International Classification of Functioning, Disability and Health (ICF): Difference between revisions
(adjusting content) |
(editing content) |
||
| Line 271: | Line 271: | ||
== Case Example of the ICF in Use == | == Case Example of the ICF in Use == | ||
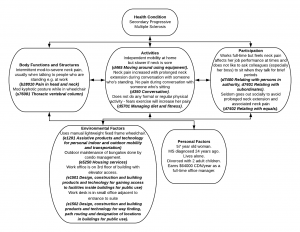
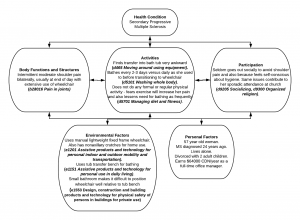
Mrs T is a 57 year old woman who was diagnosed with relapsing remitting multiple sclerosis 24 years ago. Seven years ago, her diagnosis was adjusted to Secondary Progressive MS as the condition progressed | Mrs T is a 57 year old woman who was diagnosed with relapsing remitting multiple sclerosis 24 years ago. Seven years ago, her diagnosis was adjusted to Secondary Progressive MS as the condition progressed according to its natural history. In response to progressive lower extremity weakness and disequilibrium, she was provided with a manual fixed frame wheelchair four years ago. Using the ICF, Mrs T’s situation could be summarized by the following schematic. | ||
Using the ICF, Mrs T’s | |||
<div class="clearfix">[[Image:ICF Model with WC Example(overview).png|center|thumb|300px|ICF Case Example - Overview]] </div> | <div class="clearfix">[[Image:ICF Model with WC Example(overview).png|center|thumb|300px|ICF Case Example - Overview]] </div> | ||
Revision as of 19:54, 1 July 2018
Introduction[edit | edit source]
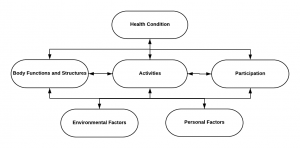
The International Classification of Functioning, Disability and Health (ICF) is a framework for describing functioning and disability in relation to a health condition. It provides a common language and framework for describing the level of function of a person within their unique environment, as opposed to classifying the person by their having a specific condition or as a 'Yes/No' answer regarding disability.[1][2] The World Confederation of Physical Therapy (WCPT) adopted a motion supporting the implementation of the ICF in physical therapy in 2003.[3]
The ICF is a framework to approach patient care that shifts the conceptual emphasis away from negative connotations such as disability and places focus on the positive abilities of the individual at the patient level rather than the systems level.
Components of the ICF[edit | edit source]
The ICF focuses on three components: body, activities/participation (at individual and societal levels) and contextual (personal and environmental).[1] These three components underscore the importance of the interplay and influence of both internal and external factors to each individual’s health status.
Body Functions and Structures[edit | edit source]
Definitions:[2]
- Body functions: The physiological functions of body systems (including psychological functions)
- Body structures: Anatomical parts of the body such as organs, limbs and their components
- Impairments: Problems in body function and structure such as significant deviation or loss
Examples:
- b28010 Pain in head and neck
- s720 Structure of shoulder region
- s810 Structures of areas of skin
Note that codes relating to body functions start with 'b' while codes relating to body structures start with 's.'
Activities and Participation[edit | edit source]
Definitions:[2]
- Activity: The execution of a task or action by an individual
- Activity limitations: Difficulties an individual may have in executing activities
- Participation: Involvement in a life situation
- Participation restrictions: Problems an individual may experience in involvement in life situations
Examples:
- d230 Carrying out daily routine
- d420 Transferring oneself
- d475 Driving
- d530 Toileting
- d910 Community life
- d920 Recreation and leisure
Note that codes relating to both activities and participation start with 'd.'
Environmental Factors[edit | edit source]
Definition:[2] The physical, social and attitudinal environment in which people live and conduct their lives. These are either barriers to or facilitators of the person's functioning.
Examples:
- e115 Products and technology for personal use in daily living
- e155 Design, construction and building products and technology of buildings for private use
- e210 Physical geography
- e355 Health professionals
Note that codes relating to environmental factors start with 'e.'
Personal Factors[edit | edit source]
Personal Factors should also be considered in this model but are not classified within the actual ICF framework.[1]
Contents of ICF Components[edit | edit source]
Each component is divided into a hierarchy with an additional digit added to the classification code for each subsequent layer in the hierarchy. The hierarchy is as follows;[1]
- Component e.g. Activities and participation
- Chapter e.g. Mobility (Chapter 4)
- Block e.g. Walking and Moving (d450-d469)
- Two level category e.g. Moving around in different locations (d460)
- Three level category e.g. Moving around within the home (d4600)
Measurement[edit | edit source]
A generic qualifier scale can be used to record the extent of the problem for each identified impairment, activity limitation and participation restriction. Environmental factors can also be qualified as either barriers or facilitators.[4]
| Qualifier for Impairments of Body Functions & Structures | Qualifier for Impairments of Activities & Participation | |
|---|---|---|
| 0 | No impairment | No difficulty |
| 1 | Mild impairment (present <25% of time, with tolerable intensity, occurring rarely over last 30 days) | Mild difficulty (present <25% of time, with tolerable intensity, occurring rarely over last 30 days) |
| 2 | Moderate impairment (present <50% of time, with intensity that interferes with day to day lift, occurring occasionally over last 30 days) | Moderate difficulty (present <50% of time, with intensity that interferes with day to day lift, occurring occasionally over last 30 days) |
| 3 | Severe impairment (present >50% of time, with intensity that's partially disrupting day to day lift, occurring frequently over last 30 days) | Severe difficulty (present >50% of time, with intensity that's partially disrupting day to day lift, occurring frequently over last 30 days) |
| 4 | Complete impairment (present >95% of time, with intensity that's totally disrupting day to day life, occurring daily over last 30 days) | Complete difficulty (present >95% of time, with intensity that's totally disrupting day to day life, occurring daily over last 30 days) |
| 8 | Not specified (insufficient information) | Not specified |
| 9 | Not applicable | Not applicable |
| Qualifier for Environmental Barriers | Qualifier for Environmental Facilitators | ||
|---|---|---|---|
| (.0) | No barrier | (+0) | No facilitator |
| (.1) | Mild barrier | (+1) | Mild facilitator |
| (.2) | Moderate barrier | (+2) | Moderate facilitator |
| (.3) | Severe barrier | (+3) | Substantial facilitator |
| (.4) | Complete barrier | (+4) | Complete facilitator |
| (.8) | Barrier, not specified | (+8) | Facilitator, not specified |
| (.9) | Not applicable | (+9) | Not applicable |
Performance versus Capacity[edit | edit source]
Definitions;
- Capacity: what a person can do in a standardised environment e.g. during clinical assessment.[2] It indicates the extent of activity limitation as a direct manifestation of a person's health status, without any assistance (whether assistance of another person, equipment or environmental modification).[4]
- Performance: what a person actually does in his/her usual environment e.g. at home.[2] It indicates the extent of participation restriction or the "lived experience" by describing all physical, social and attitudinal environmental factors.[4] It measures the difficulty a person experiences in doing things, assuming that they want to do them.[4]
The gap between these two constructs reflects the impact that different environments can have on activities and participation.[2] This gap can then guide intervention (e.g. on environmental factors) to help improve a patient's performance.[2]
Core Sets[edit | edit source]
The ICF Core Sets were developed as a practical tool to facilitate the systematic and comprehensive description of functioning in clinical practice.[5][6] They are compiled in order to provide health care professionals with a better understanding of the needs of their patient populations.[7] Core sets for twelve chronic diseases were initially developed because of their prevalence and the significant impact on function they can cause.[8] These twelve diseases are;[8]
- Breast Cancer
- Chronic Ischaemic Heart Disease
- Chronic Widespread Pain
- Depression
- Diabetes Mellitus
- Low Back Pain
- Obesity
- Obstructive Pulmonary Diseases
- Osteoarthritis
- Osteoporosis
- Rheumatoid Arthritis
- Stroke
Additional Core Sets have subsequently been developed for various other conditions and populations including;
- Ankylosing Spondylitis
- Multiple Sclerosis
- Cerebral Palsy
- Spinal Cord Injury
- Traumatic Brain Injury
- Neurological conditions in acute and post-acute care
- Musculoskeletal conditions in acute and post-acute care
- Geriatric patients in post-acute care
- Head and neck cancer
- Acute arthritis
All available core sets can be viewed here.
The ICF in Relation to Wheelchair Users[edit | edit source]
The following table suggests some factors that should be considered when evaluating a patient and his/her wheelchair using the ICF.[9][10]
| Body Structures and Functions | Activities | Participation | Environmental Factors | Personal Factors |
|---|---|---|---|---|
| Global & mental function | Mobility in the home | Quality of Life | Assistive equipment | Age |
| Sensory function & pain | Mobility in the community | Community participation | Seating system | Understanding & performance of WC skills |
| Voice & speech function | ADLs | Social engagement | Environmental control | BMI |
| Seating position | Physical activity & exercise | Self-care | Wheelchair design & seating configuration | Duration of impairment |
| Wheelchair & seating assessment | Self-esteem | Home, community & work barriers | Marital & socio-economic status | |
| Neuromusculoskeletal and movement-related functions | Work / employment | Transportation | Gender | |
| Severity of condition | Ethnicity | |||
| Cognition | ||||
| Fitness level | ||||
| Upper extremities & trunk |
Uses of the ICF in Research and Clinical Practice with Users of Wheelchairs[edit | edit source]
The ICF has been used in various ways in relation to research and clinical practice involving users of wheelchairs.
For example, Morgan et al (2017) recommended the ICF as a useful tool for identifying key wheelchair skills that needed to be taught during initial rehabilitation versus those that can be addressed once a patient has returned to community life.[7] Using the ICF, the authors identified three areas in which there was a disconnect between what was actually being taught during initial wheelchair rehabilitation and what should ideally be taught;[7]
- Use of the environment for training
- Addressing and accommodating for a psychological adjustment period
- Teaching how to care for and maintain the wheelchair
Similarly, Requejo et al (2015) noted that limitations and restrictions imposed by possible pain and dysfunction in wheelchair users can be defined using the ICF. The authors stated that the ICF can be used both to identify key elements that must be addressed during rehabilitation and also for guiding the provision and classification of assistive technology.[9] Thus, using the ICF can reduce the risk of a mismatch between the needs and capacities of the patient versus the type of wheelchair he is provided, which can in turn decrease the risk of pain, fatigue, pressure ulcers and increase quality of life, confidence and community participation.[9]
Mortenson et al (2008) used the ICF to evaluate wheelchair-specific outcome measures in relation to wheelchair activity and participation. They found two issues when using the ICF for this purpose. First, the majority of items in the outcome measures were coded as d465 (Moving around with equipment) on the ICF, thus the authors suggested that without a subsequent level to break this category down further, this code provides insufficient detail.[11] For example, there is no way to specify the type of equipment being used, the surface in question or whether the patient has to negotiate kerbs, inclines or thresholds. Second, the ICF does not include any subjective elements related to activity and participation.[11]
McDonald et al (2016) suggested that the ICF in itself would be a useful outcome measure in relation to wheelchair seating, positioning and mobility. [12] The authors note that wheelchairs have two main purposes; 1) compensating for or improving body functions and structure and 2) enhancing performance in seating, function and wheeled mobility. Thus, determining the overall success of wheelchair prescription can be a complicated task when reconciling these two purposes. In addition, these two purposes do not include social or environmental factors.[12] By using the ICF as an outcome measure for wheelchair prescription, all contextual factors would be considered and, importantly, given equal weight when determining the suitability of a given wheelchair for a given patient.[12]
Case Example of the ICF in Use[edit | edit source]
Mrs T is a 57 year old woman who was diagnosed with relapsing remitting multiple sclerosis 24 years ago. Seven years ago, her diagnosis was adjusted to Secondary Progressive MS as the condition progressed according to its natural history. In response to progressive lower extremity weakness and disequilibrium, she was provided with a manual fixed frame wheelchair four years ago. Using the ICF, Mrs T’s situation could be summarized by the following schematic.
Alternatively, a health care professional could use the ICF to focus on certain related aspects of Mrs T’s situation in order to plan an intervention. For example;
Resources[edit | edit source]
- An introduction to the International Classification of Functioning, Disability and Health (ICF) from the WCPT
- Using the ICF in Clinical Practice from the WCPT
- World Health Organization ICF Resources, a summary from the WCPT
- ICF Core Sets
- ICF Checklist Version 2.1a Clinician Form
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Sykes C. Health classifications 1 - An introduction to the ICF. WCPT Keynotes. World Confederation for Physical Therapy. 2006.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 The ICF: An Overview. Available at: https://www.wcpt.org/sites/wcpt.org/files/files/GH-ICF_overview_FINAL_for_WHO.pdf
- ↑ Escorpizo R, Stucki G, Cieza A, Davis K, Stumbo T, Riddle DL. Creating an interface between the International Classification of Functioning, Disability and Health and physical therapist practice. Phys Ther. 2010;90:1053-63.
- ↑ 4.0 4.1 4.2 4.3 World Health Organization. ICF Checklist Version 2.1a, Clinician Form. 2003. Available at: http://www.who.int/classifications/icf/training/icfchecklist.pdf
- ↑ Kesselring J, Coenen M, Cieza A, Thompson A, Kostanjsek N, Stucki G. Developing the ICF Core Sets for multiple sclerosis to specify functioning. Mult Scler. 2008;14:252-4.
- ↑ Rauch A, Cieza A, Stucki G. How to apply the International Classification of Functioning, Disability and Health (ICF) for rehabilitation management in clinical practice. Eur J Phys Rehabil. 2008;44(3):329-42.
- ↑ 7.0 7.1 7.2 Morgan KA, Engsberg JR, Gray DB. Important wheelchair skills for new manual wheelchair users: health care professional and wheelchair user perspectives. Disabil Rehabil Assist Technol. 2017 Jan;12(1):28-38.
- ↑ 8.0 8.1 Sykes C. Health classifications 2 - Using the ICF in clinical practice. WCPT Keynotes. World Confederation for Physical Therapy. 2007.
- ↑ 9.0 9.1 9.2 Requejo PS, Furumasu J, Mulroy SJ. Evidence-Based Strategies for Preserving Mobility for Elderly and Aging Manual Wheelchair Users. Top Geriatr Rehabil. 2015 Jan-Mar;31(1):26-41.
- ↑ Mausen S. Why wheelchair and seating assessment by ICF? Is it necessary or a waste of time? Lecture presented at 2015 International Seating Symposium; University of Pittsburgh.
- ↑ 11.0 11.1 Mortenson WB, Miller WC, Auger C. Issues for the selection of wheelchair-specific activity and participation outcome measures: a review. Arch Phys Med Rehabil. 2008 Jun;89(6):1177-86.
- ↑ 12.0 12.1 12.2 McDonald R, Rushton P, Giesbrecht E, Kirby RL, Viswanathan P, Casey J.Outcome measurement in wheelchair seating, positioning and mobility. European Seating Symposium, Dublin, Ireland. European Seating Symposium. 2016. 4 pp. [Conference contribution]