|
|
| (32 intermediate revisions by 8 users not shown) |
| Line 1: |
Line 1: |
| <div class="editorbox">'''Original Editors '''- [[User:Amanda Mattingly|Amanda Mattingly]] from [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project]]. | | <div class="editorbox">'''Original Editors '''- [[User:Amanda Mattingly|Amanda Mattingly]] from [[Pathophysiology of Complex Patient Problems|Bellarmine University's Pathophysiology of Complex Patient Problems project]]. '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} </div> |
| '''Lead Editors''' - Your name will be added here if you are a lead editor on this page. [[Physiopedia:Editors|Read more.]] </div> | |
| | |
| == Definition/Description == | | == Definition/Description == |
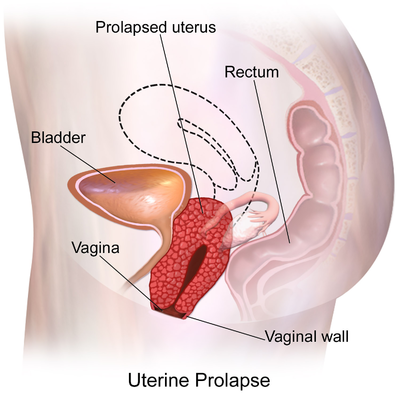
| | [[File:Uterine Prolapse diagram.png|right|frameless|400x400px]] |
| | Uterine prolapse is the herniation of the uterus from its natural anatomical location into the vaginal canal, through the hymen, or through the introitus of the vagina. This is due to the weakening of its surrounding support structures. Uterine prolapse is one of the multiple conditions that are classified under the broader term of [[Pelvic Organ Prolapse|pelvic organ prolapse]]. |
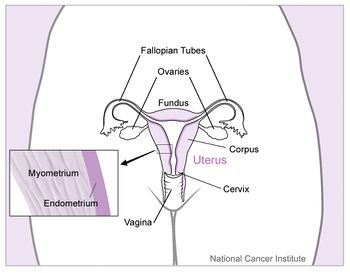
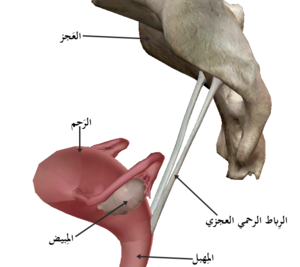
| | * In its usual state, the uterus rests in the apical compartment of pelvic organs. The [[Female Genital Tract|uterus and vagina]] are suspended from the [[sacrum]] and lateral pelvic sidewall via the [[The Uterine And Cervical Ligaments|uterosacral and cardinal ligament complexes]]. The weakening of these ligaments allows for the prolapse of the uterus into the vaginal vault. |
| | * Although uterine prolapse is not inherently life-threatening, it can lead to sexual dysfunction, poor body image, and lower quality of life due to associated bowel or bladder incontinence.<ref name=":0">Chen CJ, Thompson H. [https://www.statpearls.com/ArticleLibrary/viewarticle/30897 Uterine Prolapse]. StatPearls [Internet]. 2020 Nov 19.Available from:https://www.statpearls.com/ArticleLibrary/viewarticle/30897 (accessed 4.4.2021)</ref>.<ref name="three">Bordman R, Telner D, Jackson B, Little D. Step-by-step approach to managing pelvic organ prolapse. Canadian Family Physician; 2007; 53: 485-487.</ref> <ref name="twentyone">Mater Mothers' Hospital. Prolapse. http://brochures.mater.org.au/Home/Brochures/Mater-Mothers--Hospitals/Prolapse (accessed 5 April 2010).</ref> |
| | * Upon diagnosis, patients should be reassured that uterine prolapse is a common and well-known condition. Additionally, educating patients regarding potential sequelae and available treatments will allow them to know what to expect and make them active participants in their own care<ref name=":0" />. |
| | [[File:Uterus and nearby organs.jpeg|right|frameless|350x350px]] |
|
| |
|
| Uterine prolapse is the condition of the uterus collapsing, falling down, or downward displacement of the uterus with relation to the vagina.<ref name="one">Goodman CC, Snyder TEK. Differential Diagnosis for Physical Therapists. 4th ed. St. Louis: Saunders Elsevier, 2007.</ref> It is also defined as the bulging of the uterus into the vagina.<ref name="two">Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd ed. St. Louis: Saunders Elsevier, 2009</ref> <ref name="nineteen">Women's Surgery Center. Pelvic Organ Prolapse. http://www.gyndr.com/genital_prolapse_surgery.php (accessed 5 April 2010).</ref>
| | == Etiology == |
| | | The risk factors for uterine prolapse are the same as for other pelvic organ prolapses. |
|
| | * The Oxford Family Planning Association study found that pelvic organ prolapse became more likely with successive births. |
| | | * Women with [[Obesity|BMI >25]] were more likely to experience uterine prolapse than women with BMI in the normal range. |
| [[Image:Pelvic floor.jpg|left]]
| | * [[Older People - An Introduction|Advancing age]] has been shown to correlate markedly with rates of prolapse. |
| | | * Additional risk factors include [[Connective Tissue Disorders|connective tissue disorder]]<nowiki/>s such as [[Marfan Syndrome|Marfan]] syndrome and [[Ehlers-Danlos Syndrome|Ehler’s Danlos]] syndrome<ref name=":0" /> |
| <ref name="twenty">Natural Childbirth. Childbirth and your pelvic floor. http://childbirth.amuchbetterway.com/childbirth-and-your-pelvic-floor/ (accessed 5 April 2010).</ref><br>
| |
| | |
| <br>
| |
| | |
| <br>
| |
| | |
| <br>
| |
| | |
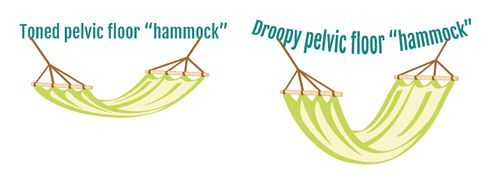
| When in proper alignment, the uterus and the adjacent structures are suspended in the proper position by the uterosacral, round, broad, and cardinal ligaments. The musculature of the pelvic floor forms a sling-like structure that supports the uterus, vagina, urinary bladder, and rectum.<ref name="two" /> Uterine prolapse is a result of pelvic floor relaxation or structural overstretching of the muscles of the pelvic wall and ligamentous structures.
| |
| | |
| [[Image:Different prolapse.jpg|thumb|right]]<br>
| |
| | |
| <br>
| |
| | |
| '''Uterine prolapse is characterized under a more general classification called pelvic organ prolapse which encompasses descent of the anterior, middle and posterior structures into the vagina'''.<ref name="three">Bordman R, Telner D, Jackson B, Little D. Step-by-step approach to managing pelvic organ prolapse. Canadian Family Physician; 2007; 53: 485-487.</ref>
| |
| | |
| *Those organs that bulge anterior into the vagina are the urinary bladder which is called a cystocele, the urethra, which is called a urethrocele or a combination, which is a cystourethrocele.<ref name="two" />,<ref name="three" />
| |
| *The uterus and the vaginal vault, which is the apex of the vagina, make up the organs that constitute the middle portion descent into the vagina. The vaginal vault often prolapses as a result of a hysterectomy.<ref name="three" />
| |
| *The rectal bulge is called a rectocele and a bulge of part of the intestine and peritoneum is called an enterocele, these make up the posterior portion of pelvic organ prolapse.<ref name="two" />,<ref name="three" />
| |
| *The information from this point forward will focus on uterine prolapse. | |
| | |
| <br>
| |
| | |
| <br>'''Uterine prolapse is classified using a four part grading system:'''
| |
| | |
| Grade 1: Descent of the uterus to above the hymen
| |
| | |
| Grade 2: Descent of the uterus to the hymen
| |
| | |
| Grade 3: Descent of the uterus beyond the hymen
| |
| | |
| Grade 4: Total prolapse.<ref name="three" /> <br>
| |
| | |
| <ref name="twentyone">Mater Mothers' Hospital. Prolapse. http://brochures.mater.org.au/Home/Brochures/Mater-Mothers--Hospitals/Prolapse (accessed 5 April 2010).</ref>
| |
| | |
| == Prevalence ==
| |
| | |
| Each source presents with a different prevalence depending on the researcher and the population used. One study stated that the prevalence of pelvic organ prolapse, a clinical classification for all of the pelvic structures prolapse into the vagina, was 50% for women who have give birth, though most women are asymptomatic.<ref name="three" /> Another article cited that 50% of the female population in the United States are affected by pelvic order prolapse with a prevalence rate that can vary from 30% to 93%, varying among different populations.<ref name="four">Kudish BI, Iglesia CB, Sokol RJ, Cochrane B, Richter HE, Larson J, et al. Effect of weight change on natural history of pelvic organ prolapse. Obstet Gynecol 2009; 113: 81-88.</ref> A questionnaire based study stated that 46.8% of the responses were positive for symptoms of pelvic organ prolapse and of the response group, 46.9% were vaginally examined with 21% having clinically relevant pelvic organ prolapse.<ref name="five">Hove MC, Pool-Goudzwaard AL, Eijkemans MJC, Steegers-Theunissen RPM, Burger CW, Vierhout ME. Prediction model and prognositc index to estimate clinically relevant pelvic organ prolapse ina general female population. Int Urogynecol J 2009; 20: 1013-1021.</ref>
| |
| | |
| == Characteristics/Clinical Presentation ==
| |
| | |
| The primary symptoms of a uterine prolapse are backache, perineal pain, and a sense of "heaviness" in the vaginal area.<ref name="two" /> Pain associated with uterine prolapse can be located centrally or suprapubic, and can be described as "dragging" in the groin. This pain is due to stretching of the ligamentous supports and secondarily to abrasion of the prolapsed tissues.<ref name="one" /> If the prolapse has progressed into a grade three or third degree prolapse, the person may feel as though they have a lump at the vaginal opening and have irritation and abrasion of the exposed mucous membrane of the cervix and vagina. This is possible both during sexual intercourse and from wiping with toileting procedures. The person may report that the symptoms are relieved by lying down and exacerbated with prolonged standing, walking, coughing or straining. An associated and often common complication of uterine prolapse is urinary incontinence.<ref name="two" /> Other descriptions used are the feeling of sitting on a small ball and a report of repeated bladder infections.<ref name="twentyfive">Vorvick LJ. Uterine prolapse. http://www.nlm.nig.gov/medlineplus/pring/ency/article/001508.htm (accessed 8 April 2010).</ref> <br>
| |
| | |
| ----
| |
| | |
| <u>'''[[Image:Uterine prolapse mayoclinic.jpg|frame|right|300x200px]]Summary from Differential Diagnosis for Physical Therapists''':</u>
| |
| | |
| *'''Lump in vaginal opening'''
| |
| *'''Pelvic discomfort, backache'''
| |
| *'''Abdominal cramping'''
| |
| *'''Symptoms relieved by lying down'''
| |
| *'''Symptoms made worse by prolonged standing, walking, coughing, or straining'''
| |
| *'''[http://www.acog.org/publications/patient_education/bp081.cfm Urinary incontinence]'''
| |
| | |
| <ref name="eleven">Mayo Clinic Staff. Uterine Prolapse Image. http://www.mayoclinic.com/health/medical/IM01785 (accessed 5 May 2010).</ref>
| |
| | |
| == Associated Co-morbidities ==
| |
| | |
| Obesity is a co-morbidity that often leads to progression and complication with uterine prolapse. In a study by the NIH over a five year period, 55.7% of the women in the study gained weight and the rate of prolapse increased from 40.9% to 43.8%. Looking specifically at uterine prolapse, when comparing participants with healthy BMI’s to overweight and obese persons, the risk of prolapse increased by 43% and 69%, respectively. However, the loss of weight did not presuppose a reversal of the uterine prolapse.<ref name="four" /> Other associated diseases that exacerbate uterine prolapse are chronic constipation and chronic obstructive pulmonary disease (COPD) due to the relationship between increased intra-abdominal pressure (bearing down) with increase in severity of the prolapse.<ref name="twelve">Mayo clinic staff. Uterine Prolapse. http://www.mayoclinic.com/health/uterine-prolapse/DS00700/DSECTION=risk-factors (accessed 5 April 2010).</ref>
| |
| | |
| == Medications ==
| |
| | |
| [[Image:HRT.jpg|right|400x400px]]<ref>Nazario B. Slideshow: all about menopause and perimenopause. http://www.webmd.com/menopause/slideshow-menopause-overview (accessed 11 April 2010).</ref>Hormone replacement therapy in the oral or vaginal form is indicated or a possible treatment to assist in maintaining elasticity of the pelvic floor musculature.<ref name="two" /><ref name="three" />
| |
| | |
| Women who have damage to tissue during childbirth do not frequently notice the laxity and pelvic relaxation until they enter menopause. Vaginal tissue and supporting structures depend on estrogen for their strength and elasticity. As estrogen levels decrease in certain situations (menopause and breast feeding mothers), the symptom become more apparent.
| |
| | |
| Estrogen replacement can come in the form of pills, vaginal rings, patches, or vaginal creams and are often indicated for lower grades of prolapse as the primary form of treatment. More severe prolapse is less likely to respond to estrogen therapy alone, however, it can be used as an adjunct to other treatments. Estrogen replacement can also be used after surgery to maintain results of surgery and help to revitalize dry and thin vaginal tissue.<ref name="ten">Streicher LF. Uterine prolapse and pelvic relaxation. www.mygyne.info/uterineProlapse.htm (accessed 5 April 2010).</ref>
| |
| | |
| == Diagnostic Tests/Lab Tests/Lab Values ==
| |
| | |
| Observation is often the first means of diagnosis.<ref name="two" /> Physical examination is the primary means for diagnosis. A bimanual test is performed with a speculum while the person is at rest and when the person is straining. If prolapse is not apparent with the first method, the person repeats the test while standing with one foot on a chair. The person is then graded using a first through third degree categorization. A first degree prolapse is characterized by descent of the uterus to above the hymen. A second degree prolapse is to the level of the hymen and a third degree prolapse is below the level of the hymen and protrudes through the vaginal opening.<ref name="two" /> Urine culture is ordered if needed. If still unsure about the diagnosis, a pelvic ultrasonography or cystography can be ordered.<ref name="three" />
| |
| | |
| == Causes ==
| |
| | |
| Women most at risk for this condition are those who have had multiple pregnancies and deliveries in combination with obesity. Associated risk factors are trauma to the pudendal or sacral nerves when giving birth. The disorder has been attributed to prolonged labor, bearing down before full dilation, and forceful delivery of the placenta. Decreased muscle tone due to aging, excessive strain during bowel movement and complications of pelvic surgery have also been associated with prolapse of the uterus and adjacent organs.<ref name="two" /> Associated risk also exists with pelvic tumors and neurologic condition like spina bifida and diabetic neuropathy which interferes with innervation of pelvic musculature.<ref name="two" /> Genetics are suspected in this condition due to multiple familial relations and generations with this and related conditions.<ref name="ten" /> A recent article has found that Cesarean section may lower the risk for pelvic organ prolapse.<ref name="twentysix">Reuters Health Information. Cesarean section may lower risk of pelvic organ prolapse. American Journal of Obstetrics and Gynecology 2009;200:243-245.</ref>
| |
| | |
| <u>'''Summary of Causes:'''</u>
| |
| | |
| *Multiple pregnancies and deliveries
| |
| *Obesity
| |
| *Trauma to pudendal or sacral nerves
| |
| *Aging related muscle changes
| |
| *Excessive strain during bowel movements
| |
| *Pelvic tumors
| |
| *Genetic predisposition <br><br>
| |
| | |
| <span id="fck_dom_range_temp_1271009608359_357"></span>
| |
| | |
| == Systemic Involvement ==
| |
| | |
| The digestive and urinary system can be impacted by uterine prolapse if the uterus obstructs the bladder/urethra and the rectum, decreasing the ability to void.<ref name="six">Hove MC, Pool-Goudzwaard Al, Eijkemans MJC, Steegers-Theunissen RPM, Burger CW, Vierhout ME. The prevalence of pelvic organ prolapse symptoms and signs and their relation with bladder and bowel disorders in a general female population. Int Urogynecol J 2009; 20:1037-1045.</ref> The reproductive system can also be impacted by painful intercourse, decreasing the ability for reproduction.<ref name="one" />
| |
| | |
| == Medical Management (current best evidence) ==
| |
| | |
| <u>'''Corrective Surgery'''</u>
| |
| | |
| Corrective surgery was a once popular first step for uterine prolapse but has fallen second choice to rehabilitation. When surgery is indicated, it is a management tool for second, third, and fourth-degree uterine prolapse.<ref name="two" /> Pelvic organ prolapse surgery has a success rate of 65% to 90% and has a repeated rate of operation at 30%. Patients who have more than one compartment involved may need a combination of surgeries and surgery can often predispose patients to prolapse in another compartment. Surgery can be either open or laparoscopic of the abdomen or can be in the vagina using fasciae, mesh, tape or sutures to suspend the organs. Another surgical procedure that is used in attempt to conserve the uterus is a sacrohysteropexy which is a Y-shaped graft that attaches the uterus to the sacrum.<ref name="three" /> One case study that examined the effectiveness in laparoscopic sacrohysteropexy, stated that this procedure “maintains durable anatomic restoration, normal vaginal axis and sexual function.” It also requires less time and less adhesion formation due to the laparoscopic approach versus an abdominal route.<ref name="seven">Faraj R, Broome J. Laparoscopic sacrohysteropexy and myomectomy for uterine prolapse: a case report and review of the literature. Journal of Medical Case Reports 2009; 3: 99-102.</ref> Vaginal hysterectomy, vesicourethral suspension, and abdominal hysterectomy are other possible approaches.<ref name="two" /> Important components for consideration of a surgical approach are:
| |
| | |
| *Degree of prolapse | |
| *Desire for future pregnancies
| |
| *Other medical conditions
| |
| *The woman's desire to retain vaginal function
| |
| *The woman's age and general health<ref name="twentyfive" />
| |
| | |
| {{#ev:youtube|gdAMSE2ViTY}}<ref>Pedro Torres. Total Uterine Prolapse. Available from: http://www.youtube.com/watch?v=gdAMSE2ViTY [last accessed 4/5/10]</ref>
| |
| | |
| '''<u>Pessary</u>'''
| |
| | |
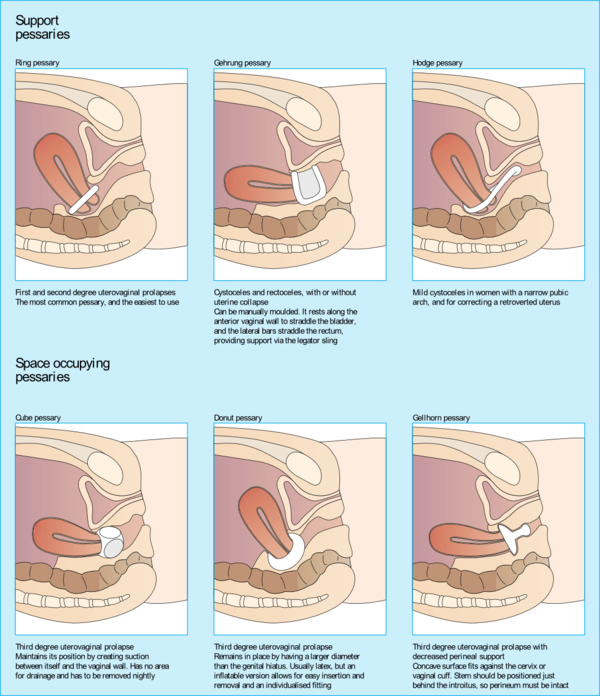
| A pessary is a shaped device made to support the uterus in the vagina. This is often a non-surgical approach used for both uterine prolapse and urinary incontinence. There is a supportive type for milder prolapse and a space-occupying type for more serious prolapse. The goal of the pessary is to find the largest fit that is comfortable. They are to be removed regularly for cleaning by the individual with correct education or by a health care professional.<ref name="three" /> There are rings, rings with a rubber support, cubes, donut shapes and inflatable balls. Depending on the degree of prolapse will determine the type that is chosen. <ref name="ten" />Patients who are not eligible for use of a pessary are those who cannot perform maintenance care of the pessary, those with vaginal ulcerations or lesions, severe atrophy of the vagina and women who develop recurrent vaginitis.<ref name="eight">UroToday. NIDDK UI Symposium - Devices for the Woman with Pelvic Organ Prolapse/Urinary Incontinence - Session Highlights. http://www.urotoday.com/48/browse_categories/urinary_incontinence_ui/niddk_ui_symposium___devices_for_the_woman_with_pelvic_organ_prolapseurinary_incontinence__session_highlights06102009.html (accessed 5 April 2010).</ref> Signs of improper fit are: those who have pain when wearing the pessary, vaginal ulceration and infection, and the inability to have a bowel movement or urinate.<ref name="ten" />
| |
| | |
| [[Image:Pessaries.jpg|frame|center]] <ref name="thirteen">Global Library of Women's Medicine. Stress Urinary Incontinence. http://www.glowm.com/index.html?p=glowm.cml/section_view&amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;articleid=60 (accessed 5 April 2010).</ref> | |
| | |
| '''<u>No Treatment</u>'''
| |
| | |
| Surgical treatment is not appropriate when the woman has recently had a baby. Tissue damaged during childbirth that has caused an associated prolapse, often begins to improve when undergoing tissue healing. A symptomatic prolapse in the first few weeks after delivery, especially in breastfeeding mothers have lower estrogen levels, does not necessarily predispose the mother to long term issues. Improvement tends to occur after discontinuation of nursing and the return of normal hormone levels. Other women and/or physicians do not elect for medical treatment for Stage 1 and Stage 2 prolapse and take a wait and see approach.<ref name="ten" />
| |
| | |
| == Physical Therapy Management (current best evidence) ==
| |
| | |
| Pelvic floor strengthening exercise is currently the front line treatment before surgery and also following surgery, these include but are not limited to Kegel exercises.<ref name="two" /><ref name="three" /> Other methods currently used are pelvic floor musculature re-education, postural education, biofeedback and electrical stimulation.<ref name="two" />
| |
| | |
| '''<u>Pelvic Floor Training</u>'''
| |
| | |
| Pelvic floor muscles are seventy percent slow-twitch muscle fibers, which assist in muscle endurance with generation of slow and sustained contractions. These muscles are designed to have a less intense contraction, whereas the other thirty percent, which are fast twitch, are designed for quick and forceful contraction. An example of fast twitch muscles are the muscles that close the urethra during increased intra-abdominal pressure.<ref name="thirty" /> Pelvic floor training is progressive resistive exercises for the pelvic floor that are often titled Kegel exercises. These exercises improve urethral resistance and pelvic visceral support by increasing the voluntary periurethral muscles. Pelvic floor exercises enhance the voluntary closing mechanisms. A thorough assessment of pelvic floor function is necessary to determine the muscular strength and endurance by manual muscle test. <ref name="twentytwo">Institut Francais de Readapation URo-Genitale. Physical therapy for female pelvic floor disorders. Current Opinion in Obstetrics and Gynecology 1994;6:331-335.</ref> Kegel exercises are often explained as contracting the muscles that stop the flow of urine. A sustained pelvic contraction for a minimum of two seconds is likely to ensure a better response to physical therapy. A five point rating scale is used to describe the contractile strength during pelvic musculature examination.
| |
| | |
| {| width="446" cellspacing="1" cellpadding="1" border="1" align="center" style="width: 446px; height: 163px;"
| |
| |+ '''Five-Point Rating Scale<ref name="twentyseven" />'''
| |
| |-
| |
| | Grade<span id="fck_dom_range_temp_1270905286363_914"></span>
| |
| | Description
| |
| |-
| |
| | 0
| |
| | No contraction
| |
| |-
| |
| | 1
| |
| | Flicker, only with muscles stretched
| |
| |-
| |
| | 2
| |
| | Weak squeeze, 2 second hold
| |
| |-
| |
| | 3
| |
| | Fair squeeze with definite "lift" (in which the contraction can be felt to move in an upward direction)
| |
| |-
| |
| | 4
| |
| | Good squeeze, good hold with lift (the contraction must be able to be repeated a few times)
| |
| |-
| |
| | 5
| |
| | Strong squeeze, good lift, repeatable
| |
| |}
| |
| | |
| One important observation with success of Kegel exercise is the identification of the correct musculature contraction by a specialized Physical Therapist. Approximately 19% to 31% of women who believe they perform Kegels actually perform them correctly. The woman is instructed to contract her muscles around the examiners fingers while the examiner determines if the patient is using auxiliary muscles like the abdomen, gluteals, or thighs. Bearing down is a common mistake when asked to perform a pelvic muscle contraction. Once the women has achieved holding the outer layer of the pelvic floor (bulbocavernosus and ischiocavernosis) in conjunction with higher level muscles like the levator ani, she should attempt to hold both for ten seconds.<ref name="twentyseven" /> An article by Lianne Herbruck listed a chart of instructions that summate the correct Kegel exercise procedure for pelvic floor muscle training.
| |
| | |
| {| width="430" cellspacing="1" cellpadding="1" border="1" align="center" style="width: 430px; height: 351px;"
| |
| |+ '''Proper Performance of Kegel Exercises for Pelvic Floor Muscle Training'''<ref name="thirty">Herbruck LF. Stress urinary incontinence: an overview of diagnosis and treatment options. Urologic Nursing 2008; 28: 186-199.</ref>
| |
| |-
| |
| | Kegel exercises are performed to strengthen the muscles of the pelvic floor to help increase support of the bladder and the urethra. They also can be used postpartum to facilitate circulation to the perineum, which promotes faster healing and increases pelvic floor muscle tone.
| |
| |-
| |
| | Have the woman contract the muscles in the perineum/pelvic floor as if she is trying to prevent passage of intestinal gas. (The old adage of "stopping the flow of urine" can actually encourage retention and cause dysfunction of the micturation reflex).
| |
| |-
| |
| |
| |
| She should feel the muscles draw upward and inward.
| |
| | |
| |-
| |
| | She should avoid straining or bearing-down motions while performing the contractions. (This can be avoided by exhaling gently with an open mouth as she contracts the muscles.)
| |
| |-
| |
| | Contractions should be intense, but should not involve abdomen, thighs, or buttocks.
| |
| |-
| |
| | The woman should be able to hold this contraction for 5 to 10 seconds, but may need to work up to that.
| |
| |-
| |
| | The woman should rest for 10 seconds between contractions.
| |
| |-
| |
| | Kegels should be performed at least 10 times, 3 times a day, or from 30 to 80 times a day.
| |
| |}
| |
| | |
| Current research prescribes a frequency of 30 contraction per day with an emphasis on increasing the strength and intensity of the contraction. A greater emphasis is placed on devoting a particular time to exercise and gradually increasing the amount and intensity of the exercise.<ref name="twentyseven" /> Though these exercises can improve function, they cannot reverse a Grade 3 or 4 uterine prolapse.<ref name="twentythree">Mayo Clinic. Pelvic floor weakness. Health Letter 2009:4-5.</ref> These exercises are often indicated as treatment for stress urinary incontinence, pelvic organ prolapse, pelvic pain and defecatory dysfunction.<ref name="twentyseven">Throwbridge ER, Fenner DE. conservative management of pelvic organ prolapse. Clinical Obstetrics and Gynecology 2005;48:668-681.</ref>
| |
| | |
| '''<u>Vaginal Cones</u>'''
| |
| | |
| This exercise is used as a adjunct to contraction exercises of the pelvic floor. The patient inserts weighted cones into the vagina and is instructed to maintain the position of the weighted cone. This method provides proprioceptive feedback to desired pelvic sustained contraction.<ref name="twentytwo" /> This is thought to help improve the tone through active and sustained muscle contraction.<ref name="thirty" /><br>
| |
| | |
| '''<u>Colpexin Sphere</u>'''
| |
| | |
| The Colpexin Sphere is an intravaginal device that provides support to the pelvic floor musculature and assists in elevation for more effective pelvic floor musculature exercises. "The Colpexin Sphere is a smooth, round sphere made of medical grade polycarbonate plastic with an attached braided nylon string for easy removal. It provides dual benefits for the management of pelvic organ prolapse and improvement of pelvic floor muscle weakness. The Colpexin Sphere is available only by prescription."<ref name="thirtyone">Marine Medical. The Colpexin Sphere. http://www.colpexin.com/about.cfm (accessed 11 April 2010).</ref> This is especially helpful for those who have urinary incontinence in association with uterine prolapse. This device is appropriate for candidates who prefer a conservative approach to pelvic floor prolapse management and urinary incontinence.<ref name="thirty" /> <ref name="thirtyone" />[[Image:Colpexin sphere.jpg|center|400x300px]]
| |
| | |
| '''<u></u>'''
| |
| | |
| '''<u></u>'''
| |
| | |
| '''<u></u>'''
| |
| | |
| '''<u>Biofeedback</u>'''
| |
| | |
| Biofeedback is used to detect and amplify internal physiological events and conditions using a monitoring instrument. This training helps to develop conscious control over these body processes. The objectives are to assist patients in gaining greater awareness and voluntary control over muscular control and contraction. This allows for a refined control of pelvic floor musculature for functional training. This technique uses a color video screen connected to a computerized unit which monitors different channels using intravaginal probe or surface electrodes depending on the muscles being selected.<ref name="twentytwo" /> The identification of the levator ani is important with contraction during the Kegel exercises. If they are weak or absent, physical therapy is indicated.<ref name="thirty" />
| |
| | |
| '''<u>Behavioral modification</u>'''
| |
| | |
| This technique is used to bring attention to the possible interactions between the patient's symptoms and their environment and provide techniques for behavioral modification. Such techniques consist of conditioning, fluid intake regulation, and use of devices. Bladder training is used for patients with associated incontinence for bladder prompted training, bladder drills, bladder habit training, and bladder retraining. In bladder retraining the patient is to keep a record of voiding activity over seven days and gradually increase increments between urination toward a normal three hour interval. The patient attempts to resist the urge to urinate by squeezing the pelvic floor and sphincter muscles until the urge resolves.<ref name="twentytwo" />
| |
| | |
| '''<u>Electrical Stimulation</u>'''
| |
| | |
| Electrical stimulation is used to inhibit the micturition reflex and contract pelvic floor muscles. Using a vaginal or anal probe, the electrical stimulation produces a contraction of the levator ani muscle. Electrical stimulation is also used based on the theory that low-level electrical currents might re-innervate the pelvic floor and change the ratio of slow-to-fast-twitch muscle fibers.<ref name="thirty" /> Electrostimulation is used in treatment of stress incontinence, enhancing the periurethral sphincter and urge incontinence, inhibiting the overactive detruser muscle. There are no side-effects except some discomfort but it is contraindicated for pregnancy, vaginal infection, retention and demand pacemaker.<ref name="twentytwo" />
| |
| | |
| '''<u></u>'''
| |
| | |
| '''<u></u>'''
| |
| | |
| '''<u></u>'''
| |
| | |
| '''<u></u>'''
| |
| | |
| '''<u></u>'''
| |
| | |
| '''<u></u>'''
| |
| | |
| '''<u>Education</u>'''
| |
| | |
| Education is an important aspect of treatment, especially education on positions of irritation and management of pain. Education plays an important role during exercise and discussion of sexual intercourse with gravity assisted positions. Supine with a pillow or wedge support under the pelvis can be useful position for rest, pelvic floor exercise performance and during intercourse.<ref name="one" /> Education is also important to help the patient understand why maintaining an ideal body weight limits the pressure the abdominal content places on the pelvic floor. Patients also be instructed to squeeze or perform a Kegel contraction when they are lifting or straining. Discussing bowel habits where the patient does not strain using the pelvic floor when having a bowel movement is an important component of bowel movement retraining. Women should also be advised on correct posture to aid in preventing strain on the pelvic floor muscles.<ref name="twentyseven" /><br>
| |
| | |
| Currently, there is no treatment protocol that has been shown to be the most effective. Most physical therapist who treat pelvic organ prolapse use pelvic floor muscle training defined as explanation of the anatomy and physiology, verbal explanation of pelvic floor muscle training technique in combination with educational material, biofeedback and electrical stimulation. Most outcome measures are patient-reported symptoms, pelvic floor muscle strength and quality of life. Fewer physical therapist are currently using a prolapse grading system than the above listed outcome measures.<ref name="twentyeight">Hagen S, Stark D. Physiotherapists and prolapse: who's doing what, how and why? Journal of the Association of Chartered Physiotherapists in Women's Health 2008; 103: 5-11.</ref>
| |
| | |
| <br>
| |
| | |
| In a study by Jarvis et al., preoperative and postoperative physical therapy was found to improve outcomes (quality of life questionnaire, urinary symptoms, and maximum pelvic floor muscle squeeze on mamometry) compared to a surgical group without per-operative physical therapy. This is an important indicator that physical therapy can play both a preventative role for surgical intervention but also plays an important role when surgery is indicated as the primary treatment.<ref name="twentynine">Jarvis SK, Hallam TK, Lujic S, Abbott JA, Vancaillie TG. Peri-operative physiotherapy improves outcomes for women undergoing incontinence and or prolapse surgery: results of a randomised controlled trial. Australian and New Zealand Journal of Obstetrics and Gynaecology 2005; 45: 300-303.</ref>
| |
| | |
| == Alternative/Holistic Management (current best evidence) ==
| |
| | |
| '''Methods considered in association with pelvic floor muscle strengthening are:'''
| |
| | |
| *weight loss for preventative measures | |
| *smoking cessation
| |
| *treatment of constipation to decrease intra-abdominal pressure<ref name="three" />
| |
| *adequate hydration
| |
| *increased fiber intake
| |
| *developing regular bowel habits
| |
| *regular exercise
| |
| *hormone replacement therapy.<ref name="two" />
| |
| *Education for the use of tight undergarments to help support and relieve symptoms of the prolapse.<ref name="twentyseven" />
| |
| | |
| == Differential Diagnosis ==
| |
| | |
| '''<u></u>'''
| |
| | |
| '''<u></u>'''
| |
| | |
| '''<u></u>'''
| |
| | |
| '''<u></u>'''
| |
| | |
| '''<u>[http://www.mayoclinic.com/health/cystocele/DS00665 Cystocele]</u>''': herniation of the urinary bladder into the vagina <ref name="two" />[[Image:Cystocele.jpg|center|200x200px]]
| |
| | |
| [[Image:Cystocele.jpg|center|2px]]<ref name="fourteen">Drug Information Online. Cystocele. http://www.drugs.com/cg/cystocele-aftercare-instructions.html (accessed 5 April 2010).</ref><br>'''<u>[http://www.mayoclinic.com/health/rectocele/DS00704 Retrocele]</u>''': herniation of the rectum into the vagina. Part of the rectum protrudes into the posterior wall of the vagina forming a pouch in the intestine. <ref name="two" /><ref name="fifteen">Drug Information Online. Rectocele. http://www.drugs.com/cg/rectocele.html (accessed 5 April 2010).</ref>[[Image:Rectocele.jpg|center|200x200px]]
| |
| | |
| <u>'''[http://www.acog.org/publications/patient_education/bp012.cfm Cystourethrocele]'''</u>: bladder and urethra prolapse into the vagina <ref name="two" />
| |
| | |
| '''<u>[http://www.acog.org/publications/patient_education/bp012.cfm Urethrocele]</u>''': bladder neck prolapses into the vagina <ref name="two" /><ref name="sixteen">MD Guidlines. Urethrocele with Stress Incontinence. http://www.mdguidelines.com/urethrocele-with-stress-incontinence (accessed 5 April 2010).</ref>[[Image:Urethrocele.jpg|center|250x250px]]
| |
| | |
| '''<u>[http://www.mayoclinic.com/health/enterocele/DS00765 Enterocele]</u>''': Part of the intestine and peritoneum prolapses into the vagina <ref name="two" /><ref name="seventeen">Nevade Surgery and Cancer Center. Enterocele. http://www.nvscc.com/enterocele.htm (accessed 6 April 2010).</ref>[[Image:Enterocele ncc.jpg|center|200x200px]]
| |
| | |
| <span id="fck_dom_range_temp_1270497621218_788"></span>'''<u>[http://www.acog.org/publications/patient_education/bp012.cfm Vaginal vault prolapse]</u>''': apex of vagina prolapses <ref name="two" />
| |
| | |
| <br>
| |
| | |
| == Case Reports ==
| |
| | |
| '''Faraj J, Broome J. Case Reports Laparoscopic sacrohysteropexy and myomectomy for uterine prolapse: a case report and review of the literature. Journal of Medical Case Reports 2009; 3: 99.'''
| |
| | |
| '''Abstract<br>'''A large number of hysterectomies are carried out for uterine prolapse, menorrhagia and other symptomatic but benign gynaecological conditions, which has increased interest in new approaches to treat these disorders. These new procedures are less invasive and offer reduced risk and faster recovery. Sacrohysteropexy can be carried out instead of vaginal hysterectomy in the treatment of uterine prolapse. It involves using a synthetic mesh to suspend the uterus to the sacrum; this maintains durable anatomic restoration, normal vaginal axis and sexual function. A laparoscopic approach has major advantages over the abdominal route including shorter recovery time and less adhesion formation. We describe a laparoscopic sacrohysteropexy in a 55-year-old Caucasian British woman that was technically difficult. An intramural uterine fibroid was encroaching just above the uterosacral ligament making mesh positioning impossible. This was removed and the procedure completed successfully. Posterior wall fibroid is not a contraindication for laparoscopic sacrohysteropexy. This procedure has increasingly become an effective treatment of uterine prolapse in women who have no indication for hysterectomy.
| |
| | |
| '''Available at''': [http://jmedicalcasereports.com/content/3/1/99 jmedicalcasereports.com/content/3/1/99] <br>
| |
| | |
| <br>'''Karateke A, Gurbuz K, Kabaca C, Mengulluoglu M. Sacrocervicopexy and Combined Operations Involving Cases of Total Uterine Prolapse 2003; 13: 164-168.'''
| |
| | |
| '''Abstract<br>'''Objective: To determine the outcome of sacrocervicopexy and combined operations in the treatment of uterovaginal prolapse in women with desire to preserving both uterus and fertility. Clinical Presentation and Intervention: Sacrocervicopexy with Prolene mesh and combined operations were performed in 3 women with total uterine prolapse because of the patient’s desire to retain fertility in 2 cases and refusal of hysterectomy in the 3rd patient. The 1st case was a 38-year-old woman, gravida 2, parity 1; the 2nd case a 42-year-old woman, gravida 3, parity 2, and the 3rd a 39-year-old woman, gravida 1, parity 1. Douglas pouch was obliterated with Moschcowitz operation. All of the women underwent sacrocervicopexy with Prolene mesh. The repair of a paravaginal defect and prophylactic Burch urethropexy were accomplished through entering Retzius’ space. Genital hiatus was narrowed via approximating levator muscles transvaginally. No serious intraoperative complications occurred and no recurrence was detected during the follow-up period. There was no postoperative complication except for some degree of pain in the 1st postoperative month in 1 case. Conclusion: The results indicate that sacrocervicopexy and repair of all concomitant defects in the pelvic floor are effective procedures in the treatment of uterovaginal prolapse in cases where there is a desire to retain fertility and uterus
| |
| | |
| '''Available at:''' [http://content.karger.com/ProdukteDB/produkte.asp?Aktion=ShowPDF&ArtikelNr=76957&Ausgabe=229975&ProduktNr=224259&filename=76957.pdf content.karger.com/ProdukteDB/produkte.asp]
| |
| | |
| <br>'''Kang LM, Liu CH, Huang Cl, Lee MG. Uterine prolapse results in vesical stones, ureteral stone, and acute renal failure: a case report. Journal of Urology ROC 2000; 11: 190-192.'''
| |
| | |
| '''Abstract<br>'''We present a case of a 66-year-old woman who visited our hospital on account of acute renal failure combined with vesical stones and ureteral stone due to uterine prolapse. An emergency percutaneous nephrostomy was performed, and supportive treatment was administered. On the 5th day post-hospitalization, the renal function of the patient had recovered to a normal range. Then cystoscopy, ureteroscopy, and electrohydraulic lithotripsy were performed to remove the vesical stones and ureteral stone. Finally we consulted a gynecologist to perform a vaginal hysterectomy together with anterior and posterior colporraphy, and culdoplasty to treat the uterine prolapse. The patient was discharged in a stable condition. Since then, the patient has visited our outpatient department regularly, and no more acute renal failure or urolithiasis have
| |
| | |
| '''Available at: '''[http://www.tua.org.tw/magazine/FileM/dw2005121154454_%E5%BA%B7%E7%AB%8B%E7%9B%9F499-1.pdf www.tua.org.tw/magazine/FileM/dw2005121154454_%E5%BA%B7%E7%AB%8B%E7%9B%9F499-1.pdf]
| |
|
| |
|
| == Resources <br> == | | == Epidemiology == |
|
| |
|
| MayoClinic.com: [http://www.mayoclinic.com/health/uterine-prolapse/DS00700 www.mayoclinic.com/health/uterine-prolapse/DS00700]
| | It is difficult to distinguish rates of uterine prolapse from pelvic organ prolapse as most studies cohort them together. |
| | * Approximately 50% of women in the US can be expected to have some degree of pelvic organ prolapse in advanced age ( affects 9.7% of women between ages 20-39 and 49.7% of women >80 years old). |
| | * In less developed countries such as Nepal, greater than 1 million women out of approximately 15 million women have been found to have uterine prolapse, equating to approximately 7% of the Nepalese female population<ref name=":0" /> |
|
| |
|
| Cleveland Clinic: [http://my.clevelandclinic.org/disorders/Uterine_Prolapse/hic_Uterine_Prolapse.aspx my.clevelandclinic.org/disorders/Uterine_Prolapse/hic_Uterine_Prolapse.aspx]
| | == Clinical Presentation == |
| | Image 3: Uterosacral ligament |
| | [[File:Uterosacral ligament.png|right|frameless]] |
| | The symptoms of uterine prolapse include: |
| | * a sensation of heaviness and pressure in the vagina |
| | * a distinct lump or bulge within the vagina |
| | * a bulge protruding out of the vagina |
| | * painful sexual intercourse. |
| | Uterine prolapse is described in 4 stages, indicating how far it has descended. Other pelvic organs (such as the bladder or bowel) may also be prolapsed into the vagina. |
| | * Stage I – the uterus is in the upper half of the vagina |
| | * Stage II – the uterus has descended nearly to the opening of the vagina |
| | * Stage III – the uterus protrudes out of the vagina |
| | * Stage IV – the uterus is completely out of the vagina<ref name=":1">Vic Health [https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/prolapsed-uterus#treatments-for-uterine-prolapse Uterus Prolapse] Available from:https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/prolapsed-uterus#treatments-for-uterine-prolapse (accessed 4.4.2021)</ref>. |
|
| |
|
| Medline Plus: [http://www.nlm.nih.gov/medlineplus/ency/article/001508.htm www.nlm.nih.gov/medlineplus/ency/article/001508.htm]
| | == Treatment/Management == |
| | [[File:Pelvic-floor-muscles hammock.jpg|right|frameless|500x500px]] |
| | Treatment of uterine prolapse is largely dependent on the extent to which a patient is experiencing symptoms. Treatments include surgical and non-surgical options, the choice of which will depend on general health, the severity of the condition and plans for a future pregnancy. |
|
| |
|
| Merck: [http://www.merck.com/mmpe/sec18/ch250/ch250c.html www.merck.com/mmpe/sec18/ch250/ch250c.html]
| | Proper diagnosis and management of uterine prolapse can majorly impact a patient’s quality of life and can have long-term physical and mental health effects. Healthcare practitioners should thoroughly counsel patients with uterine prolapse so they can make informed decisions and choose the treatment that is right for them<ref name=":0" />. |
|
| |
|
| Medscape: [http://search.medscape.com/medscape-search?queryText=uterine%20prolapse search.medscape.com/medscape-search]
| | Options include: |
| | * Pelvic floor exercises |
| | * Vaginal pessary |
| | * Vaginal surgery.<ref name=":1" /> |
| | # Pelvic floor muscle training: |
| | * Typically taught to patients in association with a physiotherapist. They have been shown to result in subjective improvement in symptoms by patients as well as objective improvement in the The Pelvic Organ Prolapse Quantification (POP-Q) system score by examiners. |
| | [[File:Pessary.png|right|frameless|696x696px]] |
| | 2. Vaginal pessaries: |
| | * Objects often made of silicone that are inserted into the vagina to provide support for the prolapsed pelvic organs. |
| | * Vaginal pessaries can be an effective way of reducing the symptoms of a prolapse, but they will not be appropriate for everyone. Together with pelvic floor exercises, they may provide a non-surgical solution to manage a uterine prolapse. |
| | * Vaginal pessaries provide a solution in 84% of cases of advanced pelvic organ prolapse with mild adverse events in 31% of cases. |
| | * Patients must be fitted for a pessary and commonly try several pessaries before finding the appropriate one. The examiner should be able to sweep a single finger between the pessary and vaginal walls. The patient should be able to walk, bend, and urinate comfortably without shifting the pessary. Complications of pessary placement include vaginal irritation/ulceration, discharge, pain, bleeding, and odor. |
| | * Regular reassessments of pessary fit should be performed to ensure that the pessary is not rubbing against the walls of the vagina, as this can lead to irritation of the vaginal mucosa and predispose patients to infection. Patients with dementia or poor follow up are not good candidates for pessary placement as they require frequent cleaning and regular reassessment of position to prevent complications. |
| | 3. Surgical management |
| | * Decision should be made after a detailed discussion with the patient regarding the desire for future vaginal intercourse, effects on body image, cultural views, alternative treatments, and potential complications. |
| | * In moderate to severe cases, the prolapse may have to be surgically repaired. In laparoscopic surgery, instruments are inserted through the navel. The uterus is pulled back into its correct position and reattached to its supporting ligaments. The operation can also be performed with an abdominal incision. |
| | * Surgery may fail and the prolapse can recur if the original cause of the prolapse, such as obesity, coughing or straining, is not addressed<ref name=":1" /><ref name=":0" />. |
|
| |
|
| {{#ev:youtube|4vCCy41lATo}}<ref>snowheadcouk. 600,000 Women in West Nepal suffer from Uterine Prolapse. Available from: http://www.youtube.com/watch?v=4vCCy41lATo [last accessed 4/6/10</ref>
| | == Physiotherapy == |
| | Physical therapists play a major role in the nonsurgical management of Uterine prolapse. Along with pessary support, pelvic-floor muscle training (PFMT) is cited in highly credible reviews as a main nonsurgical option for women with Uterine prolapse.<ref>Saunders K. [https://academic.oup.com/ptj/article/97/4/455/3057463 Recent advances in understanding pelvic-floor tissue of women with and without pelvic organ prolapse: considerations for physical therapists.] Physical therapy. 2017 Feb 28;97(4):455-63. Available from:https://academic.oup.com/ptj/article/97/4/455/3057463 (last accessed 11.1.2020)</ref> |
|
| |
|
| An international area of research and advocacy for women with uterine prolapse occurs through the women of Nepal. Currently they have the highest rate of uterine prolapse in the world and the poorest conditions for women based on position in society. To get more involved, the following site has been provided:
| | See the great physiotherapy section in [[Pelvic Organ Prolapse]] |
|
| |
|
| The Advocacy Project: [http://www.advocacynet.org/page/upa www.advocacynet.org/page/upa] | | == Complications == |
| | The weakness of pelvic floor attachments allowing for prolapse of the apical compartment can additionally allow for prolapse of the anterior and posterior compartments resulting in a compounded cystocele, rectocele, and/or enterocele. These often concomitant conditions can result in urinary incontinence, fecal incontinence, and long term morbidity<ref name=":0" />.<article> |
| | In addition to physical discomfort, it is common for patients to experience anxiety, depression, and poor self-esteem as a result of their condition thus, referral for psychotherapy should be offered<ref name=":0" />. |
| | ==References == |
| | <references /> |
|
| |
|
| == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) ==
| | [[Category:Womens_Health]] |
| <div class="researchbox">
| | [[Category:Pelvic Health]] |
| <rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1fEDSjbVglhftIGLKNZUNvZNqEbjiwkxDNu-giQ2lS6Di9dYk6|charset=UTF-8|short|max=10</rss>
| | [[Category:Pelvis]] |
| </div>
| | [[Category:Pelvis - Conditions]] |
| == References<br> ==
| | [[Category:Conditions]] |
| <references /></div>
| | [[Category:Bellarmine_Student_Project]] |
| [[Category:Articles]] [[Category:Condition]] [[Category:Womens_Health]] [[Category:Bellarmine_Student_Project]] [[Category:Videos]] | |