucasian population.<ref name=":0" /> <ref name=":1" /> <ref>Abramo A, Kopylov P, Tagil M. Evaluation of a treatment protocol in distal radius fractures: a prospective study in 581 patients using DASH as outcome. Acta Orthopaedica. 2008;79(3):376-385</ref> <ref name=":2">Bienek T, Kusz D, Cielinski L. Peripheral nerve compression neuropathy after fractures of the distal radius. J Hand Surg. (British and European Volume). 2006;31B(3):256-260.</ref> <ref name=":11">Kay S, McMahon M, Stiller K. An advice and exercise program has some benefits over natural recovery after distal radius fracture: a randomized trial. Aust J Physiother. 2008;54:253-259. | ||
</ref> | </ref> There is typically a history of a fall or similar trauma to the upper extremity. Pain and swelling in the forearm or wrist are common. Bruising and deformity in the wrist or forearm are also possible.<ref>Nelson DL. Wrist Fracture [Internet]. Greenbrae California: David Nelson MD; 2012 [cited 2017 Oct 19]. Available from: <nowiki>http://www.davidlnelson.md/articles/Wrist_Fracture.htm</nowiki></ref> | ||
In women, the incidence of occurrence increases with age starting at 40 years old, whereas before this age the incidence in men is much higher. Occurrences in younger adults are usually the result of a high-energy trauma such as a motor vehicle accident, fall from height or athletic participation.<ref>Kenneth J. Koval, Joseph D. Zuckerman, Handbook of fractures, Philadelphia, second edition, 1994, pg 134-135</ref> | In women, the incidence of occurrence increases with age starting at 40 years old, whereas before this age the incidence in men is much higher. Occurrences in younger adults are usually the result of a high-energy trauma such as a motor vehicle accident, fall from height or athletic participation.<ref>Kenneth J. Koval, Joseph D. Zuckerman, Handbook of fractures, Philadelphia, second edition, 1994, pg 134-135</ref> In older adults, such fractures are often the result of a low-energy or moderate trauma such as falling from standing height. This may reflect the greater fragility of the bone due to osteoporosis in the older adult.<ref name=":0" /> <ref>Leung F, Ozkan M, Chow SP. Conservative treatment of intra-articular fractures of the distal radius – factors affecting functional outcomes. Hand Surg. 2000;5(2):145-153.</ref> | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Distal radial fractures can be classified based on their clinical appearance and typical deformity. Dorsal displacement, dorsal angulation, dorsal comminution and radial shortening may all be used to describe the presentation of the fracture. Classification based on fracture patterns such as intra-articular (articular surfaces disrupted) or extra-articular (articular surface of radius intact) may also be used.<ref name=":0" /> <ref name=":6">Bushnell BD, Bynum DK. Malunion of the distal radius. J Am Acad Orthop Surg. 2007;15:27-40. | Distal radial fractures can be classified based on their clinical appearance and typical deformity. Dorsal displacement, dorsal angulation, dorsal comminution and radial shortening may all be used to describe the presentation of the fracture. Classification based on fracture patterns such as intra-articular (articular surfaces disrupted) or extra-articular (articular surface of radius intact) may also be used.<ref name=":0" /> <ref name=":6">Bushnell BD, Bynum DK. Malunion of the distal radius. J Am Acad Orthop Surg. 2007;15:27-40. | ||
</ref> | </ref> | ||
1. Classification of intra-articular fracture | 1. Classification of intra-articular fracture | ||
*Type Ι: stable, without comminution | *Type Ι: stable, without comminution | ||
*Type ΙΙ: unstable die-punch, dorsal of volar | *Type ΙΙ: unstable die-punch, dorsal of volar | ||
- ΙΙa: reducible<br> | - ΙΙa: reducible<br> - ΙΙb: irreducible<br> | ||
*Type ΙΙΙ: spike fracture; contuses volar structures | *Type ΙΙΙ: spike fracture; contuses volar structures | ||
*Type ΙV: split fracture : medial complex fractured with dorsal and palmar fragments displaced separately | *Type ΙV: split fracture : medial complex fractured with dorsal and palmar fragments displaced separately | ||
| Line 53: | Line 53: | ||
*Type A1: extra-articular ulna, radius intact | *Type A1: extra-articular ulna, radius intact | ||
*Type A2: extra-articular radius, ulna intact | *Type A2: extra-articular radius, ulna intact | ||
*Type A3: extra-articular, multi fragmentary radius fracture <ref name=":3">Kenneth J. Koval, Joseph D. Zuckerman, Handbook of fractures, Philadelphia, second edition, 1994, pg 135-138</ref> | *Type A3: extra-articular, multi fragmentary radius fracture <ref name=":3">Kenneth J. Koval, Joseph D. Zuckerman, Handbook of fractures, Philadelphia, second edition, 1994, pg 135-138</ref> | ||
=== Types of Fractures === | === Types of Fractures === | ||
| Line 61: | Line 61: | ||
This is typically due to a fall on an outstretched hand and results in a dorsal extra-articular or intra-articular displacement of the fractured radius: | This is typically due to a fall on an outstretched hand and results in a dorsal extra-articular or intra-articular displacement of the fractured radius: | ||
* Intra-articular fractures are generally seen in the younger age group secondary to higher energy forces | * Intra-articular fractures are generally seen in the younger age group secondary to higher energy forces | ||
* More than 90% of distal radius fractures are of this pattern <ref name=":3" /> | * More than 90% of distal radius fractures are of this pattern <ref name=":3" /> | ||
==== Smith's Fracture ==== | ==== Smith's Fracture ==== | ||
This is a reverse Colles with a volar displacement and a fall on a flexed wrist with forearm fixed in supination <ref name=":3" /> | This is a reverse Colles with a volar displacement and a fall on a flexed wrist with forearm fixed in supination <ref name=":3" /> | ||
==== Barton's Fracture ==== | ==== Barton's Fracture ==== | ||
| Line 71: | Line 71: | ||
This is an intra-articular fracture with subluxation or dislocation of the carpus bone. Of the eight grades for distal radial fractures in the Frykman Classification system, half include ulnar styloid involvement. | This is an intra-articular fracture with subluxation or dislocation of the carpus bone. Of the eight grades for distal radial fractures in the Frykman Classification system, half include ulnar styloid involvement. | ||
Complications are common and diverse. They may be the result of injury or treatment and are associated with poorer outcomes. These can include:<ref name=":4">Oren T, Wolf J. Soft- Tissue complications associated with distal radius fractures. Operative Techniques in Orthopaedics.19; 2009: 100—106.</ref> | Complications are common and diverse. They may be the result of injury or treatment and are associated with poorer outcomes. These can include:<ref name=":4">Oren T, Wolf J. Soft- Tissue complications associated with distal radius fractures. Operative Techniques in Orthopaedics.19; 2009: 100—106.</ref> | ||
* upper extremity stiffness | * upper extremity stiffness | ||
* carpal tunnel syndrome or medial nerve involvement | * carpal tunnel syndrome or medial nerve involvement | ||
| Line 82: | Line 82: | ||
* post-traumatic osteoarthritis | * post-traumatic osteoarthritis | ||
* compartment syndrome | * compartment syndrome | ||
* infection (mostly by open fractures)<ref name=":3" /> <ref name=":4" /> | * infection (mostly by open fractures) <ref name=":3" /> <ref name=":4" /> | ||
* [[Complex Regional Pain Syndrome (CRPS)|complex regional pain syndrome]] <ref name=":2" /> <ref name=":7">Kleinman WB. Distal radius instability and stiffness; common complications of distal radius fractures. Hand Clin. 2010;26:245-264.</ref> <ref name=":12">Handoll HHG, Madhok R. Conservative interventions for treating distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-112.</ref> <ref name=":8">Patel VP, Paksima N. Complications of distal radius fracture fixation. Bulletin of NYU Hospital for Joint Diseases. 2010;68(2):112-8.</ref> | * [[Complex Regional Pain Syndrome (CRPS)|complex regional pain syndrome]] <ref name=":2" /> <ref name=":7">Kleinman WB. Distal radius instability and stiffness; common complications of distal radius fractures. Hand Clin. 2010;26:245-264.</ref> <ref name=":12">Handoll HHG, Madhok R. Conservative interventions for treating distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-112.</ref> <ref name=":8">Patel VP, Paksima N. Complications of distal radius fracture fixation. Bulletin of NYU Hospital for Joint Diseases. 2010;68(2):112-8.</ref> <sup></sup> | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
| Line 89: | Line 89: | ||
Because the mechanism of injury for a distal radial fracture is usually a high energy traumatic incident, radiographs should be taken to confirm the diagnosis and ensure that the surrounding tissues are still intact. Other injuries causing radial sided pain may include [[Triangular Fibrocartilage Complex Injuries|TFCC tear or perforation]], [http://emedicine.medscape.com/article/1239331-overview Galeazzi fracture] (fracture to the distal 2/3 of the radius), [[Scaphoid Fracture|scaphoid fracture]], or radiocarpal ligament injury.<br> | Because the mechanism of injury for a distal radial fracture is usually a high energy traumatic incident, radiographs should be taken to confirm the diagnosis and ensure that the surrounding tissues are still intact. Other injuries causing radial sided pain may include [[Triangular Fibrocartilage Complex Injuries|TFCC tear or perforation]], [http://emedicine.medscape.com/article/1239331-overview Galeazzi fracture] (fracture to the distal 2/3 of the radius), [[Scaphoid Fracture|scaphoid fracture]], or radiocarpal ligament injury.<br> | ||
*'''Malunion''' - Distal radius malunion is the most common complication, affecting up to 17% of patients. Physical therapists may assess the effect of malunion to determine if surgery is appropriate by performing a detailed physical exam that includes a preoperative history, location and severity of pain, and functional loss.<ref name=":6" /> <ref name=":8" /> | *'''Malunion''' - Distal radius malunion is the most common complication, affecting up to 17% of patients. Physical therapists may assess the effect of malunion to determine if surgery is appropriate by performing a detailed physical exam that includes a preoperative history, location and severity of pain, and functional loss.<ref name=":6" /> <ref name=":8" /> | ||
*'''Compartment Syndrome''' - Incidence of this complication affects only 1% of patients. Elevate, observe, and loosen cast immediately if compartment syndrome is suspected.<ref name=":8" /> | *'''Compartment Syndrome''' - Incidence of this complication affects only 1% of patients. Elevate, observe, and loosen cast immediately if compartment syndrome is suspected.<ref name=":8" /> | ||
*'''[[Complex Regional Pain Syndrome (CRPS)]] '''- This complication is observed in 8-35% of patients.<ref name=":8" /> | *'''[[Complex Regional Pain Syndrome (CRPS)]] '''- This complication is observed in 8-35% of patients.<ref name=":8" /> CRPS should be suspected when pain, decreased ROM, skin temperature, color, and swelling are out of proportion to the injury. In order to obtain a good functional outcome for this patient population, early recognition and a multidisciplinary treatment approach to address pain and function requires psychiatric and physical/occupational therapy interventions. | ||
*'''[[Dupuytren’s Contracture|Dupuytren’s Disease]]''' - Patients develop mild contractures in the palm along the fourth and fifth rays within six months of a distal radial fracture. The severity of the contractures determines the treatment course.<ref name=":8" /> | *'''[[Dupuytren’s Contracture|Dupuytren’s Disease]]''' - Patients develop mild contractures in the palm along the fourth and fifth rays within six months of a distal radial fracture. The severity of the contractures determines the treatment course.<ref name=":8" /> | ||
*'''Nerve Pathology''' – Neuropathy may present acutely or throughout treatment. The median nerve is most common (4%), however 1% of patients have ulnar or radial involvement.<ref name=":2" /> | *'''Nerve Pathology''' – Neuropathy may present acutely or throughout treatment. The median nerve is most common (4%), however 1% of patients have ulnar or radial involvement.<ref name=":2" /> Physiotherapists may need to refer the patient to an orthopedic surgeon.<ref name=":8" /> | ||
*'''Acute Carpal Tunnel Syndrome''' – Physiotherapists must be able to identify acute carpal tunnel syndrome, as delayed treatment is associated with poor outcomes, incomplete recovery or a prolonged functional recovery time.<ref name=":2" /> <ref name=":8" /> | *'''Acute Carpal Tunnel Syndrome''' – Physiotherapists must be able to identify acute carpal tunnel syndrome, as delayed treatment is associated with poor outcomes, incomplete recovery or a prolonged functional recovery time.<ref name=":2" /> <ref name=":8" /> | ||
*'''Tendon Complications '''- Physiotherapists should be prepared to refer patients to surgery in the event of tendon complications secondary to irritation with inflammation or rupture from impingement.<ref name=":8" /> | *'''Tendon Complications '''- Physiotherapists should be prepared to refer patients to surgery in the event of tendon complications secondary to irritation with inflammation or rupture from impingement.<ref name=":8" /> | ||
*'''Capsule Contracture''' - Even after physical therapy treatment, some patients do not regain full forearm rotation due to contracture of the distal radioulnar joint capsule. Dorsal contracture limits pronation, volar contracture limits supination, and both may occur together. A DRUJ capsulectomy may be considered if functional ROM is not regained.<ref name=":7" /> | *'''Capsule Contracture''' - Even after physical therapy treatment, some patients do not regain full forearm rotation due to contracture of the distal radioulnar joint capsule. Dorsal contracture limits pronation, volar contracture limits supination, and both may occur together. A DRUJ capsulectomy may be considered if functional ROM is not regained.<ref name=":7" /> | ||
== Diagnostic procedures == | == Diagnostic procedures == | ||
| Line 108: | Line 108: | ||
*The classification should prescribe the treatment | *The classification should prescribe the treatment | ||
*The classification should suggest the long-term, functional results of treatment or be correlated with these anticipated results <ref name=":3" /> | *The classification should suggest the long-term, functional results of treatment or be correlated with these anticipated results <ref name=":3" /> | ||
== Outcome Measures == | == Outcome Measures == | ||
A '''Distal Radius Fracture Complication Checklist and Score Sheet''' was developed to improve prospective data collection.<ref>McKay SD, MacDermid JC, Roth JH, Richards Rs. “Assessment of complications of distal radius fractures and development of a complication checklist.” J. Hand Surg. Am., nr 5; 26, September 2001: 916-22.</ref> | A '''Distal Radius Fracture Complication Checklist and Score Sheet''' was developed to improve prospective data collection.<ref>McKay SD, MacDermid JC, Roth JH, Richards Rs. “Assessment of complications of distal radius fractures and development of a complication checklist.” J. Hand Surg. Am., nr 5; 26, September 2001: 916-22.</ref> The checklist includes a classification for all DRF complications, each of which is graded for severity (Mild = 1, Moderate = 2, Severe = 3). A total score is then calculated. The categories of the questionnaire are | ||
* nerve complications | * nerve complications | ||
* bone/joint complications | * bone/joint complications | ||
| Line 119: | Line 119: | ||
=== Self-Report Outcome Measures === | === Self-Report Outcome Measures === | ||
*[[Visual Analogue Scale|Visual Analogue Scale (VAS)]] to evaluate pain <ref name=":9">Walenkamp M., et al. Surgery versus conservative treatment in patients with type A distal radius fractures, a randomised controlled trial. BMC Musculoskeletal disorders 2014, 15:90.</ref> | *[[Visual Analogue Scale|Visual Analogue Scale (VAS)]] to evaluate pain <ref name=":9">Walenkamp M., et al. Surgery versus conservative treatment in patients with type A distal radius fractures, a randomised controlled trial. BMC Musculoskeletal disorders 2014, 15:90.</ref> | ||
*The [[DASH Outcome Measure|Disability of the Arm, Shoulder and Hand questionnaire (DASH)]] <ref name=":9" /> <ref name=":10">Leiv M. Hove, Lindau T, Holmer P. Distal radius fractures: current concepts. Berlin, Heidelberg- Springer (2014) pg. 53- 58</ref> | *The [[DASH Outcome Measure|Disability of the Arm, Shoulder and Hand questionnaire (DASH)]] <ref name=":9" /> <ref name=":10">Leiv M. Hove, Lindau T, Holmer P. Distal radius fractures: current concepts. Berlin, Heidelberg- Springer (2014) pg. 53- 58</ref> | ||
*The Gartland and Werley Score is an objective measurement to predict overall recovery. | *The Gartland and Werley Score is an objective measurement to predict overall recovery. | ||
*The [[PRWE Score|Patient-Rated Wrist Evaluation]] (PRWE) <ref name=":9" /> <ref name=":10" /> | *The [[PRWE Score|Patient-Rated Wrist Evaluation]] (PRWE) <ref name=":9" /> <ref name=":10" /> | ||
*The Michigan Hand Outcomes Questionnaire (MHQ) is a hand-specific outcome instrument divided in six scales: | *The Michigan Hand Outcomes Questionnaire (MHQ) is a hand-specific outcome instrument divided in six scales: | ||
# overall hand function | # overall hand function | ||
| Line 138: | Line 138: | ||
=== Physical Outcome Measures === | === Physical Outcome Measures === | ||
*ROM of the wrist with a goniometer <ref name=":9" /> | *ROM of the wrist with a goniometer <ref name=":9" /> | ||
*Grip Strength is an important outcome measure because it is an important function in daily activities. <ref name=":10" /> | *Grip Strength is an important outcome measure because it is an important function in daily activities. <ref name=":10" /> Grip strength can be measured with a dynamometer.<ref name=":9" /> | ||
== Examination == | == Examination == | ||
| Line 145: | Line 145: | ||
Physical therapists must conduct a thorough physical exam including subjective and objective information. | Physical therapists must conduct a thorough physical exam including subjective and objective information. | ||
*'''Subjective exam''' includes any information given by the patient about pain experienced, limitations of ROM of the wrist, and activity limitations.<ref name=":2" /> | *'''Subjective exam''' includes any information given by the patient about pain experienced, limitations of ROM of the wrist, and activity limitations.<ref name=":2" /> | ||
*'''Objective exam''' includes assessment of wrist and digit ROM, grip and forearm strength, bony and soft-tissue abnormalities, skin integrity, and nerve involvement.<ref name=":2" /> | *'''Objective exam''' includes assessment of wrist and digit ROM, grip and forearm strength, bony and soft-tissue abnormalities, skin integrity, and nerve involvement.<ref name=":2" /> Be aware that the contralateral extremity may be an unreliable control.<ref name=":10" /> | ||
<br>Health care professionals should always evaluate the ligamentous integrity in the presence of carpal instability and persistent pain as early as possible in order to avoid poor functional outcomes and prolonged recovery. Specific fracture patterns and high energy injuries are strongly indicative of intercarpal ligament involvement.<ref name=":7" /> | <br>Health care professionals should always evaluate the ligamentous integrity in the presence of carpal instability and persistent pain as early as possible in order to avoid poor functional outcomes and prolonged recovery. Specific fracture patterns and high energy injuries are strongly indicative of intercarpal ligament involvement.<ref name=":7" /> <br> | ||
To confirm the diagnosis, the doctor will ask for an x-ray. X-rays are the most common and broadly available diagnostic imaging technique. They can show if a bone is broken and whether there is displacement (gap between broken bones). In addition, they can also show how many pieces of broken bone there are.<ref name=":5" /> | To confirm the diagnosis, the doctor will ask for an x-ray. X-rays are the most common and broadly available diagnostic imaging technique. They can show if a bone is broken and whether there is displacement (gap between broken bones). In addition, they can also show how many pieces of broken bone there are.<ref name=":5" /> <br> | ||
== Medical Management (current best evidence) == | == Medical Management (current best evidence) == | ||
Orthopedic surgeons typically recommend surgical repair of displaced articular fractures of the distal radius for active, healthy people.<ref name=":13">Leone J, Bhandari M, Adili A, McKenzie S, Moro JK, Dunlop RB. Predictors of early and late instability following conservative treatment of exta-articular distal radius fractures. Arch Orthop Trauma Surg. 2004;124:38-41.</ref> | Orthopedic surgeons typically recommend surgical repair of displaced articular fractures of the distal radius for active, healthy people.<ref name=":13">Leone J, Bhandari M, Adili A, McKenzie S, Moro JK, Dunlop RB. Predictors of early and late instability following conservative treatment of exta-articular distal radius fractures. Arch Orthop Trauma Surg. 2004;124:38-41.</ref> The sheer variety of reduction and fixation options is noted based on a series of five Cochrane reviews focusing on this topic alone. Methods include: closed reduction and percutaneous pinning, either extra-focal or intra-focal; bridging external fixation with or without supplemental Kirschner-wire fixation; dorsal plating; fragment-specific fixation; open reduction and internal fixation with a volar plate through a classic Henry approach; or a combination of these methods.<ref name=":0" /> <ref name=":1" /> <ref name=":6" /> <ref name=":12" /> <ref name=":8" /> <ref name=":13" /> <ref name=":14">Herzberg G. Intra-articular fracture of the distal radius: arthroscopic-assisted reduction. J Hand Surg. 2010;35A:1517-1519.</ref> According to Bushnell and Bynum (2007), surgical “complications include edema, hematoma, stiffness, infection, neurovascular injury, loss of fixation, recurrent malunion, nonunion or delayed union, instability, tendon irritation or ruptures, osteoarthritis, residual ulnar-side pain, median neuropathy, complex regional pain syndrome, and problems with the bone-graft harvest site."<ref name=":6" /> | ||
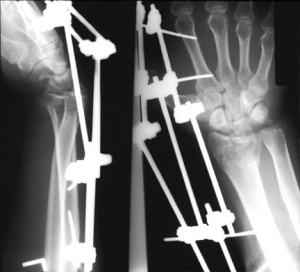
*'''External Fixation''' – External fixation is typically a cl[[Image:ExternalFixRadius.jpg|thumb|right|Figure 2. Radiographic image of external fixator.]]osed, minimally invasive method in which metal pins or screws are driven into the bone via small incisions in the skin. These pins can then be fixed externally by either a plaster cast or securing them into an external fixator frame.<ref name=":0" /> <ref name=":1" /> | *'''External Fixation''' – External fixation is typically a cl[[Image:ExternalFixRadius.jpg|thumb|right|Figure 2. Radiographic image of external fixator.]]osed, minimally invasive method in which metal pins or screws are driven into the bone via small incisions in the skin. These pins can then be fixed externally by either a plaster cast or securing them into an external fixator frame.<ref name=":0" /> <ref name=":1" /> In comparison to a standard immobilization procedure, external fixation of distal radius fractures reduces redisplacement and yields better anatomical results. However, current evidence for better functional outcomes from external fixation is weak and is also associated with high risk for complications such as pin site infections and radial nerve injuries. A radiographic example is shown in Figure 2. | ||
*[http://orthoinfo.aaos.org/topic.cfm?topic=A00196&return_link=0 '''Internal fixation'''] – Internal fixation involves open surgery where the fractured [[Image:Internalfixation plate.gif|thumb|right|Figure 3. Radiographic image of internal fixator plate.]]bone is exposed. Dorsal, volar or T-plates with screws may be used.<ref name=":6" /> | *[http://orthoinfo.aaos.org/topic.cfm?topic=A00196&return_link=0 '''Internal fixation'''] – Internal fixation involves open surgery where the fractured [[Image:Internalfixation plate.gif|thumb|right|Figure 3. Radiographic image of internal fixator plate.]]bone is exposed. Dorsal, volar or T-plates with screws may be used.<ref name=":6" /> However, due to the invasive and demanding nature of open surgery, there is an increased risk of infection and soft-tissue damage and therefore this type of fixation is usually reserved for more severe injuries.<ref name=":12" /> Figure 3 is a radiographic image of internal fixation. {{#ev:youtube|DmXkjliVLuk}} | ||
*'''[http://www.nlm.nih.gov/medlineplus/ency/article/002963.htm Bone Grafts]''' - Upon reduction of distal radial fractures, bony voids are common and can be reduced by inserting bone grafts or bone graft substitutes. Autogenous bone material obtained from the patient themselves or allogenous bone material obtained from cadaver or live donors can be used as filler for reducing bony voids.<ref>Handoll HHG, Huntley JS. Bone grafts and bone substitutes for treating distal radial fractures in adults (Review). The Cochrane Library. 2009;3:1-87.</ref> | *'''[http://www.nlm.nih.gov/medlineplus/ency/article/002963.htm Bone Grafts]''' - Upon reduction of distal radial fractures, bony voids are common and can be reduced by inserting bone grafts or bone graft substitutes. Autogenous bone material obtained from the patient themselves or allogenous bone material obtained from cadaver or live donors can be used as filler for reducing bony voids.<ref>Handoll HHG, Huntley JS. Bone grafts and bone substitutes for treating distal radial fractures in adults (Review). The Cochrane Library. 2009;3:1-87.</ref> However, current research describes risk of complications including infection, nerve injury, or donor site pain, and limited evidence that bone scaffolding may improve anatomical or functional outcomes.<ref name=":15">Handoll HHG, Watts AC. Internal fixation and comparisons of different fixation methods for treating distal radial fractures in adults (Protocol). The Cochrane Library. 2008;4:1-14.</ref> Bone grafting is required by most procedures except closing wed[[Image:Percutaneous pinning xray image free.jpg|thumb|right|Figure 4: Percutaneous pinning radiograph.]]ge.<ref name=":6" /> <br> | ||
*'''Percutaneous Pinning''' - Another strategy in reducing and stabilizing the fractures is percutaneous pinning, which involves insertion of pins, threads or wires through the skin and into the bone.<ref name=":6" /> <ref name=":14" /> | *'''Percutaneous Pinning''' - Another strategy in reducing and stabilizing the fractures is percutaneous pinning, which involves insertion of pins, threads or wires through the skin and into the bone.<ref name=":6" /> <ref name=":14" /> This procedure is typically less invasive and reduction of the fracture is closed upon which the pins placed in the bone are used to fix the distal radial fragment. Current indications for the best technique of pinning, the extent and duration of immobilization are uncertain, in which the excess of complications are likely to outweigh therapeutic benefits of pinning. Figure 4 is a radiograph of pinning. <br> | ||
* '''Closed Reduction''' - In closed reduction, displaced radial fragments are repositioned using different maneuvers while the arm is in traction. Different methods include manual reduction in which two people pull in the opposite directions to produce and maintain longitudinal traction and mechanical methods of reduction including the use of “finger traps.” However there is insufficient evidence establishing the effectiveness of different methods of closed reduction used in treating distal radial fractures.<ref name=":8" /> | * '''Closed Reduction''' - In closed reduction, displaced radial fragments are repositioned using different maneuvers while the arm is in traction. Different methods include manual reduction in which two people pull in the opposite directions to produce and maintain longitudinal traction and mechanical methods of reduction including the use of “finger traps.” However there is insufficient evidence establishing the effectiveness of different methods of closed reduction used in treating distal radial fractures.<ref name=":8" /> | ||
*Arthroscopic-assisted reduction has many advantages over open reduction. In addition to being less invasive, arthroscopic-assisted reduction allows for direct visualization and reduction of articular displacement, opportunity to diagnose and treat associated ligamentous injuries, removal of articular cartilage debris, and lavage of radiocarpal joint. The primary limitations for arthroscopic reduction are due the limited number of surgeons with experience, a longer, more difficult procedure, and the potential for compartment syndrome or acute carpal tunnel syndrome with fluid extravasation.<ref name=":13" /> <sup> | *Arthroscopic-assisted reduction has many advantages over open reduction. In addition to being less invasive, arthroscopic-assisted reduction allows for direct visualization and reduction of articular displacement, opportunity to diagnose and treat associated ligamentous injuries, removal of articular cartilage debris, and lavage of radiocarpal joint. The primary limitations for arthroscopic reduction are due the limited number of surgeons with experience, a longer, more difficult procedure, and the potential for compartment syndrome or acute carpal tunnel syndrome with fluid extravasation.<ref name=":13" /> <sup><br></sup> | ||
== Physical Therapy Management (current best evidence) == | == Physical Therapy Management (current best evidence) == | ||
Current physical therapy management for distal radius fractures covers post-surgical or post-immobilization treatment.<ref name=":11" /> | Current physical therapy management for distal radius fractures covers post-surgical or post-immobilization treatment.<ref name=":11" /> The treatment of distal radius fractures is controversial and further research is required. There is a great need of versatility in the treatment options and there is no gold standard of treatment. The best treatment option must be decided in accordance to the type of fracture evaluated from the radiographs after temporary reduction. <br>Two third of all dorsal radius fractures are relocated and are especially extra articular. Surgical treatment is used when the fracture re- displacement occurs. It contains surgical reduction and fixation with a volar locking plate or in the other case (people with displaced extra-articular DRF’s)<br>We list the possible treatments on.<br><u>Treatmen</u>t<br>There is one basic rule with broken bones, broken pieces must be prevented from moving out of place. There are several treatment positions for distal radial fracture, the choice depends on: | ||
*Nature of fracture | *Nature of fracture | ||
*Age | *Age | ||
*Activity level | *Activity level | ||
*And the surgeon’s personal preferences <ref name=":5" /> | *And the surgeon’s personal preferences <ref name=":5" /> | ||
<u>Non-surgical Treatment</u><br>When the broken bone is in a good position you can apply a plaster until the bone heals. | <u>Non-surgical Treatment</u><br>When the broken bone is in a good position you can apply a plaster until the bone heals. | ||
| Line 176: | Line 176: | ||
<br>If the bone is not in a good position, then it may be necessary to realign the broken bone fragments. The doctor will remove the broken pieces into their original place. This action or act is called the 'reduction’. But when a bone is straightened without making an incision to open the skin, they call it a closed reduction. | <br>If the bone is not in a good position, then it may be necessary to realign the broken bone fragments. The doctor will remove the broken pieces into their original place. This action or act is called the 'reduction’. But when a bone is straightened without making an incision to open the skin, they call it a closed reduction. | ||
<br>After the bone is aligned, a splint or cast may be placed and will be removed about 6 weeks after the fracture happened (they change the cast after 2 to 3 weeks when the swelling goes down otherwise it will be too big). After this, physical therapy will be started to improve the function of the injured wrist.<ref name=":5" /> | <br>After the bone is aligned, a splint or cast may be placed and will be removed about 6 weeks after the fracture happened (they change the cast after 2 to 3 weeks when the swelling goes down otherwise it will be too big). After this, physical therapy will be started to improve the function of the injured wrist.<ref name=":5" /> | ||
<br><u>Surgical Treatment</u><br>Now and then the position of the bone is so much out of place that surgery may be required. <br>Procedure: they making an incision to directly access the broken bones to improve alignment (open reduction). | <br><u>Surgical Treatment</u><br>Now and then the position of the bone is so much out of place that surgery may be required. <br>Procedure: they making an incision to directly access the broken bones to improve alignment (open reduction). | ||
| Line 187: | Line 187: | ||
*Metal pins (usually stainless steel or titanium) | *Metal pins (usually stainless steel or titanium) | ||
*Plate and screws | *Plate and screws | ||
*External fixator (a a stabilizing frame outside the body that holds the bones in the proper position so they can heal)<ref name=":5" /> | *External fixator (a a stabilizing frame outside the body that holds the bones in the proper position so they can heal)<ref name=":5" /> | ||
<u>Recovery</u><br>Because the kinds of distal radius fractures are so varied and the treatment options are so broad, recovery is different for each individual. Talk to your doctor for specific information about your recovery program and return to daily activities.<ref name=":5" /> <br> | |||
<br><u>Pain Management</u><br>Most fractures hurt for a few days to a couple of weeks. Many patients find that using ice, elevation and simple, non-prescription medications for pain relief are all that are needed to relieve pain.<ref name=":5" /> | |||
<br><u>Pain Management</u><br>Most fractures hurt for a few days to a couple of weeks. Many patients find that using ice, elevation and simple, non-prescription medications for pain relief are all that are needed to relieve pain.<ref name=":5" /> | |||
| Line 213: | Line 211: | ||
*Preferred modalities after immobilization: | *Preferred modalities after immobilization: | ||
Heat/ cold modalities > ultrasound > electrical stimulation/ CPM > EMG/biofeedback <ref>Michlovitz S., et al. “Distal Radius Fractures: Therapy Practice Patterns” J Hand Ther. 14, (2001): 249-257.</ref> | Heat/ cold modalities > ultrasound > electrical stimulation/ CPM > EMG/biofeedback <ref>Michlovitz S., et al. “Distal Radius Fractures: Therapy Practice Patterns” J Hand Ther. 14, (2001): 249-257.</ref> | ||
<br>It has been proven that an advice- and exercise program provides some additional benefits over no intervention for adults following a distal radius fracture. Especially pain and activity limitations had better outcome measures.<ref>Kay S, McMahon M, Stiller K. An advice and exercise program has some benefits over natural recovery after distal radius fracture. Australian Journal of Physiotherapy. 2008. 54: 253-259.</ref> | <br>It has been proven that an advice- and exercise program provides some additional benefits over no intervention for adults following a distal radius fracture. Especially pain and activity limitations had better outcome measures.<ref>Kay S, McMahon M, Stiller K. An advice and exercise program has some benefits over natural recovery after distal radius fracture. Australian Journal of Physiotherapy. 2008. 54: 253-259.</ref> | ||
<br>The Functional outcome following is as follows : closed reduction and plaster immobilization <ref name=":9" /> | <br>The Functional outcome following is as follows: closed reduction and plaster immobilization <ref name=":9" /> | ||
<br><u>Advice</u><br>Use of self- management approach developing positive health behaviors during rehabilitation. <br>Self- Management programs can provide benefits in participants’ knowledge, symptom management, self- management behaviours, self- efficacy and aspects of health status. <br>These programs are usually given to patients with chronic illnesses.<ref>Bruder A, Taylor N, Dodd K, Shields N. Physiotherapy intervention practice patterns used in rehabilitation after distal radius fracture. Physiotherapy. 2013. 99: 233-240.</ref> | <br><u>Advice</u><br>Use of self- management approach developing positive health behaviors during rehabilitation. <br>Self- Management programs can provide benefits in participants’ knowledge, symptom management, self- management behaviours, self- efficacy and aspects of health status. <br>These programs are usually given to patients with chronic illnesses.<ref>Bruder A, Taylor N, Dodd K, Shields N. Physiotherapy intervention practice patterns used in rehabilitation after distal radius fracture. Physiotherapy. 2013. 99: 233-240.</ref> | ||
This table below shows some details of a recommended physical therapy treatment for the first twelve weeks following fracture reduction.<ref>Brotzman BS, Wilk KE. Handbook of Orthopaedic Rehabilitation, 2nd ed. Philadelphia: Mosby. 2007. | This table below shows some details of a recommended physical therapy treatment for the first twelve weeks following fracture reduction.<ref>Brotzman BS, Wilk KE. Handbook of Orthopaedic Rehabilitation, 2nd ed. Philadelphia: Mosby. 2007. | ||
</ref> | </ref> | ||
During the first two months, patients report severe pain during movement and severe disability during activities of daily living as assessed with valid and reliable outcome measures such as the Patient Rated Wrist Evaluation (PRWE) and the Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH).<ref name=":16">MacDermid JC, Roth JH, Richards RS. Pain and disability reported in the year following a distal radius fracture: A cohort study. BMC Musculoskelet Disord. 2003;4:24-36.</ref> | During the first two months, patients report severe pain during movement and severe disability during activities of daily living as assessed with valid and reliable outcome measures such as the Patient Rated Wrist Evaluation (PRWE) and the Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH).<ref name=":16">MacDermid JC, Roth JH, Richards RS. Pain and disability reported in the year following a distal radius fracture: A cohort study. BMC Musculoskelet Disord. 2003;4:24-36.</ref> These deficits are reflected in decreased range of motion and decreased grip strength measurements with strength being more highly correlated with functional ability. However, most patients achieve the majority of recovery within the first six months. A small minority of patients will experience persistent pain and disability at one year post injury regardless of treatment protocol,<ref name=":2" /> <ref name=":16" /> <ref>Moore CM, Leonardi-Bee J. The prevalence of pain and disability one year post fracture of the distal radius in a UK population: A cross sectional survey. BMC Musculoskeletl Disord. 2008;9:129-138.</ref> especially when pushing up from sit to stand and carrying weight. Patients expressing atypical recovery from distal radial fractures need modified treatment programs with goals toward increasing workability.<br><br> | ||
== Key Research == | == Key Research == | ||
Handoll et al conducted eight Cochrane Reviews targeting distal radial fractures. There was insufficient data from which to draw conclusions. This may be due to poor study design and the heterogeneity of distal radial fractures themselves.<br>• Different methods of external fixation for treating distal radial fractures in adults <ref name=":1" /> | Handoll et al conducted eight Cochrane Reviews targeting distal radial fractures. There was insufficient data from which to draw conclusions. This may be due to poor study design and the heterogeneity of distal radial fractures themselves.<br>• Different methods of external fixation for treating distal radial fractures in adults <ref name=":1" /> <sup><br></sup>• External Fixation versus conservative treatment for distal radial fractures in adults <ref name=":0" /> <sup><br></sup>• Internal fixation and comparisons of different fixation methods for treating distal radial fractures in adults <ref name=":12" /> <sup><br></sup>• Closed reduction methods for treating distal radial fractures in adults <ref name=":8" /> <sup><br></sup>• Percutaneous pinning for treating distal radial fractures in adults <ref name=":14" /> <sup><br></sup>• Bone grafts and bone substitutes for treating distal radial fractures in adults <ref name=":15" /> <sup><br></sup>• Conservative interventions for treating distal radial fractures in adults <ref>Handoll HHG, Huntley JS, Madhok R. Closed reduction methods for treating distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-29. | ||
</ref> <sup> | </ref> <sup><br></sup>• Rehabilitation for distal radial fractures in adults <ref>Handoll HHG, Vaghela MV, Madhok R. Percutaneous pinning for treating distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-70. | ||
</ref> | </ref> | ||
In a randomized control trial, Kay et al (2008) were supportive of physical therapy intervention, although limitations in the study abound.<ref name=":11" /> While no significant differences in grip strength and wrist extension were found in the experimental group, it is important to note that some of the secondary measures showed significant improvement as compared to the control group. These include benefits in activity, pain | In a randomized control trial, Kay et al (2008) were supportive of physical therapy intervention, although limitations in the study abound.<ref name=":11" /> While no significant differences in grip strength and wrist extension were found in the experimental group, it is important to note that some of the secondary measures showed significant improvement as compared to the control group. These include benefits in activity, pain and satisfaction.<br> | ||
== Resources<br> == | == Resources<br> == | ||
Revision as of 03:50, 25 October 2017
Original Editors - Diane Hodges Popps
Top Contributors - Laura Ritchie, Diane Hodges Popps, Jocelyn Fu, Kim Jackson, Admin, Katherine Knight, Nupur Smit Shah, Ulrike Lambrix, Jess Bell, Evan Thomas, WikiSysop, Karen Wilson, Lauren Lopez, Tony Lowe, Jorge Rodríguez Palomino, Felicia Daigle, Jeremy Brady, Elien Lebuf and Tarina van der Stockt
Definition/Description[edit | edit source]
The radius is the larger of the two bones of the forearm, located radially. The distal end of the radius is considered as the three centimeters proximal to the radiocarpal joint, where the radius interfaces with the lunate and scaphoid bone of the wrist. A fracture of the distal radius can be caused by falling on the outstretched arm. [1] The majority of distal radial fractures are closed injuries in which the overlying skin remains intact.[2] [3] The radius is the most commonly broken bone in the arm.
For centuries they called this fracture a dislocation of the wrist but this description remains obscure. It was redefined by an Irish surgeon and anatomist, Abraham Colles, in 1814. Subsequently, the name of this injury was changed to a Colles fracture and the name continues to be used by surgeons.[4]
Clinically Relevant Anatomy[edit | edit source]
The wrist joint (also known as the radiocarpal joint) is a synovial joint in the upper limb, marking the area of transition between the forearm and the hand.
The wrist joint is formed distally by the proximal row of carpal bones (except the pisiform);
- os scaphoid
- os lunate
- os triquete
The wrist joint is formed proximally by the distal end of the radius and the articular disk (see below).
Multiplanar wrist motion is based on three articulations:
- radioscaphoid
- radiolunate
- distal radioulnar joints
The ulna is not part of the wrist joint – it articulates with the radius in two locations, the superior and the inferior radio-ulnar joint. Eighty percent of axial load is supported by the distal radius and 20% by the ulna. It is prevented from articulating with the carpal bones by a fibrocartilginous ligament, called the articular disk, which lies over the superior surface of the ulna.
Together, the carpal bones form a convex surface which articulates with the concave surface of the radius and articular disk. All the carpal joints are art sellaris (the concave part) and the radius the convex part of the joint is seen as an art sphaeroidea.
There are several known ligamentous attachments to the distal radius. These often remain intact during distal radius fractures. The volar ligaments are stronger and give more stability to the radiocarpal articulation than the dorsal ligaments.[5]
Epidemiology /Etiology[edit | edit source]
Distal radial fractures is one of the most common fractures of the upper extremity in adults, accounting for one-sixth of all fractures in the emergency department. It is seen predominantly in the older caucasian population.[2] [3] [6] [7] [8] There is typically a history of a fall or similar trauma to the upper extremity. Pain and swelling in the forearm or wrist are common. Bruising and deformity in the wrist or forearm are also possible.[9]
In women, the incidence of occurrence increases with age starting at 40 years old, whereas before this age the incidence in men is much higher. Occurrences in younger adults are usually the result of a high-energy trauma such as a motor vehicle accident, fall from height or athletic participation.[10] In older adults, such fractures are often the result of a low-energy or moderate trauma such as falling from standing height. This may reflect the greater fragility of the bone due to osteoporosis in the older adult.[2] [11]
Characteristics/Clinical Presentation[edit | edit source]
Distal radial fractures can be classified based on their clinical appearance and typical deformity. Dorsal displacement, dorsal angulation, dorsal comminution and radial shortening may all be used to describe the presentation of the fracture. Classification based on fracture patterns such as intra-articular (articular surfaces disrupted) or extra-articular (articular surface of radius intact) may also be used.[2] [12]
1. Classification of intra-articular fracture
- Type Ι: stable, without comminution
- Type ΙΙ: unstable die-punch, dorsal of volar
- ΙΙa: reducible
- ΙΙb: irreducible
- Type ΙΙΙ: spike fracture; contuses volar structures
- Type ΙV: split fracture : medial complex fractured with dorsal and palmar fragments displaced separately
- Type V: explosion fracture; severe communication with major soft-tissue injury
2. Classification of extra-articular fracture
- Type A: extra-articular
- Type A1: extra-articular ulna, radius intact
- Type A2: extra-articular radius, ulna intact
- Type A3: extra-articular, multi fragmentary radius fracture [13]
Types of Fractures[edit | edit source]
Colles Fracture[edit | edit source]
This is typically due to a fall on an outstretched hand and results in a dorsal extra-articular or intra-articular displacement of the fractured radius:
- Intra-articular fractures are generally seen in the younger age group secondary to higher energy forces
- More than 90% of distal radius fractures are of this pattern [13]
Smith's Fracture[edit | edit source]
This is a reverse Colles with a volar displacement and a fall on a flexed wrist with forearm fixed in supination [13]
Barton's Fracture[edit | edit source]
This is an intra-articular fracture with subluxation or dislocation of the carpus bone. Of the eight grades for distal radial fractures in the Frykman Classification system, half include ulnar styloid involvement.
Complications are common and diverse. They may be the result of injury or treatment and are associated with poorer outcomes. These can include:[14]
- upper extremity stiffness
- carpal tunnel syndrome or medial nerve involvement
- malunion
- carpal instability
- DRUJ dysfunction
- Dupuytren's disease
- radiocarpal arthritis
- tendon/ligament injuries
- post-traumatic osteoarthritis
- compartment syndrome
- infection (mostly by open fractures) [13] [14]
- complex regional pain syndrome [7] [15] [16] [17]
Differential Diagnosis[edit | edit source]
Because the mechanism of injury for a distal radial fracture is usually a high energy traumatic incident, radiographs should be taken to confirm the diagnosis and ensure that the surrounding tissues are still intact. Other injuries causing radial sided pain may include TFCC tear or perforation, Galeazzi fracture (fracture to the distal 2/3 of the radius), scaphoid fracture, or radiocarpal ligament injury.
- Malunion - Distal radius malunion is the most common complication, affecting up to 17% of patients. Physical therapists may assess the effect of malunion to determine if surgery is appropriate by performing a detailed physical exam that includes a preoperative history, location and severity of pain, and functional loss.[12] [17]
- Compartment Syndrome - Incidence of this complication affects only 1% of patients. Elevate, observe, and loosen cast immediately if compartment syndrome is suspected.[17]
- Complex Regional Pain Syndrome (CRPS) - This complication is observed in 8-35% of patients.[17] CRPS should be suspected when pain, decreased ROM, skin temperature, color, and swelling are out of proportion to the injury. In order to obtain a good functional outcome for this patient population, early recognition and a multidisciplinary treatment approach to address pain and function requires psychiatric and physical/occupational therapy interventions.
- Dupuytren’s Disease - Patients develop mild contractures in the palm along the fourth and fifth rays within six months of a distal radial fracture. The severity of the contractures determines the treatment course.[17]
- Nerve Pathology – Neuropathy may present acutely or throughout treatment. The median nerve is most common (4%), however 1% of patients have ulnar or radial involvement.[7] Physiotherapists may need to refer the patient to an orthopedic surgeon.[17]
- Acute Carpal Tunnel Syndrome – Physiotherapists must be able to identify acute carpal tunnel syndrome, as delayed treatment is associated with poor outcomes, incomplete recovery or a prolonged functional recovery time.[7] [17]
- Tendon Complications - Physiotherapists should be prepared to refer patients to surgery in the event of tendon complications secondary to irritation with inflammation or rupture from impingement.[17]
- Capsule Contracture - Even after physical therapy treatment, some patients do not regain full forearm rotation due to contracture of the distal radioulnar joint capsule. Dorsal contracture limits pronation, volar contracture limits supination, and both may occur together. A DRUJ capsulectomy may be considered if functional ROM is not regained.[15]
Diagnostic procedures[edit | edit source]
Radiographic parameters are used to check the normal anatomy and to detect anatomical anomalies.
There are many classification systems that describe fractures of the distal radius. Classification systems should follow the following two principles:
- The classification should prescribe the treatment
- The classification should suggest the long-term, functional results of treatment or be correlated with these anticipated results [13]
Outcome Measures[edit | edit source]
A Distal Radius Fracture Complication Checklist and Score Sheet was developed to improve prospective data collection.[18] The checklist includes a classification for all DRF complications, each of which is graded for severity (Mild = 1, Moderate = 2, Severe = 3). A total score is then calculated. The categories of the questionnaire are
- nerve complications
- bone/joint complications
- tendon complications
Self-Report Outcome Measures[edit | edit source]
- Visual Analogue Scale (VAS) to evaluate pain [19]
- The Disability of the Arm, Shoulder and Hand questionnaire (DASH) [19] [20]
- The Gartland and Werley Score is an objective measurement to predict overall recovery.
- The Patient-Rated Wrist Evaluation (PRWE) [19] [20]
- The Michigan Hand Outcomes Questionnaire (MHQ) is a hand-specific outcome instrument divided in six scales:
- overall hand function
- activities of daily living
- pain
- work performance
- aesthetics
- patient satisfaction with hand function
Disease-Specific Outcome Measures[edit | edit source]
- Boston Carpal Tunnel Questionnaire
- Health Assessment Questionnaire (HAQ)
- The Arthritis Impact Measurement Scale (AIMS)
- Australian/Canadian Osteoarthritis Hand Index
Physical Outcome Measures[edit | edit source]
- ROM of the wrist with a goniometer [19]
- Grip Strength is an important outcome measure because it is an important function in daily activities. [20] Grip strength can be measured with a dynamometer.[19]
Examination[edit | edit source]
Physical therapists must conduct a thorough physical exam including subjective and objective information.
- Subjective exam includes any information given by the patient about pain experienced, limitations of ROM of the wrist, and activity limitations.[7]
- Objective exam includes assessment of wrist and digit ROM, grip and forearm strength, bony and soft-tissue abnormalities, skin integrity, and nerve involvement.[7] Be aware that the contralateral extremity may be an unreliable control.[20]
Health care professionals should always evaluate the ligamentous integrity in the presence of carpal instability and persistent pain as early as possible in order to avoid poor functional outcomes and prolonged recovery. Specific fracture patterns and high energy injuries are strongly indicative of intercarpal ligament involvement.[15]
To confirm the diagnosis, the doctor will ask for an x-ray. X-rays are the most common and broadly available diagnostic imaging technique. They can show if a bone is broken and whether there is displacement (gap between broken bones). In addition, they can also show how many pieces of broken bone there are.[1]
Medical Management (current best evidence)[edit | edit source]
Orthopedic surgeons typically recommend surgical repair of displaced articular fractures of the distal radius for active, healthy people.[21] The sheer variety of reduction and fixation options is noted based on a series of five Cochrane reviews focusing on this topic alone. Methods include: closed reduction and percutaneous pinning, either extra-focal or intra-focal; bridging external fixation with or without supplemental Kirschner-wire fixation; dorsal plating; fragment-specific fixation; open reduction and internal fixation with a volar plate through a classic Henry approach; or a combination of these methods.[2] [3] [12] [16] [17] [21] [22] According to Bushnell and Bynum (2007), surgical “complications include edema, hematoma, stiffness, infection, neurovascular injury, loss of fixation, recurrent malunion, nonunion or delayed union, instability, tendon irritation or ruptures, osteoarthritis, residual ulnar-side pain, median neuropathy, complex regional pain syndrome, and problems with the bone-graft harvest site."[12]
- External Fixation – External fixation is typically a closed, minimally invasive method in which metal pins or screws are driven into the bone via small incisions in the skin. These pins can then be fixed externally by either a plaster cast or securing them into an external fixator frame.[2] [3] In comparison to a standard immobilization procedure, external fixation of distal radius fractures reduces redisplacement and yields better anatomical results. However, current evidence for better functional outcomes from external fixation is weak and is also associated with high risk for complications such as pin site infections and radial nerve injuries. A radiographic example is shown in Figure 2.
- Internal fixation – Internal fixation involves open surgery where the fractured bone is exposed. Dorsal, volar or T-plates with screws may be used.[12] However, due to the invasive and demanding nature of open surgery, there is an increased risk of infection and soft-tissue damage and therefore this type of fixation is usually reserved for more severe injuries.[16] Figure 3 is a radiographic image of internal fixation.
- Bone Grafts - Upon reduction of distal radial fractures, bony voids are common and can be reduced by inserting bone grafts or bone graft substitutes. Autogenous bone material obtained from the patient themselves or allogenous bone material obtained from cadaver or live donors can be used as filler for reducing bony voids.[23] However, current research describes risk of complications including infection, nerve injury, or donor site pain, and limited evidence that bone scaffolding may improve anatomical or functional outcomes.[24] Bone grafting is required by most procedures except closing wedge.[12]
- Percutaneous Pinning - Another strategy in reducing and stabilizing the fractures is percutaneous pinning, which involves insertion of pins, threads or wires through the skin and into the bone.[12] [22] This procedure is typically less invasive and reduction of the fracture is closed upon which the pins placed in the bone are used to fix the distal radial fragment. Current indications for the best technique of pinning, the extent and duration of immobilization are uncertain, in which the excess of complications are likely to outweigh therapeutic benefits of pinning. Figure 4 is a radiograph of pinning.
- Closed Reduction - In closed reduction, displaced radial fragments are repositioned using different maneuvers while the arm is in traction. Different methods include manual reduction in which two people pull in the opposite directions to produce and maintain longitudinal traction and mechanical methods of reduction including the use of “finger traps.” However there is insufficient evidence establishing the effectiveness of different methods of closed reduction used in treating distal radial fractures.[17]
- Arthroscopic-assisted reduction has many advantages over open reduction. In addition to being less invasive, arthroscopic-assisted reduction allows for direct visualization and reduction of articular displacement, opportunity to diagnose and treat associated ligamentous injuries, removal of articular cartilage debris, and lavage of radiocarpal joint. The primary limitations for arthroscopic reduction are due the limited number of surgeons with experience, a longer, more difficult procedure, and the potential for compartment syndrome or acute carpal tunnel syndrome with fluid extravasation.[21]
Physical Therapy Management (current best evidence)[edit | edit source]
Current physical therapy management for distal radius fractures covers post-surgical or post-immobilization treatment.[8] The treatment of distal radius fractures is controversial and further research is required. There is a great need of versatility in the treatment options and there is no gold standard of treatment. The best treatment option must be decided in accordance to the type of fracture evaluated from the radiographs after temporary reduction.
Two third of all dorsal radius fractures are relocated and are especially extra articular. Surgical treatment is used when the fracture re- displacement occurs. It contains surgical reduction and fixation with a volar locking plate or in the other case (people with displaced extra-articular DRF’s)
We list the possible treatments on.
Treatment
There is one basic rule with broken bones, broken pieces must be prevented from moving out of place. There are several treatment positions for distal radial fracture, the choice depends on:
- Nature of fracture
- Age
- Activity level
- And the surgeon’s personal preferences [1]
Non-surgical Treatment
When the broken bone is in a good position you can apply a plaster until the bone heals.
If the bone is not in a good position, then it may be necessary to realign the broken bone fragments. The doctor will remove the broken pieces into their original place. This action or act is called the 'reduction’. But when a bone is straightened without making an incision to open the skin, they call it a closed reduction.
After the bone is aligned, a splint or cast may be placed and will be removed about 6 weeks after the fracture happened (they change the cast after 2 to 3 weeks when the swelling goes down otherwise it will be too big). After this, physical therapy will be started to improve the function of the injured wrist.[1]
Surgical Treatment
Now and then the position of the bone is so much out of place that surgery may be required.
Procedure: they making an incision to directly access the broken bones to improve alignment (open reduction).
Depending on the fracture, there are several of options for holding the bone in the correct position while it heals:
- Cast
- Metal pins (usually stainless steel or titanium)
- Plate and screws
- External fixator (a a stabilizing frame outside the body that holds the bones in the proper position so they can heal)[1]
Recovery
Because the kinds of distal radius fractures are so varied and the treatment options are so broad, recovery is different for each individual. Talk to your doctor for specific information about your recovery program and return to daily activities.[1]
Pain Management
Most fractures hurt for a few days to a couple of weeks. Many patients find that using ice, elevation and simple, non-prescription medications for pain relief are all that are needed to relieve pain.[1]
Rehabilitation
We have compared several treatments with each other and found different grades of effectiveness.
- During immobilization:
ROM exercises> compressive wrap> dexterity exercises> resting splints > soft tissue mobilization > joint mobilization > dynamic splints
- Preferred modalities during immobilization:
Heat/cold modalities> ; at less than 10% of the treatments ;
ultrasound > electrical stimulation> CPM (continuous passive motion) > EMG/ biofeedback
- After immobilization:
ROM exercises > compressive wrap/ dexterity exercises/ joint mobilization> soft tissue mobilization > dynamic splints > resting splints
- Preferred modalities after immobilization:
Heat/ cold modalities > ultrasound > electrical stimulation/ CPM > EMG/biofeedback [25]
It has been proven that an advice- and exercise program provides some additional benefits over no intervention for adults following a distal radius fracture. Especially pain and activity limitations had better outcome measures.[26]
The Functional outcome following is as follows: closed reduction and plaster immobilization [19]
Advice
Use of self- management approach developing positive health behaviors during rehabilitation.
Self- Management programs can provide benefits in participants’ knowledge, symptom management, self- management behaviours, self- efficacy and aspects of health status.
These programs are usually given to patients with chronic illnesses.[27]
This table below shows some details of a recommended physical therapy treatment for the first twelve weeks following fracture reduction.[28]
During the first two months, patients report severe pain during movement and severe disability during activities of daily living as assessed with valid and reliable outcome measures such as the Patient Rated Wrist Evaluation (PRWE) and the Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH).[29] These deficits are reflected in decreased range of motion and decreased grip strength measurements with strength being more highly correlated with functional ability. However, most patients achieve the majority of recovery within the first six months. A small minority of patients will experience persistent pain and disability at one year post injury regardless of treatment protocol,[7] [29] [30] especially when pushing up from sit to stand and carrying weight. Patients expressing atypical recovery from distal radial fractures need modified treatment programs with goals toward increasing workability.
Key Research[edit | edit source]
Handoll et al conducted eight Cochrane Reviews targeting distal radial fractures. There was insufficient data from which to draw conclusions. This may be due to poor study design and the heterogeneity of distal radial fractures themselves.
• Different methods of external fixation for treating distal radial fractures in adults [3]
• External Fixation versus conservative treatment for distal radial fractures in adults [2]
• Internal fixation and comparisons of different fixation methods for treating distal radial fractures in adults [16]
• Closed reduction methods for treating distal radial fractures in adults [17]
• Percutaneous pinning for treating distal radial fractures in adults [22]
• Bone grafts and bone substitutes for treating distal radial fractures in adults [24]
• Conservative interventions for treating distal radial fractures in adults [31]
• Rehabilitation for distal radial fractures in adults [32]
In a randomized control trial, Kay et al (2008) were supportive of physical therapy intervention, although limitations in the study abound.[8] While no significant differences in grip strength and wrist extension were found in the experimental group, it is important to note that some of the secondary measures showed significant improvement as compared to the control group. These include benefits in activity, pain and satisfaction.
Resources
[edit | edit source]
Clinical Bottom Line[edit | edit source]
Due to the fact that distal radial fractures are one of the most common injuries in orthopedics, it is important for physical therapists to understand the risk factors and treatment options. Although further research is needed to ascertain proper post surgical management, it is recommended based on current evidence that patients should be routinely referred to a physical therapist for education and an exercise program.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 American Academy of Orthopaedic Surgeons. Distal Radius Fractures [Internet]. Rosemont Illinois: American Academy of Orthopaedic Surgeons; 2013 [cited 2017 Oct 19]. Available from: http://orthoinfo.aaos.org/topic.cfm?topic=a00412
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Handoll HHG, Huntley JS, Madhok R. External Fixation versus conservative treatment for distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-78.
- ↑ 3.0 3.1 3.2 3.3 3.4 Handoll HHG, Huntley JS, Madhok R. Different methods of external fixation for treating distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-67.
- ↑ Benjamin JA. 1965. Abraham Colles (1773–1843) Distinguished surgeon from Ireland. Invest Urol 3:321–323
- ↑ Kenneth J. Koval, Joseph D. Zuckerman, Handbook of fractures, Philadelphia, second edition, 1994, pg 134.
- ↑ Abramo A, Kopylov P, Tagil M. Evaluation of a treatment protocol in distal radius fractures: a prospective study in 581 patients using DASH as outcome. Acta Orthopaedica. 2008;79(3):376-385
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Bienek T, Kusz D, Cielinski L. Peripheral nerve compression neuropathy after fractures of the distal radius. J Hand Surg. (British and European Volume). 2006;31B(3):256-260.
- ↑ 8.0 8.1 8.2 Kay S, McMahon M, Stiller K. An advice and exercise program has some benefits over natural recovery after distal radius fracture: a randomized trial. Aust J Physiother. 2008;54:253-259.
- ↑ Nelson DL. Wrist Fracture [Internet]. Greenbrae California: David Nelson MD; 2012 [cited 2017 Oct 19]. Available from: http://www.davidlnelson.md/articles/Wrist_Fracture.htm
- ↑ Kenneth J. Koval, Joseph D. Zuckerman, Handbook of fractures, Philadelphia, second edition, 1994, pg 134-135
- ↑ Leung F, Ozkan M, Chow SP. Conservative treatment of intra-articular fractures of the distal radius – factors affecting functional outcomes. Hand Surg. 2000;5(2):145-153.
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 12.6 Bushnell BD, Bynum DK. Malunion of the distal radius. J Am Acad Orthop Surg. 2007;15:27-40.
- ↑ 13.0 13.1 13.2 13.3 13.4 Kenneth J. Koval, Joseph D. Zuckerman, Handbook of fractures, Philadelphia, second edition, 1994, pg 135-138
- ↑ 14.0 14.1 Oren T, Wolf J. Soft- Tissue complications associated with distal radius fractures. Operative Techniques in Orthopaedics.19; 2009: 100—106.
- ↑ 15.0 15.1 15.2 Kleinman WB. Distal radius instability and stiffness; common complications of distal radius fractures. Hand Clin. 2010;26:245-264.
- ↑ 16.0 16.1 16.2 16.3 Handoll HHG, Madhok R. Conservative interventions for treating distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-112.
- ↑ 17.00 17.01 17.02 17.03 17.04 17.05 17.06 17.07 17.08 17.09 17.10 Patel VP, Paksima N. Complications of distal radius fracture fixation. Bulletin of NYU Hospital for Joint Diseases. 2010;68(2):112-8.
- ↑ McKay SD, MacDermid JC, Roth JH, Richards Rs. “Assessment of complications of distal radius fractures and development of a complication checklist.” J. Hand Surg. Am., nr 5; 26, September 2001: 916-22.
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 Walenkamp M., et al. Surgery versus conservative treatment in patients with type A distal radius fractures, a randomised controlled trial. BMC Musculoskeletal disorders 2014, 15:90.
- ↑ 20.0 20.1 20.2 20.3 Leiv M. Hove, Lindau T, Holmer P. Distal radius fractures: current concepts. Berlin, Heidelberg- Springer (2014) pg. 53- 58
- ↑ 21.0 21.1 21.2 Leone J, Bhandari M, Adili A, McKenzie S, Moro JK, Dunlop RB. Predictors of early and late instability following conservative treatment of exta-articular distal radius fractures. Arch Orthop Trauma Surg. 2004;124:38-41.
- ↑ 22.0 22.1 22.2 Herzberg G. Intra-articular fracture of the distal radius: arthroscopic-assisted reduction. J Hand Surg. 2010;35A:1517-1519.
- ↑ Handoll HHG, Huntley JS. Bone grafts and bone substitutes for treating distal radial fractures in adults (Review). The Cochrane Library. 2009;3:1-87.
- ↑ 24.0 24.1 Handoll HHG, Watts AC. Internal fixation and comparisons of different fixation methods for treating distal radial fractures in adults (Protocol). The Cochrane Library. 2008;4:1-14.
- ↑ Michlovitz S., et al. “Distal Radius Fractures: Therapy Practice Patterns” J Hand Ther. 14, (2001): 249-257.
- ↑ Kay S, McMahon M, Stiller K. An advice and exercise program has some benefits over natural recovery after distal radius fracture. Australian Journal of Physiotherapy. 2008. 54: 253-259.
- ↑ Bruder A, Taylor N, Dodd K, Shields N. Physiotherapy intervention practice patterns used in rehabilitation after distal radius fracture. Physiotherapy. 2013. 99: 233-240.
- ↑ Brotzman BS, Wilk KE. Handbook of Orthopaedic Rehabilitation, 2nd ed. Philadelphia: Mosby. 2007.
- ↑ 29.0 29.1 MacDermid JC, Roth JH, Richards RS. Pain and disability reported in the year following a distal radius fracture: A cohort study. BMC Musculoskelet Disord. 2003;4:24-36.
- ↑ Moore CM, Leonardi-Bee J. The prevalence of pain and disability one year post fracture of the distal radius in a UK population: A cross sectional survey. BMC Musculoskeletl Disord. 2008;9:129-138.
- ↑ Handoll HHG, Huntley JS, Madhok R. Closed reduction methods for treating distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-29.
- ↑ Handoll HHG, Vaghela MV, Madhok R. Percutaneous pinning for treating distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-70.
1. ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Handoll HHG, Huntley JS, Madhok R. External Fixation versus conservative treatment for distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-78.
level of evidence: 3A
2. ↑ 2.0 2.1 2.2 2.3 2.4 Handoll HHG, Huntley JS, Madhok R. Different methods of external fixation for treating distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-67.
level of evidence: 3A
3. ↑ Abramo A, Kopylov P, Tagil M. Evaluation of a treatment protocol in distal radius fractures: a prospective study in 581 patients using DASH as outcome. Acta Orthopaedica. 2008;79(3):376-385
level of evidence:2A
4. ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Bienek T, Kusz D, Cielinski L. Peripheral nerve compression neuropathy after fractures of the distal radius. J Hand Surg. (British and European Volume). 2006;31B(3):256-260.
level of evidence: 5
5. ↑ 5.0 5.1 5.2 5.3 Kay S, McMahon M, Stiller K. An advice and exercise program has some benefits over natural recovery after distal radius fracture: a randomized trial. Aust J Physiother. 2008;54:253-259.
level of evidence;3A
6. ↑ 6.0 6.1 Leung F, Ozkan M, Chow SP. Conservative treatment of intra-articular fractures of the distal radius – factors affecting functional outcomes. Hand Surg. 2000;5(2):145-153.
level of evidence:2A
7. ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 Bushnell BD, Bynum DK. Malunion of the distal radius. J Am Acad Orthop Surg. 2007;15:27-40.
level of evidence: 2C
8. ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Kleinman WB. Distal radius instability and stiffness; common complications of distal radius fractures. Hand Clin. 2010;26:245-264.
level of evidence: 3A
9. ↑ Leone J, Bhandari M, Adili A, McKenzie S, Moro JK, Dunlop RB. Predictors of early and late instability following conservative treatment of exta-articular distal radius fractures. Arch Orthop Trauma Surg. 2004;124:38-41.
level of evidence: 2B
10. ↑ 10.0 10.1 Handoll HHG, Madhok R. Conservative interventions for treating distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-112.
level of evidence: 2C
11. ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 11.7 11.8 Patel VP, Paksima N. Complications of distal radius fracture fixation. Bulletin of NYU Hospital for Joint Diseases. 2010;68(2):112-8.
level of evidence: 5
12. ↑ 12.0 12.1 12.2 Herzberg G. Intra-articular fracture of the distal radius: arthroscopic-assisted reduction. J Hand Surg. 2010;35A:1517-1519.
13. ↑ 13.0 13.1 13.2 Handoll HHG, Watts AC. Internal fixation and comparisons of different fixation methods for treating distal radial fractures in adults (Protocol). The Cochrane Library. 2008;4:1-14.
level of evidence: 3A
14. ↑ 14.0 14.1 14.2 Handoll HHG, Huntley JS, Madhok R. Closed reduction methods for treating distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-29.
level of evidence: 2A
15. ↑ 15.0 15.1 15.2 Handoll HHG, Vaghela MV, Madhok R. Percutaneous pinning for treating distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-70.
level of evidence: 2A
16. ↑ 16.0 16.1 Handoll HHG, Huntley JS. Bone grafts and bone substitutes for treating distal radial fractures in adults (Review). The Cochrane Library. 2009;3:1-87.
level of evidence: 2A
17. ↑ 17.0 17.1 Handoll HHG, Madhok R, Howe TE. Rehabilitation for distal radial fractures in adults (Review). The Cochrane Library. 2008;4:1-78.
level of evidence: 2A of 3A
18. ↑ 18.0 18.1 18.2 MacDermid JC, Roth JH, Richards RS. Pain and disability reported in the year following a distal radius fracture: A cohort study. BMC Musculoskelet Disord. 2003;4:24-36.
level of evidence: 2A
19. ↑ Moore CM, Leonardi-Bee J. The prevalence of pain and disability one year post fracture of the distal radius in a UK population: A cross sectional survey. BMC Musculoskeletl Disord. 2008;9:129-138.
level of evidence: 2B
20. ↑ Brotzman BS, Wilk KE. Handbook of Orthopaedic Rehabilitation, 2nd ed. Philadelphia: Mosby.2007.
level of evidence: 5
21. Benjamin JA. 1965. Abraham Colles (1773–1843) Distinguished surgeon from Ireland. Invest Urol 3:321–323
level of evidence: 5
22. http://orthoinfo.aaos.org/topic.cfm?topic=a00412
level of evidence: 5
23. Kenneth J. Koval, Joseph D. Zuckerman, Handbook of fractures, Philadelphia, second edition, 1994, pg 134
level of evidence:5
24. Kenneth J. Koval, Joseph D. Zuckerman, Handbook of fractures, Philadelphia, second edition, 1994, pg 134-135
level of evidence; 5
25. Kenneth J. Koval, Joseph D. Zuckerman, Handbook of fractures, Philadelphia, second edition, 1994, pg 135-138
level of evidence: 5
26. Kenneth J. Koval, Joseph D. Zuckerman, Handbook of fractures, Philadelphia, second edition, 1994, pg 135-138
level of evidence: 5
27. Melone CP Jr., Open treatment for displaced articular fractures of the distal radius, clin Ortop, pg 258-262
level of evidence 1C
28. McKay, SD (2001, 26 september). Assessment of complications of distal radius fractures and development of a complication checklist. Geraadpleegd op: 17/04/2015 http://www.sciencedirect.com.ezproxy.vub.ac.be:2048/science/article/pii/S0363502301444273#
Level of evidence: 2A
29. UCONN health. hand and wrist conditions and treatments. Geraadpleegd op: 17/04/2015 http://www.nemsi.uchc.edu/clinical_services/orthopaedic/handwrist/distal_radius.html
Level of evidence: 5
30. Jack, A (2013, 25 september). Distal radial fracture imaging. Geraadpleegd op: 17/04/2015 http://emedicine.medscape.com/article/398406-overview
Level of evidence: 5
31. Walenkamp M., et al. “Surgery versus conservative treatment in patients with type A distal radius fractures, a randomised controlled trial.’’ BMC Musculoskeletal disorders 2014, 15:90.
http://www.biomedcentral.com/1471-2474/15/90 Level of Evidence, 1B
32. Oren T., Wolf J., MD. “Soft- Tissue complications associated with distal radius fractures.” Operative Techniques in Orthopaedics, 19 , 2009, pg. 100—106.
Level of Evidence, 2B
33. Bot A., Ring D., “Recovery after fracture of the distal radius” Hand Clin 28, (2012) 235-243.
Level of Evidence, 3A
34. Bruder A., Taylor N., Dodd K., Shields N. “Physiotherapy intervention practice patterns used in rehabilitation after distal radius fracture” Physiotherapy 99 (2013) 233- 240.
Level of Evidence, 2B
35. P. Cherubino, A. Bini, D. Marcolli. “Management of distal radius fractures: Treatment protocol and functional results” Injury, Int.J. Care injured 41 (2010) 1120- 1126
Level of Evidence, 5
36. Michlovitz S., et al. “Distal Radius Fractures: Therapy Practice Patterns” J Hand Ther. 14, (2001): 249-257.
Level of Evidence, 2B
37. Kay S., McMahon M., Stiller K. “An advice and exercise program has some benefits over natural recovery after distal radius fracture” Australian Journal of Physiotherapy vol.54 (2008) pg. 253- 259.
Level of Evidence, 1B
38. Leiv M. Hove, Lindau T., Holmer P. “Distal radius fractures: current concepts” Berlin, Heidelberg- Springer (2014) pg. 53- 58
Level of Evidence, 5
39. Mitsukane M., et al. “Immediate effects of repetitive wrist extension on grip strength in patients with distal radial fractures” Archives of physical medicine and rehabilitation, 12 october 2014.
Level of Evidence, 1B
40. McKay SD, MacDermid JC, Roth JH, Richards Rs. “Assessment of complications of distal radius fractures and development of a complication checklist.” J. Hand Surg. Am., nr 5; 26, September 2001: 916-22. Level of Evidence, 2B
41. Nelson, DL, ‘wrist fractures’, (2012)
http://www.davidlnelson.md/articles/Wrist_Fracture.htm
Level of Evidence, 5