Femoral Neck Hip Fracture
Original Editor - Delmoitie Giovanni
Top Contributors - Delmoitie Giovanni, Lucinda hampton, Simisola Ajeyalemi, Jessie Tourwe, Joyce De Gelas, Kim Jackson, Admin, Tolulope Adeniji, Aminat Abolade, Debontridder Jordy, Annelies Beckers, Sara Evenepoel, Yarne Leuckx, Vidya Acharya, Claire Knott, Lauren Lopez, Elien Lebuf and Karen Wilson
Introduction[edit | edit source]
Hip Fracture (Image R: hip fracture xray):
- Vernacular term for fracture of the femoral neck, typically resulting from a fall in an old person with osteoporosis; more common in women; requires surgical repair with internal fixation and can lead to prolonged or permanent loss of mobility and shortened life span[1].
- Common injuries sustained by older patients who are both more likely to have unsteadiness of gait and reduced bone mineral density, predisposing to fracture.
- The biggest risk factors for a hip fracture are osteoporosis and cognitive impairment.[2][3]
- About one-third of elderly people living independently fall every year, with 10% of these falls resulting in a hip fracture.[4]
- A serious injury that occurs mostly in elderly people and complications can be life-threatening.[5][3]
- In younger patients femur fractures are the result of a high energy trauma, such as a motor accident, gunshot wound, or jump/fall from a height.[3]
- High mortality, long-term disability and huge socio-economic burden are the main consequences of a hip fracture.
Clinically Relevant Anatomy[edit | edit source]
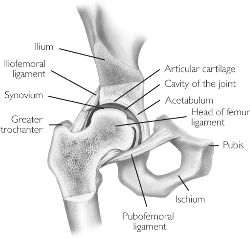
The hip joint is a
- Ball and socket joint, formed by the head of the femur and the acetabulum of the pelvis.
- Very sturdy joint, due to the tight fitting of the bones and the strong surrounding ligaments and muscles.
The femur connects at the acetabulum of the pelvis and projects laterally before angling medially and inferiorly to form the knee.
A hip fracture occurs just below the head of femur (HOF) ie the region of the femur called the femoral neck. A femoral neck fracture disconnects the HOF from the rest of the femur,
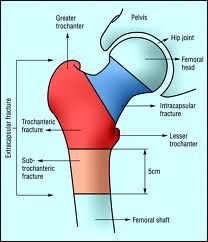
Hip fractures can be classified into intracapsular (femoral neck) fractures and extracapsular fractures. The intracapsular fractures are contained within the hip capsule itself. Those fractures are subcapital neck fracture and transcervical neck fracture. The extracapsular fractures are intertrochantericic and subtrochanteric fracture. You also have a greater and lesser trochantefracturees[6] (figure1)
Click Hip Anatomy for more details
Epidemiology[edit | edit source]
Approximately 1.6 million hip fractures occur worldwide each year, by 2050 this number could reach between 4.5 million and 6.3 million.
- Between 1990 and 2000, there was nearly a 25% increase in hip fractures worldwide. The peak number of hip fractures occurred at 75-79 years of age for both sexes.
- Nearly 75% of all hip fractures occur in women.
- Men account for 25% of hip fractures occurring in the over 50 population.
- Hip fractures are invariably associated with chronic pain, reduced mobility, disability, and an increasing degree of dependence.
- After sustaining a hip fracture 10-20% of formerly community dwelling patients require long term nursing care, with the rate of nursing home admission rising with age.
- In white women, the lifetime risk of hip fracture is 1 in 6.
- A 50 year old woman has a 2.8% risk of death related to hip fracture during her remaining lifetime.
- 5-10% of patients experience a recurrent hip fracture, with the mean interval between the first and second fracture being 3.3 years .
- Up to 20% of patients die in the first year following hip fractures, mostly due to pre-existing medical conditions. Less than half those who survive the hip fracture regain their previous level of function[7]
Classification of Hip Fractures[edit | edit source]
Hip fractures: Classified into intracapsular and extracapsular fractures[8]
Intracapsular fractures (femoral neck fractures): Occurs within the hip capsule; accounts for 45% of all acute hip fractures in the elderly[9]; susceptible to malunion/avascular necrosis of the HOF because of the limited blood supply to the area.
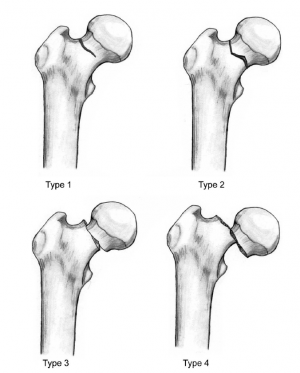
Intracapsular fractures are further classified as nondisplaced or displaced based on radiographic findings[10]
- Type 1: undisplaced and incomplete fracture
- Type 2: undisplaced complete fracture
- Type 3: complete fracture but incompletely displaced
- Type 4: complete fracture and completely displaced
Extracapsular fractures: intertrochanteric fracture or subtronchanteric fracture.
- Intertrochanteric fracture: occurs between the greater and the lesser trochanter[8]; intertrochanteric region has a good blood supply, avascular necrosis or nonunion is rare.
- Subtronchanteric fracture: occurs below the lesser trochanter, approximately 2.5 inches below
Etiology[edit | edit source]
Most commonly:
- Falls in the elderly: in elderly patients, the mechanism of injury various from falls directly onto the hip to a twisting mechanism in which the patient’s foot is planted and the body rotates. There is generally deficient elastic resistance in the fractured bone[2].
- More than 50% of hip fracture patients have osteoporosis, and nearly all are osteopenia[11]
- The majority of fragility hip fractures occurred inside the home[12]
- Significant trauma (e.g. motor vehicle collisions) in younger patients
- About 3% of hip fractures are related to localized bone weakness at the fracture site, secondary to tumor, followed by bone cysts, or Paget’s disease.
Risk factors[edit | edit source]
Risk factors for hip fracture include[13][14]:
- Gender: prevalent in women; postmenopausal twice as likely as premenopausal to have hip fracture[15]
- Reduced Bone density[16]
- Fall[17]
- Medications: Some medications can cause a decrease in bone density like cortisone.
- Nutrition: It is well known that calcium and vitamin D increase bone mass, so a lack of it can cause several fractures, including hip fractures. Some eating disorders like anorexia and bulimia can weaken your bones, zo you become more fragile to have a hip fracture.
- Age: the older you get, the higher the risk is for hip fractures. 90% of these fractures occur in persons over 70 years old.
- Alcohol and tobacco: These products can reduce the bone mass, causing a higher risk to have a hip fracture
- Medical problems: Endocrine disorders can cause fragility of the bones
- Physical inactivity: Physical activity is very important for the muscle mass and the bone mass, so if you practice enough sports you will have less risk to have hip fractures.
- Stroke disease increases risk factor for falls which can cause a hip fracture.
- Parkinson’s disease increases risk factor for falls which can cause a hip fracture.
Risk factors other than low bone mineral density (BMD), defined by the National Osteoporosis Foundation (National Osteoporosis Foundation, 1998) are previous history of fracture as an adult, history of fracture in a first-degree relative, low body weight, and current cigarette smoking.[18]Another risk factor that is frequently discussed for the last years is the proximal femoral geometry, it is suggested as an important marker for the hip fracture risks.[18]
Characteristics/Clinical Presentation[edit | edit source]
- Dull ache in the groin and/or hip region[11]
- Inability to put weight on the injured leg causing immobility right after the fall[19]
- Shorter leg on the side of the injured hip
- External rotation of the injured leg[19]
- Stiffness, bruising and swelling in and around the hip
Diagnostic Procedures[edit | edit source]
The diagnosis of a hip fracture is established based on patient history, physical examination, and radiography.[19]
- Plain radiographs (sensitivity 93-98%) is the first-line investigation for suspected NOF fractures.
- In patients with a suspected occult NOF fracture, MRI (sensitivity 99-100%) is recommended by many institutions as the second-line test if available within 24 hours, with CT or nuclear medicine bone scan third-line[2]
Outcome Measures[edit | edit source]
- Berg Balance Scale
- BOOMER
Prognosis[edit | edit source]
Hip fractures carry an approximately 30% risk of mortality at 1 year,[20]and 25% to 75% of community-dwelling adults may not regain their pre-fracture level of function.[21][22]Predictors of mortality include significant comorbid disease, low pre-injury cognitive function, abnormal preoperative ECG, age >85 years, and decreased pre-fracture mobility. Early surgery was not associated with improved function and increased mortality though it was associated with reduced pain and length of stay. Early surgery also resulted in fewer complications. These conclusions were obtained by comparing patients having surgery within 24 hours with those having surgery after 24 hours on the following outcomes[23]:
- Mean pain scores over the first 5 hospital days
- Number of days of severe and very severe pain over hospital days 1 to 5 (assessed by asking patients if they were experiencing no pain, or mild, moderate, or severe pain)
- Major postoperative complications
- Length of hospital stay
- Mortality through 6 months
- FIM locomotion (a 2-item subscale focusing on walking and climbing stairs) score at 6 months
- FIM self-care (a 6-item scale of self-care activities including bathing and dressing)
- FIM transferring (a 3-item scale focusing on transfers from the bed, toilet, and tub).[23]
In the study of Diamond TH et al. the main prognostic factors such as pre-existing illness and osteoporotic risk factor; outcome data such as fracture-related complications, mortality, and level of function as measured by the Barthel index of activities of daily living at 6 and 12 months postfracture.
The results of these outcome measures are that fracture-related complications affected similar proportions of men and women (30% v. 32%), and mean length of hospital stay was similar. Fourteen percent of men died in hospital compared with only 6% of women (P = 0.06). Men had more risk factors for osteoporosis (P < 0.01).[24]
Physical functioning (measured by the Barthel index) deteriorated significantly in men from 14.9 at baseline to 13.4 at six months (P < 0.05) and 12.4 at 12 months (P < 0.05) after fracture.[24]
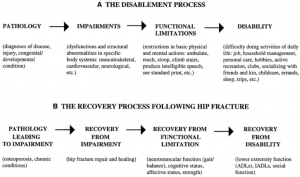
Jay Magaziner et al. investigated eight areas of function after hip fracture. This eight areas of function include upper and lower extremity physical and instrumental activities of daily living, gait and balance, social, cognitive, and affective function. They were measured by personal interview and direct observation during hospitalization at 2, 6, 12, 18, and 24 months. Levels of recovery are described in each area, and time to reach maximal recovery was estimated using Generalized Estimating Equations and longitudinal data. Most areas of functioning showed progressive lessening of dependence over the first postfracture year, with different levels of recovery and time to maximum levels observed for each area. New dependency in physical and instrumental tasks for those not requiring equipment or human assistance prefracture ranged from as low as 20.3% for putting on pants to as high as 89.9% for climbing five stairs. Recuperation times were specific to area of function, ranging from approximately 4 months for depressive symptoms (3.9 months), upper extremity function (4.3 months), and cognition (4.4 months) to almost a year for lower extremity function[25]
Physical Examination[edit | edit source]
On physical examination, findings on the patient with a hip fracture may include the following:
- limited and painful hip range of motion, especially in internal rotation.
- the injured leg is shortened, externally rotated, and abducted in the supine position
- Pain is noted upon attempted passive hip motion.
- Ecchymosis may or may not be present.
- An antalgic gait pattern may be present.
- Tenderness to palpation around the inguinal area, over the femoral neck. This area may also be swollen.
- Increased pain on the extremes of hip rotation, an abduction lurch, and an inability to stand on the involved leg
For more on Hip examination, click www.physio-pedia.com/Hip_Examination
Medical Management[edit | edit source]
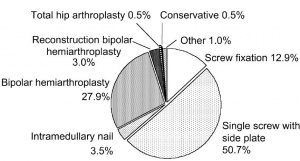
The management of hip fracture is usually a combination of surgery and rehabilitation. It also depends on the location of the fracture and whether it is displaced. In comparison to conservative management (bed rest and traction), operative management results in a reduced length of hospital stay and improved rehabilitation.[26] Surgery <48 hours after admission may be associated with lower morbidity and may decrease hospital stay.[27][28] It is associated with a 29% risk reduction in mortality as well as a significant reduction in in-hospital pneumonia (relative risk reduction 41%) and pressure sores (relative risk reduction 52%).[29][30]
Intracapsular Fractures
- Undisplaced: internal fixation with a dynamic hip screw, or multiple cannulated screws[31]
- Displaced
- For patients < 60 years of age, most surgeons favor early (<12-24 hours from injury) open reduction and internal fixation partly due to a potential increased risk of avascular necrosis to the femoral head. However, the evidence is conflicting regarding rates of avascular necrosis and timing of surgery.[32][33]
- For patients 60 to 80 years of age, management is controversial. Evidence from meta-analyses suggests that arthroplasty significantly reduces the risk of revision surgery at 1 year, does not increase the risk of mortality at 1 year, but significantly increases the risk of infection and blood loss, and increases operating time as compared with internal fixation. [34][35][36]
- For patients > 80 years of age, most surgeons favor arthroplasty[37][32]. Total hip arthroplasty may reduce pain and functional limitation more than hemiarthroplasty. [38][35][38]
Extracapsular Fractures
Surgical stabilization is standard treatment, and non-operative measures are only considered for patients who are at very high surgical risk or who have a limited life expectancy. The goal of surgery is to achieve a stable fracture reduction and fixation, allowing early weight bearing and mobilization of the patient. Non-operative management is only considered for non-ambulatory patients with minimal pain and for medically unstable patients with a major un-correctable comorbid disease or terminal illness.[6]For displaced intertronchanteric fractures, operative management includes internal fixation with either a dynamic hip screw,[39] or a cephalomedullary nail. [40] Dynamic hip screw is preferred because of decreased complication rate and reoperation rate.[41] [42]
Physical Therapy Management[edit | edit source]
In a study by Mangione et al, moderate to large improvements in physical performance and quality of life was found in patients who had a 10- week home-based progressive resistance exercise program[43] In another study, a meta-analyses, showed that balance training within 6 months improves person with hip fracture physical functioning, gait, lower limb strength, performance task, and activity of daily living.[44] Also, among patients who had completed standard rehabilitation after hip fracture, the use of a home-based functionally oriented exercise program resulted in modest improvement in physical function at 6 months after randomization.[45]
The patient training begins the day after surgery from a sitting position, with abducted hip during transfer from bed to chair.[46] ) On the second and third post-operative day the patient can start with walking between parallel bars, and later on, they can walk with a walker or a cane. A warming up on a stationary bicycle for 10 to 15 minutes is recommended.[47] Progressive weight-bearing as tolerated till full weight-bearing should start soon after surgery according to general physical status. When internal fixation is performed, partial weight-bearing is recommended for a period of 8–10 weeks (according to the radiological evaluation of fracture healing), and after 3 months full weight-bearing should be allowed. Range of motion exercises for the hip, knee and ankle. The patient can also begin strengthening exercises based on the surgeon's orders (typically six weeks post-op). Patients should also undergo balance and proprioceptive rehab and these abilities are quickly lost with inactivity.
Prolonged bed rest can increase the risk of pressure sores, atelectasis, pneumonia, deconditioning, and thromboembolic complications. Weight-bearing immediately after hip fracture surgery is safe in most patients.[48] Complications following hip surgery involve blood clots, pneumonia, wound infections, and more, all of which can be reduced with activity[49]
Another key component of rehabilitation following hip fracture is education on its prevention. Home safety to prevent falls, regular moderate exercise can slow bone loss and maintain muscle strength, also improve balance and coordination.
There are some important rules postoperative:
- internal rotation from hip flexion is very stressful for the joint
- impact activities should be avoided for six weeks postoperative
- depending on the surgical procedure is unloaded or partially loaded mobilize postoperatively crucial to the joint
- Avoid straight leg raise for 4 weeks postoperatively to not provoke irritation of the nerve
- Cardiovascular training is important
Weight-bearing exercises are very important for mobility, balance, activities of daily living and quality of life[50], examples: stepping in different directions, standing up and sitting down, tapping the foot and stepping onto and off a block.
For patients who underwent a prosthetic replacement have to avoid for approximately 12 weeks:
- Hip flexion greater than 70–90°
- External rotation of the leg
- Adduction of the leg past midline
- Should not bend forward from the waist more than 90
Rehabilitation program components[51]:
- Hip extension (theraband and manual exercise)
- Heel raises onto toes (theraband and manual exercise)
- Resisted rowing (double arm lifting) (theraband and manual exercise)
- Standing diagonal reach (theraband and manual exercise)
- Modified get up and go (theraband and manual exercise)
- Overhead arm extensions (theraband and manual exercise)
- Repeated chair stands (vest and manual exercise)
- Lunges - forward and back (vest and manual exercise)
- Stepping up and down step (vest, manual exercise and plyometric step)
- Calf raises - both legs and one leg (manual exercise)
Clinical Bottom Line[edit | edit source]
The number of hip fractures worldwide will increase up to 7-21 million incidences each year in 2050.[52] Mortality associated with a hip fracture is about 5-10% after one month. One year after fracture, about a third of patients will have died, compared with an expected annual mortality of about 10% in this age group.[52]Thus, only a third of the deaths are directly attributable to the hip fracture itself, but patients and relatives often think that the fracture has played a crucial part in the final illness. More than 10% of survivors will be unable to return to their previous residence. Most of the remainder will have some residual pain or disability. Most people who sustain the injury require surgery followed by a period of rehabilitation. Treatment is generally surgical to replace or repair the broken bone. Some loss of function is to be expected in most patients.
References[edit | edit source]
- ↑ Free dictionary Hip fracture: Available from:https://medical-dictionary.thefreedictionary.com/hip+fracture (last accessed 14.10.2020)
- ↑ 2.0 2.1 2.2 Radiopedia NOF fractures Available from:https://radiopaedia.org/articles/femoral-neck-fracture (last accessed 14.10.2020)
- ↑ 3.0 3.1 3.2 Antapur et al. Fractures in the elderly: when is a hip replacement a necessity? Clinical Interventions in Aging. 2011
- ↑ Tinetti ME, Kumar C. The patient who falls: “It's always a trade-off. JAMA. 2010 Jan 20;303(3):258–266.
- ↑ Marks R. Vitamin C and Hip Fractures-Review. EC Orthopaedics. 2020;11:33-41.
- ↑ 6.0 6.1 Bateman, Laura, et al. "Medical management in the acute hip fracture patient: a comprehensive review for the internist." The Ochsner Journal 12.2 (2012): 101-110.
- ↑ IOF Facts and stats Available from:https://www.iofbonehealth.org/facts-statistics#category-16 (last accessed 14.10.2020)
- ↑ 8.0 8.1 Zuckerman JD. Hip fracture. N Engl J Med. 1996 Jun 6;334(23):1519–1525.
- ↑ Canale ST. Campbell's Operative Orthopaedics. St. Louis, MO: Mosby;; 1998. pp. 2181–2223.
- ↑ Garden RS. The structure and function of the proximal end of the femur. J Bone Joint Surg Br. 1961 Aug;43B(3):576–589.
- ↑ 11.0 11.1 Rao, Shobha S., and Manjula Cherukuri. "Management of hip fracture: the family physician’s role." Am Fam Physician 73.12 (2006): 2195-2200.
- ↑ Dhibar DP, Gogate Y, Aggarwal S, Garg S, Bhansali A, Bhadada SK. Predictors and outcome of fragility hip fracture: A prospective study from North India. Indian journal of endocrinology and metabolism. 2019 May 1;23(3):282.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6683687/ (last accessed 14.10.2020)
- ↑ Grisso, Jeane Ann, et al. "Risk factors for falls as a cause of hip fracture in women." New England Journal of Medicine 324.19 (1991)
- ↑ http://www.mayoclinic.com/health/hip-fracture/DS00185/DSECTION=risk-factors (visited on april 2016)
- ↑ Banks E, Reeves GK, Beral V, Balkwill A, Liu B Roddam A. Million Women Study Collaborators. Hip fracture incidence in relation to age, menopausal status, and age at menopause: prospective analysis. PLoS Med. 2009 Nov;6(11) e1000181. Epub 2009 Nov 1.
- ↑ Angthong C, Suntharapa T, Harnroongroj T. [Major risk factors for the second contralateral hip fracture in the elderly] Acta Orthop Traumatol Turc. 2009 May-Jul;43(3):193–198. Turkish.
- ↑ Yang Y, Komisar V, Shishov N, Lo B, Korall AM, Feldman F, Robinovitch SN. The Effect Of Fall Biomechanics On Risk For Hip Fracture In Older Adults: A Cohort Study Of Video‐Captured Falls In Long‐Term Care. Journal of bone and mineral research. 2020 May 13.
- ↑ 18.0 18.1 Parker, Martyn, and Antony Johansen. "Hip fracture." British Medical Journal 7557 (2006): 27.
- ↑ 19.0 19.1 19.2 Dinçel, V. Ercan, et al. "The association of proximal femur geometry with hip fracture risk." Clinical Anatomy 21.6 (2008): 575-580.
- ↑ Magaziner J, Simonsick EM, Kashner TM, et al. Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol. 1990;45:M101-M107.
- ↑ Borgquist L, Ceder L, Thorngren KG. Function and social status 10 years after hip fracture. Prospective follow-up of 103 patients. Acta Orthop Scand. 1990;61:404-410.
- ↑ Marottoli RA, Berkman LF, Cooney LM Jr. Decline in physical function following hip fracture. J Am Geriatr Soc. 1992;40:861-866
- ↑ 23.0 23.1 Gretchen M Orosz et al., Association of Timing of Surgery for Hip Fracture and Patient Outcomes. JAMA. 2004;291(14):1738-1743.
- ↑ 24.0 24.1 Diamond TH et al., Hip fracture in elderly men: prognostic factors and outcomes. The Medical Journal of Australia [1997, 167(8):412-415]
- ↑ Jay Magaziner et al., Recovery from Hip Fracture in Eight Areas of Function. Journal of Gerontology: Medical Sciences 2000, Vol. 55A, No. 9, M498–M507.
- ↑ Handoll HH, Parker MJ. Conservative versus operative treatment for hip fractures in adults. Cochrane Database Syst Rev. 2008;(3):CD000337
- ↑ Mak JC, Cameron ID, March LM; National Health and Medical Research Council (Australia). Evidence-based guidelines for the management of hip fractures in older persons: an update. Med J Aust. 2010;192:37-41.
- ↑ Khan SK, Kalra S, Khanna A, et al. Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury. 2009;40:692-697.
- ↑ Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ. 2010;182:1609-1616
- ↑ Moja L, Piatti A, Pecoraro V, et al. Timing matters in hip fracture surgery: patients operated within 48 hours have better outcomes. A meta-analysis and meta-regression of over 190,000 patients. PLoS One. 2012;7:e46175
- ↑ Mak JC, Cameron ID, March LM; National Health and Medical Research Council (Australia). Evidence-based guidelines for the management of hip fractures in older persons: an update. Med J Aust. 2010;192:37-41
- ↑ 32.0 32.1 Bhandari M, Devereaux PJ, Tornetta P 3rd, et al. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg Am. 2005;87:2122-2130.
- ↑ Duckworth AD, Bennet SJ, Aderinto J, et al. Fixation of intracapsular fractures of the femoral neck in young patients: risk factors for failure. J Bone Joint Surg Br. 2011;93:811-816
- ↑ Bhandari M, Devereaux PJ, Swiontkowski MF, et al. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysis. J Bone Joint Surg Am. 2003;85-A:1673-1681.
- ↑ 35.0 35.1 Parker MJ, Gurusamy K. Internal fixation versus arthroplasty for intracapsular proximal femoral fractures in adults. Cochrane Database Syst Rev. 2006;(4):CD001708.
- ↑ Burgers PT, Van Geene AR, Van den Bekerom MP, et al. Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis and systematic review of randomized trials. Int Orthop. 2012;36:1549-1560.[
- ↑ National Institutes of Health (NIH). Osteoporosis prevention, diagnosis, and therapy. NIH Consens Statement. 2000;17:1-45.
- ↑ 38.0 38.1 Keating JF, Grant A, Masson M, et al. Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty. Health Technol Assess. 2005;9:iii-x, 1-65
- ↑ Johnell O, Kanis JA, Oden A, et al. Predictive value of BMD for hip and other fractures. J Bone Miner Res. 2005;20:1185-1194.
- ↑ De Laet C, Kanis JA, Oden A, et al. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int. 2005;16:1330-1338
- ↑ National Institute for Health and Care Excellence. Hip fracture: management. May 2017. http://www.nice.org.uk/ (last accessed 9 August 2017)
- ↑ Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2010;(9):CD000093
- ↑ Mangione KK, Craik RL, Palombaro KM, Tomlinson SS, Hofmann MT. Home-based leg-strengthening exercise improves function 1 year after hip fracture: a randomized controlled study. J Am Geriatr Soc. 2010 Oct. 58(10):1911-7.
- ↑ Wu JQ, Mao LB, Wu J. Efficacy of balance training for hip fracture patients: a meta-analysis of randomized controlled trials. Journal of orthopaedic surgery and research. 2019 Dec 1;14(1):83.
- ↑ Latham, Nancy K., et al. "Effect of a home-based exercise program on functional recovery following rehabilitation after hip fracture: a randomized clinical trial." Jama 311.7 (2014): 700-708.
- ↑ Luciani, D., et al. "The importance of rehabilitation after lower limb fractures in elderly osteoporotic patients." Aging clinical and experimental research 25.1 (2013): 113-115.
- ↑ Sylliaas, Hilde, et al. "Progressive strength training in older patients after hip fracture: a randomized controlled trial." Age and ageing (2011): afq167.
- ↑ Scheerlinck, T., et al. "Hip fracture treatment: outcome and socio-economic aspects: a one-year survey in a Belgian university hospital." Acta orthopaedica belgica 69.2 (2003): 145-156
- ↑ Daniel Pendick. ‘’After hip fracture, exercise at home boosts day-to-day function’’ Harvard health publication (2014)
- ↑ Edward Leblanc, k. i. m., and Leanne l. Leblanc. "Hip fracture: diagnosis, treatment, and secondary prevention." American family physician89.12 (2014).
- ↑ Latham, Nancy K., et al. "Effect of a home-based exercise program on functional recovery following rehabilitation after hip fracture: a randomized clinical trial." Jama 311.7 (2014): 700-708.
- ↑ 52.0 52.1 Kannus, P., et al. "Epidemiology of hip fractures." Bone 18.1 (1996): S57-S63.