Labral Tear: Difference between revisions
No edit summary |
Ahmed M Diab (talk | contribs) No edit summary |
||
| (34 intermediate revisions by 13 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors ''' - [[User:Bilitis Crokaert|Bilitis Crokaert]] | '''Original Editors ''' - [[User:Bilitis Crokaert|Bilitis Crokaert]] as part of the Vrije Universiteit Brussel Project. | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Definition/Description == | ||
An acetabular labral tear can cause pain if the labrum is torn, frayed, or damaged. Labral tears cause groin pain or pain in the anterior side of the hip, and less commonly buttock pain.<ref name="Groh">Groh MM, Herrera J. A comprehensive review of labral tears. Curr Rev Musculoskelet Med 2009 Jun;2(2):105-17.</ref> This mechanically induced pathology is thought to result from excessive forces at the [[Hip Anatomy|hip joint]]. For example, a tear could decrease the acetabular contact area and increase stress, which would result in articular damage, and destabilize the hip joint.<ref name="Lewis">Lewis CL, Sahrmann SA. Acetabular Labral Tears. Phys Ther 2006;86:110-121.</ref> | |||
Labral tears could be further classified as: | |||
== | *'''Anterior labral tears''' - the pain will generally be more consistent and is situated on the anterior hip (anterosuperior quadrant) or at the groin.<ref name="McCarthy">McCarthy JC, Noble PC, Schuck MR, et al. The Otto E. Aufranc Award: the role of labral lesions to development of early degenerative hip disease. Clin Orthop 2001;393:25–37.</ref><ref>O’Leary JA, Berend K, Vail TP. The relationship between diagnosis and outcome in arthroscopy of the hip. Arthroscopy 2001;17:181–188.</ref><ref name="Byrd">Byrd JW. Labral lesions: an elusive source of hip pain case reports and literature review. Arthroscopy 1996;12:603–612.</ref><ref name="Binningsley">Binningsley D. Tear of the acetabular labrum in an elite athlete. Br J Sports Med 2003;37:84–88.</ref><ref name="Hase">Hase T, Ueo T. Acetabularlabral tear: arthroscopic diagnosis and treatment. Arthroscopy 1999;15:138 –141.</ref><ref name="Klaue">Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg Br 1991;73:423– 429.</ref> They frequently occur in individuals in European countries and the United States. | ||
*'''Posterior labral tears''' - are situated in the lateral region or deep in the posterior buttocks. They occur less frequently in individuals in European countries and the United States, but are more common in individuals from Japan.<ref name="McCarthy" /><ref name="Byrd" /><ref name="Hase" /> | |||
== Clinically Relevant Anatomy == | |||
The acetabular labrum is a fibro-cartilaginous rim, which encompasses the circumference of the acetabulum. It helps to keep the head of the [[femur]] inside the acetabulum, and varies greatly in form and thickness.<br> | |||
The labrum has three surfaces:1 | |||
#'''Internal articular surface''' - adjacent to the joint (avascular) | |||
#'''External articular surface''' - contacting the joint capsule (vascular) | |||
#'''Basal surface''' - attached to the acetabular bone and ligaments.<br> | |||
The transverse ligaments surround the hip and help hold it in place while moving.<br> | |||
On the anterior aspect, the labrum is triangular in the radial section. On the posterior aspect, the labrum is dimensionally square but with a rounded distal surface.<ref name="Narvani">Narvani AA, Tsiridis E, Tai CC, Thomas P. Acetabular labrum and its tears. Br J Sports Med 2003;37:207-211.</ref><ref name="Lovell">Lovell G. The diagnosis of chronic groin pain in athletes; a review of 189 cases. Aust J Sci Med Sport 1995;27:76-9</ref><br> | |||
The functions of the acetabular labrum are: | |||
== | *Joint stability | ||
*Sensitive shock absorber | |||
*Joint lubricator | |||
*Pressure distributor | |||
*Decreasing contact stress between the acetabular and the femoral cartilage<ref name="Byrd" /><ref name="Martin">Martin RL, Enseki KR, Draovitch P, et al. Acetabular labral tears of the hip: examination and diagnostic challenges. J Orthop Sports Phys Ther 2006;36:503-15.</ref><ref name="Groh" /><br> | |||
[[Image:Hip.jpg]] | |||
== Epidemiology/Etiology == | |||
In studies of patients with a labral tear, researchers have attributed the injury to a variety of causes: | |||
*Direct trauma - e.g. motor accidents, falling with or without a hip dislocation, slipping | |||
*Sporting activities that require frequent external rotations or hyperextension - e.g. ballet, soccer, and hockey, running and sprinting | |||
*Specific movements including torsional or twisting movements, hyper abduction, hyper extension, and hyper extension with lateral rotation | |||
The condition is not age related. The reported age of people with hip pain and a labral tear spans from 8 to 75 years old. | |||
Structural risk factors for the condition include: | |||
*[[Hip Dysplasia|Acetabular dysplasia]] | |||
<ref | *Degeneration | ||
*Capsular laxity and hip hypermobility | |||
*[[Femoroacetabular Impingement|Femeroacetabular impingement]] (FAI) (Byrd and Jones 2003, Wenger et al. 2004)<ref name="Lewis" /> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
- | *Sex - Occurs in both sexes with the same frequency<ref name="Dorrell">Dorrell JH, Catterall A. A torn acetabular labrum. J Bone Joint Surg 1986;68:400-3.</ref><ref name="Klaue" /><ref name="Fitzgerald">Fitzgerald RH. Acetabular labrum tears. Diagnosis and treatment. Clin Orthop Relat Res 1995 Feb;(311):60-8.</ref><ref name="Leunig">Leunig M, Werlen S, Ungersbock A, et al. Evaluation of the acetabulum labrum by MR arthrograpy. J Bone Joint Surg Br 1997;79:230-4</ref> | ||
*Symptoms - A constant dull pain with periods of sharp pain that worsens during activity. Walking, pivoting, prolonged sitting and impact activities aggravate symptoms. Some patients describe night time pain<ref name="Groh" />. The symptoms can have a long duration, with an average of greater than two years.<ref name="Farjo">Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for acetabular labral tears. Arthroscopy 1999;15:132–137.</ref>The injury is usually caused by the hip joint being stressed in rotation. The pain is mainly in the groin, but could be in the trochanteric and buttock region. | |||
*Mechanical Symptoms - A variety of mechanical symptoms have been reported, including clicking (most frequently),locking or catching, or giving away. The significance of these signs is questionable.<ref name="Leibold">Leibold M, Huijbregts P, Jensen R. Concurrent criterion-related validity of physical examination tests for hip labral lesions: a systematic review. J Manual Manip Ther 2008;16:24-41</ref> | |||
*Range of motion: It usually isn't restricted however at extremes, invoke pain. | |||
**These specific manoeuvres may cause pain in the groin:<ref name="Narvani" /> | |||
***[[FADIR (Flexion, Adduction, Internal Rotation) Test|Flexion, adduction, and internal rotation (FADDIR TEST)]]<nowiki/>of the hip joint are related to anterior superior tears | |||
***Passive hyperextension, abduction, and external rotation are related to posterior tears<br> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
The differential diagnosis of labral tears | The differential diagnosis of labral tears may include the following diagnoses: | ||
< | *[[Pubalgia|Athletic pubalgia]] | ||
*[[Snapping Hip Syndrome|Snapping_Hip]] | |||
*[[Septic (Infectious) Arthritis]] | |||
*[[A Morton foot : cause of piriformis syndrome|Piriformis syndrome]] | |||
*Contusion | |||
*Strain | |||
*[[Osteitis Pubis|Osteitis pubis]] | |||
*[[Trochanteric Bursitis]] | |||
*[[Avascular necrosis of the femoral head]] | |||
*Fracture | |||
*Dislocation | |||
*[[Inguinal Hernia|Inguinal]] or femoral hernia | |||
*[[Legg-Calve-Perthes Disease|Legg-Calve Perthes disease]] | |||
*[[Slipped Capital Femoral Epiphysis]] | |||
*[[Referred Pain]] from the [[Lumbosacral Biomechanics|lumbosacral]] and [[Sacroiliac Joint|sacroiliac]] areas | |||
*Tumor<ref name="Schmerl">Schmerl M, Pollard H, Hoskins W. Labral injuiries of the hip: a review of diagnosis and management. J Manipulative Physiol Ther 2005 Oct;28(8):632.</ref> | |||
== | === Investigations === | ||
Plain radiographs and computed tomography may show hip dysplasia, arthritis, and acetabular cysts in patients with acetabular labrum tears, they are useful for excluding other types of hip pathology. MRI helps in diagnosing acetabular labral tears. | |||
Includes relative rest, anti-inflammatory medications, and pain medications if necessary. Combined with a 10-12 week intensive physiotherapy. The pain | *'''MRA (magnetic resonance arthography)''' - Produces the best result, as the intra-articular or systemic infusion of gadolinium is required to obtain the detail necessary to study the labrum. The principle of the procedure relies upon capsular distension. The outline the labrum with contrast and filling any tears that may be present. MRA has limitations regarding the sensivity for diagnose acetabular labral and articular cartilage abnormalities, it has also been proven that MRA may be less effective in identifying posterior and lateral tears.<ref name="McCarthy" /> | ||
*'''Diagnostic-image-guided intra-articular hip injections''' - Can also be helpful in the diagnosis of labral tears. | |||
*'''Hip arthroscopy''' - Used as a diagnostic gold standard for ALT and is used as therapeutic medium. | |||
<br> | |||
== Conservative Management == | |||
Includes relative rest, anti-inflammatory medications, and pain medications if necessary. Combined with a 10-12 week intensive physiotherapy program. The patient's pain may lessen during this period but it is possible that the pain will return once the patient returns to his normal activities. When conservative management is unable to control the patient’s symptoms, surgical intervention may be considered.<ref name="Troelsen">Troelsen A, Mechlenburg I, Gelineck J, Bolvig L, Jacobsen S, Søballe K. What is the role of clinical tests and ultrasound in acetabular labral tear diagnostics? Acta Orthop 2009 Jun;80(3):314-8.</ref><br> | |||
== Outcome Measures == | == Outcome Measures == | ||
*[[Lower Extremity Functional Scale (LEFS)]] | |||
*[[International Hip Outcome Tool (iHOT)]] | |||
See [[Outcome Measures|Outcome Measures Database]] for more | |||
== Examination == | == Examination == | ||
=== Physical Examination === | |||
The test is considered positive if one or more of these symptoms are reproduced during the test: click, clunk, or pain in the groin region.<ref name="Troelsen" /><ref name="Springer">Springer BA, Gill NW, Freedman BA, Ross AE, Javernick MA, Murphy KP. Acetabular labral tears: diagnostic accuracy of clinical examination by a physical therapist, orthopaedic surgeon and orthopaedic residents. N Am J Sports Phys Ther 2009;4(1):38-45.</ref> | |||
*'''Impingement test''' - The hip joint is passively flexed to 90°, internally rotated, and adducted (see video below). | |||
*'''[[FABER Test]]''' - The lower extremity is passively placed in a figure-of–four position, and slight pressure is applied to the medial side of the knee. (Positive in 7 of 18 cases) | |||
*'''[[Straight Leg Raise Test|Resisted straight leg raise test]]''' - The patient's hip is flexed 30° with the knee in extension and a downward pressure applied.(Positive in 1 of 18 cases) | |||
*'''[[McCarthy test|McCarthy sign]]/[[Thomas Test]]''' (hip flexion to extension manoeuvre) - With the patient in a supine position, the subject fully flexes both hips. The examiner slowly/passively extends the subject’s lower extremities and moves the hips into external rotation. The test is repeated, but with the hip in internal rotation. | |||
*'''Internal rotation load/grind test''' - With the patient in a supine position, the examiner passively flexes the patient's hip to 100°, and then rotates the subject’s hip from internal rotation to external rotation while pushing along the axis of the femur through the knee to elicit ‘grind’ (see video below). | |||
*'''Fitzgerald Test''' - For assessment of the anterior labrum. The patient's hip is acutely flexed and then extended while internally rotated and in full abduction. | |||
*'''Patrick test''' - For assessment of the posterior labrum. The patient's hip is flexed and then extended while in abduction and external rotation. | |||
{{#ev:youtube|Rtp4oz0_3YY}}<ref>British Journal of Sports. Hip & Groin Exam (7 of 7): Labral tear Available fromhttps://www.youtube.com/watch?v=Rtp4oz0_3YY. Accessed on 15/12/22.</ref> | |||
== Medical Management == | |||
=== Arthroscopy === | |||
Repair of the acetabular labral lesion can be preformed in either the supine or lateral position. In the supine position, a stand fracture table is used with an oversized perinal post to apply traction. The affected hip is placed into slight extension/adduction to allow approach to the joint. During traction it is important that there is a minimized pressure in the perineal area to avoid neurologic complications. The procedure is under the guidance of fluoroscopy. If the distraction is obtain a 14 or a 16 gauge spinal needle is inserted into the joint to break the vacuum seal and allow further distraction. Three portals are used (the anterolateral, anterior and the distal lateral accessory). <br>For repair of a detached labrum, the edges of the tear are delineated and suture anchors are placed on top of the acetabular rim in the area of detachment. If the tear in the labrum has a secure outer rim and is still attached to the acetabulum, a suture in the mid substance of the tear can be used to secure.<ref name="Garrison">Garrison C, Osler MT, Singleton SB. Rehabilitation after arthroscopy of an acetabular labral tear. N Am J Sports Phys Ther 2007;2(4):241-250</ref> | |||
{{#ev:youtube|sTWBZifEiyI}} | |||
== Physical Therapy Management <ref name="Garrison" /> == | |||
Movements that cause stress in the area need to be avoided. The rehabilitation protocol following acetabular labral debridement or repair are divided into four phases. | |||
== | === Phase 1 - Initial Exercise (Week 1-4) === | ||
The primary goals following a acetabularlabral debridement or repair are to the minimize pain and the inflammation, and initiate early motion exercises. This phase initially consists of isometric contraction exercises for the hip adductors, abductors, transverse abdominals and extensor muscles. Following a labral debridement, closed-chain activities such as low-level leg press or shuttle can begin with limited resistance. Assistive device for those with increased pain with weight bearing. Active movements within painful limits. [[Transversus Abdominis|Transversus abdominis]] and [[Lumbar Multifidus|multifidus]] isolated contraction and associated light exercises, such as bridging and crouching close to the floor on hands and knees<ref name=":0">Yazbek PM, Ovanessian V, Martin RL, Fukuda TY. Nonsurgical treatment of acetabular labrum tears: a case series. journal of orthopaedic & sports physical therapy. 2011 May;41(5):346-53.</ref> | |||
<br>Weight bearing protocol following a debridement is 50% for 7 to 10 days, and non-weight bearing or toe-touch weight bearing for 3 to 6 weeks in case of a labral repair. Unnecessary hypomobility will limit progress in future phases, thus it is important to ensure that the patient maintains adequate mobility and range during this phase. | |||
<br>''Treatment modalities: '' | <br>'''Treatment modalities:''' | ||
*[[Aquatherapy|Aquatic therapy]] is a suitable treatment approach - movement in the water allows for improvement in [[Gait Cycle|gait]] by allowing appropriate loads to be placed on the joint without causing unnecessary stress to the healing tissue. For example, the patient may perform light jogging in the water using a flotation device. It is import to know that the patient's range of motion precautions, as these may vary in debridement or repair. | |||
*Manual therapy for pain reduction and improvement in joint mobility and proprioception. Considerations include gentle hip joint mobilizations contract-relax stretching for internal and external rotation, long axis distraction, and assessment of lumbo-sacral mobility. | |||
*[[Cryotherapy|Cryotherapy]] | |||
*Appropriate pain management through medication. | |||
*Gentle [[stretching]] of hip muscle groups including [[Psoas Major|psoas]], [[Quadriceps Muscle|quadriceps]], hamstring muscles with passive range of motion. | |||
*Stationary bike without resistance, with seat height that limits the hip to less than 90° | |||
*Exercises such as: water walking, [[piriformis]] stretch, ankle pumps. | |||
To progress to phase 2, ROM has to be greater or equal to 75%. | |||
- | === Phase 2 - Intermediate Exercise (Week 5-7) === | ||
The goal of this phase is to continue to improve ROM and soft tissue flexibility . Manual therapy should continue with mobilization that is more aggressive, passive ROM exercises should become more aggressive as needed, for external- and internal rotation. Discontinuation of assistive device is done. | |||
*Flexibility exercises involving the [[piriformis]], adductor group, psoas/[[Quadriceps Muscle|rectus femoris]] should continue | |||
*Stationary bike with resistance | |||
*Maitland’s manual mobilization (grades 3 and 4) and combined movements | |||
*Pelvic rotation maneuver | |||
*Sacroiliac distraction | |||
*Sidestepping with an abductor band for resistance | |||
*Core strengthening (lumbopelvic stabilization exercises added to moderate exercises, such as lateral bridge and mini squat, and to light sensory motor training) | |||
*Non-competitive swimming | |||
*Exercises such as wall sits with abductor band, two leg bridging | |||
*Standing hip flexion and extension (progressive load), 3 × 10 reps • Standing hip abduction and adduction, with elastic resistance near a support bar (progressive load), 3 × 10 reps • Lunge (progressive load), 3 × 10 reps • Shuttle machine (progressive load), 3 × 10 reps, 70% MR • Knee flexion-extension on chair (progressive load), 3 × 10 reps, 70% MR • Sidestepping gait with an elastic band over midfeet, 3 × 1 min • Dynamic valgus control with single-limb squat, 3 × 1 min <ref name=":0" /> | |||
*To improve balance• Balancing • Balance board • DynaDisc • Jumping board<ref name=":0" /> | |||
To | To progress to the third phase it is important that the patient has a [[Gait Cycle|normal gait pattern]] with no [[Trendelenburg Sign|Trendelenburg sign]]. The patient should have symmetrical and passive ROM measurement with minimal complaints of pain. | ||
=== Phase 3 - Advanced Exercise (Week 8-12) === | |||
exercises such as | *Manual therapy should be performed as needed | ||
*Flexibility and passive ROM interventions should become slightly more aggressive if the limitations persist (if the patient has reached his full ROM or flexibility, terminal stretches should be initiated) | |||
*Strengthening exercises: walking lunges, lunges with trunk rotations, resistend sportcord, walking forward/backwards, plyometric bounding in the water. Muscle strength maintenance (progressive load) and address any persisting muscular imbalance. | |||
*Core (lumbopelvic stabilization exercises) added to Swiss ball exercises and advanced sensory motor training | |||
*Exercises such as core ball stabilization, golf progression, lunges | |||
== | To progress to the fourth phases it is important that there is symmetrical ROM and flexibility of the psoas and piriformis. | ||
=== Phase 4 - Sport Specific Training (Week 12-*) === | |||
In this phase it is important to return safely and effectively back to competition or previous activity level. Manual therapy, flexibility, and ROM exercises can continue as appropriate.<br> | |||
It is important the the patient has good muscular endurance, good eccentric muscle control, and the ability to generate power.<br> | |||
The patient can be given sport specific exercises and has to have the ability to demonstrate a good neuromuscular control of the lower extremity during the activities. | |||
Exercises such as: sport specific drills, functional testing<br><br> | |||
== Key Research == | |||
* Greaves LL, et al. Effect of acetabular labral tears, repair and resection on hip cartilage strain: a 7T MR study. J Biomech. 2010 Mar 22;43(5):858-63. doi: 10.1016/j.jbiomech.2009.11.016. http://www.jbiomech.com/article/S0021-9290(09)00652-6/abstract (accessed 27 January 2014)<br> | |||
* Springer BA, et al. Acetabular labral tears: diagnostic accuracy of clinical examination by a physical therapist, orthopaedic surgeon, and orthopaedic residents. N Am J Sports Phys Ther. 2009 Feb;4(1):38-45. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2953315/pdf/najspt-04-038.pdf (accessed 27 January 2014).<br> | |||
* Nishii T, et al. Acetabular labral tears: contrast-enhanced MR imaging under continuous leg traction. Skeletal Radiol. 1996 May;25(4):349-56. | |||
== | == Presentations == | ||
{{#ev:youtube|EtoOycWxQBo}} | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Vrije_Universiteit_Brussel_Project | [[Category:Injury]] | ||
[[Category:Hip]] | |||
[[Category:Joints]] | |||
[[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | |||
[[Category:Vrije_Universiteit_Brussel_Project]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Sports Injuries]] | |||
[[Category:Conditions]] | |||
[[Category:Hip - Conditions]] | |||
Latest revision as of 11:46, 3 May 2024
Original Editors - Bilitis Crokaert as part of the Vrije Universiteit Brussel Project.
Top Contributors - Bilitis Crokaert, Admin, Kim Jackson, Daphne Jackson, Anas Mohamed, Evan Thomas, Shreya Pavaskar, Ahmed M Diab, Trista Chan, 127.0.0.1, WikiSysop, Simisola Ajeyalemi, Vidya Acharya and Wanda van Niekerk
Definition/Description[edit | edit source]
An acetabular labral tear can cause pain if the labrum is torn, frayed, or damaged. Labral tears cause groin pain or pain in the anterior side of the hip, and less commonly buttock pain.[1] This mechanically induced pathology is thought to result from excessive forces at the hip joint. For example, a tear could decrease the acetabular contact area and increase stress, which would result in articular damage, and destabilize the hip joint.[2]
Labral tears could be further classified as:
- Anterior labral tears - the pain will generally be more consistent and is situated on the anterior hip (anterosuperior quadrant) or at the groin.[3][4][5][6][7][8] They frequently occur in individuals in European countries and the United States.
- Posterior labral tears - are situated in the lateral region or deep in the posterior buttocks. They occur less frequently in individuals in European countries and the United States, but are more common in individuals from Japan.[3][5][7]
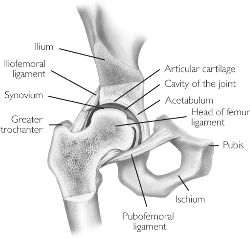
Clinically Relevant Anatomy[edit | edit source]
The acetabular labrum is a fibro-cartilaginous rim, which encompasses the circumference of the acetabulum. It helps to keep the head of the femur inside the acetabulum, and varies greatly in form and thickness.
The labrum has three surfaces:1
- Internal articular surface - adjacent to the joint (avascular)
- External articular surface - contacting the joint capsule (vascular)
- Basal surface - attached to the acetabular bone and ligaments.
The transverse ligaments surround the hip and help hold it in place while moving.
On the anterior aspect, the labrum is triangular in the radial section. On the posterior aspect, the labrum is dimensionally square but with a rounded distal surface.[9][10]
The functions of the acetabular labrum are:
- Joint stability
- Sensitive shock absorber
- Joint lubricator
- Pressure distributor
- Decreasing contact stress between the acetabular and the femoral cartilage[5][11][1]
Epidemiology/Etiology[edit | edit source]
In studies of patients with a labral tear, researchers have attributed the injury to a variety of causes:
- Direct trauma - e.g. motor accidents, falling with or without a hip dislocation, slipping
- Sporting activities that require frequent external rotations or hyperextension - e.g. ballet, soccer, and hockey, running and sprinting
- Specific movements including torsional or twisting movements, hyper abduction, hyper extension, and hyper extension with lateral rotation
The condition is not age related. The reported age of people with hip pain and a labral tear spans from 8 to 75 years old.
Structural risk factors for the condition include:
- Acetabular dysplasia
- Degeneration
- Capsular laxity and hip hypermobility
- Femeroacetabular impingement (FAI) (Byrd and Jones 2003, Wenger et al. 2004)[2]
Characteristics/Clinical Presentation[edit | edit source]
- Sex - Occurs in both sexes with the same frequency[12][8][13][14]
- Symptoms - A constant dull pain with periods of sharp pain that worsens during activity. Walking, pivoting, prolonged sitting and impact activities aggravate symptoms. Some patients describe night time pain[1]. The symptoms can have a long duration, with an average of greater than two years.[15]The injury is usually caused by the hip joint being stressed in rotation. The pain is mainly in the groin, but could be in the trochanteric and buttock region.
- Mechanical Symptoms - A variety of mechanical symptoms have been reported, including clicking (most frequently),locking or catching, or giving away. The significance of these signs is questionable.[16]
- Range of motion: It usually isn't restricted however at extremes, invoke pain.
- These specific manoeuvres may cause pain in the groin:[9]
- Flexion, adduction, and internal rotation (FADDIR TEST)of the hip joint are related to anterior superior tears
- Passive hyperextension, abduction, and external rotation are related to posterior tears
- These specific manoeuvres may cause pain in the groin:[9]
Differential Diagnosis[edit | edit source]
The differential diagnosis of labral tears may include the following diagnoses:
- Athletic pubalgia
- Snapping_Hip
- Septic (Infectious) Arthritis
- Piriformis syndrome
- Contusion
- Strain
- Osteitis pubis
- Trochanteric Bursitis
- Avascular necrosis of the femoral head
- Fracture
- Dislocation
- Inguinal or femoral hernia
- Legg-Calve Perthes disease
- Slipped Capital Femoral Epiphysis
- Referred Pain from the lumbosacral and sacroiliac areas
- Tumor[17]
Investigations[edit | edit source]
Plain radiographs and computed tomography may show hip dysplasia, arthritis, and acetabular cysts in patients with acetabular labrum tears, they are useful for excluding other types of hip pathology. MRI helps in diagnosing acetabular labral tears.
- MRA (magnetic resonance arthography) - Produces the best result, as the intra-articular or systemic infusion of gadolinium is required to obtain the detail necessary to study the labrum. The principle of the procedure relies upon capsular distension. The outline the labrum with contrast and filling any tears that may be present. MRA has limitations regarding the sensivity for diagnose acetabular labral and articular cartilage abnormalities, it has also been proven that MRA may be less effective in identifying posterior and lateral tears.[3]
- Diagnostic-image-guided intra-articular hip injections - Can also be helpful in the diagnosis of labral tears.
- Hip arthroscopy - Used as a diagnostic gold standard for ALT and is used as therapeutic medium.
Conservative Management[edit | edit source]
Includes relative rest, anti-inflammatory medications, and pain medications if necessary. Combined with a 10-12 week intensive physiotherapy program. The patient's pain may lessen during this period but it is possible that the pain will return once the patient returns to his normal activities. When conservative management is unable to control the patient’s symptoms, surgical intervention may be considered.[18]
Outcome Measures[edit | edit source]
See Outcome Measures Database for more
Examination[edit | edit source]
Physical Examination[edit | edit source]
The test is considered positive if one or more of these symptoms are reproduced during the test: click, clunk, or pain in the groin region.[18][19]
- Impingement test - The hip joint is passively flexed to 90°, internally rotated, and adducted (see video below).
- FABER Test - The lower extremity is passively placed in a figure-of–four position, and slight pressure is applied to the medial side of the knee. (Positive in 7 of 18 cases)
- Resisted straight leg raise test - The patient's hip is flexed 30° with the knee in extension and a downward pressure applied.(Positive in 1 of 18 cases)
- McCarthy sign/Thomas Test (hip flexion to extension manoeuvre) - With the patient in a supine position, the subject fully flexes both hips. The examiner slowly/passively extends the subject’s lower extremities and moves the hips into external rotation. The test is repeated, but with the hip in internal rotation.
- Internal rotation load/grind test - With the patient in a supine position, the examiner passively flexes the patient's hip to 100°, and then rotates the subject’s hip from internal rotation to external rotation while pushing along the axis of the femur through the knee to elicit ‘grind’ (see video below).
- Fitzgerald Test - For assessment of the anterior labrum. The patient's hip is acutely flexed and then extended while internally rotated and in full abduction.
- Patrick test - For assessment of the posterior labrum. The patient's hip is flexed and then extended while in abduction and external rotation.
Medical Management[edit | edit source]
Arthroscopy[edit | edit source]
Repair of the acetabular labral lesion can be preformed in either the supine or lateral position. In the supine position, a stand fracture table is used with an oversized perinal post to apply traction. The affected hip is placed into slight extension/adduction to allow approach to the joint. During traction it is important that there is a minimized pressure in the perineal area to avoid neurologic complications. The procedure is under the guidance of fluoroscopy. If the distraction is obtain a 14 or a 16 gauge spinal needle is inserted into the joint to break the vacuum seal and allow further distraction. Three portals are used (the anterolateral, anterior and the distal lateral accessory).
For repair of a detached labrum, the edges of the tear are delineated and suture anchors are placed on top of the acetabular rim in the area of detachment. If the tear in the labrum has a secure outer rim and is still attached to the acetabulum, a suture in the mid substance of the tear can be used to secure.[21]
Physical Therapy Management [21][edit | edit source]
Movements that cause stress in the area need to be avoided. The rehabilitation protocol following acetabular labral debridement or repair are divided into four phases.
Phase 1 - Initial Exercise (Week 1-4)[edit | edit source]
The primary goals following a acetabularlabral debridement or repair are to the minimize pain and the inflammation, and initiate early motion exercises. This phase initially consists of isometric contraction exercises for the hip adductors, abductors, transverse abdominals and extensor muscles. Following a labral debridement, closed-chain activities such as low-level leg press or shuttle can begin with limited resistance. Assistive device for those with increased pain with weight bearing. Active movements within painful limits. Transversus abdominis and multifidus isolated contraction and associated light exercises, such as bridging and crouching close to the floor on hands and knees[22]
Weight bearing protocol following a debridement is 50% for 7 to 10 days, and non-weight bearing or toe-touch weight bearing for 3 to 6 weeks in case of a labral repair. Unnecessary hypomobility will limit progress in future phases, thus it is important to ensure that the patient maintains adequate mobility and range during this phase.
Treatment modalities:
- Aquatic therapy is a suitable treatment approach - movement in the water allows for improvement in gait by allowing appropriate loads to be placed on the joint without causing unnecessary stress to the healing tissue. For example, the patient may perform light jogging in the water using a flotation device. It is import to know that the patient's range of motion precautions, as these may vary in debridement or repair.
- Manual therapy for pain reduction and improvement in joint mobility and proprioception. Considerations include gentle hip joint mobilizations contract-relax stretching for internal and external rotation, long axis distraction, and assessment of lumbo-sacral mobility.
- Cryotherapy
- Appropriate pain management through medication.
- Gentle stretching of hip muscle groups including psoas, quadriceps, hamstring muscles with passive range of motion.
- Stationary bike without resistance, with seat height that limits the hip to less than 90°
- Exercises such as: water walking, piriformis stretch, ankle pumps.
To progress to phase 2, ROM has to be greater or equal to 75%.
Phase 2 - Intermediate Exercise (Week 5-7)[edit | edit source]
The goal of this phase is to continue to improve ROM and soft tissue flexibility . Manual therapy should continue with mobilization that is more aggressive, passive ROM exercises should become more aggressive as needed, for external- and internal rotation. Discontinuation of assistive device is done.
- Flexibility exercises involving the piriformis, adductor group, psoas/rectus femoris should continue
- Stationary bike with resistance
- Maitland’s manual mobilization (grades 3 and 4) and combined movements
- Pelvic rotation maneuver
- Sacroiliac distraction
- Sidestepping with an abductor band for resistance
- Core strengthening (lumbopelvic stabilization exercises added to moderate exercises, such as lateral bridge and mini squat, and to light sensory motor training)
- Non-competitive swimming
- Exercises such as wall sits with abductor band, two leg bridging
- Standing hip flexion and extension (progressive load), 3 × 10 reps • Standing hip abduction and adduction, with elastic resistance near a support bar (progressive load), 3 × 10 reps • Lunge (progressive load), 3 × 10 reps • Shuttle machine (progressive load), 3 × 10 reps, 70% MR • Knee flexion-extension on chair (progressive load), 3 × 10 reps, 70% MR • Sidestepping gait with an elastic band over midfeet, 3 × 1 min • Dynamic valgus control with single-limb squat, 3 × 1 min [22]
- To improve balance• Balancing • Balance board • DynaDisc • Jumping board[22]
To progress to the third phase it is important that the patient has a normal gait pattern with no Trendelenburg sign. The patient should have symmetrical and passive ROM measurement with minimal complaints of pain.
Phase 3 - Advanced Exercise (Week 8-12)[edit | edit source]
- Manual therapy should be performed as needed
- Flexibility and passive ROM interventions should become slightly more aggressive if the limitations persist (if the patient has reached his full ROM or flexibility, terminal stretches should be initiated)
- Strengthening exercises: walking lunges, lunges with trunk rotations, resistend sportcord, walking forward/backwards, plyometric bounding in the water. Muscle strength maintenance (progressive load) and address any persisting muscular imbalance.
- Core (lumbopelvic stabilization exercises) added to Swiss ball exercises and advanced sensory motor training
- Exercises such as core ball stabilization, golf progression, lunges
To progress to the fourth phases it is important that there is symmetrical ROM and flexibility of the psoas and piriformis.
Phase 4 - Sport Specific Training (Week 12-*)[edit | edit source]
In this phase it is important to return safely and effectively back to competition or previous activity level. Manual therapy, flexibility, and ROM exercises can continue as appropriate.
It is important the the patient has good muscular endurance, good eccentric muscle control, and the ability to generate power.
The patient can be given sport specific exercises and has to have the ability to demonstrate a good neuromuscular control of the lower extremity during the activities.
Exercises such as: sport specific drills, functional testing
Key Research[edit | edit source]
- Greaves LL, et al. Effect of acetabular labral tears, repair and resection on hip cartilage strain: a 7T MR study. J Biomech. 2010 Mar 22;43(5):858-63. doi: 10.1016/j.jbiomech.2009.11.016. http://www.jbiomech.com/article/S0021-9290(09)00652-6/abstract (accessed 27 January 2014)
- Springer BA, et al. Acetabular labral tears: diagnostic accuracy of clinical examination by a physical therapist, orthopaedic surgeon, and orthopaedic residents. N Am J Sports Phys Ther. 2009 Feb;4(1):38-45. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2953315/pdf/najspt-04-038.pdf (accessed 27 January 2014).
- Nishii T, et al. Acetabular labral tears: contrast-enhanced MR imaging under continuous leg traction. Skeletal Radiol. 1996 May;25(4):349-56.
Presentations[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Groh MM, Herrera J. A comprehensive review of labral tears. Curr Rev Musculoskelet Med 2009 Jun;2(2):105-17.
- ↑ 2.0 2.1 Lewis CL, Sahrmann SA. Acetabular Labral Tears. Phys Ther 2006;86:110-121.
- ↑ 3.0 3.1 3.2 McCarthy JC, Noble PC, Schuck MR, et al. The Otto E. Aufranc Award: the role of labral lesions to development of early degenerative hip disease. Clin Orthop 2001;393:25–37.
- ↑ O’Leary JA, Berend K, Vail TP. The relationship between diagnosis and outcome in arthroscopy of the hip. Arthroscopy 2001;17:181–188.
- ↑ 5.0 5.1 5.2 Byrd JW. Labral lesions: an elusive source of hip pain case reports and literature review. Arthroscopy 1996;12:603–612.
- ↑ Binningsley D. Tear of the acetabular labrum in an elite athlete. Br J Sports Med 2003;37:84–88.
- ↑ 7.0 7.1 Hase T, Ueo T. Acetabularlabral tear: arthroscopic diagnosis and treatment. Arthroscopy 1999;15:138 –141.
- ↑ 8.0 8.1 Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg Br 1991;73:423– 429.
- ↑ 9.0 9.1 Narvani AA, Tsiridis E, Tai CC, Thomas P. Acetabular labrum and its tears. Br J Sports Med 2003;37:207-211.
- ↑ Lovell G. The diagnosis of chronic groin pain in athletes; a review of 189 cases. Aust J Sci Med Sport 1995;27:76-9
- ↑ Martin RL, Enseki KR, Draovitch P, et al. Acetabular labral tears of the hip: examination and diagnostic challenges. J Orthop Sports Phys Ther 2006;36:503-15.
- ↑ Dorrell JH, Catterall A. A torn acetabular labrum. J Bone Joint Surg 1986;68:400-3.
- ↑ Fitzgerald RH. Acetabular labrum tears. Diagnosis and treatment. Clin Orthop Relat Res 1995 Feb;(311):60-8.
- ↑ Leunig M, Werlen S, Ungersbock A, et al. Evaluation of the acetabulum labrum by MR arthrograpy. J Bone Joint Surg Br 1997;79:230-4
- ↑ Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for acetabular labral tears. Arthroscopy 1999;15:132–137.
- ↑ Leibold M, Huijbregts P, Jensen R. Concurrent criterion-related validity of physical examination tests for hip labral lesions: a systematic review. J Manual Manip Ther 2008;16:24-41
- ↑ Schmerl M, Pollard H, Hoskins W. Labral injuiries of the hip: a review of diagnosis and management. J Manipulative Physiol Ther 2005 Oct;28(8):632.
- ↑ 18.0 18.1 Troelsen A, Mechlenburg I, Gelineck J, Bolvig L, Jacobsen S, Søballe K. What is the role of clinical tests and ultrasound in acetabular labral tear diagnostics? Acta Orthop 2009 Jun;80(3):314-8.
- ↑ Springer BA, Gill NW, Freedman BA, Ross AE, Javernick MA, Murphy KP. Acetabular labral tears: diagnostic accuracy of clinical examination by a physical therapist, orthopaedic surgeon and orthopaedic residents. N Am J Sports Phys Ther 2009;4(1):38-45.
- ↑ British Journal of Sports. Hip & Groin Exam (7 of 7): Labral tear Available fromhttps://www.youtube.com/watch?v=Rtp4oz0_3YY. Accessed on 15/12/22.
- ↑ 21.0 21.1 Garrison C, Osler MT, Singleton SB. Rehabilitation after arthroscopy of an acetabular labral tear. N Am J Sports Phys Ther 2007;2(4):241-250
- ↑ 22.0 22.1 22.2 Yazbek PM, Ovanessian V, Martin RL, Fukuda TY. Nonsurgical treatment of acetabular labrum tears: a case series. journal of orthopaedic & sports physical therapy. 2011 May;41(5):346-53.