Quadriceps Muscle Contusion: Difference between revisions
No edit summary |
No edit summary |
||
| (7 intermediate revisions by the same user not shown) | |||
| Line 3: | Line 3: | ||
== Introduction == | == Introduction == | ||
[[File:Hematoma VL quads.png|thumb|416x416px|Hematoma progression [[Vastus Lateralis|Vastus lateralis]]]] | [[File:Hematoma VL quads.png|thumb|416x416px|Hematoma progression [[Vastus Lateralis|Vastus lateralis]]]] | ||
Contusion injuries to the [[Quadriceps Muscle|quadriceps]] are common in athletics. Usually the mechanism of injury is a direct blow to the quadriceps causing significant muscle damage. Contusions cause rupture to the muscle fibers at or directly adjacent to the area of impact, usually leading to hematoma formation within the muscle causing pain and loss of motion. A contracted muscle will absorb force better and result in a less severe injury. | Contusion injuries to the [[Quadriceps Muscle|quadriceps]] are common in athletics. Usually the mechanism of injury is a direct blow to the quadriceps causing significant [[Muscle Injuries|muscle damage]]. Contusions cause rupture to the [[Muscle Cells (Myocyte)|muscle fibers]] at or directly adjacent to the area of impact, usually leading to hematoma formation within the muscle causing [[Pain Assessment|pain]] and loss of motion. A contracted muscle will absorb force better and result in a less severe injury. | ||
* In sports without padding for the thigh and upper leg, eg soccer and rugby, quadriceps contusions are a major disabling injury. Better protective equipment may decreasing the frequency of this injury, however, research is | * In sports without padding for the thigh and upper leg, eg soccer and rugby, quadriceps contusions are a major disabling injury. Better [[Protective Sports Equipments|protective equipment]] may decreasing the frequency of this injury, however, research is scant.<ref>Kary JM. Diagnosis and management of quadriceps strains and contusions. Current reviews in musculoskeletal medicine. 2010 Oct;3(1):26-31. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2941577/<nowiki/>(accessed 5.12.2022)</ref> | ||
* Quadriceps contusions can lead to two serious complications: [[Compartment Syndrome]] and [[Myositis Ossificans of the Quadriceps|myositis ossificans.]]<ref name=":0">Kary JM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2941577/ Diagnosis and management of quadriceps strains and contusions]. Current reviews in musculoskeletal medicine. 2010 Oct 1;3(1-4):26-31 '''Level of evidence 2A'''</ref> <ref name=":3">Christopher M. Larson, MD; Louis C. Almekinders, MD; Spero G. Karas, MD; William E. Garrett, MD, PhD. [https://www.ncbi.nlm.nih.gov/pubmed/20086513 Evaluating and managing muscle contusions and myositis ossificans].2002 Feb;30(2):41-50.'''Level of evidence 5'''</ref> | * Quadriceps contusions can lead to two serious complications: [[Compartment Syndrome]] and [[Myositis Ossificans of the Quadriceps|myositis ossificans.]]<ref name=":0">Kary JM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2941577/ Diagnosis and management of quadriceps strains and contusions]. Current reviews in musculoskeletal medicine. 2010 Oct 1;3(1-4):26-31 '''Level of evidence 2A'''</ref> <ref name=":3">Christopher M. Larson, MD; Louis C. Almekinders, MD; Spero G. Karas, MD; William E. Garrett, MD, PhD. [https://www.ncbi.nlm.nih.gov/pubmed/20086513 Evaluating and managing muscle contusions and myositis ossificans].2002 Feb;30(2):41-50.'''Level of evidence 5'''</ref> | ||
| Line 16: | Line 16: | ||
Muscle contusions are caused by direct trauma. Direct trauma can affect any part of the quadriceps femoris, with the vastus intermedius muscle most commonly affected.<ref name=":8" /> | Muscle contusions are caused by direct trauma. Direct trauma can affect any part of the quadriceps femoris, with the vastus intermedius muscle most commonly affected.<ref name=":8" /> | ||
The injury consists of a well-defined sequence of events | The injury consists of a well-defined sequence of events | ||
If there is major untreated and/or unresolved bleeding deep in the muscle tissue, [[Myositis Ossificans of the Quadriceps|myositis ossificans]] can occur. | * [[Muscle Injuries|Myonecrosis]] and hematoma forms followed by scar formation then [[Muscle Injuries: Regeneration Strategies|muscle regeneration]] | ||
* Small muscle fiber tears lead to hemorrhage and swelling into the anterior compartment<ref name=":9">Orthobullets Quadriceps Contusion Available:https://www.orthobullets.com/knee-and-sports/3103/quadriceps-contusion (accessed 5.12.2022)</ref> | |||
* If there is major untreated and/or unresolved bleeding deep in the muscle tissue, [[Myositis Ossificans of the Quadriceps|myositis ossificans]] can occur.<ref name=":8" /> | |||
== Clinical Presentation == | == Clinical Presentation == | ||
| Line 36: | Line 38: | ||
|Normal | |Normal | ||
| | | | ||
* Capillary rupture: Blood into connective tissue | * [[Capillaries|Capillary]] rupture: Blood into [[Connective Tissue|connective tissue]] | ||
* Mild ecchymosis | * Mild ecchymosis | ||
* Feels soreness after cooling down or the following day | * Feels soreness after cooling down or the following day | ||
* The injured area may be tender to touch | * The injured area may be tender to touch | ||
* Ability to stretch the muscle may be reduced slightly. | * Ability to [[Stretching|stretch]] the muscle may be reduced slightly. | ||
* The strength of the muscle may also be slightly affected. | * The [[Muscle Strength Testing|strength]] of the muscle may also be slightly affected. | ||
|6 days | |6 days | ||
|- | |- | ||
| Line 67: | Line 69: | ||
<br> | <br> | ||
== | == Presentation == | ||
The diagnosis is made by questioning an accurate history from the patient and completing a physical examination. | The diagnosis is made by questioning an accurate history from the patient and completing a physical examination. | ||
=== | === Examination === | ||
* Pain: worsening severity over the first 24-48 hours; worse with dynamic movements and with knee flexion | |||
* | * Observation: Antalgic gait | ||
* Palpation: possible palpable defect indicating partial or complete muscle tear, swelling, ecchymosis, point tenderness. | |||
* | * Circumference measures: compare thigh firmness and circumference to contralateral side | ||
* Strength testing of the quadriceps: resist knee extension and hip flexion, compared to the uninjured side, helps in assessing severity of injury. | |||
* Measurement of knee flexion is used as a prognostic indicator in quadriceps contusions. Based on this, thigh contusions can be graded into 3 groups that are based on the severity of injury | |||
* Provocative tests: active straight leg raise to test integrity of extensor mechanism | |||
* | * Neurovascular: distal neurovascular exam to evaluate for thigh compartment syndrome.<ref name=":9" /><ref name=":1">Alonso A, Hekeik P, Adams R. [https://www.ncbi.nlm.nih.gov/pubmed/11676801 Predicting a recovery time from the initial assessment of a quadriceps contusion injury.] Aust J Physiother. 2000;46(3):167-77.'''Level of evidence 1A''' | ||
* | </ref> | ||
< | |||
== Outcome Measures == | == Outcome Measures == | ||
The [[Lower Extremity Functional Scale (LEFS)|‘Lower Extremity Functional Scale]]’ is used to evaluate the functionality for a wide range of lower limb conditions to know whether the person is having any difficulty with certain activities. | The [[Lower Extremity Functional Scale (LEFS)|‘Lower Extremity Functional Scale]]’ is used to evaluate the functionality for a wide range of lower limb conditions to know whether the person is having any difficulty with certain activities. | ||
== Imaging == | == Imaging == | ||
The best techniques for measuring the soft tissue damage and for complications caused by the initial injury are [[MRI Scans|magnetic resonance imaging (MRI)]] and [[Ultrasound Scans|diagnostic ultrasound]]. Both have been highly sensitive to oedema and haemorrhage. These methods are expensive but can speed up the healing process by detecting the severity quick. <ref name=":1" /> <ref name=":6">Shawn Bonsell,* MD, Paul T. Freudigman, MD, and Howard A. Moore, MD. [http://journals.sagepub.com/doi/abs/10.1177/03635465010290062501?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed Quadriceps Muscle Contusion Resulting in Osteomyelitis of the Femur in a High School Football Player]. American journal of sports medicine. 2001;29(6)818-820. '''Level of evidence 3B'''</ref>Ultrasound can be used to identify a localized hematoma formation caused from a contusion and provide real-time imaging for needle aspiration. If there is concern for bony involvement, radiographs will evaluate for bony injury. Subsequently, radiographs are useful in identifying heterotopic bone formation, known as myositis ossificans (MO), which is a delayed complication of severe muscle contusions. | The best techniques for measuring the soft tissue damage and for complications caused by the initial injury are [[MRI Scans|magnetic resonance imaging (MRI)]] and [[Ultrasound Scans|diagnostic ultrasound]]. Both have been highly sensitive to oedema and haemorrhage. These methods are expensive but can speed up the healing process by detecting the severity quick. <ref name=":1" /> <ref name=":6">Shawn Bonsell,* MD, Paul T. Freudigman, MD, and Howard A. Moore, MD. [http://journals.sagepub.com/doi/abs/10.1177/03635465010290062501?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed Quadriceps Muscle Contusion Resulting in Osteomyelitis of the Femur in a High School Football Player]. American journal of sports medicine. 2001;29(6)818-820. '''Level of evidence 3B'''</ref>Ultrasound can be used to identify a localized hematoma formation caused from a contusion and provide real-time imaging for needle aspiration. If there is concern for bony involvement, radiographs will evaluate for bony injury. Subsequently, radiographs are useful in identifying heterotopic bone formation, known as myositis ossificans (MO), which is a delayed complication of severe muscle contusions. | ||
== Risk factors == | == Risk factors == | ||
* Contact sports and sports that require quick starts, i.e. running races and other track events. | * Contact sports and sports that require quick starts, i.e. running races and other track events. | ||
| Line 147: | Line 100: | ||
* Medical history of any bleeding disorder.<ref>Quadriceps Contusion (Cork Thigh).Available from https://sma.org.au/resources-advice/injury-fact-sheets/quadriceps-contusion-cork-thigh/. Accessed on 17 August 2018. | * Medical history of any bleeding disorder.<ref>Quadriceps Contusion (Cork Thigh).Available from https://sma.org.au/resources-advice/injury-fact-sheets/quadriceps-contusion-cork-thigh/. Accessed on 17 August 2018. | ||
</ref> | </ref> | ||
== | == Management == | ||
First line of treatment for acute injuries, begin immediately to minimize hematoma formation: immobilisation, cryotherapy, [[NSAIDs|NSAID]]<nowiki/>s, physical therapy.<ref name=":9" /> | |||
After three to four weeks, if the patient still moves with pain and isn’t able to perform a painless, full range of motion, radiographic imaging should be performed. This is to detect whether myositis ossificans is present. | # NSAIDs can be useful short term for decreasing pain, long-term use of NSAIDs for contusions is usually not necessary and is discouraged. NSAIDs have been promoted for prevention of myositis ossificans after severe quadriceps contusions. Evidence for this use is inferred from studies showing a decrease in heterotopic bone formation after total hip replacement in those patients given indomethacin for at least 7 days. | ||
# After three to four weeks, if the patient still moves with pain and isn’t able to perform a painless, full range of motion, radiographic imaging should be performed. This is to detect whether myositis ossificans is present. <ref name=":6" /> <ref name=":4">Diaz JA, Fischer DA, Rettig AC, Davis TJ, Shelbourne KD. [http://journals.sagepub.com/doi/abs/10.1177/03635465030310022201?journalCode=ajsb Severe quadriceps muscle contusions in athletes]: a report of three cases. The American Journal of Sports Medicine. 2003 Mar;31(2):289-93.'''Level of evidence 3A'''</ref> | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
The main goals of therapy with patient with a quadriceps muscle contusion are relieving the pain and improving the ROM. The treatment is non-operative and exists out of three phases:<ref name=":6" /> | |||
#<sup></sup>Rest, ice, compression.Compression is important in order to limit the hemorrhage for the first 24 to 48 hours. Immobilization in 120 degrees of flexion using an ace wrap or hinged knee brace immediately after injury for 24-48 hours, frequent use of cold therapy. Knee flexed helps to avoid muscle stiffness | |||
# <sup></sup>Rest, ice, compression.Compression is important in order to limit the hemorrhage for the first 24 to 48 hours. | |||
# Active and passive quadriceps muscle stretching with emphasis on knee flexion.After 24 h, the brace or wrap should be removed and gentle, active, pain-free range of motion at the knee should be instituted along with stretching and isometric quadriceps strengthening. The active phase of treatment, including functional rehabilitation, can begin when pain-free, active knee flexion of at least 120° is attained. | # Active and passive quadriceps muscle stretching with emphasis on knee flexion.After 24 h, the brace or wrap should be removed and gentle, active, pain-free range of motion at the knee should be instituted along with stretching and isometric quadriceps strengthening. The active phase of treatment, including functional rehabilitation, can begin when pain-free, active knee flexion of at least 120° is attained. | ||
# | # Begin functional rehabilitation and sport-specific activities once full and pain-free ROM achieved | ||
== Return to sports criteria == | == Return to sports criteria == | ||
The athlete should be pain free, attain 120° of knee flexion with hip extended, and perform all aspects of functional field testing without limitations . Protective thigh padding is recommended prior to resuming sports in order to reduce recurrence. See [[Return to Sport]]. A five step approach in aim to reach maximum functional recovery, see image below. | |||
[[File:Return to Sport.png|center|frameless|749x749px]] | |||
== Viewing == | |||
# How to treat a bruise / haematoma / swelling of the quadriceps using [[Kinesio Taping|kinesiology tape]] (4 minutes viewing) | |||
{{#ev:youtube|VIGIgEHN-wA}}2. Steve Jurch of Jurch Performance Education Discusses Contusions & How to Speed up Recovery Time (15 minutes viewing){{#ev:youtube|y6wdY7ikkgM}} | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Contusions are one of the most common muscle injuries besides muscle-strains. They can sometimes evolve to a more complicated injury such as myositis ossificans or compartment syndrome, to which you have to pay attention. The options for treatment are mostly physiotherapy and in some serious complications an operation will be needed. Physiotherapy is designed to reduce the pain and improve the ROM of the patients, by giving cryokinetics, soft tissue massage and electrotherapy. | Contusions are one of the most common muscle injuries besides muscle-strains. They can sometimes evolve to a more complicated injury such as myositis ossificans or compartment syndrome, to which you have to pay attention. The options for treatment are mostly physiotherapy and in some serious complications an operation will be needed. Physiotherapy is designed to reduce the pain and improve the ROM of the patients, by giving cryokinetics, soft tissue massage and electrotherapy. | ||
Latest revision as of 07:19, 5 December 2022
Introduction[edit | edit source]
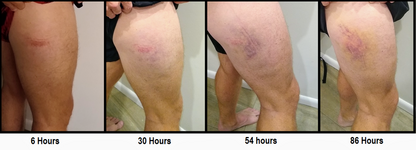
Contusion injuries to the quadriceps are common in athletics. Usually the mechanism of injury is a direct blow to the quadriceps causing significant muscle damage. Contusions cause rupture to the muscle fibers at or directly adjacent to the area of impact, usually leading to hematoma formation within the muscle causing pain and loss of motion. A contracted muscle will absorb force better and result in a less severe injury.
- In sports without padding for the thigh and upper leg, eg soccer and rugby, quadriceps contusions are a major disabling injury. Better protective equipment may decreasing the frequency of this injury, however, research is scant.[1]
- Quadriceps contusions can lead to two serious complications: Compartment Syndrome and myositis ossificans.[2] [3]
Epidemiology[edit | edit source]
Demographics: 2:1 male: female ratio
Athletes: football, soccer, rugby most common sports; more common during competition than practice.
Pathophysiology[edit | edit source]
Muscle contusions are caused by direct trauma. Direct trauma can affect any part of the quadriceps femoris, with the vastus intermedius muscle most commonly affected.[4]
The injury consists of a well-defined sequence of events
- Myonecrosis and hematoma forms followed by scar formation then muscle regeneration
- Small muscle fiber tears lead to hemorrhage and swelling into the anterior compartment[5]
- If there is major untreated and/or unresolved bleeding deep in the muscle tissue, myositis ossificans can occur.[4]
Clinical Presentation[edit | edit source]
Quadriceps muscle contusions are easily elucidated by a history of blunt trauma and clinical examination usually reveals skin discolouration, tenderness, swelling and varying degrees of pain and tenderness alongside a limited range of motion and difficulties to weight bear.[4]
Classification[edit | edit source]
Next to muscle strains is traumatic muscle contusions the most frequent type of quadriceps injury in sports. A direct external forceful blow to the quadriceps causing significant muscle damage is the usual mechanism of this injury. In comparison to strains, contusions will cause rupture to the muscle fibers at or directly adjacent to the area of impact. This typically leads to hematoma formation within the muscle causing pain and loss of motion. The extent of pain and loss of movement will be dependent on the amount of fore and the impact of the force at the time of trauma. [2] [6] [7]Quadriceps contusions are graded mild, moderate or severe between 12 and 24 hours. A mild contusion has more than 90 degrees of knee flexion; moderate between 45 and 90 degrees of knee flexion and severe less than 45 grades of knee flexion. [8]
There are three grades in contusions: [6][9]
| Pain | Active knee flexion | Gait | Description | Average loss of activity |
|---|---|---|---|---|
| Mild | > 90degree | Normal |
|
6 days |
| Moderate | 45 - 90 degree | Antalgic |
|
56 days |
| Severe | < 45 degree | Severely antalgic |
|
> 60 days |
Presentation[edit | edit source]
The diagnosis is made by questioning an accurate history from the patient and completing a physical examination.
Examination[edit | edit source]
- Pain: worsening severity over the first 24-48 hours; worse with dynamic movements and with knee flexion
- Observation: Antalgic gait
- Palpation: possible palpable defect indicating partial or complete muscle tear, swelling, ecchymosis, point tenderness.
- Circumference measures: compare thigh firmness and circumference to contralateral side
- Strength testing of the quadriceps: resist knee extension and hip flexion, compared to the uninjured side, helps in assessing severity of injury.
- Measurement of knee flexion is used as a prognostic indicator in quadriceps contusions. Based on this, thigh contusions can be graded into 3 groups that are based on the severity of injury
- Provocative tests: active straight leg raise to test integrity of extensor mechanism
- Neurovascular: distal neurovascular exam to evaluate for thigh compartment syndrome.[5][10]
Outcome Measures[edit | edit source]
The ‘Lower Extremity Functional Scale’ is used to evaluate the functionality for a wide range of lower limb conditions to know whether the person is having any difficulty with certain activities.
Imaging[edit | edit source]
The best techniques for measuring the soft tissue damage and for complications caused by the initial injury are magnetic resonance imaging (MRI) and diagnostic ultrasound. Both have been highly sensitive to oedema and haemorrhage. These methods are expensive but can speed up the healing process by detecting the severity quick. [10] [11]Ultrasound can be used to identify a localized hematoma formation caused from a contusion and provide real-time imaging for needle aspiration. If there is concern for bony involvement, radiographs will evaluate for bony injury. Subsequently, radiographs are useful in identifying heterotopic bone formation, known as myositis ossificans (MO), which is a delayed complication of severe muscle contusions.
Risk factors[edit | edit source]
- Contact sports and sports that require quick starts, i.e. running races and other track events.
- Warm up and cool down habits.
- Off season/preseason/season training habits.
- Poor muscle conditioning.
- Playing position.
- Level of competition.
- Protective equipment use.
- Playing experience.
- Injury history, especially to the thigh, hip and/or knee.
- Medical history of any bleeding disorder.[12]
Management[edit | edit source]
First line of treatment for acute injuries, begin immediately to minimize hematoma formation: immobilisation, cryotherapy, NSAIDs, physical therapy.[5]
- NSAIDs can be useful short term for decreasing pain, long-term use of NSAIDs for contusions is usually not necessary and is discouraged. NSAIDs have been promoted for prevention of myositis ossificans after severe quadriceps contusions. Evidence for this use is inferred from studies showing a decrease in heterotopic bone formation after total hip replacement in those patients given indomethacin for at least 7 days.
- After three to four weeks, if the patient still moves with pain and isn’t able to perform a painless, full range of motion, radiographic imaging should be performed. This is to detect whether myositis ossificans is present. [11] [13]
Physical Therapy Management[edit | edit source]
The main goals of therapy with patient with a quadriceps muscle contusion are relieving the pain and improving the ROM. The treatment is non-operative and exists out of three phases:[11]
- Rest, ice, compression.Compression is important in order to limit the hemorrhage for the first 24 to 48 hours. Immobilization in 120 degrees of flexion using an ace wrap or hinged knee brace immediately after injury for 24-48 hours, frequent use of cold therapy. Knee flexed helps to avoid muscle stiffness
- Active and passive quadriceps muscle stretching with emphasis on knee flexion.After 24 h, the brace or wrap should be removed and gentle, active, pain-free range of motion at the knee should be instituted along with stretching and isometric quadriceps strengthening. The active phase of treatment, including functional rehabilitation, can begin when pain-free, active knee flexion of at least 120° is attained.
- Begin functional rehabilitation and sport-specific activities once full and pain-free ROM achieved
Return to sports criteria[edit | edit source]
The athlete should be pain free, attain 120° of knee flexion with hip extended, and perform all aspects of functional field testing without limitations . Protective thigh padding is recommended prior to resuming sports in order to reduce recurrence. See Return to Sport. A five step approach in aim to reach maximum functional recovery, see image below.
Viewing[edit | edit source]
- How to treat a bruise / haematoma / swelling of the quadriceps using kinesiology tape (4 minutes viewing)
2. Steve Jurch of Jurch Performance Education Discusses Contusions & How to Speed up Recovery Time (15 minutes viewing)
Clinical Bottom Line[edit | edit source]
Contusions are one of the most common muscle injuries besides muscle-strains. They can sometimes evolve to a more complicated injury such as myositis ossificans or compartment syndrome, to which you have to pay attention. The options for treatment are mostly physiotherapy and in some serious complications an operation will be needed. Physiotherapy is designed to reduce the pain and improve the ROM of the patients, by giving cryokinetics, soft tissue massage and electrotherapy.
References[edit | edit source]
- ↑ Kary JM. Diagnosis and management of quadriceps strains and contusions. Current reviews in musculoskeletal medicine. 2010 Oct;3(1):26-31. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2941577/(accessed 5.12.2022)
- ↑ 2.0 2.1 Kary JM. Diagnosis and management of quadriceps strains and contusions. Current reviews in musculoskeletal medicine. 2010 Oct 1;3(1-4):26-31 Level of evidence 2A
- ↑ Christopher M. Larson, MD; Louis C. Almekinders, MD; Spero G. Karas, MD; William E. Garrett, MD, PhD. Evaluating and managing muscle contusions and myositis ossificans.2002 Feb;30(2):41-50.Level of evidence 5
- ↑ 4.0 4.1 4.2 Radiopedia Quadriceps Injury Available:https://radiopaedia.org/articles/quadriceps-injury (accessed 5.12.2022)
- ↑ 5.0 5.1 5.2 Orthobullets Quadriceps Contusion Available:https://www.orthobullets.com/knee-and-sports/3103/quadriceps-contusion (accessed 5.12.2022)
- ↑ 6.0 6.1 Faude O, Rößler R, Junge A. Football injuries in children and adolescent players: are there clues for prevention?. Sports medicine. 2013 Sep 1;43(9):819-37 Level of evidence 2A
- ↑ G. Pasta, G. Nanni, [...], and S. Bianchi. Journal of ultrasound. Sonography of the quadriceps muscle: Examination technique, normal anatomy, and traumatic lesions. 2010 Jun; 13(2):76-84. Level of evidence 2A
- ↑ Huntoon EA. Essentials of Physical Medicine and Rehabilitation. InMayo Clinic Proceedings 2003 Apr 1 (Vol. 78, No. 4, p. 291). Elsevier.
- ↑ Lee JC, Mitchell AW, Healy JC. Imaging of muscle injury in the elite athlete. The British journal of radiology. 2012 Aug;85(1016):1173-85.
- ↑ 10.0 10.1 Alonso A, Hekeik P, Adams R. Predicting a recovery time from the initial assessment of a quadriceps contusion injury. Aust J Physiother. 2000;46(3):167-77.Level of evidence 1A
- ↑ 11.0 11.1 11.2 Shawn Bonsell,* MD, Paul T. Freudigman, MD, and Howard A. Moore, MD. Quadriceps Muscle Contusion Resulting in Osteomyelitis of the Femur in a High School Football Player. American journal of sports medicine. 2001;29(6)818-820. Level of evidence 3B
- ↑ Quadriceps Contusion (Cork Thigh).Available from https://sma.org.au/resources-advice/injury-fact-sheets/quadriceps-contusion-cork-thigh/. Accessed on 17 August 2018.
- ↑ Diaz JA, Fischer DA, Rettig AC, Davis TJ, Shelbourne KD. Severe quadriceps muscle contusions in athletes: a report of three cases. The American Journal of Sports Medicine. 2003 Mar;31(2):289-93.Level of evidence 3A







