Uterine Prolapse
Original Editors - Amanda Mattingly from Bellarmine University's Pathophysiology of Complex Patient Problems project. Top Contributors - Amanda Mattingly, Admin, Lucinda hampton, Kim Jackson, WikiSysop, 127.0.0.1, Elaine Lonnemann, Wendy Walker, Oyemi Sillo and Nicole Hills
Definition/Description[edit | edit source]
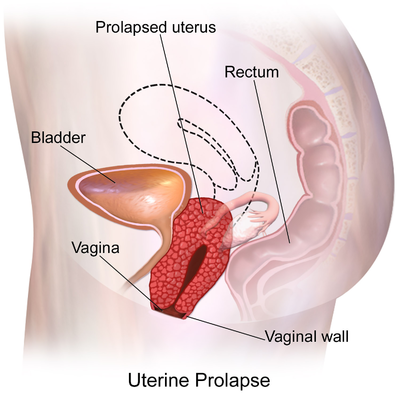
Uterine prolapse is the herniation of the uterus into the vaginal canal due to the weakening of its support structures. This is a common condition that is not life-threatening; however, it causes significant morbidity among women.[1]
Uterine prolapse is the herniation of the uterus from its natural anatomical location into the vaginal canal, through the hymen, or through the introitus of the vagina. This is due to the weakening of its surrounding support structures. Uterine prolapse is one of the multiple conditions that are classified under the broader term of pelvic organ prolapse.
In its usual state, the uterus rests in the apical compartment of pelvic organs. The uterus and vagina are suspended from the sacrum and lateral pelvic sidewall via the uterosacral and cardinal ligament complexes. The weakening of these ligaments allows for the prolapse of the uterus into the vaginal vault.
Although uterine prolapse is not inherently life-threatening, it can lead to sexual dysfunction, poor body image, and lower quality of life due to associated bowel or bladder incontinence.[1]
Uterine prolapse is classified using a four-part grading system:
- Grade 1: Descent of the uterus to above the hymen
- Grade 2: Descent of the uterus to the hymen
- Grade 3: Descent of the uterus beyond the hymen
- Grade 4: Total prolapse.[2] [3]
Etiology[edit | edit source]
The risk factors for uterine prolapse are the same as for other pelvic organ prolapses.
- The Oxford Family Planning Association study found that pelvic organ prolapse became more likely with successive births.
- Women with BMI >25 were more likely to experience uterine prolapse than women with BMI in the normal range.
- Advancing age has been shown to correlate markedly with rates of prolapse.
- Additional risk factors include connective tissue disorders such as Marfan syndrome and Ehler’s Danlos syndrome[1]
Epidemiology[edit | edit source]
It is difficult to distinguish rates of uterine prolapse from pelvic organ prolapse as most studies cohort them together.
- Approximately 50% of women in the US can be expected to have some degree of pelvic organ prolapse in advanced age ( affects 9.7% of women between ages 20-39 and 49.7% of women >80 years old).
- In less developed countries such as Nepal, greater than 1 million women out of approximately 15 million women have been found to have uterine prolapse, equating to approximately 7% of the Nepalese female population[1]
Clinical Presentation[edit | edit source]
Pessary[edit | edit source]
Differential Diagnosis[edit | edit source]
Cystocele: herniation of the urinary bladder into the vagina [6]
[7]
Retrocele: herniation of the rectum into the vagina. Part of the rectum protrudes into the posterior wall of the vagina forming a pouch in the intestine. [6][8]
Cystourethrocele: bladder and urethra prolapse into the vagina [6]
Urethrocele: bladder neck prolapses into the vagina [6][9]
Enterocele: Part of the intestine and peritoneum prolapses into the vagina [6][10]
Vaginal vault prolapse: apex of vagina prolapses [6]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Chen CJ, Thompson H. Uterine Prolapse. StatPearls [Internet]. 2020 Nov 19.Available from:https://www.statpearls.com/ArticleLibrary/viewarticle/30897 (accessed 4.4.2021)
- ↑ Bordman R, Telner D, Jackson B, Little D. Step-by-step approach to managing pelvic organ prolapse. Canadian Family Physician; 2007; 53: 485-487.
- ↑ Mater Mothers' Hospital. Prolapse. http://brochures.mater.org.au/Home/Brochures/Mater-Mothers--Hospitals/Prolapse (accessed 5 April 2010).
- ↑ Pedro Torres. Total Uterine Prolapse. Available from: http://www.youtube.com/watch?v=gdAMSE2ViTY [last accessed 4/5/10]
- ↑ Global Library of Women's Medicine. Stress Urinary Incontinence. http://www.glowm.com/index.html?p=glowm.cml/section_view&articleid=60 (accessed 5 April 2010).
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Cite error: Invalid
<ref>tag; no text was provided for refs namedtwo - ↑ Drug Information Online. Cystocele. http://www.drugs.com/cg/cystocele-aftercare-instructions.html (accessed 5 April 2010).
- ↑ Drug Information Online. Rectocele. http://www.drugs.com/cg/rectocele.html (accessed 5 April 2010).
- ↑ MD Guidlines. Urethrocele with Stress Incontinence. http://www.mdguidelines.com/urethrocele-with-stress-incontinence (accessed 5 April 2010).
- ↑ Nevade Surgery and Cancer Center. Enterocele. http://www.nvscc.com/enterocele.htm (accessed 6 April 2010).
- ↑ Diane Lee. Integrated Systems Model for Physiotherapy in Womens' Health. Available from: https://www.youtube.com/watch?v=5oslM6Pe9AU [last accessed 8/2/15]