Hypermobility Syndrome
Original Editors - Free Picke
Top Contributors - Julie Schuermans, Emma Guettard, Free Picke, Blondeel Jonathan, Uchechukwu Chukwuemeka, Admin, Simisola Ajeyalemi, Kim Jackson, WikiSysop, 127.0.0.1, Wanda van Niekerk and Kirenga Bamurange Liliane Read more.
Search Strategy[edit | edit source]
Search on Pubmed and Pedro with keywords: “hypermobility”, “hypermobility syndrome” , “hypermobility ”and “therapy”. Search in libraries books about sport injuries, sports medicine, sport anatomy.
Definition/Description
[edit | edit source]
The hypermobility syndrome(HMS) was first described in 1967 by Kirk et al as the occurrence of musculoskeletal symptoms in hypermobile in healthy persons.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Meanwhile, other names are given to HMS, such as joint hypermobility syndrome and benign hypermobility joint syndrome. HMS is a dominant inherited connective tissue disorder described as “generalized articular hypermobility, with or without subluxation or dislocation.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The primary symptom is excessive laxity of multiple joints. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Hypermobility syndrome is different from localized joint hypermobility and other disorders that have generalized joint hypermobility, such as Ehlers-Danlos Syndrome, Rheumatoid Arthritis, Systemic Lupus Erythematosus, and Marfan Syndrome.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title HMS may occur also in chromosomal and genetic disorders such as Down syndrome and in metabolic disorders such as homocystinuria and hyperlysinemia.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Laboratory tests are used to exclude these other systemic disorders when HMS is suspected.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Clinically Relevant Anatomy[edit | edit source]
The pathophysiology in Hypermobility Syndrome is not yet fully understood, it appears to be a systemic collagen abnormality. The abnormality in collagen ratios is related with joint hypermobility and laxity of other tissues. The ratio of collagen (type I,II and III) is decreased in skin.
The diagnostic criteria for HMS includes joint abnormalities but it also affects cardiac tissue, smooth muscle in the female genital system and the gastrointestinal system. HMS also affects the joint position sense.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Epidemiology /Etiology[edit | edit source]
Joint hypermobility happen most often in children and reduce with age.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Joint mobility is highest at birth, there is a decrease in children around nine to twelve years old.
In adolescent girls there is a peak at the age of fifteen years, after this age the joint mobility decreases, as well in boys as in girls. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Hormonal changes that occur in puberty by adolescent girls, will influence the joint mobility.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
In general, hypermobility is more common in children than adults, is more common in girls than in boys Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title, more common in Asian, African and middle eastern people. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Characteristics/Clinical Presentation[edit | edit source]
_ Acute or Traumatic'
▫ Sprains
— recurrent ankle sprains
▫Meniscus tears
▫ Acute or recurrent dislocations or subluxations of the:
— shoulder
— patella
— metacarpophalangeal joint
— temporomandibular joint
▫ Traumatic arthritis
▫Bruising
▫ Fractures
_ Chronic or Nontraumatic
▫ S'oft tissue rheumatism
— tendinitis
— epicondylitis
— rotator cuff syndrome
— synovitis
— juvenile episodic synovitis
— bursitis
▫ Chondromalacia
▫ Back pain
▫ Scoliosis
▫ Fibromyalgia
▫ Temporomandibular joint dysfunction
▫ Nerve compression disorders
— carpal tunnel syndrome
— Tarsal_Tunnel_Syndrome
— acroparesthesia
— thoracic outlet syndrome
▫ Raynaud syndrome
▫ Flat feet and sequelae
▫Unspecified arthralgia or effusion of affected joint(s)
(foot, ankle, knee, hip, back, neck, shoulder, elbow,
wrist, finger)
▫ Osteoarthritis
▫ Delayed motor development
▫ Congenital hip dislocation
Differential Diagnosis[edit | edit source]
The signs and symptoms of hypermobility syndrome are variable. Most commonly, the initial complaint in a hypermobile patient is joint pain, which may affect one or multiple joints and may be generalized or symmetric. Primary care physicians can use the five simple questions to aid in recognizing hypermobility.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Other complaints are muscle cramps[1] ( after physical activity) and joint stiffness. People with HS can suffer from subluxations and dislocations. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Diagnostic Procedures[edit | edit source]
- Brighton criteria:
Major Criteria:
- Beighton Score of ≥ 4/9
- Arthralgia for > 3 months in > 4 joints
Minor Criteria:
- Beighton score of 1–3
- Arthralgia in 1–3 joints
- History of joint dislocation
- Soft tissue lesions >3
- Marfan-like habitus
- Skin striae, hyperextensibility or scarring
- Eye signs, lid laxity
- History of varicose veins, hernia, visceral prolapse
For a diagnosis to be made either both of the the major criteria must be present or 1 major and 2 minor or 4 minor.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Requirement for diagnosis of hypermobility syndrome:
- 2 major criteria
- 1 major criteria + 2 minor criteria
- 4 minor criteria
- 2 minor criteria and unequivocally affected first-degree relative in family history
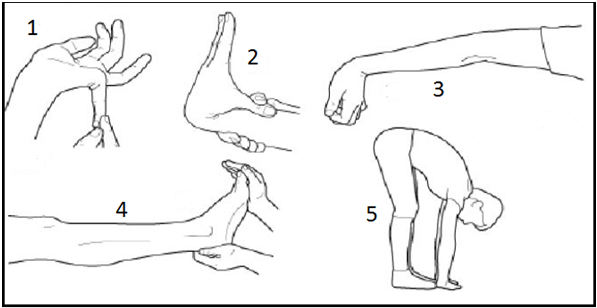
Another tests that the physiotherapist can do is: 'The Beighton score' Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- A passive dorsiflexion of the little finger above 90degrees (1 point for each hand).
- Bringing the thumb passive against the ventral side of the forearm (1 point for each thumb).
- Hyperextension of the elbow above 10 degrees ( 1 point for each elbow)
- Hyperextension of the knee above 10 degrees (1 point for each knee)
- Flexion of the trunk, whit knees straight and the palms flat on the ground ( 1 point)
According to the Beighton and Horan criteria, generalized joint laxity is present when four or more of five tests are positive, including contralateral knee hyperextension.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title In fact there is no universal agreement on a threshold for BJHMS, some researchers use a Beighton scale score of 5/9, other researchers use a score of 6/9 and still others use a modified score of 3/9.
Kinesiophobia: Tampa Scale for Kinesiophobia (TSK-I) is a questionnaire to measure pain and pain-related fear of movement. It can be used for patients with musculoskeletal complaints. This questionnaire has two sub-scales: “evaluating activity avoidance” ( a belief that activities who cause pain should be avoided) and “harm” (a belief that pain is a sign of damage of the body).[2]
Fatigue: Fatique Severity Scale (FSS) is a scale that quantifies the fatique intensity. This scale has a hight internal consistency and validity. FSS excist out 9 items with a 7-point response format that indicates the degree of agreement with each item.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Pain: Numeric Rating Scale (NRS) is a 11-point numeric scale to roughly measure any kind of pain.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Quality of Life: The Medical Outcome Study 36-item Short Form Health Survey (SF-36) is a survey to evaluate aspects of health that are most closely related to quality of life. It consist of 36 questions that measure 8 domains: body pain, physical functioning, physical limitations, general health, vitality, social functioning, emotional limitations and mental health.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Outcome Measures[edit | edit source]
- Range of motion Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - joint integrity and mobilityCite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - muscle performanceCite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - function and muscle strengthCite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - visual analog scale was used to assess musculoskeletal pain.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - quality of life was evaluated by a Short Form 36 questionnaire (SF-36).Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
add links to outcome measures here (also see Outcome Measures Database)
Examination[edit | edit source]
- ROM: Norkin and WhiteCite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - End feelCite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Manual testingCite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
add text here related to physical examination and assessment
Medical Management
[edit | edit source]
For HMS, there is no medical management. To control pain you can use NSAIDs (Non-steroidal anti-inflammatory drugs) or acetaminophen.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Physical Therapy Management
[edit | edit source]
The aim of physical therapy in hypermobility syndrome, is to approach the muscle inhibition, atrophy and the reduced joint control caused by the joint pain. Another important step of treating hypermobility syndrome is education. Without this education patients will continue to go over the normal joint range and their extreme joint range can cause a more unstable joint. Fatigue, anxiety and depression are sometimes associated with HMS, and we must try to ameliorate their quality of life. It is necessarily to encourage an active lifestyle, so give for example a schedule with exercises to fulfill at least 3 times a week. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title (Level of Evidence: 2A)
Treatment overview:
- Education of hypermobility syndrome
- Activity modification
- Streching affected joint
- strengthening excercises for affected joint
- osteopathic manipulative treatmentCite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title
Active mobilisation exercises: shoulder rolls, arm circles, neck rotations, neck lateral flexions, wrist circles, side flexions of spine, thoracic rotations in sitting.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title(Level of Evidence: 2A)
Closed chain exercises are good exercises in many regards: it may reduce strain on injured ligaments, augment proprioceptive feedback, and optimise muscle action. In the studies by Sahin et al. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title(Level of Evidence: 1B) and Ferrell et al. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title(Level of Evidence: 4) they trained specific with the knee joint, whilst the other two studies incorporated whole body exercise interventions to treat joint hypermobility syndrome.
Strengthening exercises: stabilizing muscles around hypermobile joints can be effective for joint support during movement or can reduce pain. These included shuttle-runs, bunny-hops, squat-thrusts, sitting-to-standing, step-ups and star-jumps. (30seconds or a predetermined number of repetitions) Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title(Level of Evidence: 2A)
Proprioception exercises: a decreased joint position sense (is there proof of will make patient more vulnerable for damage. Decreased sensory feedback may lead to biomechanically unsound limb positions being adopted, leading to abnormal postures. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title(Level of Evidence: 2C)
Coordination and balance exercises may improve proprioception. Exercise on board balance wood (2 to 3 minutes), mini-trampoline jumping (30 reps), walking with eyes closed, single leg balance, single leg ball rolling, forward/backward bends on one leg (eyes open or closed)
Control neutral joint position: identifying abnormal resting position of symptomatic joints, re-training postural muscles to facilitate optimal joint alignment (avoid hyperextension of knee when standing)
Re-train dynamic control: once a ‘neutral’ resting position is achieved, re-training of specific muscles to maintain joint position while moving adjacent joints (hip flexion while maintaining spinal neutral) Dynamic control will be exercised with daily activities or sports.
Motion control: improving the ability of specific muscles to control the joint through its entire range, both concentrically and eccentrically, static and posture ( on sitting to- standing quadriceps or working concentrically on standing up and eccentrically on sitting down) Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title(Level of Evidence: 1B)
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources [edit | edit source]
Clinical Bottom Line[edit | edit source]
Because hypermobility syndrome can excist with other symptoms and complaints, it is important that physiotherapists can diagnose hypermobility syndrome.
According to several articles physical therapy for HS patients includes: education of hypermobility syndrome, activity modification, stretching and strengthening excercisesexercises for affected joints and osteopathic manipulative treatment.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]