Menopause: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Cognitive Deficits" to "[[Cognitive Impairments") |
||
| (46 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
[[Category:Womens Health]] | [[Category:Womens Health]] | ||
[[Category:Pelvic Health]] | [[Category:Pelvic Health]] | ||
<div class="editorbox"> '''Original Editor '''- [[User: | <div class="editorbox"> '''Original Editor '''- [[User:Nicole Sandhu|Nicole Sandhu]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== | |||
Natural menopause occurs when there is a complete, or near complete, ovarian follicular depletion of a female's ovaries | == Introduction == | ||
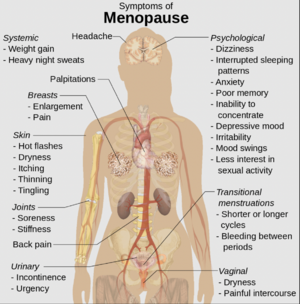
[[File:Menopause S&S.png|right|frameless]] | |||
Natural menopause occurs when there is a complete, or near-complete, ovarian follicular depletion of a female's ovaries and loss of ovarian follicular activity, resulting in the permanent cessation of her [[Menstruation and Menstrual Rehab|menstrual cycle.]]<ref name=":8">Erbil N. Attitudes towards menopause and depression, body image of women during menopause. Alexandria Journal of Medicine. 2018;54(3):241–6.</ref> It occurs at a median age of 51.4 years and the months and years leading up to this are called peri-menopause.<ref name=":9" /> Menopause before the age of 40 years old is considered abnormal.<ref name=":9">The American College of Obstetricians and Gynecologists. Menopause: Resource Overview. Available from https://www.acog.org/Womens-Health/Menopause</ref> The transition into and through menopause can have various physical, psychological, and social effects on a woman's life, <ref name=":8" /> and the ability to cope with these changes can be impacted by socioeconomic status, income, level of education, work-life, and social relations.<ref name=":10">Yangın HB, Sözer GA, Şengün N, Kukulu K. The relationship between depression and sexual function in menopause period. Maturitas. 2008;61(3):233–7.</ref> | |||
== Types of Menopause == | |||
'''Physiological Menopause:''' Also known as a spontaneous progressive decline of the menstrual cycle due to the decline of ovarian function, the average age is between 40-51 years of age. | |||
'''Pathological Menopause''' | |||
* Premature menopause: cessation of ovarian function before the age of 40.<ref>http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/womens-health/menopause/</ref> Females who experience premature menopause have a greater probability of developing early mortality and morbidity rates.<ref>Faubion SS, Kuhle CL, Shuster LT, Rocca WA. [https://www.ncbi.nlm.nih.gov/pubmed/25845383 Long-term health consequences of premature or early menopause and considerations for management. Climacteric. 2015 Jul 4;18(4):483-91.]</ref><ref>Shuster LT, Rhodes DJ, Gostout BS, Grossardt BR, Rocca WA. [https://www.sciencedirect.com/science/article/abs/pii/S0378512209002643 Premature menopause or early menopause: long-term health consequences.] Maturitas. 2010 Feb 1;65(2):161-6.</ref> | |||
* Artificial or surgical menopause: permanent cessation of ovarian function due to surgical intervention, or medical treatment like [[Chemotherapy Side Effects and Syndromes|chemotherapy]] or pelvic [[Radiation Side Effects and Syndromes|radiation therapy]].<ref>https://www.webmd.com/menopause/guide/medical-procedures-menopause</ref> | |||
* Delayed menopause: cessation of ovarian function after the age of 51. | |||
== Clinical Exam == | == Clinical Exam == | ||
=== Subjective === | |||
Symptoms of menopause and peri-menopause:<ref>[https://journals.sagepub.com/doi/full/10.1258/mi.2011.011026?casa_token=pFkyzq01Yr4AAAAA%3AS38juUhtgEkQDoHPHU3bUgbgdW-Kc5PoMYJ9oWNut9fQaEO1qV8gqgs6gsHe1KAH-vmCuTURyAuz Burger HG. Unpredictable endocrinology of the menopause transition: clinical, diagnostic and management implications. Menopause international. 2011 Dec;17(4):153-4.]</ref> | Symptoms of menopause and peri-menopause:<ref>[https://journals.sagepub.com/doi/full/10.1258/mi.2011.011026?casa_token=pFkyzq01Yr4AAAAA%3AS38juUhtgEkQDoHPHU3bUgbgdW-Kc5PoMYJ9oWNut9fQaEO1qV8gqgs6gsHe1KAH-vmCuTURyAuz Burger HG. Unpredictable endocrinology of the menopause transition: clinical, diagnostic and management implications. Menopause international. 2011 Dec;17(4):153-4.]</ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 15: | Line 24: | ||
|Hot flashes | |Hot flashes | ||
| | | | ||
* A hot flash typically begins a sudden sensation of heat in the upper chest, face, and back, often associated with perspiration<ref name=":1">Thurston RC, Joffe H. [https://www.obgyn.theclinics.com/article/S0889-8545(11)00070-2/abstract Vasomotor symptoms and menopause: findings from the Study of Women's Health across the Nation.] Obstetrics and Gynecology Clinics. 2011 Sep 1;38(3):489-501.</ref> | * A hot flash typically begins with a sudden sensation of heat in the upper chest, face, and back, often associated with perspiration.<ref name=":1">Thurston RC, Joffe H. [https://www.obgyn.theclinics.com/article/S0889-8545(11)00070-2/abstract Vasomotor symptoms and menopause: findings from the Study of Women's Health across the Nation.] Obstetrics and Gynecology Clinics. 2011 Sep 1;38(3):489-501.</ref> | ||
* Occurs in up to 85% of women. | * Occurs in up to 85% of women. | ||
* Hot flashes can begin in the late reproductive years and symptoms become more common through early menopause, late menopause, and early post menopause period.<ref name=":3">Santoro N, Epperson CN, Mathews SB. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4890704/ Menopausal symptoms and their management.] Endocrinology and Metabolism Clinics. 2015 Sep 1;44(3):497-515.</ref> | * Hot flashes can begin in the late reproductive years and symptoms become more common through early menopause, late menopause, and the early post menopause period.<ref name=":3">Santoro N, Epperson CN, Mathews SB. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4890704/ Menopausal symptoms and their management.] Endocrinology and Metabolism Clinics. 2015 Sep 1;44(3):497-515.</ref> | ||
|- | |- | ||
|Vaginal dryness and/or Sexual | |Vaginal dryness and/or Sexual dysfunction | ||
| | | | ||
* Genitourinary syndrome of menopause (GSM) | * Genitourinary syndrome of menopause (GSM) refers to atrophic symptoms that women may have in the vulvovaginal and bladder-urethral areas from the loss of estrogen that occurs with menopause. | ||
* Epithelial lining of the vagina and urethra are estrogen-dependent tissues, | * Epithelial lining of the vagina and urethra are estrogen-dependent tissues, therefore, estrogen deficiency leads to thinning of the vaginal epithelium, resulting in vaginal atrophy, which leads to dryness, itching, and often [[dyspareunia]].<ref name=":3" /> | ||
* Estrogen deficiency leads to a decrease in blood flow to the vagina and vulva, which causes decreased vaginal lubrication and sexual dysfunction.<ref name=":3" /> | * Estrogen deficiency leads to a decrease in blood flow to the vagina and vulva, which causes decreased vaginal lubrication and sexual dysfunction.<ref name=":3" /> | ||
* One of the earliest signs of estrogen insufficiency is noticed when there is a decrease in vaginal lubrication upon sexual arousal | * One of the earliest signs of estrogen insufficiency is noticed when there is a decrease in vaginal lubrication upon sexual arousal. | ||
* | * Vaginal dryness affects up to 85% of women over 40 years of age, with an additional 29-59% reporting dyspareunia and another 26-77% reporting vaginal itching and irritation. | ||
* Women may also experience heavy and unpredictable bleeding.<ref name=":10" /> | |||
|- | |- | ||
|Depression | |Depression | ||
| | | | ||
* There is a significant risk of new-onset depression during menopause when compared | * There is a significant risk of new-onset [[depression]] during menopause when compared to pre-menopausal women.<ref>Bondarev D, Sipilä S, Finni T, Kujala UM, Aukee P, Laakkonen EK, Kovanen V, Kokko K[https://journals.lww.com/menopausejournal/Abstract/publishahead/The_role_of_physical_activity_in_the_link_between.97238.aspx . The role of physical activity in the link between menopausal status and mental well-being. Menopause]. 2020 Feb 10.</ref> | ||
* There are many hypotheses as to why the rate of depression increases in menopausal women. For example, middle-aged women tend to be faced with many other challenges throughout the transition into menopause, such as grown children leaving home, marital difficulties, physical disease, and the death of parents, which can all impact one's ability to cope.<ref name=":10" /> | |||
* Changes in body shape, weight, and size, as well as sleep disturbances and changes in skin, hair, and sexual function can all contribute to depression in the menopausal years.<ref>Pearce G, Thøgersen-Ntoumani C, Duda J. Body image during the menopausal transition: a systematic scoping review. Health Psychology Review. 2013;8(4):473–89.</ref> | |||
|- | |- | ||
|Sleep disturbances | |Sleep disturbances | ||
| | | | ||
* Women with menopause report increase sleep difficulties more than women | * Women with menopause report an increase in [[Sleep Deprivation and Sleep Disorders|sleep difficulties]] more than women perimenopause such as, difficulty falling asleep and nighttime awakening. This may also be secondary to hot flashes and mood changes. | ||
* Anxiety and depression may have a negative effect on sleep during this time. | |||
* Anxiety and depression may have a negative effect on sleep during this time | * Treatment of sleep disturbance depends on clinical presentation.<ref name=":3" /> | ||
* Treatment of sleep disturbance | |||
|- | |- | ||
|Joint pain/ arthritis Musculoskeletal pain/arthralgia | |Joint pain/ arthritis Musculoskeletal pain/arthralgia | ||
| | | | ||
* Joint pain appears to increase during menopause, may be due to | * Joint pain appears to increase during menopause, which may be due to estrogen deficiency. | ||
* Analgesic | * Analgesic drugs such as oral [[NSAIDs|NSAID]]<nowiki/>s or intra-articular injections can be used as treatments. | ||
* HRT(hormonal replacement therapy) | * Although still under review, HRT (hormonal replacement therapy) has not been shown to decrease joint pain. | ||
* Musculoskeletal pain | * Musculoskeletal pain increases in both pre and post menopause, however, the mechanism in which estrogen causes musculoskeletal pain is still not clear. | ||
* Weight control and regular exercise | * Weight control and regular exercise are recommended as the best treatments for musculoskeletal pain during menopause.<ref>Watt FE. [https://journals.sagepub.com/doi/full/10.1177/2053369118757537?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed Musculoskeletal pain and menopause.] Post reproductive health. 2018 Mar;24(1):34-43.</ref> | ||
|- | |- | ||
|Cognitive changes | |[[Cognitive Impairments|Cognitive changes]] | ||
| | | | ||
* Estrogen plays a role in cognitive function | * Estrogen plays a role in cognitive function therefore, with estrogen deficiency women may experience [[memory]] loss and difficulty concentrating.<ref name=":3" /> | ||
|} | |} | ||
{{#ev:youtube|ZSRO8GsLKg8|300}}<ref>My Doctor - Kaiser Permanente. Understanding Menopause. Available from: https://www.youtube.com/watch?v=ZSRO8GsLKg8 [last accessed 18/2/2020]</ref> | {{#ev:youtube|ZSRO8GsLKg8|300}}<ref>My Doctor - Kaiser Permanente. Understanding Menopause. Available from: https://www.youtube.com/watch?v=ZSRO8GsLKg8 [last accessed 18/2/2020]</ref> | ||
Stages of Reproductive Aging Workshop (STRAW) staging system | === Objective === | ||
[[File:Menopause.jpg|thumb|300x300px]] | |||
Stages of Reproductive Aging Workshop (STRAW) is a staging system developed from data from multiple longitudinal cohort studies. This system is considered the gold standard for assessments with menopausal women and includes criteria for the reproductive years, the menopausal transition, perimenopause, final menstrual period (FMP), and postmenopause based upon bleeding patterns, endocrine findings, and symptoms. The STRAW system is used mainly in research, however, it may be helpful in the clinical setting for patients and clinicians to assess fertility potential, contraceptive needs, and the potential need for hormone therapy.<ref name=":0">Harlow S, Gass M, Hall J, Lobo R, Maki P, Rebar R, Sherman S, Sluss P, de Villiers T. [https://academic.oup.com/jcem/article/97/4/1159/2833227 Executive summary of the stages of reproductive aging workshop+ 10. Menopause.] 2012 Apr 1;19(4):387-95.</ref> | |||
{| class="wikitable" | {| class="wikitable" | ||
!Stage<ref name=":0" /> | !Stage<ref name=":0" /> | ||
| Line 63: | Line 74: | ||
|- | |- | ||
|Early menopausal transition | |Early menopausal transition | ||
| | |Marked by increased variability in menstrual cycle length | ||
|- | |- | ||
|Late menopausal transition | |Late menopausal transition | ||
|Marked by the occurrence of amenorrhea of 60 days or longer | |Marked by the occurrence of amenorrhea of 60 days or longer | ||
Characterized by increased variability in cycle length | Characterized by increased variability in cycle length and extreme fluctuations in hormonal levels | ||
|- | |- | ||
|Early postmenopause period | |Early postmenopause period | ||
| Line 77: | Line 88: | ||
|} | |} | ||
== | == Long term Effects of Menopause == | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 95: | Line 96: | ||
|Bone loss | |Bone loss | ||
| | | | ||
* The loss cortical bone affected by estrogen deficiency and | * The loss of cortical bone affected by estrogen deficiency and age related trabecular bone loss.<ref>Khosla S, Melton III LJ, Riggs BL. The unitary model for estrogen deficiency and the pathogenesis of osteoporosis: is a revision needed?. Journal of Bone and Mineral Research. 2011 Mar;26(3):441-51.</ref> | ||
|- | |- | ||
|Cardiovascular disease | |Cardiovascular disease | ||
| | | | ||
* The American College of Cardiology/American Heart Association (ACC/AHA) Guidelines recognize the postmenopausal state as a risk factor for CVD<ref>Stone NJ, Robinson JG, Lichtenstein AH, Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014 Jul 1;63(25 Part B):2889-934.</ref> | * The American College of Cardiology/American Heart Association (ACC/AHA) Guidelines recognize the postmenopausal state as a risk factor for CVD.<ref>Stone NJ, Robinson JG, Lichtenstein AH, Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014 Jul 1;63(25 Part B):2889-934.</ref> | ||
* The increased risk may be due to a change in the lipid profile | * The increased risk may be due to a change in the lipid profile - an increase in low density lipids (LDLs) in women going through menopause. <ref name=":7">.Ko SH, Kim HS. [https://www.mdpi.com/2072-6643/12/1/202/htm Menopause-Associated Lipid Metabolic Disorders and Foods Beneficial for Postmenopausal Women.] Nutrients. 2020 Jan;12(1):202.</ref> | ||
|- | |- | ||
|Body composition | |Body composition | ||
| | | | ||
* During the postmenopausal period women often gain fat mass,central abdominal fats and lose lean mass | * During the postmenopausal period women often gain fat mass, central abdominal fats, and lose lean mass. | ||
* Spontaneous decrease of activities, decrease energy expenditure, | * Spontaneous decrease of activities, decrease in energy expenditure, and decreased metabolic rate. | ||
* | * Decrease in estrogen levels accompanied by an increased level of follicle stimulating hormone. <ref name=":4">Proietto J. [https://www.racgp.org.au/afp/2017/june/obesity-and-weight-management-at-menopause/ Obesity and weight management at menopause.] Australian family physician. 2017 Jun;46(6):368.</ref> | ||
|- | |- | ||
|Balance | |Balance | ||
| | | | ||
* Estrogen deficiency has been linked with impaired balance | * Estrogen deficiency has been linked with impaired balance in postmenopausal women.<ref>Yang L, Xu Y, Zhang Y, Vijayakumar S, Jones SM, Lundberg YY. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6081893/ Mechanism underlying the effects of estrogen deficiency on otoconia.] Journal of the Association for Research in Otolaryngology. 2018 Aug 30;19(4):353-62.</ref> | ||
|} | |} | ||
== Management == | == Management == | ||
=== Physical Therapy Intervention === | |||
As part of the healthcare team, physiotherapists should be aware of the menopausal process and the symptoms that can come along with this transition. Many of the symptoms and health concerns described above can have a negative impact on women's health and overall quality of life. It is crucial to be able to identify symptoms in menopausal women through individualized assessments and provide appropriate management strategies, such as exercise and pain management, or referrals to other healthcare professionals when needed. | |||
=== Sexual Health === | |||
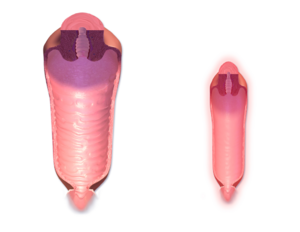
[[File:Vaginal Canal Normal vs. Menopause.png|thumb|Vaginal canal before and after menopause ]] | |||
Sexual health may be negatively impacted by some of the issues stated above. Simple, non‐hormonal interventions for sexual dysfunction are often overlooked. Several studies show that education on vaginal lubricants, moisturizers, and dilator use (as needed) can have a positive impact on sexual health.<ref name=":2">Carter J, Goldfrank D, Schover LR. Simple strategies for vaginal health promotion in cancer survivors. The journal of sexual medicine. 2011 Feb 1;8(2):549-59.</ref> [[Pelvic Floor Dysfunction|Pelvic health]] physiotherapists are well-positioned to assist patients with this. | |||
=== Exercise === | |||
Classified into: | |||
# Weight-bearing exercise: | |||
* Low impact weight-bearing activity such as walking, Tai Chi, and yoga. | |||
* High impact weight-bearing activity such as jogging and vibration platforms. | |||
2. Resistance and Strength Training Exercise: | |||
* Examples include weight lifting, swimming, cycling.<ref name=":6">[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6279907/ Hong AR, Kim SW. Effects of resistance exercise on bone health. Endocrinology and Metabolism.] 2018 Dec 1;33(4):435-44..</ref> | |||
Physical activity and exercise have been shown to have reduce the risk of osteoporosis, cardiovascular disease depression and obesity. | |||
==== Osteoporosis and Bone Density ==== | |||
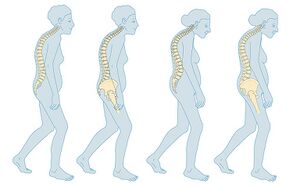
[[File:Menopause - Osteoporosis.jpeg|thumb|BMD, especially of the vertebrae, decreases with menopause]] | |||
Studies show that physiotherapists are able to assist in providing guidance around exercise and exercise prescription in people at risk of [[osteoporosis]] and reduced bone density. However, not all exercises have the same osteogenic effects on [[Bone Density|bone mineral density (BMD)]]. [[Resistance exercises|Resistance exercise]] has a stronger osteogenic effect, and for exercise to be effective its mechanical load should exceed that of [[Activities of Daily Living|activities of daily life]]. | |||
To obtain the best results, a combination of exercises that include both resistance and weight-bearing exercises is the best choice to optimize strength and function. Resistance exercise affects muscular loading whereas weight-bearing exercises have a mechanical loading effect on bone. | |||
The mechanisms in which exercise impacts bone density is still not clear but research suggests that exercise increases the activity of osteoblasts and inhibits osteoclast activity. Enhanced bone strength increases the cross-sectional area due to mechanical loading, which in turn increases bone resistance.<ref name=":6" /> A systematic review encompassing only randomized controlled trials, conducted by Howe et al. (2011), examined the effectiveness of exercise interventions in preventing bone loss and fractures in postmenopausal women, and they found that exercise was a safe and effective way to prevent bone loss in this population.<ref>Guirguis-Blake JM, Michael YL, Perdue LA, Coppola EL, Beil TL. [https://jamanetwork.com/journals/jama/article-abstract/2678103 Interventions to prevent falls in older adults:] updated evidence report and systematic review for the US preventive services task force. Jama. 2018 Apr 24;319(16):1705-16.</ref><ref name=":5">Howe TE, Shea B, Dawson LJ, Downie F, Murray A, Ross C, Harbour RT, Caldwell LM, Creed G[https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000333.pub2/abstract . Exercise for preventing and treating osteoporosis in postmenopausal women.] Cochrane database of systematic reviews. 2011(7).</ref> | |||
Additionally, higher levels of participation in physical activity were independently associated with lower weight, waist circumference, and risk of substantial weight gain.<ref name=":4" /> | Additionally, higher levels of participation in physical activity were independently associated with lower weight, waist circumference, and risk of substantial weight gain.<ref name=":4" /> | ||
==== <u>Cardiovascular Disease (CVD)</u>==== | |||
Regular and gradual aerobic exercise programs can improve cardiorespiratory endurance and decrease the risk of [[Cardiovascular Disease|Cardiovascular Disease (CVD)]]. Some research suggests that exercise increases levels of high-density lipoproteins (HDL), decreases low-density lipoproteins (LDL), and controls [[hypertension]], which in turn improves cardiovascular health.<ref>Nystoriak MA, Bhatnagar A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6172294/ Cardiovascular effects and benefits of exercise. Frontiers in cardiovascular medicine]. 2018 Sep 28;5:135.</ref> | |||
==== Depression ==== | |||
Exercise therapy has the ability to relieve some symptoms in persons with depression when compared to participants without clinical depressive symptoms.<ref>Wegner M, Helmich I, Machado S, E Nardi A, Arias-Carrión O, Budde H. [http://www.eurekaselect.com/122692/article Effects of exercise on anxiety and depression disorders: review of meta-analyses and neurobiological mechanisms.] CNS & Neurological Disorders-Drug Targets (Formerly Current Drug Targets-CNS & Neurological Disorders). 2014 Aug 1;13(6):1002-14.</ref> | |||
Research shows an increase in levels of brain-derived neurotrophic factor (BDNF) in the depressed population, however, this did not result in an improvement in depressive symptoms. The mechanisms in which exercise impacts depression is not clear.<ref>Szuhany KL, Otto MW. [https://www.sciencedirect.com/science/article/abs/pii/S0022395619314062?via%3Dihub Assessing BDNF as a mediator of the effects of exercise on depression.] Journal of Psychiatric Research. 2020 Feb 8.</ref> | |||
==== <u>Obesity</u> ==== | |||
Regular exercise programs show to increase metabolic rate and energy expenditure, promoting the loss of abdominal fats and helping with [[obesity]]. | |||
=== Aquatic Therapy === | |||
Exercise in the water allows for a reduction of stress on muscles and joints. Aquatic therapy could be a good alternative for women who experience pain due to stress on joints. | |||
==== Benefits of Aquatic Therapy ==== | |||
* The Bouncy effect protects joints from the stress of exercise that in turn relieves joint pain from conditions like arthritis. | |||
* Improves general blood circulation and reduces swelling. | |||
* Provides a comfortable environment for strengthening exercise programs | |||
* Improves cardiorespiratory capacity and endurance.<ref>Casilda-López J, Valenza MC, Cabrera-Martos I, Díaz-Pelegrina A, Moreno-Ramírez MP, Valenza-Demet G. [https://www.ncbi.nlm.nih.gov/pubmed/28141662 Effects of a dance-based aquatic exercise program in obese postmenopausal women with knee osteoarthritis]: a randomized controlled trial. Menopause. 2017 Jul 1;24(7):768-73.</ref> | |||
* Can help to improve balance. | |||
=== Diet === | |||
Physicians or a Registered Dietitian/Nutritionist can advise on the dietary needs of women going through menopause. Vitamin D and calcium supplements may benefit this population, however, a dietician or a naturopathic doctor should be consulted when determining supplementation. | |||
Patients should discuss treatment options with their | ''<u>Low caloric diet</u>'' (calculated according to each individual's total calorie intake) with <u>''exercise''</u> shows to be most effective for weight loss and loss of abdominal fats. Van Gemert and colleagues (2019) looked at an exercise program involving 4hrs/week, 60 minutes/day exercise varying between resistance and endurance exercises.<ref>Van Gemert WA, Peeters PH, May AM, Doornbos AJ, Elias SG, Van Der Palen J, Veldhuis W, Stapper M, Schuit JA, Monninkhof EM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6371569/ Effect of diet with or without exercise on abdominal fat in postmenopausal women–a randomised trial.] BMC public health. 2019 Dec 1;19(1):174.</ref> | ||
== Medical Interventions == | |||
Patients should discuss treatment options with their physician and healthcare team. This may include menopause [[Hormone Replacement Therapy|hormone replacement therapy]]<ref>Jalava-Broman J, Junttila N, Sillanmäki L, Mäkinen J, Rautava P[https://www.sciencedirect.com/science/article/pii/S0378512219305286 . Psychological behavior patterns and coping with menopausal symptoms among users and non-users of hormone replacement therapy in Finnish cohorts of women aged 52–56 years]. Maturitas. 2020 Mar 1;133:7-12.</ref> to aid with the issues listed above. Hormonal replacement therapy (HRT) may be a supportive method includes [[estrogen]] with progestin, for example, Resveratrol (phytoestrogen) has been shown to positively affect improvements in cognitive decline and cerebrovascular function.<ref>Evans HM, Howe PR, Wong RH. [https://www.ncbi.nlm.nih.gov/pubmed/28054939 Effects of resveratrol on cognitive performance, mood and cerebrovascular function in post-menopausal women; a 14-week randomised placebo-controlled intervention trial.] Nutrients. 2017 Jan;9(1):27.</ref> | |||
Psychological Intervention: Connecting with other women going through menopause or speaking to a therapist may add extra support for menopausal women. | |||
== Resources == | == Resources == | ||
| Line 167: | Line 175: | ||
For further information on managing menopause, please refer to this [https://www.youtube.com/watch?v=__YJtdBy734 presentation] by Dr. Kathryn Macaulay | For further information on managing menopause, please refer to this [https://www.youtube.com/watch?v=__YJtdBy734 presentation] by Dr. Kathryn Macaulay | ||
== References == | == References == | ||
<references /> | <references /> | ||
Latest revision as of 11:16, 17 February 2023
Introduction[edit | edit source]
Natural menopause occurs when there is a complete, or near-complete, ovarian follicular depletion of a female's ovaries and loss of ovarian follicular activity, resulting in the permanent cessation of her menstrual cycle.[1] It occurs at a median age of 51.4 years and the months and years leading up to this are called peri-menopause.[2] Menopause before the age of 40 years old is considered abnormal.[2] The transition into and through menopause can have various physical, psychological, and social effects on a woman's life, [1] and the ability to cope with these changes can be impacted by socioeconomic status, income, level of education, work-life, and social relations.[3]
Types of Menopause[edit | edit source]
Physiological Menopause: Also known as a spontaneous progressive decline of the menstrual cycle due to the decline of ovarian function, the average age is between 40-51 years of age.
Pathological Menopause
- Premature menopause: cessation of ovarian function before the age of 40.[4] Females who experience premature menopause have a greater probability of developing early mortality and morbidity rates.[5][6]
- Artificial or surgical menopause: permanent cessation of ovarian function due to surgical intervention, or medical treatment like chemotherapy or pelvic radiation therapy.[7]
- Delayed menopause: cessation of ovarian function after the age of 51.
Clinical Exam[edit | edit source]
Subjective[edit | edit source]
Symptoms of menopause and peri-menopause:[8]
| Symptoms | Information |
|---|---|
| Hot flashes |
|
| Vaginal dryness and/or Sexual dysfunction |
|
| Depression |
|
| Sleep disturbances |
|
| Joint pain/ arthritis Musculoskeletal pain/arthralgia |
|
| Cognitive changes |
Objective[edit | edit source]
Stages of Reproductive Aging Workshop (STRAW) is a staging system developed from data from multiple longitudinal cohort studies. This system is considered the gold standard for assessments with menopausal women and includes criteria for the reproductive years, the menopausal transition, perimenopause, final menstrual period (FMP), and postmenopause based upon bleeding patterns, endocrine findings, and symptoms. The STRAW system is used mainly in research, however, it may be helpful in the clinical setting for patients and clinicians to assess fertility potential, contraceptive needs, and the potential need for hormone therapy.[15]
| Stage[15] | Signs/Symptoms[15] |
|---|---|
| Late reproductive years | May begin to notice changes in her menstrual cycle (ie. a shorter cycle) |
| Early menopausal transition | Marked by increased variability in menstrual cycle length |
| Late menopausal transition | Marked by the occurrence of amenorrhea of 60 days or longer
Characterized by increased variability in cycle length and extreme fluctuations in hormonal levels |
| Early postmenopause period | Corresponds to the end of “perimenopause,” a term still in common usage that means the time around menopause |
| Late postmenopause period | Symptoms of vaginal dryness and urogenital atrophy become increasingly prevalent at this time |
Long term Effects of Menopause[edit | edit source]
| Health Concerns | Information |
|---|---|
| Bone loss |
|
| Cardiovascular disease | |
| Body composition |
|
| Balance |
|
Management[edit | edit source]
Physical Therapy Intervention[edit | edit source]
As part of the healthcare team, physiotherapists should be aware of the menopausal process and the symptoms that can come along with this transition. Many of the symptoms and health concerns described above can have a negative impact on women's health and overall quality of life. It is crucial to be able to identify symptoms in menopausal women through individualized assessments and provide appropriate management strategies, such as exercise and pain management, or referrals to other healthcare professionals when needed.
Sexual Health[edit | edit source]
Sexual health may be negatively impacted by some of the issues stated above. Simple, non‐hormonal interventions for sexual dysfunction are often overlooked. Several studies show that education on vaginal lubricants, moisturizers, and dilator use (as needed) can have a positive impact on sexual health.[21] Pelvic health physiotherapists are well-positioned to assist patients with this.
Exercise[edit | edit source]
Classified into:
- Weight-bearing exercise:
- Low impact weight-bearing activity such as walking, Tai Chi, and yoga.
- High impact weight-bearing activity such as jogging and vibration platforms.
2. Resistance and Strength Training Exercise:
- Examples include weight lifting, swimming, cycling.[22]
Physical activity and exercise have been shown to have reduce the risk of osteoporosis, cardiovascular disease depression and obesity.
Osteoporosis and Bone Density[edit | edit source]
Studies show that physiotherapists are able to assist in providing guidance around exercise and exercise prescription in people at risk of osteoporosis and reduced bone density. However, not all exercises have the same osteogenic effects on bone mineral density (BMD). Resistance exercise has a stronger osteogenic effect, and for exercise to be effective its mechanical load should exceed that of activities of daily life.
To obtain the best results, a combination of exercises that include both resistance and weight-bearing exercises is the best choice to optimize strength and function. Resistance exercise affects muscular loading whereas weight-bearing exercises have a mechanical loading effect on bone.
The mechanisms in which exercise impacts bone density is still not clear but research suggests that exercise increases the activity of osteoblasts and inhibits osteoclast activity. Enhanced bone strength increases the cross-sectional area due to mechanical loading, which in turn increases bone resistance.[22] A systematic review encompassing only randomized controlled trials, conducted by Howe et al. (2011), examined the effectiveness of exercise interventions in preventing bone loss and fractures in postmenopausal women, and they found that exercise was a safe and effective way to prevent bone loss in this population.[23][24]
Additionally, higher levels of participation in physical activity were independently associated with lower weight, waist circumference, and risk of substantial weight gain.[19]
Cardiovascular Disease (CVD)[edit | edit source]
Regular and gradual aerobic exercise programs can improve cardiorespiratory endurance and decrease the risk of Cardiovascular Disease (CVD). Some research suggests that exercise increases levels of high-density lipoproteins (HDL), decreases low-density lipoproteins (LDL), and controls hypertension, which in turn improves cardiovascular health.[25]
Depression[edit | edit source]
Exercise therapy has the ability to relieve some symptoms in persons with depression when compared to participants without clinical depressive symptoms.[26]
Research shows an increase in levels of brain-derived neurotrophic factor (BDNF) in the depressed population, however, this did not result in an improvement in depressive symptoms. The mechanisms in which exercise impacts depression is not clear.[27]
Obesity[edit | edit source]
Regular exercise programs show to increase metabolic rate and energy expenditure, promoting the loss of abdominal fats and helping with obesity.
Aquatic Therapy[edit | edit source]
Exercise in the water allows for a reduction of stress on muscles and joints. Aquatic therapy could be a good alternative for women who experience pain due to stress on joints.
Benefits of Aquatic Therapy[edit | edit source]
- The Bouncy effect protects joints from the stress of exercise that in turn relieves joint pain from conditions like arthritis.
- Improves general blood circulation and reduces swelling.
- Provides a comfortable environment for strengthening exercise programs
- Improves cardiorespiratory capacity and endurance.[28]
- Can help to improve balance.
Diet[edit | edit source]
Physicians or a Registered Dietitian/Nutritionist can advise on the dietary needs of women going through menopause. Vitamin D and calcium supplements may benefit this population, however, a dietician or a naturopathic doctor should be consulted when determining supplementation.
Low caloric diet (calculated according to each individual's total calorie intake) with exercise shows to be most effective for weight loss and loss of abdominal fats. Van Gemert and colleagues (2019) looked at an exercise program involving 4hrs/week, 60 minutes/day exercise varying between resistance and endurance exercises.[29]
Medical Interventions[edit | edit source]
Patients should discuss treatment options with their physician and healthcare team. This may include menopause hormone replacement therapy[30] to aid with the issues listed above. Hormonal replacement therapy (HRT) may be a supportive method includes estrogen with progestin, for example, Resveratrol (phytoestrogen) has been shown to positively affect improvements in cognitive decline and cerebrovascular function.[31]
Psychological Intervention: Connecting with other women going through menopause or speaking to a therapist may add extra support for menopausal women.
Resources[edit | edit source]
American College of Obstetricians and Gynecologists: Menopause Resource Overview
For further information on managing menopause, please refer to this presentation by Dr. Kathryn Macaulay
References[edit | edit source]
- ↑ 1.0 1.1 Erbil N. Attitudes towards menopause and depression, body image of women during menopause. Alexandria Journal of Medicine. 2018;54(3):241–6.
- ↑ 2.0 2.1 The American College of Obstetricians and Gynecologists. Menopause: Resource Overview. Available from https://www.acog.org/Womens-Health/Menopause
- ↑ 3.0 3.1 3.2 Yangın HB, Sözer GA, Şengün N, Kukulu K. The relationship between depression and sexual function in menopause period. Maturitas. 2008;61(3):233–7.
- ↑ http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/womens-health/menopause/
- ↑ Faubion SS, Kuhle CL, Shuster LT, Rocca WA. Long-term health consequences of premature or early menopause and considerations for management. Climacteric. 2015 Jul 4;18(4):483-91.
- ↑ Shuster LT, Rhodes DJ, Gostout BS, Grossardt BR, Rocca WA. Premature menopause or early menopause: long-term health consequences. Maturitas. 2010 Feb 1;65(2):161-6.
- ↑ https://www.webmd.com/menopause/guide/medical-procedures-menopause
- ↑ Burger HG. Unpredictable endocrinology of the menopause transition: clinical, diagnostic and management implications. Menopause international. 2011 Dec;17(4):153-4.
- ↑ Thurston RC, Joffe H. Vasomotor symptoms and menopause: findings from the Study of Women's Health across the Nation. Obstetrics and Gynecology Clinics. 2011 Sep 1;38(3):489-501.
- ↑ 10.0 10.1 10.2 10.3 10.4 Santoro N, Epperson CN, Mathews SB. Menopausal symptoms and their management. Endocrinology and Metabolism Clinics. 2015 Sep 1;44(3):497-515.
- ↑ Bondarev D, Sipilä S, Finni T, Kujala UM, Aukee P, Laakkonen EK, Kovanen V, Kokko K. The role of physical activity in the link between menopausal status and mental well-being. Menopause. 2020 Feb 10.
- ↑ Pearce G, Thøgersen-Ntoumani C, Duda J. Body image during the menopausal transition: a systematic scoping review. Health Psychology Review. 2013;8(4):473–89.
- ↑ Watt FE. Musculoskeletal pain and menopause. Post reproductive health. 2018 Mar;24(1):34-43.
- ↑ My Doctor - Kaiser Permanente. Understanding Menopause. Available from: https://www.youtube.com/watch?v=ZSRO8GsLKg8 [last accessed 18/2/2020]
- ↑ 15.0 15.1 15.2 Harlow S, Gass M, Hall J, Lobo R, Maki P, Rebar R, Sherman S, Sluss P, de Villiers T. Executive summary of the stages of reproductive aging workshop+ 10. Menopause. 2012 Apr 1;19(4):387-95.
- ↑ Khosla S, Melton III LJ, Riggs BL. The unitary model for estrogen deficiency and the pathogenesis of osteoporosis: is a revision needed?. Journal of Bone and Mineral Research. 2011 Mar;26(3):441-51.
- ↑ Stone NJ, Robinson JG, Lichtenstein AH, Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014 Jul 1;63(25 Part B):2889-934.
- ↑ .Ko SH, Kim HS. Menopause-Associated Lipid Metabolic Disorders and Foods Beneficial for Postmenopausal Women. Nutrients. 2020 Jan;12(1):202.
- ↑ 19.0 19.1 Proietto J. Obesity and weight management at menopause. Australian family physician. 2017 Jun;46(6):368.
- ↑ Yang L, Xu Y, Zhang Y, Vijayakumar S, Jones SM, Lundberg YY. Mechanism underlying the effects of estrogen deficiency on otoconia. Journal of the Association for Research in Otolaryngology. 2018 Aug 30;19(4):353-62.
- ↑ Carter J, Goldfrank D, Schover LR. Simple strategies for vaginal health promotion in cancer survivors. The journal of sexual medicine. 2011 Feb 1;8(2):549-59.
- ↑ 22.0 22.1 Hong AR, Kim SW. Effects of resistance exercise on bone health. Endocrinology and Metabolism. 2018 Dec 1;33(4):435-44..
- ↑ Guirguis-Blake JM, Michael YL, Perdue LA, Coppola EL, Beil TL. Interventions to prevent falls in older adults: updated evidence report and systematic review for the US preventive services task force. Jama. 2018 Apr 24;319(16):1705-16.
- ↑ Howe TE, Shea B, Dawson LJ, Downie F, Murray A, Ross C, Harbour RT, Caldwell LM, Creed G. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane database of systematic reviews. 2011(7).
- ↑ Nystoriak MA, Bhatnagar A. Cardiovascular effects and benefits of exercise. Frontiers in cardiovascular medicine. 2018 Sep 28;5:135.
- ↑ Wegner M, Helmich I, Machado S, E Nardi A, Arias-Carrión O, Budde H. Effects of exercise on anxiety and depression disorders: review of meta-analyses and neurobiological mechanisms. CNS & Neurological Disorders-Drug Targets (Formerly Current Drug Targets-CNS & Neurological Disorders). 2014 Aug 1;13(6):1002-14.
- ↑ Szuhany KL, Otto MW. Assessing BDNF as a mediator of the effects of exercise on depression. Journal of Psychiatric Research. 2020 Feb 8.
- ↑ Casilda-López J, Valenza MC, Cabrera-Martos I, Díaz-Pelegrina A, Moreno-Ramírez MP, Valenza-Demet G. Effects of a dance-based aquatic exercise program in obese postmenopausal women with knee osteoarthritis: a randomized controlled trial. Menopause. 2017 Jul 1;24(7):768-73.
- ↑ Van Gemert WA, Peeters PH, May AM, Doornbos AJ, Elias SG, Van Der Palen J, Veldhuis W, Stapper M, Schuit JA, Monninkhof EM. Effect of diet with or without exercise on abdominal fat in postmenopausal women–a randomised trial. BMC public health. 2019 Dec 1;19(1):174.
- ↑ Jalava-Broman J, Junttila N, Sillanmäki L, Mäkinen J, Rautava P. Psychological behavior patterns and coping with menopausal symptoms among users and non-users of hormone replacement therapy in Finnish cohorts of women aged 52–56 years. Maturitas. 2020 Mar 1;133:7-12.
- ↑ Evans HM, Howe PR, Wong RH. Effects of resveratrol on cognitive performance, mood and cerebrovascular function in post-menopausal women; a 14-week randomised placebo-controlled intervention trial. Nutrients. 2017 Jan;9(1):27.