Spondyloarthropathy--AS: Difference between revisions
No edit summary |
No edit summary |
||
| Line 149: | Line 149: | ||
== Medical Management <br> == | == Medical Management <br> == | ||
According to Braun et al <ref name="0">Braun, J. von, Van Den Berg, R., Baraliakos, X., et al. 2010 update of the ASAS/EULAR recommendations for the management of ankylosing spondylitis. Annals of the rheumatic diseases, 2011, vol. 70, no 6, p. 896-904. | |||
Level of Evidence 5</ref> (2010, Level of Evidence 5) the overarching principles of the management of patients with AS are: | |||
*Requirement of a multidisciplinary treatment coordinated by the rheumatologist. | |||
*The primary goal is to maximise long term health-related quality of life. Therefore it is important to control symptoms and inflammation, prevent progressive structural damage, preserve/normalise function and social participation. | |||
*The treatment should aim at the best care and requisites a shared decision between the patient and the rheumatologist. | |||
*A combination of non-pharmacological and pharmacological treatment modalities is required. | |||
1. General treatment | |||
The treatment of patients with AS should be individualised according to: | |||
*The present manifestations of the disease (peripheral, axial, entheseal, extra-articular symptoms and signs). | |||
*The level of current symptoms, prognostic indicators and clinical findings. | |||
*The general clinical status (gender, age, comorbidity, psychosocial factors, concomitant medications). | |||
2. Disease monitoring | |||
The disease monitoring of patients with AS should include: | |||
*Patient history (eg, questionnaires) | |||
*Laboratory tests | |||
*Clinical parameters | |||
*Imaging | |||
*The frequency of monitoring should be individualised depending on: course of symptoms, treatment and severity | |||
3. Non-pharmacological treatment | |||
*Patient education and regular exercise form the cornerstone of non-pharmacological treatment of patients with AS. | |||
*Home exercises are effective. However, physical therapy with supervised exercises, land or water based, individually or in a group, should be preferred as these are more effective than home exercises. | |||
*Self-help groups and patient associations may be useful. | |||
4. Extra-articular manifestations and comorbidities | |||
*Psoriasis, uveitis and IBD are some of the frequently observed extra-articular manifestations. They should be managed in collaboration with the respective specialists. | |||
*Rheumatologists should be aware of the increased risk of cardiovascular disease and osteoporosis in patients with AS. | |||
5. Non-steroidal anti-inflammatory drugs | |||
*For AS patients with pain and stiffness, NSAID, including Coxibs, are recommended as first-line drug treatment. | |||
*For patients with persistently active, symptomatic disease, continuous treatment with NSAID is preferred.<br> | |||
6. Analgesics: after previously recommended treatments have failed, are contraindicated, and/or poorly tolerated.<br><br>7. Anti-TNF therapy | |||
*According to the ASAS recommendations, anti-TNF therapy should be given to patients with persistently high disease activity despite conventional treatments.<br> | |||
*Shifting to a second TNF blocker may be beneficial, especially in patients with loss of response. | |||
*No evidence exists to support the use of biological agents other than TNF inhibitors in AS. | |||
8. Surgery | |||
*In patients with refractory pain or disability and radiographic evidence of structural damage, independent of age, total hip arthroplasty should be considered. | |||
*In patients with severe disabling deformity, spinal corrective osteotomy may be considered. | |||
*A spinal surgeon should be consulted in patients with AS and an acute vertebral fracture. | |||
9. Changes in the disease course: Other causes than inflammation (eg. spinal fracture) should be considered if a significant change in the course of the disease occurs and appropriate evaluation, including imaging, should be performed.<br> | |||
== Physical Therapy Management <br> == | == Physical Therapy Management <br> == | ||
Revision as of 21:14, 1 February 2017
Original Editors
Top Contributors - Adam Bockey, Elise Jespers, Elaine Lonnemann, Kim Jackson, Admin, 127.0.0.1, WikiSysop, Wendy Walker and Lucinda hampton
Search Strategy[edit | edit source]
Keywords: spondyloartrhropathy, ankylosing spondylitis, Reiter's syndrome, Marie-Strumpell disease, bamboo spine
Databases: PubMed, Pedro, Web of Science, emedicine
Definition/Description[edit | edit source]
Spondyloarthropathies are a diverse group of inflammatory arthritides that share certain genetic predisposing factors and clinical features. The group primarily includes Ankylosing Spondylitis, reactive arthritis (including Reiter’s syndrome), psoriatic arthritis, inflammatory bowel disease–associated spondyloarthropathy, and undifferentiated spondyloarthropathy.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Level 5
The primary pathologic sites are the sacroiliac joints, the bony insertions of the annulus fibrosis of the intervertebral discs, and the apophyseal joints of the spine.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
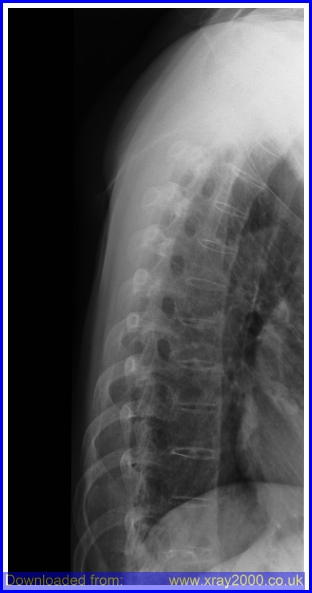
Ankylosing Spondylitis (AS) also known as Marie- Strumpell disease or bamboo spine, is an inflammatory arthropathy of the axial skeleton, usually involving the sacroiliac joints, apophyseal joints, costovertebral joints, and intervertebral disc articulations.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title AS is a chronic progressing inflammatory disease that causes inflammation of the spinal joints that can lead to severe, chronic pain and discomfort. In advanced stages, the inflammation can lead to new bone formation of the spine, causing the spine to fuse in a fixed position often creating a forward stooped posture.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Clinically Relevant Anatomy[edit | edit source]
The vertebral column exists of 24 vertebrae: seven cervical vertebrae, twelve thoracic vertebrae and five lumbar vertebrae. The vertebrae are joined together by ligaments and separated by intervertebral discs. The discs exist of an inner nucleus pulposus and an outer annulus fibrosis, consisting of fibrocartilage rings.
Patients with spondyloarthropathy have a high propensity for inflammation at the sites where tendons, ligaments and joint capsules attach to the bone. These sites are known as entheses. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleLevel 5
The sacroiliac joint consists of a cartilaginous part and a fibrous (or ligamentous) compartment with very strong anterior and posterior sacroiliac ligaments. This makes the SIJ an amphiarthrosis with movement restricted to slight rotation and translation. Another specific feature of the SIJs is that two different types of cartilage cover the two articular surfaces. While the sacral cartilage is purely hyaline, the iliac side is covered by a mixture of hyaline and fibrous cartilage. Due to its fibrocartilaginous components, the sacroiliac joint is a so-called articular enthesis.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleLevel 1B
Epidemiology /Etiology[edit | edit source]
Ankylosing spondylitis (the most common spondyloarthropathy) has a prevalence of 0.1 to 0.2 percent in the general U.S. population and is related to the prevalence of HLA-B27. Diagnostic criteria for the spondyloarthropathies have been developed for research purposes, the criteria rarely are almost not used in clinical practice. There is no laboratory test to diagnose ankylosing spondylitis but the HLA-B27 gene has been found to be present in about 90 to 95 percent of affected white patients in central Europe and North America Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleLevel 5
AS is 3 times more common in men than in women and most often begins between the ages of 20-40.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title (Level 5) Recent studies have shown that AS may be just as prevalent in women, but diagnosed less often because of a milder disease course with fewer spinal problems and more involvement of joints such as the knees and ankles. Prevalence of AS is nearly 2 million people or 0.1% to 0.2% of the general population in the United States. It occurs more often in Caucasians and some Native American than in African Americans, Asians, or other nonwhite groups.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title AS is 10 to 20 times more common with first degree relatives of AS patients than in the general population. The risk of AS in first degree relatives with the HLA-B27 allele is about 20%.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Characteristics/Clinical Presentation[edit | edit source]
The most characteristic feature of spondyloarthropathies is inflammatory back pain. Another characteristic feature is enthesitis, which involves inflammation at sites where tendons, ligaments, or joint capsules attach to bone.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Level 5 Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Level 5
Additional clinical features include inflammatory back pain, dactylitis, and extra-articular manifestations such as uveitis and skin rash.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Level 5
There can also be buttock, or hip pain and stiffness for more than 3 months in a person, usually male under 40 years of age.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title It is mostly worse in the morning, lasting more than 1 hour and is described as a dull ache that is poorly localized, but it can be intermittently sharp or jolting. Overtime pain can become severe and constant and coughing, sneezing, and twisting motions may worsen the pain. Pain may radiate to the thighs, but does not typically go below the knee. Buttock pain is often unilateral, but may alternate from side to side.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Paravertebral muscle spasm, aching, and stiffness are common, making sacrioliac areas and spinous process very tender upon palpation.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title A flexed posture eases the back pain and paraspinal muscle spasm; therefore, kyphosis is common in untreated patients.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Enthesitis (inflammation of tendons, ligaments, and capsular attachments to bone) may cause pain or stiffness and restriction of mobility in the axial skeleton.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Dactylitis (inflammation of an entire digit), commonly termed “sausage digit,” also occurs in the spondyloarthropathies and is thought to arise from joint and tenosynovial inflammation Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Level 5.
Since AS is a systemic disease an intermittent low grade fever, fatigue, or weight loss can occur.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
In advanced stages the spine can become fused and a loss of normal lordosis with accompanying increased kyphosis of the thoracic spine, painful limitations of cervical joint motion, and loss of spine flexibility in all planes of motion. A decrease in chest wall excursion less than 2 cm could be an indicator of AS because chest wall excursion is an indicator of decreased axial skeleton mobility.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Anterior uveitis is the most frequent extra-articular manifestation, occurring in 25 to 30 percent of patients. The uveitis usually is acute, unilateral, and recurrent. Eye pain, red eye, blurry vision, photophobia, and increased lacrimation are presenting signs. Cardiac manifestations include aortic and mitral root dilatation, with regurgitation and conduction defects. Fibrosis may develop in the upper lobes of the lungs in patients with longstanding disease. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Level 5
Differential Diagnosis[edit | edit source]
Most Common differential diagnosisCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
- Rheumatoid arthritis
- Psoriasis
- Reiter's syndrome
- Fracture
- Osteoarthritis
- Inflammatory bowel diseaseCite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title : Ulcerative colitis and Crohn’s disease - Psoriatic spondylitis Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Scheuermann’s disease Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Paget’s disease Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title Level 5
Differential Diagnosis of Ankylosing Spondylitis and Thoracic Spinal StenosisCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
| Ankylosing Spondylitis | Thoracic Spinal Stenosis | |
|---|---|---|
| History | Morning stiffness Intermittent aching pain Male predominance Sharp pain Bilateral sacroiliac pain may refer to posterior thigh |
Intermittent aching pain Pain may refer to both legs with walking |
| Active movements | Restricted | May be normal |
| Passive movements | Restricted | May be normal |
| Resisted isometric movements |
Normal | Normal |
| Special tests | None | Bicycle test of van Gelderen may be positive Stoop test may be positive |
| Reflexes | Normal | May be affected in long standing cases |
| Sensory deficit | None | Usually temporary |
| Diagnostic imaging | Plain films are diagnostic | Computed tomography scans are diagnostic |
In the early stages of ankylosing spondylitis, the changes in the sacroiliac joint are similar to that of rheumatoid arthritis, however the changes are almost always bilateral and symmetrical. This fact allows ankylosing spondylitis to be distinguished from psoriasis, Reiter's syndrome, and infection. Changes at the sacroiliac joint occur throughout the joint, but are predominantly found on the iliac side.
Diagnostic Procedures[edit | edit source]
AS can be diagnosed by the modified New York criteria, the patient must have radiographic evidence of sacroiliitis and one of the following: (1) restriction of the lumbar spine motion in both the sagittal and frontal planes, (2) restriction of chest expansion (usually < 2.5 cm) (3) a history of back pain includes onset at <40 year, gradual onset, morning stiffness, improvement with activity, and duration >3 months.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Imaging tests
- X-rays. Radiographic findsing of symmetric, bilateral sacroiliitis include blurring of joint margins, extaarticular sclerosis, erosion, and joint space narrowing. As bony tissue bridges the vertebral bodies and posterior arches, the lumbar and thoracic spine creates a “bamboo spine” image on radiographs.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Computerized tomography (CT). CT scans combine X-ray views taken from many different angles into a cross-sectional image of internal structures. CT scans provide more detail, and more radiation exposure, than do plain X-rays.Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Magnetic resonance imaging (MRI). Intraarticular inflammation, early cartilage changes and underlying bone marrow edema and osteitis can be seen using an MRI technique called short tau inversion recovery (STIR). Using radio waves and a strong magnetic field, MRI scans are better at visualizing soft tissues such as cartilage. Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title - Lab tests. There is no laboratory test to diagnose ankylosing spondylitis but the HLA-B27 gene has been found to be present in about 90 to 95 percent of affected white patients in central Europe and North America Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title Level 5. The presence of the HLA-B27 antigen is a useful adjunct to the diagnosis, but cannot be diagnostic alone.Cite error: Invalid<ref>tag; name cannot be a simple integer. Use a descriptive title
Four out of five positive responses to the following questions may help with the determining of AS:
- Did the back discomfort begin before age 40
- Did the discomfort begin slowly
- Has the discomfort persisted for 3 months
- Was morning stiffness a problem
- Did the discomfort improve with exercise
Specificity= 0.82, Sensitivity =0.23
LR for four out of five positive responses = 1.3Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Chronic low back pain (LBP), the leading symptom of ankylosing spondylitis (AS) and undifferentiated axial spondyloarthritis (SpA), precedes the development of radiographic sacroiliitis, sometimes by many years. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Level 4
It is also noted that patients with ankylosing spondylitis (AS) have an increased risk of bone loss and vertebral fractures. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Level 3B
In summary, the diagnostic procedures for Ankylosing Spondylitis include:
- Imaging tests such as X-ray and CT scans
- HLA B27 gene presence (genetical factor)
- Blood samples with focus on CRP levels
- BASDAI, BASMI and BASFI Cite error: Invalid
<ref>tag; name cannot be a simple integer. Use a descriptive title Level 1B
Outcome Measures[edit | edit source]
Modified Health Assessment Questionnaire (MHAQ)
Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Level 1B
ASQoL Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Level 1B
Assessment of the duration of morning stiffness using “0–10 cm” horizontal visual analogue scale, as well as duration of morning stiffness in minutes. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Level 1B
Self-report joint tenderness: this is carried out on a joint diagram with the joint names written beside it as a guide and the patient is asked to tick the box matching the painful joint(s) [30] Level 1B
Self-reported soft tissue tenderness (enthesitis): this is carried out on a skeleton model and the patient is asked to highlight the places he feels pain. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Level 1B
Examination[edit | edit source]
Physical examination of the spine involves the cervical, thoracic and lumbar region.
Cervical involvement often occurs late. The stooping of the neck can be measured by the occiput-to-wall distance. The patient stands with the back and heels against the wall and the distance between the back of the head and the wall is measured. Video occiput-to-wall test
The thoracic spine can be tested by the chest expansion. It is measured at the fourth intercostal space and in women just below the breasts. The patient should be asked to force a maximal inspiration and expiration and the difference in chest expansion is measured. A chest expansion of less than 5 cm is suspicious and < 2.5 cm is abnormal and raises the possibility of AS unless there is another reason for it, like emphysema. The normal thoracic kyphosis of the dorsal spine is accentuated. The costovertebral, costotransverse and manubriosternal joints should be palpated to detect inflammation which causes pain on palpitation.
The lumbar spine can be tested by the Schober’s test. This is performed by making a mark between the posterior superior iliac spines at the 5th lumbar spinous process. A second mark is placed 10 cm above the first one and the patient is asked to bend forward with extended knees. The distance between the two marks increases from 10 to at least 15 cm in normal people, but only to 13 or less in case of AS. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Level 5
Medical Management
[edit | edit source]
According to Braun et al Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title (2010, Level of Evidence 5) the overarching principles of the management of patients with AS are:
- Requirement of a multidisciplinary treatment coordinated by the rheumatologist.
- The primary goal is to maximise long term health-related quality of life. Therefore it is important to control symptoms and inflammation, prevent progressive structural damage, preserve/normalise function and social participation.
- The treatment should aim at the best care and requisites a shared decision between the patient and the rheumatologist.
- A combination of non-pharmacological and pharmacological treatment modalities is required.
1. General treatment
The treatment of patients with AS should be individualised according to:
- The present manifestations of the disease (peripheral, axial, entheseal, extra-articular symptoms and signs).
- The level of current symptoms, prognostic indicators and clinical findings.
- The general clinical status (gender, age, comorbidity, psychosocial factors, concomitant medications).
2. Disease monitoring
The disease monitoring of patients with AS should include:
- Patient history (eg, questionnaires)
- Laboratory tests
- Clinical parameters
- Imaging
- The frequency of monitoring should be individualised depending on: course of symptoms, treatment and severity
3. Non-pharmacological treatment
- Patient education and regular exercise form the cornerstone of non-pharmacological treatment of patients with AS.
- Home exercises are effective. However, physical therapy with supervised exercises, land or water based, individually or in a group, should be preferred as these are more effective than home exercises.
- Self-help groups and patient associations may be useful.
4. Extra-articular manifestations and comorbidities
- Psoriasis, uveitis and IBD are some of the frequently observed extra-articular manifestations. They should be managed in collaboration with the respective specialists.
- Rheumatologists should be aware of the increased risk of cardiovascular disease and osteoporosis in patients with AS.
5. Non-steroidal anti-inflammatory drugs
- For AS patients with pain and stiffness, NSAID, including Coxibs, are recommended as first-line drug treatment.
- For patients with persistently active, symptomatic disease, continuous treatment with NSAID is preferred.
6. Analgesics: after previously recommended treatments have failed, are contraindicated, and/or poorly tolerated.
7. Anti-TNF therapy
- According to the ASAS recommendations, anti-TNF therapy should be given to patients with persistently high disease activity despite conventional treatments.
- Shifting to a second TNF blocker may be beneficial, especially in patients with loss of response.
- No evidence exists to support the use of biological agents other than TNF inhibitors in AS.
8. Surgery
- In patients with refractory pain or disability and radiographic evidence of structural damage, independent of age, total hip arthroplasty should be considered.
- In patients with severe disabling deformity, spinal corrective osteotomy may be considered.
- A spinal surgeon should be consulted in patients with AS and an acute vertebral fracture.
9. Changes in the disease course: Other causes than inflammation (eg. spinal fracture) should be considered if a significant change in the course of the disease occurs and appropriate evaluation, including imaging, should be performed.
Physical Therapy Management
[edit | edit source]
add text here
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.