Femoral Fractures: Difference between revisions
No edit summary |
No edit summary |
||
| Line 21: | Line 21: | ||
# Partial fracture: incomplete break of a bone. This type of fracture refers to the way the bone breaks. In an incomplete fracture, the bone cracks but doesn’t break all the way through. In contrast, there is a complete fracture, where the bone snaps into two or more parts.<ref>Cleveland Clinic. Fractures. 2013. (Available at http://my.clevelandclinic.org/services/orthopaedics-rheumatology/diseases-conditions/hic-fractures, assessed 21 December 2014)fckLR</ref><ref>WebMD. Broken bone: types of fractures, symptoms and prevention. 2014. (Available at http://www.webmd.boots.com/a-to-z-guides/bone-fractures-types-symptoms-prevention, accessed on 21 december 2014)fckLR</ref> | # Partial fracture: incomplete break of a bone. This type of fracture refers to the way the bone breaks. In an incomplete fracture, the bone cracks but doesn’t break all the way through. In contrast, there is a complete fracture, where the bone snaps into two or more parts.<ref>Cleveland Clinic. Fractures. 2013. (Available at http://my.clevelandclinic.org/services/orthopaedics-rheumatology/diseases-conditions/hic-fractures, assessed 21 December 2014)fckLR</ref><ref>WebMD. Broken bone: types of fractures, symptoms and prevention. 2014. (Available at http://www.webmd.boots.com/a-to-z-guides/bone-fractures-types-symptoms-prevention, accessed on 21 december 2014)fckLR</ref> | ||
# Completed displaced fracture: breaks into two or more pieces and is no longer correctly aligned. Displacement of fractures is defined in terms of the abnormal position of the distal fracture fragment in relation to the proximal bone. <ref>2.0 2.1 WebMD. Understanding Bone Fractures - the Basics. 2014. (Available at http://www.webmd.com/a-to-z-guides/understanding-fractures-basic-information, accessed 19 December 2014) fckLR</ref> | # Completed displaced fracture: breaks into two or more pieces and is no longer correctly aligned. Displacement of fractures is defined in terms of the abnormal position of the distal fracture fragment in relation to the proximal bone. <ref>2.0 2.1 WebMD. Understanding Bone Fractures - the Basics. 2014. (Available at http://www.webmd.com/a-to-z-guides/understanding-fractures-basic-information, accessed 19 December 2014) fckLR</ref> | ||
| Line 92: | Line 62: | ||
==== Muscle Strength ==== | ==== Muscle Strength ==== | ||
The physical therapist has to focus on restoring the strength of the following muscles that are affected by the fracture: | The physical therapist has to focus on restoring the strength of the following muscles that are affected by the fracture: | ||
=== '''PT management''' === | === '''PT management''' === | ||
| Line 132: | Line 85: | ||
<br>Before going to bed, it is advised to massage the pre-articular structures and mobilisation of the hip. All mobilisation techniques can be used except rotations! It is also advised to use passive mobilisation techniques for retrieving the mobility of the patellar bone. The osteosynthesis is positively influenced by using isometric exercises of the hamstrings, quadriceps and glutei and the use of active exercises with low resistance to train the muscles of the hip and knee. The use of massage techniques of the quadriceps is advised straight after the verticalisation without support. The synthesis of the bone is also positively influenced by unilateral stabilisation exercises. After the consolidation period, orthopaedic therapy is recommended.<ref name="Xhardez et al.">Xhardez Y et al. Vade-mecum kinésithérapie et de reeducation fonctionnelle. 2002.</ref><br> | <br>Before going to bed, it is advised to massage the pre-articular structures and mobilisation of the hip. All mobilisation techniques can be used except rotations! It is also advised to use passive mobilisation techniques for retrieving the mobility of the patellar bone. The osteosynthesis is positively influenced by using isometric exercises of the hamstrings, quadriceps and glutei and the use of active exercises with low resistance to train the muscles of the hip and knee. The use of massage techniques of the quadriceps is advised straight after the verticalisation without support. The synthesis of the bone is also positively influenced by unilateral stabilisation exercises. After the consolidation period, orthopaedic therapy is recommended.<ref name="Xhardez et al.">Xhardez Y et al. Vade-mecum kinésithérapie et de reeducation fonctionnelle. 2002.</ref><br> | ||
As non-operative treatment there are 3 alternatives:<br>1. Skin traction: used in adults only for emergency fracture immobilisation in the field for patient comfort and to facilitate patient transport. Main disadvantage is the causing of slippage or skin necrosis when applying sufficient forces to the limb.<br>2. Skeletal traction: used for early fracture care before a definitive operative procedure can be performed. The goal is to restore the femoral length and to limit rotational and angular deformities. Skeletal traction may be applied through the distal femur or proximal tibia. Problems with skeletal traction include knee stiffness, limb shortening, prolonged hospitalisation, respiratory and skin ailments, and malunion. <br>3. Cast Brace: an external support device that permits progressive weight bearing by partially unloading the fracture through circumferential support of the soft tissues. Indications for cast bracing include open fracture, distal third fractures, and comminuted midshaft fractures of the femur. Proximal, simple transverse, or oblique fractures are less amendable to cast bracing due to high stress concentration and a propensity to angulate. The cast brace is best used after an initial period of skeletal traction. Consistently high rates of union, superior to 90%, usually by 13 to 14 weeks, have been reported in numerous studies. Problems with cast bracing include loss of reduction and subsequent malunion, shortening and angulation.<ref name="Keany" /><br> | As non-operative treatment there are 3 alternatives:<br>1. Skin traction: used in adults only for emergency fracture immobilisation in the field for patient comfort and to facilitate patient transport. Main disadvantage is the causing of slippage or skin necrosis when applying sufficient forces to the limb.<br>2. Skeletal traction: used for early fracture care before a definitive operative procedure can be performed. The goal is to restore the femoral length and to limit rotational and angular deformities. Skeletal traction may be applied through the distal femur or proximal tibia. Problems with skeletal traction include knee stiffness, limb shortening, prolonged hospitalisation, respiratory and skin ailments, and malunion. <br>3. Cast Brace: an external support device that permits progressive weight bearing by partially unloading the fracture through circumferential support of the soft tissues. Indications for cast bracing include open fracture, distal third fractures, and comminuted midshaft fractures of the femur. Proximal, simple transverse, or oblique fractures are less amendable to cast bracing due to high stress concentration and a propensity to angulate. The cast brace is best used after an initial period of skeletal traction. Consistently high rates of union, superior to 90%, usually by 13 to 14 weeks, have been reported in numerous studies. Problems with cast bracing include loss of reduction and subsequent malunion, shortening and angulation.<ref name="Keany">Keany, J. et al. Femur fracture. 2013. (Available at http://emedicine.medscape.com/article/824856-overview, accessed 6 November 2014)</ref><br> | ||
==== Physical Exercise ==== | ==== Physical Exercise ==== | ||
Revision as of 07:45, 10 December 2022
Top Contributors - Margaux Jacobs, Kim Jackson, Vanderpooten Willem, Lucinda hampton, Admin, Vidya Acharya, Nupur Smit Shah, Jentel Van De Gucht, Alex Palmer, Rachael Lowe, Daphne Jackson, Margaux Jacobs, Jason Coldwell, Aminat Abolade, Evan Thomas, WikiSysop, Lauren Lopez and 127.0.0.1
Introduction[edit | edit source]
The femur is the largest and strongest bone in the body. Due to its strength it requires a significant force to break it. However, certain medical conditions that weaken the bone make it more vulnerable to fracture, so called pathological fractures. For example: osteoporosis: malignancy; infection.[1]
Location[edit | edit source]
There are different types of femoral fractures according where they occur, namely:
- Femoral Head Fractures: often seen in the elderly osteoporotic population where the cortical bone is weak and so is the trabecular system. It occurs spontaneously or due to low-energy trauma. In the younger population, this fracture is rare and occurs due to high-energy trauma, usually associated with hip dislocations.[2]
- Femoral Neck Fractures: one of the most frequent fractures presenting to the emergency department and orthopedic trauma teams.[3]See link for more.
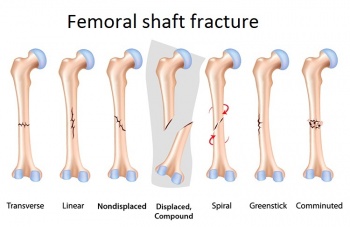
- Femoral Shaft Fractures: more common in men after a high-energy impact or in elderly women after a low-energy fall. [4] They can be described as follows: Type I - Spiral or transverse (most common) Type II – Comminuted Type III - Open [5]
- Distal femoral fracture: involve the femoral condyles and the metaphyseal region, often the resulting from high energy trauma eg motor vehicle accidents or a fall from a height. In the elderly, they may occur as an accident at home eg fall.[6]See link for more.
Types[edit | edit source]
There are 4 types of fracture:
- Femoral stress fracture
- Severe impaction fractures: the bone breaks into multiple fragments, which are driven into each other. It is a closed fracture that occurs when pressure is applied to both ends of the bone, causing it to split into two fragments that jam into each other. [7]
- Partial fracture: incomplete break of a bone. This type of fracture refers to the way the bone breaks. In an incomplete fracture, the bone cracks but doesn’t break all the way through. In contrast, there is a complete fracture, where the bone snaps into two or more parts.[8][9]
- Completed displaced fracture: breaks into two or more pieces and is no longer correctly aligned. Displacement of fractures is defined in terms of the abnormal position of the distal fracture fragment in relation to the proximal bone. [10]
Physical Therapy Management[edit | edit source]
Rehabilitation Objectives[edit | edit source]
Range Of Motion[edit | edit source]
Improve the range of motion for the hip and the knee joint. In elderly population, the focus is to achieve functional range of motion.
| Motion | Normal | Functional |
|---|---|---|
| Knee Flexion | 130 to 140 degrees | 110 degrees |
| Hip Flexion | 125-128 degrees | 90 to 110 degrees |
| Hip Extension | 0-20 degrees | 0 to 5 degrees |
| Hip Abduction | 45 to 48 degrees | 0 to 20 degrees |
| Hip adduction | 40 to 45 degrees | 0 to 20 degrees |
| Internal and External Rotation | 45 degrees | 0 to 15/20 degrees |
Muscle Strength[edit | edit source]
The physical therapist has to focus on restoring the strength of the following muscles that are affected by the fracture:
PT management[edit | edit source]
Whilst in hospital, a therapist will teach the patient how to use a walking aid to allow them to mobilise, depending on their weight bearing status. The patient should be taught basic range of movement and strengthening exercises to maintain a degree of strength and reduce the risk of blood clots.
Surgical fixation and immobilization are followed by extensive physical therapy. Under extensive therapy can be understood that the patients who underwent a femur fracture should receive a treatment by a physiotherapist who will invest time in gait training. Gait training results in increased bone formation. Even if gait training is completed using 30-50% of body weight support, an increase in bone formation could be found. [11]After a femoral fracture, most of the muscles are much weaker than before so physiotherapy is very important.
The physiotherapist will begin with a range of motion exercises for the hip, knee and ankle because mobility is decreased following immobilization. Mobilization is a very important treatment in the recovery process. The patient can also begin strengthening exercises based on the surgeon's orders (typically six weeks post-op). Patients should also undergo balance and proprioceptive rehab and these abilities are quickly lost with inactivity.
Mobility exercises[edit | edit source]
Knee: flexion and extension, abduction and adduction
Hip: flexion and extension, abduction and adduction, rotation
Functional quadriceps exercises should be initiated as soon as possible after the surgery because the quadriceps help provides stability in the knee. Flexion exercises also need to start as soon as possible, provided the fracture is adequately supported (i.e. the selected fixation approach allows for weight bearing). Physiotherapy should be continued until an acceptable functional range has been achieved or until a static position has been reached. It is necessary to record the range of movements in the knee with accuracy; first, this should be done at weekly and then at monthly intervals.
During the postoperative treatment of patients with a proximal femoral fracture, physical therapy should focus on increasing the muscle strength, to improve walking safety and efficiency. Allowing the elderly patient to become more independent.
Research indicates that strengthening the abductor and adductor muscles of the hip increase the mediolateral stability during walks. Resulting in an influence on the improvement of the patient’s dynamic balance.[12]
Orthopaedic therapy:[edit | edit source]
During the immobilisation period, the therapists need to actively mobilise the foot, with or without weight. Another important aspect is the mobilisation through a hole in the plaster of the patellar bone. The use of isometric exercises are also important to train the muscles (quadriceps, hamstring & glutei) of the upper leg. After the immobilisation period, it is necessary to fixate the leg manually or by using a brace. The fixation is needed for the re-education of hip and knee and to secure a progressively verticalisation of the leg and to make the patient independent while walking or during other activities. Also, stabilisation exercises with unilateral support are recommended, but also balneotherapy. After the consolidation therapists need to focus on progressively increased pressure, the revalidation of the gait cycle, more intense mobilisation, strength-training therapy to reverse the muscle atrophy that occurred during the immobilisation period and condition training to increase the loss of endurance during the immobilisation period.
Osteosynthesis:[edit | edit source]
Before going to bed, it is advised to massage the pre-articular structures and mobilisation of the hip. All mobilisation techniques can be used except rotations! It is also advised to use passive mobilisation techniques for retrieving the mobility of the patellar bone. The osteosynthesis is positively influenced by using isometric exercises of the hamstrings, quadriceps and glutei and the use of active exercises with low resistance to train the muscles of the hip and knee. The use of massage techniques of the quadriceps is advised straight after the verticalisation without support. The synthesis of the bone is also positively influenced by unilateral stabilisation exercises. After the consolidation period, orthopaedic therapy is recommended.[13]
As non-operative treatment there are 3 alternatives:
1. Skin traction: used in adults only for emergency fracture immobilisation in the field for patient comfort and to facilitate patient transport. Main disadvantage is the causing of slippage or skin necrosis when applying sufficient forces to the limb.
2. Skeletal traction: used for early fracture care before a definitive operative procedure can be performed. The goal is to restore the femoral length and to limit rotational and angular deformities. Skeletal traction may be applied through the distal femur or proximal tibia. Problems with skeletal traction include knee stiffness, limb shortening, prolonged hospitalisation, respiratory and skin ailments, and malunion.
3. Cast Brace: an external support device that permits progressive weight bearing by partially unloading the fracture through circumferential support of the soft tissues. Indications for cast bracing include open fracture, distal third fractures, and comminuted midshaft fractures of the femur. Proximal, simple transverse, or oblique fractures are less amendable to cast bracing due to high stress concentration and a propensity to angulate. The cast brace is best used after an initial period of skeletal traction. Consistently high rates of union, superior to 90%, usually by 13 to 14 weeks, have been reported in numerous studies. Problems with cast bracing include loss of reduction and subsequent malunion, shortening and angulation.[14]
Physical Exercise[edit | edit source]
Improving muscle strength is necessary to enhance postoperative walking capacity for rehabilitation and to diminish the risks of falls. Physical activity will help:
- Preventing other fractures
- Increasing gait speed & balance
- Increasing ADL Performance
- Regaining walking capacity as early as possible after immobilization to avoid respiratory complications[15]
- Better brain function and more social contact
Aerobic fitness is useful to include in a physical therapy plan for an improved cardiorespiratory capacity will lead to a better walking capacity.
Physical exercises are not only crucial for rehabilitation after fracture but for ongoing reinforcing of the mineral bone density, especially in vulnerable populations like elder fragile patients, osteoporotic post-menopausal women or people suffering from osteoporosis or osteopenia. Long-term odd-impact exercise-loading, is associated, similar to high-impact exercise-loading, with a 20% thicker cortex around the femoral neck [16]. In aerobic fitness, these type of movements are most frequently used.
Moderate magnitude impacts from Odd-exercise loading is mechanically less demanding and makes the body work in all directions, retraining the biomechanical qualities and properties of the bone structure and impacting positively the bone mineral density. Fitness aerobics, dance fitness, dance, ball games, gymnastics involving rapid turns and movements are good examples of odd-impact exercises.
Furthermore, duration, frequency and intensity are important and should be customized to the different age-groups.
Strengthening exercises seem to be key for the functional improvement. [17] These strength exercises may as well produce advantages in the psychosocial area which tends to be altered in elder patients that suffered a fracture. Weight-bearing exercises will reinforce the dynamic balance and functional performance [18], especially exercises in standing position since they are more challenging for the postural control [19].
Home Rehabilitation Training[edit | edit source]
Home Rehabilitation Training leads towards better rehabilitation and better performance in daily activities. Home physiotherapy training is suitable for all elder patients, including those suffering from cognitive or psychological impairment. The literature stresses the importance of home physiotherapy, in combination with day-to-day activities like going to the shop, for gaining confidence, balance, functionality and reducing as such the number of falls. Therefore it can also be seen as a way to prevent falls. [20]Fall prevention programmes are important for the elder population that already suffers a femoral fracture. The literature indicates that elder people often fall again following a previous hip or femoral fracture and that this constitutes a major health problem [21]. The study of Berggren et al. concludes that fall-prevention must be part of everyday life in fall-prone elderly. Prevention and treatment of fall-risk factors are key. These programs should include gait training with advice on assistive devices and medication, exercise programmes for balance training, treatments for cardiovascular problems, environmental modifications and hypotension.[22].
Electrical Stimulation[edit | edit source]
The literature is still not conclusive on this topic and the results of one study may contradict or, on the contrary, reinforce the results of another study. Yet there is evidence supporting the beneficial effects of electrical stimulation, especially in combination with physical therapy exercises. In a randomized controlled trial Gremeaux et al.conclude that « Low-frequency electric muscle stimulation can thus be proposed as a simple, effective, and safe complementary therapy used in conjunction with standard rehabilitation in everyday clinical practice in these patients.
In a critical literature review of 2005 Bax et al. stated that only limited evidence suggests that neuromuscular electrical stimulation can be more effective than no exercise in individuals with impaired and unimpaired quadriceps, and volitional exercises appeared more effective in most situations [23]. Low-frequency ES may lead to a significant increase in muscle strength in the operated limb and is overall well tolerated by the elder population.
The terms « Functional electrical Stimulation », « Cyclic Stimulation » or « Neuromuscular Electrical Stimulation » all refer to the same « Electrical Stimulation » but speaking of it, distinction should be made between low-frequency and high-frequency stimulation. High-frequency stimulation acts principally on fast-twitch fibers, increasing muscle strength and resistance to fatigue. It could be useful to fight muscle de-conditioning but it is mostly not well tolerated in older patients.
Low-frequency Electrical Stimulation (LFES) increases the metabolic activity of slow-twitch muscle fibers and the proportion of slow-twitch fibers. This fiber-type is more dominantly present in the Quadriceps and therefore interesting to use this low frequency on the knee-extensor muscle. Other structural adaptations are the development of mitochondrial apparatus and increase in capillary density, resulting in increased resistance to fatigue.[24]. LFES has also been used in the treatment of different neurologic and orthopedic disorders.
ES may attenuate muscle atrophy, helps regaining muscle strength faster after surgery and show a trend towards improved autonomy and walking speed [25]. The results of the study of Gremeaux et al. suggest that low-frequency electric muscle stimulation associated with conventional physiotherapy is superior to physiotherapy alone in increasing strength of the knee extensors, which is accompanied by a return to better muscular equilibrium between the operated and non-operated limb. It leads to a significant increase in muscle strength in the operated limb. In young subjects ES can produce powerful muscle contraction and give training effects as good as or better than voluntary isometric exercise[26]
References[edit | edit source]
- ↑ Very well health Femur Fracture Available;https://www.verywellhealth.com/femur-fracture-2549281 (accessed 10.12.2022)
- ↑ Orthobullets Femoral Head Fractures Available:https://www.orthobullets.com/trauma/1036/femoral-head-fractures (accessed 10.12.2022)
- ↑ Hip Fracture
- ↑ Mercer's Textbook of Orthopaedics and Trauma Tenth edition edited by Suresh Sivananthan, Eugene Sherry, Patrick Warnke, Mark D Miller
- ↑ WebMD. Broken bone: types of fractures, symptoms and prevention. 2014. (Available at http://www.webmd.boots.com/a-to-z-guides/bone-fractures-types-symptoms-prevention, accessed on 21 december 2014)fckLR
- ↑ Radiopedia Distal femoral fracture. Available: https://radiopaedia.org/articles/distal-femoral-fracture (accessed 10.12.2022)
- ↑ 2.0 2.1 WebMD. Understanding Bone Fractures - the Basics. 2014. (Available at http://www.webmd.com/a-to-z-guides/understanding-fractures-basic-information, accessed 19 December 2014) fckLR
- ↑ Cleveland Clinic. Fractures. 2013. (Available at http://my.clevelandclinic.org/services/orthopaedics-rheumatology/diseases-conditions/hic-fractures, assessed 21 December 2014)fckLR
- ↑ WebMD. Broken bone: types of fractures, symptoms and prevention. 2014. (Available at http://www.webmd.boots.com/a-to-z-guides/bone-fractures-types-symptoms-prevention, accessed on 21 december 2014)fckLR
- ↑ 2.0 2.1 WebMD. Understanding Bone Fractures - the Basics. 2014. (Available at http://www.webmd.com/a-to-z-guides/understanding-fractures-basic-information, accessed 19 December 2014) fckLR
- ↑ Carvalho DC, Garlipp CR, Bottini PV, Afaz SH, Moda MA, Cliquet Jr A. Effect of treadmill gait on bone markers and bone mineral density of quadriplegic subjects. Brazilian journal of medical and biological research. 2006;39:1357-63.
- ↑ MCarneiro B, Alves DP, Mercadante MT. Physical therapy in the post-operative of proximal femur fracture in elderly: Literature review. Acta Ortop. Bras. 2013;21:175-8.
- ↑ Xhardez Y et al. Vade-mecum kinésithérapie et de reeducation fonctionnelle. 2002.
- ↑ Keany, J. et al. Femur fracture. 2013. (Available at http://emedicine.medscape.com/article/824856-overview, accessed 6 November 2014)
- ↑ MCarneiro B, Alves DP, Mercadante MT. Physical therapy in the post-operative of proximal femur fracture in elderly: Literature review. Acta Ortop. Bras. 2013;21:175-8.
- ↑ Nikander R, Kannus P, Dastidar P, Hannula M, Harrison L, Cervinka T, Narra NG, Aktour R, Arola T, Eskola H, Soimakallio S. Targeted exercises against hip fragility. Osteoporosis International. 2009 Aug;20(8):1321-8.
- ↑ MCarneiro B, Alves DP, Mercadante MT. Physical therapy in the post-operative of proximal femur fracture in elderly: Literature review. Acta Ortop. Bras. 2013;21:175-8.
- ↑ Yang SD, Ning SH, Zhang LH, Zhang YZ, Ding WY, Yang DL. The effect of lower limb rehabilitation gymnastics on postoperative rehabilitation in elderly patients with femoral shaft fracture: a retrospective case-control study. Medicine. 2016 Aug;95(33).
- ↑ MCarneiro B, Alves DP, Mercadante MT. Physical therapy in the post-operative of proximal femur fracture in elderly: Literature review. Acta Ortop. Bras. 2013;21:175-8.
- ↑ Giusti A, Barone A, Oliveri M, Pizzonia M, Razzano M, Palummeri E, Pioli G. An analysis of the feasibility of home rehabilitation among elderly people with proximal femoral fractures. Archives of physical medicine and rehabilitation. 2006 Jun 1;87(6):826-31.
- ↑ Berggren M, Stenvall M, Olofsson B, Gustafson Y. Evaluation of a fall-prevention program in older people after femoral neck fracture: a one-year follow-up. Osteoporosis international. 2008 Jun;19(6):801-9.
- ↑ Stenvall M, Olofsson B, Lundström M, Englund U, Borssén B, Svensson O, Nyberg L, Gustafson Y. A multidisciplinary, multifactorial intervention program reduces postoperative falls and injuries after femoral neck fracture. Osteoporosis international. 2007 Feb;18(2):167-75.
- ↑ Braid V, Barber M, Mitchell SL, Martin BJ, Granat M, Stott DJ. Randomised controlled trial of electrical stimulation of the quadriceps after proximal femoral fracture. Aging clinical and experimental research. 2008 Feb;20(1):62-6.
- ↑ Gremeaux V, Renault J, Pardon L, Deley G, Lepers R, Casillas JM. Low-frequency electric muscle stimulation combined with physical therapy after total hip arthroplasty for hip osteoarthritis in elderly patients: a randomized controlled trial. Archives of physical medicine and rehabilitation. 2008 Dec 1;89(12):2265-73.
- ↑ Gremeaux V, Renault J, Pardon L, Deley G, Lepers R, Casillas JM. Low-frequency electric muscle stimulation combined with physical therapy after total hip arthroplasty for hip osteoarthritis in elderly patients: a randomized controlled trial. Archives of physical medicine and rehabilitation. 2008 Dec 1;89(12):2265-73.
- ↑ Braid V, Barber M, Mitchell SL, Martin BJ, Granat M, Stott DJ. Randomised controlled trial of electrical stimulation of the quadriceps after proximal femoral fracture. Aging clinical and experimental research. 2008 Feb;20(1):62-6.