Hill Sachs Lesion: Difference between revisions
Leana Louw (talk | contribs) No edit summary |
Leana Louw (talk | contribs) No edit summary |
||
| Line 56: | Line 56: | ||
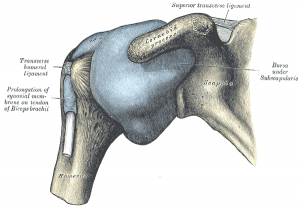
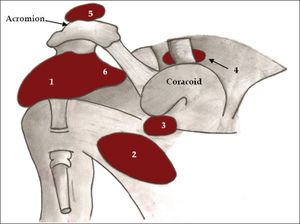
=== Bursae === | === Bursae === | ||
There are eight bursae in the shoulder complex as a result of the high amount of muscles surrounding the shoulder. They ensure a smooth contact between the muscle and the underlying structures. The subacromial bursa is the biggest in the body.<ref name="dodson" /> | There are eight bursae in the shoulder complex as a result of the high amount of muscles surrounding the shoulder. They ensure a smooth contact between the muscle and the underlying structures. The subacromial bursa is the biggest in the body.<ref name="dodson" /> | ||
[[File:Bursae shoulder joint normal.jpg|center|thumb|1. Subacromial-subdeltoid bursa; 2. Subscapular recess; 3. Subcoracoid bursa; 4. Coracoclavicular bursa; 5. Supra-acromial bursa; 6. Medial extension of subacromial-subdeltoid bursa.]] | |||
== Epidemiology/Etiology == | == Epidemiology/Etiology == | ||
| Line 90: | Line 91: | ||
* Humeral head palpable anteriorly | * Humeral head palpable anteriorly | ||
* All movements limited and painful | * All movements limited and painful | ||
* Coracoid process: Palpable fullness and positioned towards the axilla | * Coracoid process: Palpable fullness and positioned towards the axilla<span style="line-height: 1.5em;"></span> | ||
<span style="line-height: 1.5em;"></span> | |||
== Differential diagnosis == | == Differential diagnosis == | ||
* [http://www.physio-pedia.com/Bankart_lesion Bankart lesion]: | * [http://www.physio-pedia.com/Bankart_lesion Bankart lesion]: | ||
| Line 107: | Line 107: | ||
=== Physical examination === | === Physical examination === | ||
* [[Apprehension Test|Bony apprehension test]]: | * [[Apprehension Test|Bony apprehension test]]:<ref name="bushnell1" /> | ||
** Positive test: Pain/reflex muscle contraction (in case of sublaxation)<ref name="bushnell1" /> | ** Positive test: Pain/reflex muscle contraction (in case of sublaxation)<ref name="bushnell1" /> | ||
{{#ev:youtube|hy7zgoEsbzQ}} | {{#ev:youtube|hy7zgoEsbzQ}} | ||
* [http://www.physio-pedia.com/Jobes_Relocation_Test | * [http://www.physio-pedia.com/Jobes_Relocation_Test Jobe relocation test]: | ||
** Positive test: Apprehension | ** Positive test: Apprehension | ||
** Crepitus and catching may be felt during active and passive abduction and external rotation<ref name="provencher 2" /> | ** Crepitus and catching may be felt during active and passive abduction and external rotation<ref name="provencher 2" /> | ||
| Line 130: | Line 130: | ||
=== Outcome Measures === | === Outcome Measures === | ||
*[https://www.physio-pedia.com/DASH_Outcome_Measure Disabilities of the arm, shoulder and hand (DASH)] | |||
*[http://www.journalofphysiotherapy.com/article/S1836-9553(11)70045-5/fulltext Shoulder Pain and Disability Index (SPADI)] | |||
*[https://www.physio-pedia.com/Numeric_Pain_Rating_Scale Numeric Pain Rating Scale (NPRS)] | |||
== Medical management == | == Medical management == | ||
Management for humeral bone loss (as in Hill-Sachs lesion) can be directed at the restoration of the glenohumeral articular arc with either glenoid-based bone augmentation techniques (most commonly used), humeral-based strategies, or a combination. These strategies include open as well as arthroscopic procedures, depending on the extent of the pathology.<ref name="provencher 2" /> . Treating the glenoid defects is often the solution to the glenohumeral instability. | |||
Of these techniques, the (open) Latarjet procedure remains the most frequently applied procedure. This procedure includes a variety of methods. The technique whereby the bone from the processus coracoideus is used as an augment to the anteroinferior glenoid bone loss is the most common. By reforming the concavity and width of the glenoid, a Hill-Sachs lesion does not influence the anterior glenoid rim of unstable shoulders. This method is successful in preventing the overtime instability, proving at least two prospective cohort studies by Hovelius et al. (2004) and Schroder et al. (2006) (evidence based level: 1B). However, shoulder arthrosis and loss of function were negative consequences. <ref name="provencher 2" /><ref name="hovellus">Hovellus et. Al. Hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study 1 clinical results. J Shoulder Elbow Surg. 2004:13(5):509-516. (Level of evidence: 1B)</ref><ref name="schroder">Schroder et al. The modified Bristow procedure for anterior shoulder instability: 26-year outcomes in Naval Academy Midshipmen. American Journal Sports Medicine. 2006; 34(5):78-86. (Level of evidence: 1B)</ref> | Of these techniques, the (open) Latarjet procedure remains the most frequently applied procedure. This procedure includes a variety of methods. The technique whereby the bone from the processus coracoideus is used as an augment to the anteroinferior glenoid bone loss is the most common. By reforming the concavity and width of the glenoid, a Hill-Sachs lesion does not influence the anterior glenoid rim of unstable shoulders. This method is successful in preventing the overtime instability, proving at least two prospective cohort studies by Hovelius et al. (2004) and Schroder et al. (2006) (evidence based level: 1B). However, shoulder arthrosis and loss of function were negative consequences. <ref name="provencher 2" /><ref name="hovellus">Hovellus et. Al. Hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study 1 clinical results. J Shoulder Elbow Surg. 2004:13(5):509-516. (Level of evidence: 1B)</ref><ref name="schroder">Schroder et al. The modified Bristow procedure for anterior shoulder instability: 26-year outcomes in Naval Academy Midshipmen. American Journal Sports Medicine. 2006; 34(5):78-86. (Level of evidence: 1B)</ref> | ||
The majority of Hill-Sachs defects can successfully be solved with glenoid-based strategies, however, some of the Hill-Sachs injuries, especially when the glenoid is not touched, require a direct treatment of the injury. Generally taken, the Hill-Sachs deformity can be managed by two techniques: arthrosocopic and open techniques.<ref name="provencher 2" /> | The majority of Hill-Sachs defects can successfully be solved with glenoid-based strategies, however, some of the Hill-Sachs injuries, especially when the glenoid is not touched, require a direct treatment of the injury. Generally taken, the Hill-Sachs deformity can be managed by two techniques: arthrosocopic and open techniques.<ref name="provencher 2" /> | ||
CT scans make it possible to reliably asses the location and depth of the humeral lesion. Based on the latter, a surgical decision is made. Overall, sagittal- and axial-plane measurements are more accurate for evaluation of these defects than the coronal plane.<ref name="kodali" /> | |||
* '''Arthroscopic techniques:''' include the ‘Remplissage procedure’, a method whereby the defect is filled with soft tissue, usually from the infraspinatus tendon. A second arthroplasty method is the percutaneous humeroplasty, a technique that fills the lesion by using a bone tamp brought into a drilled osseus window 180 degrees from the lesion. The advantage of this procedure is that no rotational osteotomy of the humeral head is needed and the humeral head can be restored without transpositioning the soft tissue. Limitations of this technique are moderate-sized defects and the lack of management of osteochondral defects. Other procedures where arthroscopy intervenes are techniques that use various small bone plugs.<ref name="provencher 2" /> | * '''Arthroscopic techniques:''' include the ‘Remplissage procedure’, a method whereby the defect is filled with soft tissue, usually from the infraspinatus tendon. A second arthroplasty method is the percutaneous humeroplasty, a technique that fills the lesion by using a bone tamp brought into a drilled osseus window 180 degrees from the lesion. The advantage of this procedure is that no rotational osteotomy of the humeral head is needed and the humeral head can be restored without transpositioning the soft tissue. Limitations of this technique are moderate-sized defects and the lack of management of osteochondral defects. Other procedures where arthroscopy intervenes are techniques that use various small bone plugs.<ref name="provencher 2" /> | ||
| Line 150: | Line 147: | ||
<br> | <br> | ||
== | == Physiotherapy management == | ||
Several studies have shown that when the number of dislocations increases, the incidence and size of Hill Sachs lesion also increases. It can be a cause of instability and in this case, surgical treatment is considered. Frequently, authors consider that surgical treatment of recurrent shoulder dislocation is indicated when someone had more than five shoulder dislocations.<ref name="cetik" /><ref name="cutts">Cutts, S., Prempeh, M. & Drew, S. Anterior shoulder dislocation, Ann R coll Surg Engl. 2009: 91 (Level of evidence: 2A)</ref> | Several studies have shown that when the number of dislocations increases, the incidence and size of Hill Sachs lesion also increases. It can be a cause of instability and in this case, surgical treatment is considered. Frequently, authors consider that surgical treatment of recurrent shoulder dislocation is indicated when someone had more than five shoulder dislocations.<ref name="cetik" /><ref name="cutts">Cutts, S., Prempeh, M. & Drew, S. Anterior shoulder dislocation, Ann R coll Surg Engl. 2009: 91 (Level of evidence: 2A)</ref> | ||
| Line 168: | Line 165: | ||
In patients with small defects (< 20% Hill Sachs lesion), nonoperative treatment is recommended. These patients will be immobilized with a sling (2-6 weeks). After this, immobilization, a physical therapist must mobilize the joint. Patients will start with pendulum exercises, followed by passive, active-assisted and active range of motion exercises. Abduction and external rotation is restricted during the initial phase of the rehabilitation, because the ligaments need time to heal, like this we want to prevent other dislocations as well. The patient will do exercises to strengthen the deltoid muscle, the periscapular muscles (pectoralis major) and the rotator cuff muscles. Recent related evidence of A.L Chen et al proofs that the long-term success rate of nonoperative treatment is very high. (Level of evidence 3A)<ref name="andrew" /> | In patients with small defects (< 20% Hill Sachs lesion), nonoperative treatment is recommended. These patients will be immobilized with a sling (2-6 weeks). After this, immobilization, a physical therapist must mobilize the joint. Patients will start with pendulum exercises, followed by passive, active-assisted and active range of motion exercises. Abduction and external rotation is restricted during the initial phase of the rehabilitation, because the ligaments need time to heal, like this we want to prevent other dislocations as well. The patient will do exercises to strengthen the deltoid muscle, the periscapular muscles (pectoralis major) and the rotator cuff muscles. Recent related evidence of A.L Chen et al proofs that the long-term success rate of nonoperative treatment is very high. (Level of evidence 3A)<ref name="andrew" /> | ||
Based on this information the authors will be able to design a treatment program and start physiotherapy.<br><br> | Based on this information the authors will be able to design a treatment program and start physiotherapy.<br><br> | ||
<br><br> | |||
== Resources == | == Resources == | ||
== Clinical bottom line == | == Clinical bottom line == | ||
| Line 189: | Line 182: | ||
A study by Arciero et al. proves that combined humeral and glenoid bone defects have a negative effect on the glenohumeral stability. (Level of evidence 5)<ref name="arciero">Arciero RA et al., The Effect of a Combined Glenoid and Hill-Sachs Defect on Glenohumeral Stability: A Biomechanical Cadaveric Study Using 3-Dimensional Modeling of 142 Patients. The American journal of sports medicine, July 2014. (Level of evidence 5)</ref> | A study by Arciero et al. proves that combined humeral and glenoid bone defects have a negative effect on the glenohumeral stability. (Level of evidence 5)<ref name="arciero">Arciero RA et al., The Effect of a Combined Glenoid and Hill-Sachs Defect on Glenohumeral Stability: A Biomechanical Cadaveric Study Using 3-Dimensional Modeling of 142 Patients. The American journal of sports medicine, July 2014. (Level of evidence 5)</ref> | ||
== References == | == References == | ||
Revision as of 22:08, 27 August 2018
Original Editors - Lien Hennebel
Top Contributors - Jelle Van Hemelryck, Lien Hennebel, Leana Louw, Pauline Bouten, Simisola Ajeyalemi, Uchechukwu Chukwuemeka, Lucinda hampton, Shreya Pavaskar, Admin, Kim Jackson, Rachael Lowe, Fasuba Ayobami, Wanda van Niekerk, Nupur Smit Shah, 127.0.0.1 and Claire Knott
**Editing in process - Come back later for updated page***
Definition/Description[edit | edit source]
A Hill-Sachs lesion is a compression fracture or "dent" of the posterosuperolateral humeral head that occurs in association with anterior instability or dislocation of the glenohumeral joint.[1][2] It was first described by two radiologists by the name HA Hill and MD Sachs in 1940.[2] This lesion is caused by an anterior shoulder dislocation which causes a humeral head impression fracture. The posterolateral aspect of the humeral head impacts on the anterior glenoid in the dislocated position, causing instability at the glenohumeral joint.[3][4][5]
Clinically relevant anatomy[edit | edit source]
The glenohumeral joint is a synovial ball-and-socket diarthroidal joint. It is the articulation between the glenoid of the scapula and the head of humerus. It is commonly known that the shoulder joint has a loose capsule, making it the most commonly dislocated joint in the human body, of which 90% of these dislocations are anterior. This is a result of the scapular orientation of about 30 degrees anterior to the frontal plane of the body. The humerus is thus anteriorly orientated to the glenoid in the glenohumeral joint.[5][6][7]
This is a brief overview of the relevant anatomy. See the page for the glenohumeral joint for detailed information.
Bones[edit | edit source]
The glenoid of the scapula articulates with the humeral head to form a ball-and-socket joint.[6]
Labrum[edit | edit source]
The labrum, a fibrocartilaginous structure, surrounds the glenoid to ensure that there is enough contact between the surface of the glenoid and the humeral head. There is a concavity compression mechanism which plays an important role in the stability of the shoulder. The less contact there is, the higher the chance for dislocations.[8]
Ligaments[edit | edit source]
- Glenohumeral ligaments (pars superior, media and inferior): Assists in strengthening of the capsule[3]
- Coracohumeral ligament: Assists in strengthening of the capsule[3]
- Transversal humeral ligament: Functions with the Biceps Brachii muscle[6]
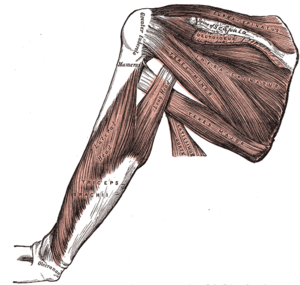
Muscles[edit | edit source]
- Abductors:
- Adductors:
- Pectoralis major
- Flexors:
- Rotator cuff (very important for the stability of the articulating humerus):
- Extensors:
- Internal Rotators:
- External Rotators:
Bursae[edit | edit source]
There are eight bursae in the shoulder complex as a result of the high amount of muscles surrounding the shoulder. They ensure a smooth contact between the muscle and the underlying structures. The subacromial bursa is the biggest in the body.[5]
Epidemiology/Etiology[edit | edit source]
Epidemiology[edit | edit source]
The incidence of Hill-Sachs lesions are approximately 40%-90% of all anterior shoulder instability cases, and even as high as 100% in patients with recurrent anterior instability.[1] A study looking at this found Hill-Sachs lesions in 65% of acute dislocations and 93% in patients with recurrent instability.[9]
A Hill-Sachs lesion occurs in about 50% of the first-time shoulder dislocations. For people with a shoulder dislocations history (i.e. shoulder instability) humeral head compression fractures are present in most cases.[10][11]
Etiology[edit | edit source]
- Anterior shoulder instability:
- Approximately 47% of the lesions are associated with the initial shoulder instability according to research studies)[12]
- Bankart lesion[13]
- 2.5 times more likely to for someone with either of those lesions to have the other as well[14]
- Anterior glenoid bone loss (in cases of recurrent instability)[15]
Characteristics/Clinical presentation[edit | edit source]
Classification[edit | edit source]
Classification systems are used to describe the amount of damage to the anterior capsule and the labrum, reflected by the depth of the lesion. Higher grade lesions are associated with increased risk of recurrent dislocation.[1][2][12]
- Grade 1: Defect in the articular surface down to (but not including) the subchondral bone
- Grade 2: Lesion includes the subchondral bone
- Grade 3: Lesion causes large defect in the subchondral bone.
Further classification can be done by looking at the percentage of the defect of humeral head involvement in the compression fracture.[16] The size of the lesion correlates in most cases to the number of previous dislocations.[11]
- Minor: <20%
- Moderate: 20%-45%
- Severe: >45%
Clinical presentation[edit | edit source]
Shoulder dislocation rarely occur isolated. It causes damage to different tissues surrounding the glenohumeral joint, such as ligaments, rotator cuff tendons, joint capsule as well as the bone and cartilage of the humeral head. This occurs when the round humeral head is forcibly impacted on the edge of the glenoid, which causes compression fractures in the humeral head. This forms a dimple structure on the articular surface of the humerus - a Hill-Sachs lesion.[17][18][10] This is always caused by dislocation, not only sublaxation.[17]
According to the page on shoulder dislocations, the following indicates an acute anterior glenohumeral dislocation:
- Arm held in abduction and external rotation
- Loss of normal contour of the deltoid and acromion prominent posteriorly and laterally
- Humeral head palpable anteriorly
- All movements limited and painful
- Coracoid process: Palpable fullness and positioned towards the axilla
Differential diagnosis[edit | edit source]
- Bankart lesion:
- Pseudo-Hill-Sachs lesion:
- It is normal that below the level of the coracoid the humeral head normally flattens out, and should not be mistaken as a Hill-Sachs lesion[18]
- Humeral avulsion fractures[11]
- Mid capsular tears[11]
- Floating anterior capsule[11]
- Reverse Hill-Sachs lesion:
Diagnostic Procedures[edit | edit source]
Physical examination[edit | edit source]
- Bony apprehension test:[7]
- Positive test: Pain/reflex muscle contraction (in case of sublaxation)[7]
- Jobe relocation test:
- Positive test: Apprehension
- Crepitus and catching may be felt during active and passive abduction and external rotation[3]
- Possible lesion indicated by audible/palpable clunk in active/passive abduction and external rotation or an unstable feeling during mid-range
Special investigations[edit | edit source]
- X-ray: [3][19]
- Grashey view (AP) in internal and external rotation; transcapular view (X-ray beam caudally from standard AP view); axillary views with exaggerated external rotation and West Pont views (if pain allows)
- Important first step at effectively evaluating the glenohumeral relationship as well as osseous pathology of the humerus and the glenoid
- Can detect bony lesions related to shoulder instability in the acute phase
- Difficult to see Hill-Sachs lesion
- Ultrasound:[19][20]
- Detect and localize a compression fracture
- Cost-effective, minimal exposure to excessive radiation, comfortable for patient
- Hill-Sachs lesions: Apparent triangular depression in the contour of the humerus[4]
- CT-scan: Reliably asses the location and depth of the humeral lesion[21]
- MRI: Detect pathology of the soft tissue; determine the amount of humeral and glenoid bone loss[21][22]
Outcome Measures[edit | edit source]
- Disabilities of the arm, shoulder and hand (DASH)
- Shoulder Pain and Disability Index (SPADI)
- Numeric Pain Rating Scale (NPRS)
Medical management[edit | edit source]
Management for humeral bone loss (as in Hill-Sachs lesion) can be directed at the restoration of the glenohumeral articular arc with either glenoid-based bone augmentation techniques (most commonly used), humeral-based strategies, or a combination. These strategies include open as well as arthroscopic procedures, depending on the extent of the pathology.[3] . Treating the glenoid defects is often the solution to the glenohumeral instability.
Of these techniques, the (open) Latarjet procedure remains the most frequently applied procedure. This procedure includes a variety of methods. The technique whereby the bone from the processus coracoideus is used as an augment to the anteroinferior glenoid bone loss is the most common. By reforming the concavity and width of the glenoid, a Hill-Sachs lesion does not influence the anterior glenoid rim of unstable shoulders. This method is successful in preventing the overtime instability, proving at least two prospective cohort studies by Hovelius et al. (2004) and Schroder et al. (2006) (evidence based level: 1B). However, shoulder arthrosis and loss of function were negative consequences. [3][23][24]
The majority of Hill-Sachs defects can successfully be solved with glenoid-based strategies, however, some of the Hill-Sachs injuries, especially when the glenoid is not touched, require a direct treatment of the injury. Generally taken, the Hill-Sachs deformity can be managed by two techniques: arthrosocopic and open techniques.[3]
CT scans make it possible to reliably asses the location and depth of the humeral lesion. Based on the latter, a surgical decision is made. Overall, sagittal- and axial-plane measurements are more accurate for evaluation of these defects than the coronal plane.[20]
- Arthroscopic techniques: include the ‘Remplissage procedure’, a method whereby the defect is filled with soft tissue, usually from the infraspinatus tendon. A second arthroplasty method is the percutaneous humeroplasty, a technique that fills the lesion by using a bone tamp brought into a drilled osseus window 180 degrees from the lesion. The advantage of this procedure is that no rotational osteotomy of the humeral head is needed and the humeral head can be restored without transpositioning the soft tissue. Limitations of this technique are moderate-sized defects and the lack of management of osteochondral defects. Other procedures where arthroscopy intervenes are techniques that use various small bone plugs.[3]
- Open humeral bony techniques include autologous bone plugs, size-matched osteoarticular allografts and rotational humeral osteotomy. The latter, a procedure that includes an osteotomy of the surgical neck and rotates the humeral head for 25 degrees, is not the best chosen method nowadays, given the related risks and the success rates of more recent procedures. The osseus humeral allograft bone plug technique uses a size-matched humeral bone plug of a donor. It is an open procedure because it is performed through a delto-pectoral approach or a deltoid-splitting approach. Advantages of this procedure are its minimal exposure and the fact that the head of the humerus remains in the capsule. A downside of this resurfacing technique is its limitation to small and moderate lesions and the risk of using cadaveric tissue.[3]
Physiotherapy management[edit | edit source]
Several studies have shown that when the number of dislocations increases, the incidence and size of Hill Sachs lesion also increases. It can be a cause of instability and in this case, surgical treatment is considered. Frequently, authors consider that surgical treatment of recurrent shoulder dislocation is indicated when someone had more than five shoulder dislocations.[16][25]
But most of the time a Hill-Sachs lesion can be neglected, certainly, if there is a minimum of glenoid bone loss and without significant involvement of the humeral head. There is no need for surgical treatment, but important is handling the instability.[16] The non-operative rehabilitation of the unstable shoulder consists about seven key factors:[26]
- The onset of pathology (in this case: traumatic event)
- The degree of instability (in this case: dislocation)
- The frequency of dislocation (in this case acute)
- TheDirection of instability (in this case: anterior)
- Concomitant pathologies (in this case: Hill Sachs lesion)
- Neuromuscular control
- Activity level
In the non-operative rehabilitation program of the traumatic dislocation of the shoulder, it's important to consider all these seven factors and thus also with the concomitant 'Hill Sachs lesion': rehabilitation program of the shoulder.[26]
According to a study from A. L. Chen (Level of evidence 3A), you can treat a Hill Sachs lesion nonoperatively. Therapy aims to prevent reoccurrence of dislocations. So the therapy is based on strengthening the deltoid muscle and the rotator cuff muscles and periscapular muscles.[27]
In patients with small defects (< 20% Hill Sachs lesion), nonoperative treatment is recommended. These patients will be immobilized with a sling (2-6 weeks). After this, immobilization, a physical therapist must mobilize the joint. Patients will start with pendulum exercises, followed by passive, active-assisted and active range of motion exercises. Abduction and external rotation is restricted during the initial phase of the rehabilitation, because the ligaments need time to heal, like this we want to prevent other dislocations as well. The patient will do exercises to strengthen the deltoid muscle, the periscapular muscles (pectoralis major) and the rotator cuff muscles. Recent related evidence of A.L Chen et al proofs that the long-term success rate of nonoperative treatment is very high. (Level of evidence 3A)[27]
Based on this information the authors will be able to design a treatment program and start physiotherapy.
Resources[edit | edit source]
Clinical bottom line[edit | edit source]
A Hill Sachs lesion is an injury that mostly is secondary to a shoulder dislocation. The humeral head ‘collides’ with the anterior part of the cavitas glenoidale, this often causes a lesion, bone loss, defect and deformity of the humeral head. There are different grades (3) in the severity of the lesion, these grades are described in the definition. The incidence of Hill Sachs lesion in patients with anterior shoulder instability approaches 100%. A Hill Sachs lesion is a deformity or a type of fracture that change the shape of the humeral head. This may cause a change in the range of motion. Other symptoms are instability feeling, pain. (Level of evidence 2A)[1] (Level of evidence 2B)[12]
The most common dislocation in the glenohumeral joint is an anterior dislocation. Secondary to this injury there may occur a Hill Sachs lesion. When the patient got a fracture in the humeral head caused by a posterior dislocation, then it is called a reverse Hill Sachs lesion. Level of evidence 2A)[1]
Conservative treatment is only recommended in cases of small bony defects (Less than 20% Hill sachs lesion), in other cases (larger and more significant lesions), surgical treatment is needed. Elderly people or people with high medical risk may be best treated nonsurgically. The conservative treatment should be based on strengthening the deltoid, the rotator cuff muscles and scapular stabilizers.(Level of evidence 2A)[1] (Level of evidence 3A)[27]
Another pathology secondary to an anterior shoulder dislocation is a bankart lesion. This is not located at the humeral head like a Hill Sachs lesion, but this is an injury of the anterior glenoid labrum of the shoulder. When people got a Hill Sachs lesion, it is often accompanied by a Bankart lesion. (Level of evidence 2B)[14]
A study by Arciero et al. proves that combined humeral and glenoid bone defects have a negative effect on the glenohumeral stability. (Level of evidence 5)[28]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Provencher MT, Frank RM, LeClere LE, Metzger PD, Ryu JJ, Bernhardson A, Romeo AA. The Hill-Sachs lesion: diagnosis, classification, and management. Journal of the American Academy of Orthopaedic Surgeons 2012;20(4):242-52.
- ↑ 2.0 2.1 2.2 Shoulder Doc. Hill-Sachs Lesion. https://www.shoulderdoc.co.uk/article/1470 (accessed 26/08/2018).
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Provencher M, Rose M, Peace W. Hill-Sachs Injuries of the Shoulder: When are these important and how should I manage them? In: Abrams JS editor. Management of the unstable shoulder: arthroscopic and open repair. Slack Incorporated, 2011.p.235-252.
- ↑ 4.0 4.1 Castro WHM, Jerosch J, Grossman TV. Examination and diagnosis of musculoskeletal disorders. Georg Thieme Verlag: Germany, 2001.
- ↑ 5.0 5.1 5.2 Dodson CC, Cordasco FA. Anterior glenohumeral joint dislocations. Orthopedic Clinics of North America 2008;39(4):507-18.
- ↑ 6.0 6.1 6.2 6.3 Gray’s Anatomy, Anatomy of the human body. 11th edition, 1918.
- ↑ 7.0 7.1 7.2 Bushnell B, Creighton R, Herring M. The bony apprehension test for instability of the shoulder: a prospective pilot analysis. Arthroscopy 2008:24(9):974-82.
- ↑ Dutton, M. Orthopaedic: Examination, evaluation, and intervention (2nd ed.). New York: The McGraw-Hill Companies, 2008.
- ↑ Yiannakopoulos CK, Mataragas E, Antonogiannakis E. A comparison of the spectrum of intra-articular lesions in acute and chronic anterior shoulder instability. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 2007;23(9):985-90.
- ↑ 10.0 10.1 10.2 10.3 10.4 Wiki Radiography. Hill-Sachs and Bankart lesion, http://www.wikiradiography.net/page/Hill-Sachs+and+Bankart+Lesions (accessed 27/08/2018).
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 Savoie F, O’Brien M. Management of Hill-Sachs Lesion, International Congress for Joint Reconstruction, 2014.
- ↑ 12.0 12.1 12.2 Calandra JJ, Baker CL, Uribe J. The incidence of Hill-Sachs lesions in initial anterior shoulder dislocations. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 1989;5(4):254-7.
- ↑ Horst K, Von Harten R, Weber C, Andruszkow H, Pfeifer R, Dienstknecht T, Pape HC. Assessment of coincidence and defect sizes in Bankart and Hill–Sachs lesions after anterior shoulder dislocation: a radiological study. The British journal of radiology, 2014;87(1034):20130673.
- ↑ 14.0 14.1 Widjaja AB, Tran A, Bailey M, Proper S. Correlation between Bankart and Hill‐Sachs lesions in anterior shoulder dislocation. ANZ journal of surgery, 2006;76(6):436-8.
- ↑ Kim DS, Yoon YS, Yi CH. Prevalence comparison of accompanying lesions between primary and recurrent anterior dislocation in the shoulder. The American journal of sports medicine, 2010;38(10):2071-6.
- ↑ 16.0 16.1 16.2 Cetik O, Uslu M, Ozsar BK. The relationship between Hill-Sachs lesion and recurrent anterior shoulder dislocation. Acta orthopaedica belgica, 2007;73(2):175-8.
- ↑ 17.0 17.1 17.2 Cluett J. Hill-Sachs Injury: Damage to the shoulder joint as result of dislocation. Orthopedics, 2013.
- ↑ 18.0 18.1 18.2 18.3 18.4 Radiopedia. Hill-Sachs lesion. https://radiopaedia.org/articles/hill-sachs-lesion (accessed 27/08/2018).
- ↑ 19.0 19.1 Omoumi P, Teixeira P, Lecouvet F, Chung CB. Glenohumeral joint instability. Journal of Magnetic Resonance Imaging, 2011;33(1):2-16.
- ↑ 20.0 20.1 Kodali P, Jones MH, Polster J, Miniaci A, Fening SD. Accuracy of measurement of Hill-Sachs lesions with computed tomography. Journal of shoulder and elbow surgery, 2011;20(8):1328-34.
- ↑ 21.0 21.1 Pancione L, Gatti G, Mecozzi B. Diagnosis of Hill-Sachs lesion of the shoulder: comparison between ultrasonography and arthro-CT. Acta Radiologica, 1997;38(4):523-6.
- ↑ Pavic R, Margetic P, Bensic M, Brnadic RL. Diagnostic value of US, MR and MR arthrography in shoulder instability. Injury, 2013;44:S26-32.
- ↑ Hovellus et. Al. Hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study 1 clinical results. J Shoulder Elbow Surg. 2004:13(5):509-516. (Level of evidence: 1B)
- ↑ Schroder et al. The modified Bristow procedure for anterior shoulder instability: 26-year outcomes in Naval Academy Midshipmen. American Journal Sports Medicine. 2006; 34(5):78-86. (Level of evidence: 1B)
- ↑ Cutts, S., Prempeh, M. & Drew, S. Anterior shoulder dislocation, Ann R coll Surg Engl. 2009: 91 (Level of evidence: 2A)
- ↑ 26.0 26.1 Wilk, K., Macrina, L., Reinold, M. Non-operative rehabilitation for traumatic and atraumatic glenohumeral instability. North american journal of sports physical therapy. 2006; 1 (1): 16-31. (Level of evidence: 1B)
- ↑ 27.0 27.1 27.2 Andrew L. Chen et al. Glenohumeral Bone Loss and Anterior Instability, Bulletin of the NYU hospital for joint diseases, 2006 (Level of evidence 3A)
- ↑ Arciero RA et al., The Effect of a Combined Glenoid and Hill-Sachs Defect on Glenohumeral Stability: A Biomechanical Cadaveric Study Using 3-Dimensional Modeling of 142 Patients. The American journal of sports medicine, July 2014. (Level of evidence 5)
Sites
http://www.eorif.com/hill-sachs-lesion
http://orthodoc.aaos.org/
http://orthopedics.about.com/
www.wikiradiography.com