Romberg Test: Difference between revisions
No edit summary |
No edit summary |
||
| Line 2: | Line 2: | ||
== Purpose<br> == | == Purpose<br> == | ||
The Romberg test is used to demonstrate the effects of posterior column disease upon human upright postural control. Posterior column disease | The Romberg test is used to demonstrate the effects of posterior column disease upon human upright postural control. Posterior column disease involves selective damaging of the posterior column, known as tabes dorsalis neurosyphilis. The Romberg test is used by physiotherapists for the clinical assessment of patients with disequilibrium or ataxia from sensory and motor disorders. | ||
A patient who has a problem with [[proprioception]] can still maintain balance by compensating with vestibular function and vision. In the Romberg test, the patient stands upright and asked to close his eyes. A loss of balance is interpreted as a positive Romberg sign. | |||
The Romberg test was first described in 1846 and was originally described for the condition tabes dorsalis. Before performing the Romberg test, it is necessary to test other aspects of the patient's balance when potential issues with ataxia or disequilibrium are present. Often, proprioceptive challenges are not the first problems faced by this population. Sometimes, it is more simple. It is important to first assess other aspects of balance impairment in order to rule out confounding factors that could lead to a false positive test<ref name="Goebel">Goebel JA. Practical management of the dizzy patient. Philadelphia: Lippincott Williams &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Wilkins, 2008.</ref><ref name="Black">Black FO, et al. Normal subject postural sway during the Romberg test. Am J Otolaryngol. 1982 Sep-Oct;3(5):309-18.</ref>. | |||
== | == Clinically Relevant Anatomy<br> == | ||
There are three sensory systems that provide input to the cerebellum to maintain truncal stability when the eyes are open: | |||
#Vision | |||
#[[Proprioception|Proprioception]] | |||
#Vestibular sense. | |||
Only two of the three systems are needed to maintain balance. When visual input is removed, instability due to lack of vision can be teased apart from other sensory impairments. If there is a more severe proprioceptive or vestibular lesion, or if there is a midline cerebellar lesion causing truncal instability, the patient will be unable to maintain the standing position, even when the eyes are open. Note that instability can also be seen with lesions in other parts of the nervous system, such as the upper or lower motor neurons, or the basal ganglia<ref name="Blumenfeld">Blumenfeld, H. Neuroexam.com - Romberg test. www.neuroexam.com/neuroexam/content.php?p=37 (accessed 31 Dec 2013).</ref><ref name="Zelczak">Zelczak TA. Neurologic examination. www.pacificu.edu/optometry/ce/courses/15840/neuroexampg3.cfm (accessed 31 Dec 2013).</ref>. | |||
== Technique<br> == | == Technique<br> == | ||
=== The | === The Original Romberg test === | ||
The test is performed as follows: | |||
#The patient is asked to remove his shoes and stand with his two feet together. The arms are held next to the body or crossed in front of the body. | |||
#The clinician asks the patient to first stand quietly with eyes open, and subsequently with eyes closed. The patient tries to maintain his balance. For safety, it is essential that the observer stand close to the patient to prevent potential injury if the patient were to fall. When the patients closes his eyes, he should not orient himself by light, sense or sound, as this could influence the test result and cause a false positive outcome. | |||
#The Romberg test is scored by counting the seconds the patient is able to stand with eyes closed. | |||
<br> | <br> | ||
[[Image:Romberg.jpg|243x257px]] | |||
The literature does not report alternative methods for scoring a Romberg test. | |||
To make the Romberg test more difficult, the clinician can attempt to disturb the patient's balance with a perturbation. It is important that the clinician does not exaggerate the perturbation. | |||
A Romberg test can also be used as follow-up assessment for patients with balance and/or proprioception impairments by comparing several different assessments with each other. | |||
If the clinician observes that the patient is able to stand for longer periods of time with the eyes closed, it is evident that the patient's balance and proprioceptive deficits have decreased<ref name="Goebel" /><ref name="Johnson">Johnson BG, et al. The sharpened Romberg test for assessing ataxia in mild acute mountain sickness. Wilderness Environ Med. 2005 Summer;16(2):62-6.</ref><ref name="Black" /><ref name="Brinkman">Brinkman DMC, et al. Kwantificering en evaluatie van 5 neurologische evenwichtstests bij proefpersonen en patiënten. Ned Tijdschr Geneeskd. 1996;140:2176-80.</ref>. | |||
The Romberg test is positive when the patient is unable to maintain balance with their eyes closed. Losing balance can be defined as increased body sway, placing one foot in the direction of the fall, or even falling. | |||
<br> | <br> | ||
{{#ev:youtube|YBQNwvWgREU|300}} | |||
<br> | <br> | ||
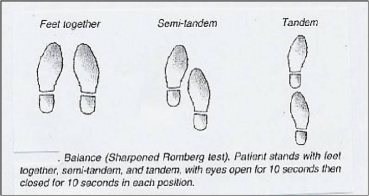
=== The Sharpened or Tandem Romberg test === | |||
The Sharpened or Tandem Romberg test is a variation of the original test. The implementation is mostly the same. For this second test, the patient has to place his feet in heel-to-toe position, with one foot directly in front of the other. As with the original Romberg test, the assessment is performed first with eyes open and then with eyes closed. The patient crosses his arms over his chest, and the open palm of the hand lies on the opposite shoulder. The patient also distributes his weight over both his feet and holds his chin parallel with the floor<ref name="Johnson" /><ref name="Black" />. <br> | |||
[[Image:Romberg 2.jpg|369x224px]] | |||
Obese and older individuals may be unable to stand in this position for prolonged periods of time. For these populations, the Romberg test does not exclusively demonstrate propropioceptive impairments in comparison to other confounding factors<ref name="Goebel" />.<br> | |||
{{#ev:youtube|NS6XtWFbqjc|300}} | |||
== Variables<br> == | |||
= | Although a patient with an acute peripheral vestibular lesion is usually inclined to move towards the side of the problem, it has been shown that chronic vestibular damage (at least partial compensation) does not produce deficits in the standard Romberg test. As well, an individual with proprioceptive problems, accessory to tabes dorsalis, would be unable to stand with the eyes closed and feet together<ref name="Goebel" />. | ||
Many believe that the sharpened Romberg test is a better indicator of vestibular impairment than the original Romberg test. The sharpened Romberg test results give an objective measure of postural stability. This can help to quantify ataxia<ref name="Goebel" />. | |||
Subject, sex, and age do not create a statistically significant difference between normal subjects between the ages of 20 and 49 years; only the Romberg sharpened test with eyes open provided a significant difference (p< 0.05) between men and women. Greater instability in subjects less than 20 and more than 50 years of age was also exhibited. When comparing a young and an old cohort, there is a significant difference in performance. | |||
Increasing the difficulty of the tandem Romberg test for patients is not helpful because it also makes the tests more difficult to perform for controls with no symptoms of vestibular disease. This would also make it harder to evaluate the test results. Decreased performance times on the modified Romberg is associated with a concomitant rise in the risk of falling<ref name="Black" /><ref name="Longridge">Longridge NS. Clinical romberg testing does not detect vestibular disease. Otol Neurotol. 2010 Jul;31(5):803-6.</ref><ref name="Agrawal">Agrawal Y. The modified Romberg balance test: normative data in US adults. Otol Neurotol, 2011 Oct,32(8):1309–1311.</ref>. | |||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | ||
Revision as of 05:12, 1 January 2014
Top Contributors - Bart Moreels, Sheik Abdul Khadir, Kim Jackson, Lucinda hampton, Daphne Jackson, Tony Lowe, Scott Buxton, Joao Costa, Lauren Lopez, Admin, Alyssa Brooks-Wells, Evan Thomas, Naomi O'Reilly, Sinead Greenan, WikiSysop, Karen Wilson and Claire Knott
Purpose
[edit | edit source]
The Romberg test is used to demonstrate the effects of posterior column disease upon human upright postural control. Posterior column disease involves selective damaging of the posterior column, known as tabes dorsalis neurosyphilis. The Romberg test is used by physiotherapists for the clinical assessment of patients with disequilibrium or ataxia from sensory and motor disorders.
A patient who has a problem with proprioception can still maintain balance by compensating with vestibular function and vision. In the Romberg test, the patient stands upright and asked to close his eyes. A loss of balance is interpreted as a positive Romberg sign.
The Romberg test was first described in 1846 and was originally described for the condition tabes dorsalis. Before performing the Romberg test, it is necessary to test other aspects of the patient's balance when potential issues with ataxia or disequilibrium are present. Often, proprioceptive challenges are not the first problems faced by this population. Sometimes, it is more simple. It is important to first assess other aspects of balance impairment in order to rule out confounding factors that could lead to a false positive test[1][2].
Clinically Relevant Anatomy
[edit | edit source]
There are three sensory systems that provide input to the cerebellum to maintain truncal stability when the eyes are open:
- Vision
- Proprioception
- Vestibular sense.
Only two of the three systems are needed to maintain balance. When visual input is removed, instability due to lack of vision can be teased apart from other sensory impairments. If there is a more severe proprioceptive or vestibular lesion, or if there is a midline cerebellar lesion causing truncal instability, the patient will be unable to maintain the standing position, even when the eyes are open. Note that instability can also be seen with lesions in other parts of the nervous system, such as the upper or lower motor neurons, or the basal ganglia[3][4].
Technique
[edit | edit source]
The Original Romberg test[edit | edit source]
The test is performed as follows:
- The patient is asked to remove his shoes and stand with his two feet together. The arms are held next to the body or crossed in front of the body.
- The clinician asks the patient to first stand quietly with eyes open, and subsequently with eyes closed. The patient tries to maintain his balance. For safety, it is essential that the observer stand close to the patient to prevent potential injury if the patient were to fall. When the patients closes his eyes, he should not orient himself by light, sense or sound, as this could influence the test result and cause a false positive outcome.
- The Romberg test is scored by counting the seconds the patient is able to stand with eyes closed.
The literature does not report alternative methods for scoring a Romberg test.
To make the Romberg test more difficult, the clinician can attempt to disturb the patient's balance with a perturbation. It is important that the clinician does not exaggerate the perturbation.
A Romberg test can also be used as follow-up assessment for patients with balance and/or proprioception impairments by comparing several different assessments with each other.
If the clinician observes that the patient is able to stand for longer periods of time with the eyes closed, it is evident that the patient's balance and proprioceptive deficits have decreased[1][5][2][6].
The Romberg test is positive when the patient is unable to maintain balance with their eyes closed. Losing balance can be defined as increased body sway, placing one foot in the direction of the fall, or even falling.
The Sharpened or Tandem Romberg test[edit | edit source]
The Sharpened or Tandem Romberg test is a variation of the original test. The implementation is mostly the same. For this second test, the patient has to place his feet in heel-to-toe position, with one foot directly in front of the other. As with the original Romberg test, the assessment is performed first with eyes open and then with eyes closed. The patient crosses his arms over his chest, and the open palm of the hand lies on the opposite shoulder. The patient also distributes his weight over both his feet and holds his chin parallel with the floor[5][2].
Obese and older individuals may be unable to stand in this position for prolonged periods of time. For these populations, the Romberg test does not exclusively demonstrate propropioceptive impairments in comparison to other confounding factors[1].
Variables
[edit | edit source]
Although a patient with an acute peripheral vestibular lesion is usually inclined to move towards the side of the problem, it has been shown that chronic vestibular damage (at least partial compensation) does not produce deficits in the standard Romberg test. As well, an individual with proprioceptive problems, accessory to tabes dorsalis, would be unable to stand with the eyes closed and feet together[1].
Many believe that the sharpened Romberg test is a better indicator of vestibular impairment than the original Romberg test. The sharpened Romberg test results give an objective measure of postural stability. This can help to quantify ataxia[1].
Subject, sex, and age do not create a statistically significant difference between normal subjects between the ages of 20 and 49 years; only the Romberg sharpened test with eyes open provided a significant difference (p< 0.05) between men and women. Greater instability in subjects less than 20 and more than 50 years of age was also exhibited. When comparing a young and an old cohort, there is a significant difference in performance.
Increasing the difficulty of the tandem Romberg test for patients is not helpful because it also makes the tests more difficult to perform for controls with no symptoms of vestibular disease. This would also make it harder to evaluate the test results. Decreased performance times on the modified Romberg is associated with a concomitant rise in the risk of falling[2][7][8].
Recent Related Research (from Pubmed)[edit | edit source]
References
[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Goebel JA. Practical management of the dizzy patient. Philadelphia: Lippincott Williams &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Wilkins, 2008.
- ↑ 2.0 2.1 2.2 2.3 Black FO, et al. Normal subject postural sway during the Romberg test. Am J Otolaryngol. 1982 Sep-Oct;3(5):309-18.
- ↑ Blumenfeld, H. Neuroexam.com - Romberg test. www.neuroexam.com/neuroexam/content.php?p=37 (accessed 31 Dec 2013).
- ↑ Zelczak TA. Neurologic examination. www.pacificu.edu/optometry/ce/courses/15840/neuroexampg3.cfm (accessed 31 Dec 2013).
- ↑ 5.0 5.1 Johnson BG, et al. The sharpened Romberg test for assessing ataxia in mild acute mountain sickness. Wilderness Environ Med. 2005 Summer;16(2):62-6.
- ↑ Brinkman DMC, et al. Kwantificering en evaluatie van 5 neurologische evenwichtstests bij proefpersonen en patiënten. Ned Tijdschr Geneeskd. 1996;140:2176-80.
- ↑ Longridge NS. Clinical romberg testing does not detect vestibular disease. Otol Neurotol. 2010 Jul;31(5):803-6.
- ↑ Agrawal Y. The modified Romberg balance test: normative data in US adults. Otol Neurotol, 2011 Oct,32(8):1309–1311.