Thoracic Spine Fracture: Difference between revisions
Abbey Wright (talk | contribs) (removed dead links) |
Kim Jackson (talk | contribs) mNo edit summary |
||
| (35 intermediate revisions by 4 users not shown) | |||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
[[File:T9-T10 change fracture from MVA.png|thumb|348x348px|T9-T10 chance fracture from MVA]] | |||
Most [[Thoracic Vertebrae|thoracic spine]] [[Fracture|fractures]] occur in the lower thoracic spine, with 60% to 70% of thoraco-lumbar fractures occurring in the T11 to L2 region, which is bio-mechanically weak for stress. The majority of these fractures occur without spinal cord injury. 20 to 40% of the fractures are associated with neurological injuries. | |||
Major (high-energy) trauma, is the most common cause of thoracic fractures such as falls from height or road traffic accidents.<ref>Leucht P, Fischer K, Muhr G, Mueller EJ. [https://www.sciencedirect.com/science/article/pii/S0020138308002829 Epidemiology of traumatic spine fractures]. Injury. 2009 Feb 1;40(2):166-72.</ref> Minor trauma can also cause a thoracic spine fracture in individuals who have a condition associated with loss of bone mass such as [[osteoporosis]]. | |||
== Etiology == | |||
# Osteoporosis is the most common precipitating factor for vertebral fracture. However, trauma, cancer, chemotherapy, infection, long term steroid use, hyperthyroidism, and radiation therapy are also known to weaken bones that can lead to compression fractures. The etiology of lower bone density can be related to smoking, alcohol abuse, lower levels of estrogen, anorexia, kidney disease, medications, proton pump inhibitors, and other medications. Risk factors include female gender, osteoporosis, osteopenia, age greater than 50, history of vertebral fractures, smoking, vitamin D deficiency, and prolonged use of corticosteroids. | |||
# Trauma is the second most common cause of spine fracture, and motor vehicle accidents are the number one cause of spinal cord injury. <ref>Whitney E, Alastra AJ. [https://www.ncbi.nlm.nih.gov/books/NBK547673/ Vertebral Fracture.] Available from:https://www.ncbi.nlm.nih.gov/books/NBK547673/ (last accessed 18.4.2020)</ref> | |||
Fracture | |||
===Types of Fractures=== | |||
There are four major types of thoracic spine fractures (based on the mechanism of injury) and a 5th rare type | |||
# '''Compression (wedge fractures) -''' Caused by axial compression alone or flexion forces, when the spine is bent forward or in side flexion at the moment of trauma. It is a stable fracture and patients rarely accompanied neurological deficits<ref name="Kandabarow 1997">Kandabarow A. Injuries of the thoracolumbar spine. Advanced Emergency Nursing Journal. 1997 Sep 1;19(3):65-80. </ref>. The most common causes in younger patients are falls and motor vehicle accidents. In older patients the most common causes are minor incidents during normal activities of daily living secondary to [[Osteoporosis|osteoporosis]] or metabolic bone diseases.<ref name="O'Connor 2009">O'Connor E, Walsham J. [https://www.ncbi.nlm.nih.gov/pubmed/19422405 Indications for thoracolumbar imaging in blunt trauma patients: a review of current literature.] Emerg Med Australas 2009;21(2):94-101.</ref> <br> | |||
#'''Burst -''' Similar to compression fractures except that the entire vertebra is evenly crushed. It is a very severe fracture, accompanied with retro-pulsed bone fragments into spinal canal. Neurological injury and posterior column injury can occur more frequently. The common cause of this fracture is due to axial loading of the anterior spine such as from a fall, landing on the buttocks or lower extremities where the concentration of axial forces is to the thoracolumbar junction'''.'''<ref name="Tisot 2009">Tisot RA, Avanzi O. [https://www.ncbi.nlm.nih.gov/pubmed/20065359 Laminar fractures as a severity marker in burst fractures of the thoracolumbar spin]e. Journal of Orthopaedic Surgery. 2009 Dec;17(3):261-4.</ref><ref name="Alpantaki 2010" /><ref name="Kandabarow 1997" /> | |||
# '''Flexion-distraction (seat belt injury/ Chance fracture) -''' Involves the separation (distraction) of the fractured vertebra. It occurs by primary distraction forces on the spine. The axis of rotation is located within or in front of the anterior vertebral body. Failures of the posterior and middle columns of the spine under tension usually from a trauma involving sudden upper body forward flexion while the lower body remains stationary (seat belt injury). Often associated with abdominal trauma due to compression of the abdominal cavity during injury. The anterior column may be mildly affected, but the annulus fibrosis and anterior longitudinal ligament are intact: preventing dislocation or subluxation. A gap between the spinous processes is often present upon palpation.<ref name="Kandabarow 1997" /> | |||
# '''Fracture-dislocation -''' Found in combination with displacement of adjacent vertebrae. It is caused by various combinations of forces. It is very unstable and can cause a complete neurological deficit. Failure of all three spinal columns under compression, flexion, rotation, or shear forces. The most unstable of all thoracolumbar spine injuries, they are highly associated with neurological deficits. They can be caused by a severe flexion force similar to that of a seat belt injury, or an object falling across the back.<ref name="Kandabarow 1997" />'''<br>''' | |||
#'''Clay-Shoveler's Fracture -''' Rare, fatigue fracture of the upper thoracic spinous process. Seen in powerlifters or in people with physically intensive jobs causing shear forces on the vertebra, hyperflexed spine, or direct trauma.<ref name="Demir 2007" /> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Presentation of symptomatic fractures includes: <ref name="Lentle 2007">Lentle BC, Brown JP, Khan A, Leslie WD, Levesque J, Lyons DJ, Siminoski K, Tarulli G, Josse RG, Hodsman A. [https://www.ncbi.nlm.nih.gov/pubmed/17408160 Recognizing and reporting vertebral fractures: reducing the risk of future osteoporotic fractures]. Can Assoc Radiol J. 2007 Feb 15;58(1):27-36.</ref><ref name="O'Connor 2009" /><ref name="Marre 2011" /><ref name="Singh 2011">Singh R, Taylor DM, D’Souza D, Gorelik A, Page P, Phal P. [https://journals.sagepub.com/doi/pdf/10.1177/102490791101800102 Mechanism of injury and clinical variables in thoracic spine fracture: a case control study]. Hong Kong J Emerg Med. 2011;18(1):5-12.</ref><ref name="Holmes 2003">Holmes JF, Panacek EA, Miller PQ, Lapidis AD, Mower WR. [https://www.ncbi.nlm.nih.gov/pubmed/12554032 Prospective evaluation of criteria for obtaining thoracolumbar radiographs in trauma patients.] The Journal of emergency medicine. 2003 Jan 1;24(1):1-7.</ref><ref name="Friedrich 2006">Friedrich M, Gittler G, Pieler-Bruha E. [https://www.ncbi.nlm.nih.gov/pubmed/16463199 Misleading history of pain location in 51 patients with osteoporotic vertebral fractures.] European Spine Journal. 2006 Dec 1;15(12):1797-800.</ref> | |||
*Chronic back pain in thoracic and/or [[Lumbar|lumbar]] region | *Chronic back pain in [[Thoracic Vertebrae|thoracic]] and/or [[Lumbar|lumbar]] region | ||
*Slower gait | *Slower gait | ||
*Decreased range of | *Decreased thoracic and lumbar range of movement | ||
*Impaired pulmonary function | *Impaired pulmonary function | ||
*Increased kyphosis especially in osteoporotic patients with compression fractures | *Increased kyphosis - especially in osteoporotic patients with compression fractures | ||
*Neurological deficits due to narrowing of spinal canal - can | *Neurological deficits due to narrowing of spinal canal - can occur as long as 1.5 years post injury | ||
Prolonging of these symptoms leads to decreased physical function and performance of activities of daily living, and increased risk of disability. | |||
Vertebral deformities are also associated with significantly increased risk of future fractures, including hip fractures<ref name="Lentle 2007" />. | |||
Patients with non-compression fractures are usually involved in a multi-trauma, and will have various injuries and sources of pain. Clinicians must use their best judgment and employ clinical screening criteria to determine if the thoracic spine is involved.<ref name="O'Connor 2009" /> | Patients with non-compression fractures are usually involved in a multi-trauma, and will have various injuries and sources of pain. Clinicians must use their best judgment and employ clinical screening criteria to determine if the thoracic spine is involved.<ref name="O'Connor 2009" /> | ||
| Line 80: | Line 39: | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Plain radiographs are historically the "gold standard" for detecting thoracolumbar fractures, although due to the organs and soft tissue in the | Plain [[X-Rays|radiographs]] are historically the "gold standard" for detecting thoracolumbar fractures, although due to the organs and soft tissue in the thoracic region, fractures can be missed on radiographs. A [[CT Scans|CT scan]] is recommended to visualise thoracic fractures and an [[MRI Scans|MRI]] to assess soft tissue damage. <ref name="Diaz 2007">Diaz J, Cullinane D, Vaslef S, et al. Practice management guidelines for the screening of thoracolumbar spine fracture. J Trauma 2007;63(3):709-18.</ref><ref name="Marre 2011">Marré B, Ballesteros V, Martínez C, Zamorano JJ, Ilabaca F, Munjin M, Yurac R, Urzúa A, Lecaros M, Fleiderman J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3175903/ Thoracic spine fractures: injury profile and outcomes of a surgically treated cohort.] European Spine Journal. 2011 Sep 1;20(9):1427-33.</ref><ref name="Singh 2011" /><br> | ||
[[Multiple Myeloma|Multiple Myeloma]] and other cancers can present as thoracic pain, but will have additional signs such as unexplained weight loss and fever. | [[Multiple Myeloma|Multiple Myeloma]] and other cancers can present as thoracic pain, but will have additional [[Red Flags in Spinal Conditions|red flag]] signs such as unexplained weight loss and fever. | ||
[ | [[Scheuermann's Kyphosis|Scheuermann Disease]] presents as exaggerated [[Thoracic Hyperkyphosis]], anterior body extension and schmorl’s nodes; can be distinguished by vetebral body height parameters on radiograph. <ref name="Masharawi 2009">Masharawi Y, Rothschild B, Peled N, Hershkovitz I. [https://www.ncbi.nlm.nih.gov/pubmed/19680108 A simple radiological method for recognizing osteoporotic thoracic vertebral compression fractures and distinguishing them from Scheuermann disease]. Spine. 2009 Aug 15;34(18):1995-9.</ref> | ||
== Examination == | == Examination == | ||
'''Screening for Fracture''' | |||
= | Algorithms for screening patients with thoracic fractures and the need for imaging have been developed but are not fully validated.<ref name="O'Connor 2009" /> | ||
Presence of one or more of the following 5 criteria in a patient with blunt multi-trauma is an indication for thoracolumbar imaging (Sn=0.99): | |||
# High Risk Mechanism of Injury (MOI): | |||
#* Motor vehicle accident at speed >70 kph | |||
#* Fall from height >3 m | |||
#* Ejection from motor vehicle or motorcycle | |||
#* Any injury outside of these criteria that could cause a thoracolumbar fracture | |||
# Painful Distracting Injury: painful torso/long-bone injury sufficient to distract the patient from noticing the pain of the thoracolumbar injury | |||
# New Neurological Signs or Back Pain/Tenderness with Clinical Findings Suspicious of a New Fracture: | |||
#* Back pain | |||
#* Back tenderness on palpation | |||
#* Palpable step in vertebral palpation | |||
#* Midline bruising | |||
#* Neurological signs consistent with a spinal cord injury | |||
# Cognitive Impairment: | |||
#* Glasgow Coma Scale (GCS) < 15 | |||
#* Abnormal mental state | |||
#* Clinical intoxication | |||
# Known Cervical Spine Fracture: evidence of a new traumatic cervical spine fracture.<ref name="O'Connor 2009" /> | |||
'''Other criteria for screening include:''' | |||
# Screening criteria for radiograph of blunt trauma patients with thoracolumbar injuries<ref name="Holmes 2003" /> (Sn=1.00, Sp=0.039) | |||
#Complaints of thoracolumbar spine pain | |||
#* Thoracolumbar spine tenderness | |||
#* Decreased level of consciousness | |||
#* Intoxication with alcohol or drugs | |||
#* Neurologic deficit | |||
#* Painful distracting injury | |||
#Three predictive variables for thoracic spine fracture based on a case control study<ref name="Singh 2011" /> (Sp=0.93): | |||
#*Fall > 2m | |||
#*Thoracic pain | |||
#*Intoxication | |||
== | == Medical Management == | ||
===Operative=== | |||
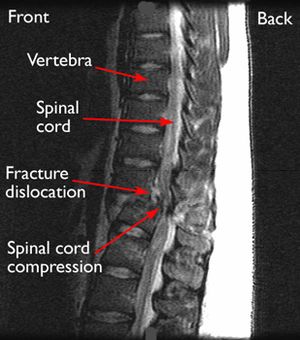
[[File:Spinal cord compression .jpg|right|frameless]] | |||
Benefits of surgical treatment of thoracolumbar fractures compared to conservative management | |||
* Avoiding an orthosis in the presence of multiple injuries and skin injuries | |||
* Immediate mobilization | |||
* Earlier rehabilitation | |||
* Better restoration of sagittal alignment<ref name="Shaffrey 1997" />. | |||
Negatives of surgical intervention | |||
* Risks of surgery including the risks of general anesthetic. | |||
* Conventional open surgical techniques may be accompanied by approach-related muscle injury, increased infection rates and higher blood loss. | |||
There is no difference between operative and non-operative treatment regarding neurological recovery and long-term functional outcomes.<ref name="Wood 2003" /> | |||
Indications for surgery | |||
* Neurological involvement and/or progressive neurological deterioration | |||
* >50% spinal canal compromise | |||
* >50% anterior vertebral body height loss, | |||
* >25° to 35° angle of kyphotic deformity | |||
* Posterior ligament complex (PLC) compromise. | |||
Surgical approaches can be anterior, posterior or a combination.<ref name="Alpantaki 2010">Alpantaki K, Bano A, Pasku D, Mavrogenis AF, Papagelopoulos PJ, Sapkas GS, Korres DS, Katonis P. [https://www.ncbi.nlm.nih.gov/pubmed/20806752 Thoracolumbar burst fractures: a systematic review of management.] Orthopedics. 2010 Jun 1;33(6):422-9.</ref> Recently, minimally invasive techniques have been described in thoracolumbar fractures. | |||
===Non-Operative=== | |||
Compression fractures, stable burst fractures and neurologically intact patients can typically be treated non-operatively:<ref name="Alpantaki 2010" /><ref name="Shaffrey 1997">Shen WJ, Liu TJ, Shen YS. [https://www.ncbi.nlm.nih.gov/pubmed/9314520 Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit]. Spine. 2001 May 1;26(9):1038-45.</ref><ref name="Wood 2003" /><ref name="Weninger 2009">Weninger P, Schultz A, Hertz H. [https://www.ncbi.nlm.nih.gov/pubmed/19009303 Conservative management of thoracolumbar and lumbar spine compression and burst fractures: functional and radiographic outcomes in 136 cases treated by closed reduction and casting.] Archives of orthopaedic and trauma surgery. 2009 Feb 1;129(2):207-19.</ref><ref name="Giele 2009">Giele BM, Wiertsema SH, Beelen A, van der Schaaf M, Lucas C, Been HD, Bramer JA. [https://www.ncbi.nlm.nih.gov/pubmed/19404808 No evidence for the effectiveness of bracing in patients with thoracolumbar fractures: a systematic review]. Acta orthopaedica. 2009 Jan 1;80(2):226-32.</ref>[[File:Fig. 4- Jewett & CASH Braces.JPG|Jewett (left) & CASH (right) braces - courtesy of Orthotic & Prosthetic Technologies, Inc., San Marcos, TX|right|frameless|180x180px]] | |||
*Bed rest/activity limitation ranging from days to weeks | |||
*Bracing: 8 to 12 weeks in Jewett or Cruciform Anterior Spinal Hyperextension (CASH) | |||
*Casting: 8 to 12 weeks | |||
*Pain medication | |||
*Physical therapy | |||
There is no consensus on the exact duration of treatment. | |||
Preventative treatment for fractures related to [[Osteoporosis|osteoporosis]] include bisophosphonates, calcium, vitamin D and exercise.<ref name="Demir 2007">Demir SÖ, Akn C, Aras M, Köseoglu F. [https://www.ncbi.nlm.nih.gov/pubmed/17314709 Spinal cord injury associated with thoracic osteoporotic fracture]. American journal of physical medicine & rehabilitation. 2007 Mar 1;86(3):242-6.</ref>[[File:Fig. 5- CASH & Jewett Braces on Patients.JPG|CASH (left) & Jewett (right) braces - courtesy of Orthotic & Prosthetic Technologies, Inc., San Marcos, TX|180x180px|right|frameless]]<br> | |||
===== | There was found to be no significant long-term difference in pain, disability and return to work for non-neurologically involved patients who received surgery compared to those who received bracing or casting.<ref name="Van Leeuwen 2000" /><ref name="Wood 2003">Wood KB, Buttermann GR, Phukan R, Harrod CC, Mehbod A, Shannon B, Bono CM, Harris MB. [https://pdfs.semanticscholar.org/bf63/6b050757d6cc05ed58f2e993cf634b0f8f42.pdf Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit: a prospective randomized study with follow-up at sixteen to twenty-two years]. JBJS. 2015 Jan 7;97(1):3-9.</ref> This indicates that the higher risk and cost of surgery may not be justified and that bracing/casting would be the preferred treatment in this patient population. Braces are a common component of both post-operative and non-operative thoracic fracture treatment protocols however there is no evidence to say that bracing is effective in the management of these fractures. .<ref name="Giele 2009" /> | ||
== Physical Therapy Management == | |||
* Management of vertebral fractures remains controversial <ref name="Alpantaki 2010" /> <sup>,</sup><ref name="Van Leeuwen 2000">van Leeuwen PJ, Bos RP, Derksen JC, de Vries J. [https://www.ncbi.nlm.nih.gov/pubmed/11028695 Assessment of spinal movement reduction by thoraco-lumbar-sacral orthoses.] Journal of rehabilitation research and development. 2000 Jul 1;37(4):395.</ref><sup>,</sup><ref name="Dai 2009">Dai LY, Jiang LS, Jiang SD. Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures. A five to seven-year prospective randomized study. J Bone Joint Surg Am 2009;91:1033-41.(LoE:2B)</ref> and research is limited on identifying physical therapy intervention. | |||
* Until recently, conservative management of fractures consisted of pain medications, rest and bracing to reduce spinal movements <ref name="Rousing 2010">Rousing R, Hansen KL, Andersen M, Jespersen SM, Thomsen K, Lauritsen JM. Twelve-months follow-up in forty-nine patients with acute/semiacute osteoporotic vertebral fractures treated conservatively or with percutaneous vertebroplasty. Spine 2010;35(5):478-82.(LoE:1B)</ref><sup>,</sup><ref name="Van Leeuwen 2000" /><sup>,</sup><ref name="Cahoj 2007">Cahoj PA, Cook JL, Robinson BS. Efficacy of percutaneous vertebral augmentation and use of physical therapy intervention following vertebral compression fractures in older adults: a systematic review. J Geriatr Phys Ther 2007;30(1):31-40. (LoE:3A)</ref><sup>,</sup><ref name="Wood 2003" />. | |||
* | * Rehabilitation programs must be designed specifically for the individual based on their physical abilities and impairments. | ||
* | * With conservative treatment, the majority of fractures heal with a significant decrease in pain in 8-12 weeks. Significant declines in pain (5.9cm on VAS) are experienced 12-24 hours post-surgery <ref name="Rousing 2010" />. | ||
* Interventions depend largely on whether the patient chose surgery or conservative treatment. | |||
* Interventions should always be prescribed and progressed based on patient tolerance. | |||
===Physical Therapy Exam=== | |||
*Thorough history including MOI and previous spine fractures | *Thorough history including MOI and previous spine fractures | ||
*Neurological screen | *Neurological screen | ||
| Line 142: | Line 132: | ||
*Identification of impairments in ROM, strength, flexibility | *Identification of impairments in ROM, strength, flexibility | ||
=== Physical Therapy Goals === | |||
=== Physical Therapy Goals | |||
*Reduce pain | *Reduce pain | ||
*Improve posture | *Improve posture | ||
| Line 189: | Line 141: | ||
*Lower extremity strengthening | *Lower extremity strengthening | ||
Bennell et al. found that a multimodal treatment approach over a 10-week period was successful in reducing pain and improving function in patients who suffered from osteoporotic vertebral fractures <ref name="Bennell 2010">Bennell KL, Matthews B, Greig A, Briggs A, Kelly A, Sherburn M, | Bennell et al. found that a multimodal treatment approach over a 10-week period was successful in reducing pain and improving function in patients who suffered from osteoporotic vertebral fractures <ref name="Bennell 2010">Bennell KL, Matthews B, Greig A, Briggs A, Kelly A, Sherburn M, Larsen J, Wark J. Effects of an exercise and manual therapy program on physical impairments, function and quality-of-life in people with osteoporotic vertebral fracture: a randomised, single-blind controlled pilot trial. BMC musculoskeletal disorders. 2010 Dec;11(1):36.</ref>. However, because it was a multimodal approach the effectiveness of each treatment is unclear.<br> | ||
===General Exercise Recommendations<ref name="Bennell 2010" /><sup>,</sup><ref name="Guide 2003">Guide to Physical Therapist Practice. 2nd ed. Revised. Alexandria, Va: American Physical Therapy Association; 2003.(LoE:5)</ref> === | |||
=== | * A major concern is re-fracture within a year of the initial injury. | ||
* Strengthening back-extensor muscles can help decrease the rate of refracture or prolong occurance of refracture <ref name="Cahoj 2007" /><sup>,</sup><ref name="Bennell 2010" /> | |||
* Improvement in reported pain levels and increased function in patients with back-extensor exercises.<ref name="Cahoj 2007" /><sup>,</sup><ref name="Huntoon 2008">Huntoon EA, Schmidt CK, Sinaki M. Significantly fewer refractures after vertebroplasty in patients who engage in back-extensor-strengthening exercises. Mayo Clin Proc 2008;83(1):54-7.(LoE:1B)</ref><sup>,</sup><ref name="Sinaki 2002">Sinaki M, Itoi E, Wahner HW, Wollan P, Gelzcer R, Mullan BP, et al. Stronger back muscles reduce the incidence of vertebral fractures: a prospective 10 year follow-up of postmenopausal women. Bone 2002;30(6):836-41.(LoE:2B)</ref><sup>,</sup><ref name="Bennell 2010" />. | |||
* Should begin strengthening back-extensor muscles as soon as they are physically able. | |||
* When developing a plan of care, the therapist should consider the individual characteristics of a vertebral fracture and possible secondary limitations. | |||
'''An example of a Physiotherapy and Home Exercise Program''' Adapted from: Bennell et al (2010). <ref name="Bennell 2010" /> Within a pain-free range, progressed as tolerated: | |||
{| class="wikitable" | |||
!Technique/Exercise | |||
!Dosage | |||
!Duration (weeks) | |||
A major concern is | !Image | ||
When developing a plan of care, the therapist should consider the individual characteristics of a vertebral fracture and possible secondary limitations. | |||
Adapted from: Bennell et al (2010). <ref name="Bennell 2010" /> | |||
Within a pain-free range, progressed as tolerated: | |||
{| | |||
|- | |- | ||
|'''Postural Taping - performed by physiotherapist''' | |||
Start from anterior aspect of each shoulder and go posteriorly + obliquely towards the opposite rib cage | |||
|worn full time | |||
|1 | |||
| | |||
|- | |- | ||
| | |'''Soft Tissue Massage - performed by physiotherapist''' | ||
''' | Stroking, circular frictions, petrissage to the erector spinae, rhomboids, and upper traps with patient prone | ||
|5 minutes | |||
|1 - 10 | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |'''Passive Accessory Postero-anterior Vertebral Mobilisation - performed by physiotherapist''' | ||
''' | Grade 2-3 mobilisations from T1 down to 2 levels below the most painful vertebral region with patient prone | ||
|5 mobilisations at each central level x 2 reps | |||
|1 - 10 | |||
| | |||
| 5 | |||
| 1-10 | |||
|- | |- | ||
| | |'''Supine Lying Over Rolled Up Towel''' | ||
''' | Towel is placed lengthwise along the back to facilitate thoracic extension | ||
|5 - 10 minutes | |||
|1 (daily) | |||
| | |||
| 5 | |||
| 1 | |||
|- | |- | ||
| | |'''Erect Sitting with Transversus Abdominus (TA) Stabilisation''' | ||
''' | Forward sitting on chair (no back rest) with chin retraction, scapular retraction, and TA contraction | ||
|10 second hold x 5 reps | |||
|1 - 10 (daily) | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |'''Elbows Back in Sitting''' | ||
''' | Hands placed behind the head with elbows pointing out to the side - press elbows back using scapular retraction | ||
|5 second hold x 5 reps | |||
|1 - 10 (daily) | |||
| | |||
| | |||
| 1-10 daily | |||
|- | |- | ||
| | |'''Trunk Mobility in Sitting''' | ||
''' | With hands on shoulders gently rotate to both directions and laterally flex to each side | ||
|5 reps in each direction | |||
|1 - 10 | |||
(daily) | |||
| [[ | |[[File:Chair Ext.JPG|thumb|213x213px|Trunk mobility in sitting - extension|none]] | ||
|- | |- | ||
| | |'''Head to wall in standing''' | ||
''' | Stand with back and heels against the wall and a rolled up towel behind the head - retract chin | ||
|10 second hold x 5 reps | |||
|1 -1 0 | |||
(daily) | |||
| 5 reps | | | ||
| 1- | |||
|- | |- | ||
| | |'''Standing corner stretch''' | ||
''' | Stand facing a corner and place both hands chest height on each side of the wall - move in closer to stretch anterior chest | ||
|10 - 30 second hold x 3 reps | |||
|2 - 10 | |||
(daily) | |||
| | |||
| | |||
|- | |- | ||
| | |'''Walking hands up wall in standing''' | ||
''' | Stand facing the wall and walk hands up until arms are up-stretched - then hold hands off wall | ||
|5 second hold x 5 reps | |||
|3 - 10 (daily) | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |'''Shoulder flexion in supine''' | ||
''' | Arms are outstretched holding onto a cane/towel - then take arms over head and hold at end range | ||
|10 second hold x 5 reps | |||
|3 - 10 (daily) | |||
| | |||
| 5 | |||
| 3-10 daily | |||
|- | |- | ||
| | |'''Standing wall push ups''' | ||
''' | Stand facing the wall with arms in front at shoulder height - keeping the body straight bend and straighten elbows | ||
|8 - 10 reps x 2 sets | |||
|1 - 10 | |||
(3x/week) | |||
| 10 | |[[File:Wall Pushups.JPG|thumb|213x213px|Standing wall pushups|none]] | ||
| | |||
|- | |- | ||
| | |'''Seated row with dumbbells''' | ||
''' | Sitting upright - pull hands up towards chest by bending elbows and then lower | ||
|8 - 10 reps x 2 sets | |||
|1 - 10 (3x/week) | |||
| | |||
| 8-10 reps | |||
| 1-10 3x/week | |||
|- | |- | ||
| | |'''Seated overhead dumbbell press''' | ||
'''Seated | Elbows are bent and out to the side - press dumbbells straight up until arms are extended overhead | ||
|8 - 10 reps x 2 sets | |||
|3 - 10 (3x/week) | |||
| | |||
| 8-10 reps | |||
| | |||
|- | |- | ||
| | |'''Bridging in supine''' | ||
''' | Knees bent and feet flat on ground - push through feet to lift back and pelvis off ground | ||
|5 - 10 second hold x 5 reps | |||
| |1 - 2 (3x/week) | ||
|[[File:Bridge.JPG|thumb|160x160px|Bridge in supine|none]] | |||
| | |||
| | |||
|- | |- | ||
| | |'''Hip extension in prone''' | ||
''' | Raise one leg off the ground and then the other | ||
|8 - 10 reps x 2 sets | |||
|3 - 10 (3x/week) | |||
|[[File:SLR Hip Ext.JPG|thumb|163x163px|Hip extension in prone|none]] | |||
| [[ | |||
|- | |- | ||
| | |'''Half squats - progress to holding dumbbells''' | ||
''' | Stand in front of chair and squat down to touch chair with buttocks - then stand up | ||
|8 - 10 reps x 2 sets | |||
- | |1 - 2 (3x/week) | ||
| | |||
| 8-10 reps | |||
| | |||
|- | |- | ||
| | |'''Step ups - progress to holding dumbbells''' | ||
''' | Step up and down a 10 cm step - alternate legs | ||
|8 - 10 reps x 2 sets | |||
|3 - 10 | |||
(3x/week) | |||
| 8-10 reps | | | ||
| | |||
|- | |- | ||
| | |'''Scapular retraction with theraband in sitting''' | ||
''' | Hold theraband in both hands with elbows tucked into sides - then perform wrist extension, forearm supination, shoulder external rotation, and scapular retraction | ||
|8 - 10 reps x 2 sets | |||
- | |1 - 10 (3x/week) | ||
|[[File:Scapula Retraction with TheraBand.JPG|thumb|213x213px|Scapular retraction with theraband in sitting + chin tuck + TA hold|none]] | |||
| 8-10 reps | |||
| | |||
3x/week | |||
|- | |- | ||
| | |'''Four-point kneeling with transversus abdominus''' | ||
''' | Push into floor with hands, knees and feet - then draw navel up and in | ||
|5 second hold x 8-10 reps <br>x 2 sets | |||
|2 | |||
(3x/week) | |||
| | |||
| 8-10 reps <br> | |||
| | |||
|- | |- | ||
| | |'''Four point kneeling with one arm and leg lift''' | ||
'''Four | Perform as above - then lift one arm off ground and progress to lifting and extending the leg on the opposite side off ground at same time | ||
|8 - 10 reps x 2 sets | |||
|3 - 10 (3x/week) | |||
|[[File:Quadruped Ext.JPG|thumb|157x157px|4 point kneeling + TA hold|none]] | |||
| 8-10 reps | |||
| | |||
3x/week | |||
|- | |- | ||
| | |'''Prone lying with arm elevation''' | ||
''' | With arms at shoulder height and bent at elbows - perform scapular retraction and then lift arms off floor | ||
|5 - 10 second hold x 5 reps | |||
|2 - 3 (3x/week) | |||
| | |||
| | |||
| 3 | |||
|- | |- | ||
| | |'''Prone trunk extension''' | ||
Lift head and shoulders off floor while maintaining chin retraction | |||
|5 - 10 second hold x 5 reps | |||
|4 - 10 (3x/week) | |||
| | |||
'''Prone trunk extension''' | |||
| 5-10 | |||
| 4-10 3x/week | |||
| | |||
|} | |} | ||
'''Complications to Consider''' <ref name="Alpantaki 2010" /><sup>,</sup><ref name="Dai 2009" /><sup>,</sup><ref name="Cahoj 2007" /> | |||
*Cardiorespiratory compromise | *Cardiorespiratory compromise | ||
*Additional Fractures | *Additional Fractures | ||
| Line 434: | Line 314: | ||
*Gait/Ambulation Abnormalities | *Gait/Ambulation Abnormalities | ||
*Loss of Balance | *Loss of Balance | ||
== Clinical Bottom Line == | |||
* There is a lack of high-quality evidence for the management of thoracic spine fractures. | |||
* Physical therapists should be familiar with screening for thoracic fractures and take an impairment-based approach when treating post-operative or non-operative patients. | |||
== Resources == | == Resources == | ||
# | #[https://neckandback.com/conditions/thoraco-lumbar-spine-fractures/ Thoraco-lumbar spine fractures]. Corenman DS | ||
# | #[https://www.mdguidelines.com/mda/fracture-thoracic-spine-without-spinal-cord-injury Fracture, thoracic spine (without spinal cord injury)]. MD Guidelines. | ||
#[https://emedicine.medscape.com/article/1267029-overview Thoracic spine fractures and dislocation]. Medscape Reference. | |||
# | |||
== References == | == References == | ||
| Line 464: | Line 337: | ||
[[Category:Primary Contact]] | [[Category:Primary Contact]] | ||
[[Category:Acute Care]] | [[Category:Acute Care]] | ||
[[Category:Conditions]] | |||
[[Category:Thoracic Spine - Conditions]] | |||
Latest revision as of 20:48, 17 October 2020
Original Editors - Tre Hinojosa, Heather Hughes, Erin Locati, and Melissa Osti as part of the Texas State University Evidence-based Practice Project
Top Contributors - Erin Locati, Melissa Osti, Lucy Aird, Heather Hughes, Jin Yoo, Kim Jackson, Abbey Wright, Tre Hinojosa, Admin, Hannah Willocx, Joshua Samuel, WikiSysop, Lucinda hampton, Liesbeth Vanden Brande, Evan Thomas, Nick Van Doorsselaer, Karen Wilson, 127.0.0.1, Claire Knott, Eric Robertson and Jeremy Brady
Definition/Description[edit | edit source]
Most thoracic spine fractures occur in the lower thoracic spine, with 60% to 70% of thoraco-lumbar fractures occurring in the T11 to L2 region, which is bio-mechanically weak for stress. The majority of these fractures occur without spinal cord injury. 20 to 40% of the fractures are associated with neurological injuries.
Major (high-energy) trauma, is the most common cause of thoracic fractures such as falls from height or road traffic accidents.[1] Minor trauma can also cause a thoracic spine fracture in individuals who have a condition associated with loss of bone mass such as osteoporosis.
Etiology[edit | edit source]
- Osteoporosis is the most common precipitating factor for vertebral fracture. However, trauma, cancer, chemotherapy, infection, long term steroid use, hyperthyroidism, and radiation therapy are also known to weaken bones that can lead to compression fractures. The etiology of lower bone density can be related to smoking, alcohol abuse, lower levels of estrogen, anorexia, kidney disease, medications, proton pump inhibitors, and other medications. Risk factors include female gender, osteoporosis, osteopenia, age greater than 50, history of vertebral fractures, smoking, vitamin D deficiency, and prolonged use of corticosteroids.
- Trauma is the second most common cause of spine fracture, and motor vehicle accidents are the number one cause of spinal cord injury. [2]
Types of Fractures[edit | edit source]
There are four major types of thoracic spine fractures (based on the mechanism of injury) and a 5th rare type
- Compression (wedge fractures) - Caused by axial compression alone or flexion forces, when the spine is bent forward or in side flexion at the moment of trauma. It is a stable fracture and patients rarely accompanied neurological deficits[3]. The most common causes in younger patients are falls and motor vehicle accidents. In older patients the most common causes are minor incidents during normal activities of daily living secondary to osteoporosis or metabolic bone diseases.[4]
- Burst - Similar to compression fractures except that the entire vertebra is evenly crushed. It is a very severe fracture, accompanied with retro-pulsed bone fragments into spinal canal. Neurological injury and posterior column injury can occur more frequently. The common cause of this fracture is due to axial loading of the anterior spine such as from a fall, landing on the buttocks or lower extremities where the concentration of axial forces is to the thoracolumbar junction.[5][6][3]
- Flexion-distraction (seat belt injury/ Chance fracture) - Involves the separation (distraction) of the fractured vertebra. It occurs by primary distraction forces on the spine. The axis of rotation is located within or in front of the anterior vertebral body. Failures of the posterior and middle columns of the spine under tension usually from a trauma involving sudden upper body forward flexion while the lower body remains stationary (seat belt injury). Often associated with abdominal trauma due to compression of the abdominal cavity during injury. The anterior column may be mildly affected, but the annulus fibrosis and anterior longitudinal ligament are intact: preventing dislocation or subluxation. A gap between the spinous processes is often present upon palpation.[3]
- Fracture-dislocation - Found in combination with displacement of adjacent vertebrae. It is caused by various combinations of forces. It is very unstable and can cause a complete neurological deficit. Failure of all three spinal columns under compression, flexion, rotation, or shear forces. The most unstable of all thoracolumbar spine injuries, they are highly associated with neurological deficits. They can be caused by a severe flexion force similar to that of a seat belt injury, or an object falling across the back.[3]
- Clay-Shoveler's Fracture - Rare, fatigue fracture of the upper thoracic spinous process. Seen in powerlifters or in people with physically intensive jobs causing shear forces on the vertebra, hyperflexed spine, or direct trauma.[7]
Characteristics/Clinical Presentation[edit | edit source]
Presentation of symptomatic fractures includes: [8][4][9][10][11][12]
- Chronic back pain in thoracic and/or lumbar region
- Slower gait
- Decreased thoracic and lumbar range of movement
- Impaired pulmonary function
- Increased kyphosis - especially in osteoporotic patients with compression fractures
- Neurological deficits due to narrowing of spinal canal - can occur as long as 1.5 years post injury
Prolonging of these symptoms leads to decreased physical function and performance of activities of daily living, and increased risk of disability.
Vertebral deformities are also associated with significantly increased risk of future fractures, including hip fractures[8].
Patients with non-compression fractures are usually involved in a multi-trauma, and will have various injuries and sources of pain. Clinicians must use their best judgment and employ clinical screening criteria to determine if the thoracic spine is involved.[4]
Differential Diagnosis[edit | edit source]
Plain radiographs are historically the "gold standard" for detecting thoracolumbar fractures, although due to the organs and soft tissue in the thoracic region, fractures can be missed on radiographs. A CT scan is recommended to visualise thoracic fractures and an MRI to assess soft tissue damage. [13][9][10]
Multiple Myeloma and other cancers can present as thoracic pain, but will have additional red flag signs such as unexplained weight loss and fever.
Scheuermann Disease presents as exaggerated Thoracic Hyperkyphosis, anterior body extension and schmorl’s nodes; can be distinguished by vetebral body height parameters on radiograph. [14]
Examination[edit | edit source]
Screening for Fracture
Algorithms for screening patients with thoracic fractures and the need for imaging have been developed but are not fully validated.[4]
Presence of one or more of the following 5 criteria in a patient with blunt multi-trauma is an indication for thoracolumbar imaging (Sn=0.99):
- High Risk Mechanism of Injury (MOI):
- Motor vehicle accident at speed >70 kph
- Fall from height >3 m
- Ejection from motor vehicle or motorcycle
- Any injury outside of these criteria that could cause a thoracolumbar fracture
- Painful Distracting Injury: painful torso/long-bone injury sufficient to distract the patient from noticing the pain of the thoracolumbar injury
- New Neurological Signs or Back Pain/Tenderness with Clinical Findings Suspicious of a New Fracture:
- Back pain
- Back tenderness on palpation
- Palpable step in vertebral palpation
- Midline bruising
- Neurological signs consistent with a spinal cord injury
- Cognitive Impairment:
- Glasgow Coma Scale (GCS) < 15
- Abnormal mental state
- Clinical intoxication
- Known Cervical Spine Fracture: evidence of a new traumatic cervical spine fracture.[4]
Other criteria for screening include:
- Screening criteria for radiograph of blunt trauma patients with thoracolumbar injuries[11] (Sn=1.00, Sp=0.039)
- Complaints of thoracolumbar spine pain
- Thoracolumbar spine tenderness
- Decreased level of consciousness
- Intoxication with alcohol or drugs
- Neurologic deficit
- Painful distracting injury
- Three predictive variables for thoracic spine fracture based on a case control study[10] (Sp=0.93):
- Fall > 2m
- Thoracic pain
- Intoxication
Medical Management[edit | edit source]
Operative[edit | edit source]
Benefits of surgical treatment of thoracolumbar fractures compared to conservative management
- Avoiding an orthosis in the presence of multiple injuries and skin injuries
- Immediate mobilization
- Earlier rehabilitation
- Better restoration of sagittal alignment[15].
Negatives of surgical intervention
- Risks of surgery including the risks of general anesthetic.
- Conventional open surgical techniques may be accompanied by approach-related muscle injury, increased infection rates and higher blood loss.
There is no difference between operative and non-operative treatment regarding neurological recovery and long-term functional outcomes.[16]
Indications for surgery
- Neurological involvement and/or progressive neurological deterioration
- >50% spinal canal compromise
- >50% anterior vertebral body height loss,
- >25° to 35° angle of kyphotic deformity
- Posterior ligament complex (PLC) compromise.
Surgical approaches can be anterior, posterior or a combination.[6] Recently, minimally invasive techniques have been described in thoracolumbar fractures.
Non-Operative[edit | edit source]
Compression fractures, stable burst fractures and neurologically intact patients can typically be treated non-operatively:[6][15][16][17][18]
- Bed rest/activity limitation ranging from days to weeks
- Bracing: 8 to 12 weeks in Jewett or Cruciform Anterior Spinal Hyperextension (CASH)
- Casting: 8 to 12 weeks
- Pain medication
- Physical therapy
There is no consensus on the exact duration of treatment.
Preventative treatment for fractures related to osteoporosis include bisophosphonates, calcium, vitamin D and exercise.[7]
There was found to be no significant long-term difference in pain, disability and return to work for non-neurologically involved patients who received surgery compared to those who received bracing or casting.[19][16] This indicates that the higher risk and cost of surgery may not be justified and that bracing/casting would be the preferred treatment in this patient population. Braces are a common component of both post-operative and non-operative thoracic fracture treatment protocols however there is no evidence to say that bracing is effective in the management of these fractures. .[18]
Physical Therapy Management[edit | edit source]
- Management of vertebral fractures remains controversial [6] ,[19],[20] and research is limited on identifying physical therapy intervention.
- Until recently, conservative management of fractures consisted of pain medications, rest and bracing to reduce spinal movements [21],[19],[22],[16].
- Rehabilitation programs must be designed specifically for the individual based on their physical abilities and impairments.
- With conservative treatment, the majority of fractures heal with a significant decrease in pain in 8-12 weeks. Significant declines in pain (5.9cm on VAS) are experienced 12-24 hours post-surgery [21].
- Interventions depend largely on whether the patient chose surgery or conservative treatment.
- Interventions should always be prescribed and progressed based on patient tolerance.
Physical Therapy Exam[edit | edit source]
- Thorough history including MOI and previous spine fractures
- Neurological screen
- Assessment of patient's pain level and location
- Palpation of the thoracic spine
- Screen for thoracic fracture
- Identification of impairments in ROM, strength, flexibility
Physical Therapy Goals[edit | edit source]
- Reduce pain
- Improve posture
- Improve thoracic mobility
- Strengthen trunk extensors
- Improve trunk control
- Provide education
- Lower extremity strengthening
Bennell et al. found that a multimodal treatment approach over a 10-week period was successful in reducing pain and improving function in patients who suffered from osteoporotic vertebral fractures [23]. However, because it was a multimodal approach the effectiveness of each treatment is unclear.
General Exercise Recommendations[23],[24] [edit | edit source]
- A major concern is re-fracture within a year of the initial injury.
- Strengthening back-extensor muscles can help decrease the rate of refracture or prolong occurance of refracture [22],[23]
- Improvement in reported pain levels and increased function in patients with back-extensor exercises.[22],[25],[26],[23].
- Should begin strengthening back-extensor muscles as soon as they are physically able.
- When developing a plan of care, the therapist should consider the individual characteristics of a vertebral fracture and possible secondary limitations.
An example of a Physiotherapy and Home Exercise Program Adapted from: Bennell et al (2010). [23] Within a pain-free range, progressed as tolerated:
| Technique/Exercise | Dosage | Duration (weeks) | Image |
|---|---|---|---|
| Postural Taping - performed by physiotherapist
Start from anterior aspect of each shoulder and go posteriorly + obliquely towards the opposite rib cage |
worn full time | 1 | |
| Soft Tissue Massage - performed by physiotherapist
Stroking, circular frictions, petrissage to the erector spinae, rhomboids, and upper traps with patient prone |
5 minutes | 1 - 10 | |
| Passive Accessory Postero-anterior Vertebral Mobilisation - performed by physiotherapist
Grade 2-3 mobilisations from T1 down to 2 levels below the most painful vertebral region with patient prone |
5 mobilisations at each central level x 2 reps | 1 - 10 | |
| Supine Lying Over Rolled Up Towel
Towel is placed lengthwise along the back to facilitate thoracic extension |
5 - 10 minutes | 1 (daily) | |
| Erect Sitting with Transversus Abdominus (TA) Stabilisation
Forward sitting on chair (no back rest) with chin retraction, scapular retraction, and TA contraction |
10 second hold x 5 reps | 1 - 10 (daily) | |
| Elbows Back in Sitting
Hands placed behind the head with elbows pointing out to the side - press elbows back using scapular retraction |
5 second hold x 5 reps | 1 - 10 (daily) | |
| Trunk Mobility in Sitting
With hands on shoulders gently rotate to both directions and laterally flex to each side |
5 reps in each direction | 1 - 10
(daily) |
|
| Head to wall in standing
Stand with back and heels against the wall and a rolled up towel behind the head - retract chin |
10 second hold x 5 reps | 1 -1 0
(daily) |
|
| Standing corner stretch
Stand facing a corner and place both hands chest height on each side of the wall - move in closer to stretch anterior chest |
10 - 30 second hold x 3 reps | 2 - 10
(daily) |
|
| Walking hands up wall in standing
Stand facing the wall and walk hands up until arms are up-stretched - then hold hands off wall |
5 second hold x 5 reps | 3 - 10 (daily) | |
| Shoulder flexion in supine
Arms are outstretched holding onto a cane/towel - then take arms over head and hold at end range |
10 second hold x 5 reps | 3 - 10 (daily) | |
| Standing wall push ups
Stand facing the wall with arms in front at shoulder height - keeping the body straight bend and straighten elbows |
8 - 10 reps x 2 sets | 1 - 10
(3x/week) |
|
| Seated row with dumbbells
Sitting upright - pull hands up towards chest by bending elbows and then lower |
8 - 10 reps x 2 sets | 1 - 10 (3x/week) | |
| Seated overhead dumbbell press
Elbows are bent and out to the side - press dumbbells straight up until arms are extended overhead |
8 - 10 reps x 2 sets | 3 - 10 (3x/week) | |
| Bridging in supine
Knees bent and feet flat on ground - push through feet to lift back and pelvis off ground |
5 - 10 second hold x 5 reps | 1 - 2 (3x/week) | |
| Hip extension in prone
Raise one leg off the ground and then the other |
8 - 10 reps x 2 sets | 3 - 10 (3x/week) | |
| Half squats - progress to holding dumbbells
Stand in front of chair and squat down to touch chair with buttocks - then stand up |
8 - 10 reps x 2 sets | 1 - 2 (3x/week) | |
| Step ups - progress to holding dumbbells
Step up and down a 10 cm step - alternate legs |
8 - 10 reps x 2 sets | 3 - 10
(3x/week) |
|
| Scapular retraction with theraband in sitting
Hold theraband in both hands with elbows tucked into sides - then perform wrist extension, forearm supination, shoulder external rotation, and scapular retraction |
8 - 10 reps x 2 sets | 1 - 10 (3x/week) | |
| Four-point kneeling with transversus abdominus
Push into floor with hands, knees and feet - then draw navel up and in |
5 second hold x 8-10 reps x 2 sets |
2
(3x/week) |
|
| Four point kneeling with one arm and leg lift
Perform as above - then lift one arm off ground and progress to lifting and extending the leg on the opposite side off ground at same time |
8 - 10 reps x 2 sets | 3 - 10 (3x/week) | |
| Prone lying with arm elevation
With arms at shoulder height and bent at elbows - perform scapular retraction and then lift arms off floor |
5 - 10 second hold x 5 reps | 2 - 3 (3x/week) | |
| Prone trunk extension
Lift head and shoulders off floor while maintaining chin retraction |
5 - 10 second hold x 5 reps | 4 - 10 (3x/week) |
Complications to Consider [6],[20],[22]
- Cardiorespiratory compromise
- Additional Fractures
- Refractures
- Osteoporosis
- Prolonged Pain
- Limited Range of Motion
- Limited Strength
- Neurological Compromise
- Postural Dysfunction
- General Deconditioning
- Gait/Ambulation Abnormalities
- Loss of Balance
Clinical Bottom Line[edit | edit source]
- There is a lack of high-quality evidence for the management of thoracic spine fractures.
- Physical therapists should be familiar with screening for thoracic fractures and take an impairment-based approach when treating post-operative or non-operative patients.
Resources[edit | edit source]
- Thoraco-lumbar spine fractures. Corenman DS
- Fracture, thoracic spine (without spinal cord injury). MD Guidelines.
- Thoracic spine fractures and dislocation. Medscape Reference.
References[edit | edit source]
- ↑ Leucht P, Fischer K, Muhr G, Mueller EJ. Epidemiology of traumatic spine fractures. Injury. 2009 Feb 1;40(2):166-72.
- ↑ Whitney E, Alastra AJ. Vertebral Fracture. Available from:https://www.ncbi.nlm.nih.gov/books/NBK547673/ (last accessed 18.4.2020)
- ↑ 3.0 3.1 3.2 3.3 Kandabarow A. Injuries of the thoracolumbar spine. Advanced Emergency Nursing Journal. 1997 Sep 1;19(3):65-80.
- ↑ 4.0 4.1 4.2 4.3 4.4 O'Connor E, Walsham J. Indications for thoracolumbar imaging in blunt trauma patients: a review of current literature. Emerg Med Australas 2009;21(2):94-101.
- ↑ Tisot RA, Avanzi O. Laminar fractures as a severity marker in burst fractures of the thoracolumbar spine. Journal of Orthopaedic Surgery. 2009 Dec;17(3):261-4.
- ↑ 6.0 6.1 6.2 6.3 6.4 Alpantaki K, Bano A, Pasku D, Mavrogenis AF, Papagelopoulos PJ, Sapkas GS, Korres DS, Katonis P. Thoracolumbar burst fractures: a systematic review of management. Orthopedics. 2010 Jun 1;33(6):422-9.
- ↑ 7.0 7.1 Demir SÖ, Akn C, Aras M, Köseoglu F. Spinal cord injury associated with thoracic osteoporotic fracture. American journal of physical medicine & rehabilitation. 2007 Mar 1;86(3):242-6.
- ↑ 8.0 8.1 Lentle BC, Brown JP, Khan A, Leslie WD, Levesque J, Lyons DJ, Siminoski K, Tarulli G, Josse RG, Hodsman A. Recognizing and reporting vertebral fractures: reducing the risk of future osteoporotic fractures. Can Assoc Radiol J. 2007 Feb 15;58(1):27-36.
- ↑ 9.0 9.1 Marré B, Ballesteros V, Martínez C, Zamorano JJ, Ilabaca F, Munjin M, Yurac R, Urzúa A, Lecaros M, Fleiderman J. Thoracic spine fractures: injury profile and outcomes of a surgically treated cohort. European Spine Journal. 2011 Sep 1;20(9):1427-33.
- ↑ 10.0 10.1 10.2 Singh R, Taylor DM, D’Souza D, Gorelik A, Page P, Phal P. Mechanism of injury and clinical variables in thoracic spine fracture: a case control study. Hong Kong J Emerg Med. 2011;18(1):5-12.
- ↑ 11.0 11.1 Holmes JF, Panacek EA, Miller PQ, Lapidis AD, Mower WR. Prospective evaluation of criteria for obtaining thoracolumbar radiographs in trauma patients. The Journal of emergency medicine. 2003 Jan 1;24(1):1-7.
- ↑ Friedrich M, Gittler G, Pieler-Bruha E. Misleading history of pain location in 51 patients with osteoporotic vertebral fractures. European Spine Journal. 2006 Dec 1;15(12):1797-800.
- ↑ Diaz J, Cullinane D, Vaslef S, et al. Practice management guidelines for the screening of thoracolumbar spine fracture. J Trauma 2007;63(3):709-18.
- ↑ Masharawi Y, Rothschild B, Peled N, Hershkovitz I. A simple radiological method for recognizing osteoporotic thoracic vertebral compression fractures and distinguishing them from Scheuermann disease. Spine. 2009 Aug 15;34(18):1995-9.
- ↑ 15.0 15.1 Shen WJ, Liu TJ, Shen YS. Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine. 2001 May 1;26(9):1038-45.
- ↑ 16.0 16.1 16.2 16.3 Wood KB, Buttermann GR, Phukan R, Harrod CC, Mehbod A, Shannon B, Bono CM, Harris MB. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit: a prospective randomized study with follow-up at sixteen to twenty-two years. JBJS. 2015 Jan 7;97(1):3-9.
- ↑ Weninger P, Schultz A, Hertz H. Conservative management of thoracolumbar and lumbar spine compression and burst fractures: functional and radiographic outcomes in 136 cases treated by closed reduction and casting. Archives of orthopaedic and trauma surgery. 2009 Feb 1;129(2):207-19.
- ↑ 18.0 18.1 Giele BM, Wiertsema SH, Beelen A, van der Schaaf M, Lucas C, Been HD, Bramer JA. No evidence for the effectiveness of bracing in patients with thoracolumbar fractures: a systematic review. Acta orthopaedica. 2009 Jan 1;80(2):226-32.
- ↑ 19.0 19.1 19.2 van Leeuwen PJ, Bos RP, Derksen JC, de Vries J. Assessment of spinal movement reduction by thoraco-lumbar-sacral orthoses. Journal of rehabilitation research and development. 2000 Jul 1;37(4):395.
- ↑ 20.0 20.1 Dai LY, Jiang LS, Jiang SD. Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures. A five to seven-year prospective randomized study. J Bone Joint Surg Am 2009;91:1033-41.(LoE:2B)
- ↑ 21.0 21.1 Rousing R, Hansen KL, Andersen M, Jespersen SM, Thomsen K, Lauritsen JM. Twelve-months follow-up in forty-nine patients with acute/semiacute osteoporotic vertebral fractures treated conservatively or with percutaneous vertebroplasty. Spine 2010;35(5):478-82.(LoE:1B)
- ↑ 22.0 22.1 22.2 22.3 Cahoj PA, Cook JL, Robinson BS. Efficacy of percutaneous vertebral augmentation and use of physical therapy intervention following vertebral compression fractures in older adults: a systematic review. J Geriatr Phys Ther 2007;30(1):31-40. (LoE:3A)
- ↑ 23.0 23.1 23.2 23.3 23.4 Bennell KL, Matthews B, Greig A, Briggs A, Kelly A, Sherburn M, Larsen J, Wark J. Effects of an exercise and manual therapy program on physical impairments, function and quality-of-life in people with osteoporotic vertebral fracture: a randomised, single-blind controlled pilot trial. BMC musculoskeletal disorders. 2010 Dec;11(1):36.
- ↑ Guide to Physical Therapist Practice. 2nd ed. Revised. Alexandria, Va: American Physical Therapy Association; 2003.(LoE:5)
- ↑ Huntoon EA, Schmidt CK, Sinaki M. Significantly fewer refractures after vertebroplasty in patients who engage in back-extensor-strengthening exercises. Mayo Clin Proc 2008;83(1):54-7.(LoE:1B)
- ↑ Sinaki M, Itoi E, Wahner HW, Wollan P, Gelzcer R, Mullan BP, et al. Stronger back muscles reduce the incidence of vertebral fractures: a prospective 10 year follow-up of postmenopausal women. Bone 2002;30(6):836-41.(LoE:2B)