Zoonotic Diseases: Difference between revisions
(prevention section) |
No edit summary |
||
| (18 intermediate revisions by 3 users not shown) | |||
| Line 7: | Line 7: | ||
[[File:Zoonotic Diseases.jpg|right|frameless|500x500px]] | [[File:Zoonotic Diseases.jpg|right|frameless|500x500px]] | ||
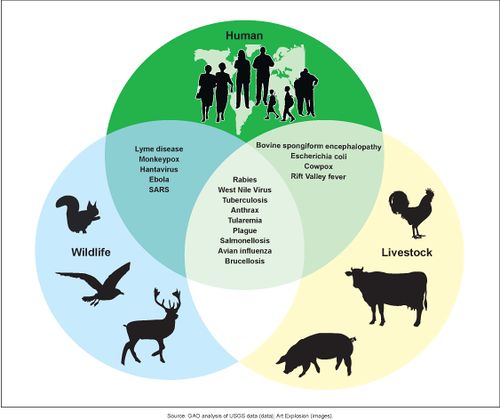
A zoonotic disease is any disease or infection that is transmissible from vertebrate animals to humans. <ref name="Van Dyke">Van Dyke JB. Veterinary zoonoses, what you need to know before you treat that puppy! American Physical Therapy Association Combined Sections Meeting; 2011 Feb 11; New Orleans, Louisianna.</ref>,<ref name="OVMA">Oregon Veterinary Medical Association. Zoonotic Diseases and Horses.fckLRhttp://oregonvma.org/care-health/zoonotic-diseases-horses. (accessed 8 March 2011).</ref> Recently emerged zoonotic diseases include globally devastating diseases such as: | A zoonotic disease is any disease or infection that is transmissible from vertebrate animals to humans. <ref name="Van Dyke">Van Dyke JB. Veterinary zoonoses, what you need to know before you treat that puppy! American Physical Therapy Association Combined Sections Meeting; 2011 Feb 11; New Orleans, Louisianna.</ref>,<ref name="OVMA">Oregon Veterinary Medical Association. Zoonotic Diseases and Horses.fckLRhttp://oregonvma.org/care-health/zoonotic-diseases-horses. (accessed 8 March 2011).</ref> Recently emerged zoonotic diseases include globally devastating diseases such as: | ||
* Coronaviruses (CoV), a large family of viruses that cause illness ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS-CoV),Severe Acute Respiratory Syndrome (SARS-CoV) and | * [[Coronaviruses]] (CoV), a large family of viruses that cause illness ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS-CoV),Severe Acute Respiratory Syndrome ([[Coronavirus Disease (COVID-19)|SARS-CoV]]) and [[Coronavirus Disease (COVID-19)|COVID 19]]<ref>WHO [https://www.who.int/health-topics/coronavirus Corona virus] Available from:https://www.who.int/health-topics/coronavirus (last accessed 5.3.2020)</ref> | ||
* Ebola virus disease | * [[Ebola Virus|Ebola]] virus disease | ||
* Highly pathogenic avian influenza | * Highly pathogenic avian influenza | ||
* Bovine spongiform | * [[Prion Diseases (or Transmissible Spongiform Encephalopathies)|Bovine spongiform encephalopathy]] <ref name=":0">Belay ED, Kile JC, Hall AJ, Barton-Behravesh C, Parsons MB, Salyer S, Walke H. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5711319/ Zoonotic disease programs for enhancing global health security. Emerging infectious diseases.] 2017 Dec;23(Suppl 1):S65. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5711319/ (last accessed 5.3.2020)</ref> | ||
Key Points | Key Points | ||
* Nearly two-thirds of human infectious diseases arise from pathogens shared with wild or domestic animals | * Nearly two-thirds of human infectious diseases arise from pathogens shared with wild or domestic animals | ||
| Line 21: | Line 21: | ||
=== How do Zoonoses spread === | === How do Zoonoses spread === | ||
Because of the close connection between people and animals, it’s important to be aware of the common ways people can get infected with germs that can cause zoonotic diseases. These can include: | Because of the close connection between people and animals, it’s important to be aware of the common ways people can get infected with germs that can cause zoonotic diseases. These can include: | ||
* Direct contact: Coming into contact with the saliva, blood, urine, mucous, feces, or other body fluids of an infected animal. Examples include petting or touching animals, and bites or scratches. | * Direct contact: Coming into contact with the saliva, [[Blood Physiology|blood]], urine, mucous, feces, or other body fluids of an infected animal. Examples include petting or touching animals, and bites or scratches. | ||
* Indirect contact: Coming into contact with areas where animals live and roam, or objects or surfaces that have been contaminated with germs. Examples include aquarium tank water, pet habitats, chicken coops, barns, plants, and soil, as well as pet food and water dishes. | * Indirect contact: Coming into contact with areas where animals live and roam, or objects or surfaces that have been contaminated with germs. Examples include aquarium tank water, pet habitats, chicken coops, barns, plants, and soil, as well as pet food and water dishes. | ||
* Vector-borne: Being bitten by a tick, or an insect like a mosquito or a flea. | * Vector-borne: Being bitten by a tick, or an insect like a mosquito or a flea. | ||
| Line 33: | Line 33: | ||
=== Prevention === | === Prevention === | ||
On a personal level | '''On a personal level''' | ||
The best way to protect oneself from many of these zoonotic diseases is to practice good hygiene after handling animals or their waste. Washing hands thoroughly with hot, soapy water after any contact will help prevention contraction of zoonotic diseases.<ref name="OVMA" /> In addition screening newly received animals, conducting a routine sanitization of the contaminated environment, equipment, and caging, wearing gloves and protective clothing will help decrease the possiblity of contracting a zoonotic disease.<ref name="ISU Fact Sheet Dermatomycoses">Iowa State University. Institutional Biosafety Committee. Guidance & Education. Zoonotic Disease Fact Sheets: dermatomycoses. http://compliance.iastate.edu/ibc/guide/zoonoticfactsheets/Dermatomycoses.pdf (accessed 8 March 2011).</ref> | The best way to protect oneself from many of these zoonotic diseases is to practice good hygiene after handling animals or their waste. Washing hands thoroughly with hot, soapy water after any contact will help prevention contraction of zoonotic diseases.<ref name="OVMA" /> In addition screening newly received animals, conducting a routine sanitization of the contaminated environment, equipment, and caging, wearing gloves and protective clothing will help decrease the possiblity of contracting a zoonotic disease.<ref name="ISU Fact Sheet Dermatomycoses">Iowa State University. Institutional Biosafety Committee. Guidance & Education. Zoonotic Disease Fact Sheets: dermatomycoses. http://compliance.iastate.edu/ibc/guide/zoonoticfactsheets/Dermatomycoses.pdf (accessed 8 March 2011).</ref> | ||
| Line 39: | Line 39: | ||
The four principal means of preventing spread of zoonoses are<ref name="Van Dyke" /> | The four principal means of preventing spread of zoonoses are<ref name="Van Dyke" /> | ||
1. parasite recognition and control | 1. [[Parasitic Infections|parasite]] recognition and control | ||
2. vaccination programs | 2. [[Vaccines|vaccination]] programs | ||
3. sanitation methods | 3. sanitation methods | ||
| Line 47: | Line 47: | ||
4. behavior training to prevent bites and scratches | 4. behavior training to prevent bites and scratches | ||
On a world wide level | '''On a world wide level''' | ||
Preventing zoonotic diseases requires coordinated actions by government authorities responsible for human and animal health. | Preventing zoonotic diseases requires coordinated actions by government authorities responsible for human and animal health. | ||
| Line 56: | Line 56: | ||
== Classes of Zoonoses == | == Classes of Zoonoses == | ||
Including [[Antiviral Drugs|viruses]], [[Bacterial Infections|bacteria]], [[Parasitic Infections|parasites]], and [[Fungal Diseases|fungi]]. | |||
=== Viral Zoonoses === | === Viral Zoonoses - 6 Common Viral Zoonoses === | ||
# Coronaviruses (CoV) are a large family of viruses that cause illness ranging from the common cold | |||
* 3 strains of corana virus are Middle East Respiratory Syndrome (MERS-CoV), Severe Acute Respiratory Syndrome (SARS-CoV, [[Coronavirus Disease (COVID-19)|Covid19]] - a new strain that has not been previously identified in humans. | |||
* Detailed investigations found that SARS-CoV was transmitted from civet cats to humans and MERS-CoV from dromedary camels to humans. | |||
* Several known coronaviruses are circulating in animals that have not yet infected humans. | |||
2. Ehrlichiosis - Ehrlichiosis is the general name used to describe diseases caused by the bacteria ''Ehrlichia chaffeensis'', ''E. ewingii'', or ''E. muris eauclairensis'' in the United States. These bacteria are spread to people primarily through the bite of infected ticks including the lone star tick (''Amblyomma americanum'') and the blacklegged tick (''Ixodes scapularis''). | |||
People with ehrlichiosis will often have fever, chills, headache, muscle aches, and sometimes upset stomach. Doxycycline is the treatment of choice for adults and children of all ages with ehrlichiosis.<ref>CDC [https://www.cdc.gov/ehrlichiosis/ Ehrlichiolis] Available from:https://www.cdc.gov/ehrlichiosis/ (last accessed 6.3.2020)</ref> | |||
3. [[Rocky Mountain Spotted Fever|Rocky Mountain Spotted Fever]] (Rickettsia ) | 3. [[Rocky Mountain Spotted Fever|Rocky Mountain Spotted Fever]] (Rickettsia ) Rocky Mountain Spotted Fever is a tick borne disease, due to an intracellular pathogen known as Rickettsia rickettsi | ||
4. [[Rabies|Rabies]] | 4. [[Rabies|Rabies]] - Rabies is an infectious, zoonotic disease that destroys brain cells and can lead to death if left untreated before symptoms appear. It is caused by a virus that lives in the saliva of a host or carrier and can be transmitted by being bitten by the carrier or if the infected saliva enters an open wound or mucous membranes. Rabies has been reported as being transmitted to people after breathing in air from caves that contained millions of bats and through organ transplants from an infected person. The most common sources of infections for humans are from wild animals and dogs.<ref>RABIES. (n.d.), [cited March 17, 2011]; Available from: Funk & Wagnalls New World Encyclopedia</ref>[[File:West nile virus.jpg|right|frameless]] | ||
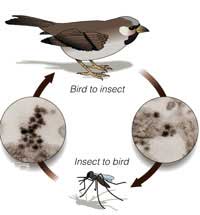
5. West Nile Virus - West Nile virus (WNV) is the leading cause of mosquito-borne disease in the continental United States. | |||
* It is most commonly spread to people by the bite of an infected mosquito. | |||
* Cases of WNV occur during mosquito season, which starts in the summer and continues through fall. | |||
* There are no vaccines to prevent or medications to treat WNV in people. | |||
* Fortunately, most people infected with WNV do not feel sick. | |||
* About 1 in 5 people who are infected develop a fever and other symptoms. | |||
* About 1 out of 150 infected people develop a serious, sometimes fatal, illness. | |||
* You can reduce your risk of WNV by using insect repellent and wearing long-sleeved shirts and long pants to prevent mosquito bites.<ref>CDC [https://www.cdc.gov/westnile/index.html West Nile Virus] Available from:https://www.cdc.gov/westnile/index.html (last accessed 6.3.2020)</ref> | |||
6. Equine Encephalitis - A mosquito borne infection normally maintained in nature by a cycle from an arthropod vector to a vertebrate reservoir host.<ref name="Van Dyke" /> | |||
* Some people experience it only as a mild illness for others it is fatal (fatal in about one-third of the cases). | |||
* Symptoms of eastern equine encephalitis usually appear three to 10 days after a bite by an infected mosquito.<ref name="Mayo Encephalitis">Mayo Foundation for Medical Education and Research. Encephalitis. [https://www.mayoclinic.com/health/encephalitis/DS00226/DSECTION=causes http://www.mayoclinic.com/health/encephalitis/DS00226/DSECTION=causes] (accessed 27 Feb 2011).</ref> | |||
* No vaccine exists for humans.<ref name="Van Dyke" /> | |||
* Personal protective measures are the primary way to avoid contracting the virus.<ref name="Van Dyke" /> | |||
=== Bacterial Zoonoses - 10 Common Bacterial Zoonoses === | |||
[[Image:Anthrax cycle.jpg|282x282px|Anthrax cycle. Image courtesy of [https://search.creativecommons.org/?q=cat%20scratch%20fever http://search.creativecommons.org/?q=cat%20scratch%20fever]|right|frameless|border]] | |||
[[Image:Anthrax cycle.jpg|282x282px|Anthrax cycle. Image courtesy of http://search.creativecommons.org/?q=cat%20scratch%20fever|right|frameless]] | |||
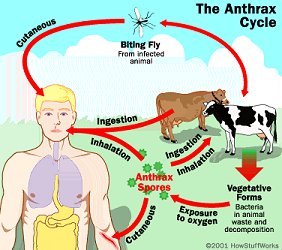
# Anthrax | # Anthrax | ||
Anthrax is an acute infectious disease caused by the spore-forming bacterium Bacillus anthracis<ref name="CDC Anthrax">Centers for Disease Control and Prevention. Emergency Preparedness and Response. Questions and Answers about Anthrax. http://www.bt.cdc.gov/agent/anthrax/faq/ (accessed 2 March 2011)</ref>, a microbe that lives in the soil.<ref name="Medline Plus Anthrax">U.S. National Library of Medicine. National Institute of Health. Medline Plus. Anthrax.http://www.nlm.nih.gov/medlineplus/anthrax.html (accessed 2 March 2011).</ref> Anthrax | Anthrax is an acute infectious disease caused by the spore-forming bacterium Bacillus anthracis<ref name="CDC Anthrax">Centers for Disease Control and Prevention. Emergency Preparedness and Response. Questions and Answers about Anthrax. http://www.bt.cdc.gov/agent/anthrax/faq/ (accessed 2 March 2011)</ref>, a microbe that lives in the soil.<ref name="Medline Plus Anthrax">U.S. National Library of Medicine. National Institute of Health. Medline Plus. Anthrax.[https://www.nlm.nih.gov/medlineplus/anthrax.html http://www.nlm.nih.gov/medlineplus/anthrax.html] (accessed 2 March 2011).</ref> | ||
* A serious infectious disease caused by gram-positive, rod-shaped bacteria known as Bacillus anthracis. | |||
2. Bartonella (Cat Scratch Fever) | * Anthrax can be found naturally in soil and commonly affects domestic and wild animals around the world. | ||
* Rare in the United States - people can get sick with anthrax if they come in contact with infected animals or contaminated animal products. | |||
* Contact with anthrax can cause severe illness in both humans and animals. | |||
* Anthrax is not contagious, which means you can’t catch it like the cold or flu. | |||
neck, and upper limbs, become swollen. | * Anthrax can occur in three forms: cutaneous, inhalation, and gastrointestinal.<ref name="CDC Anthrax" /><ref name="Medline Plus Anthrax" /> | ||
2. Bartonella (Cat Scratch Fever) - bacterial disease caused by Bartonella henselae. | |||
3. <font class="Apple-style-span" color="#AAAAAA"></font>[[Lyme Disease|Lyme ]][[Lyme Disease|Disease | * Most people with CSD have been bitten or scratched by a cat and developed a mild infection at the point of injury. | ||
* Lymph nodes, especially those around the head, neck, and upper limbs, become swollen. | |||
* Person with CSD may experience fever, headache, fatigue, and a poor appetite.<ref name="CDC" /> | |||
* Bartonella will begin in the human as a pustule that will gradually progress to regional lymphadenopathy which can last for months (or become a systemic illness in immunocompromised patients). | |||
* Can also be transmitted through the feces of fleas.<ref name="Van Dyke" /> | |||
3. <font class="Apple-style-span" color="#AAAAAA"></font>[[Lyme Disease|Lyme ]][[Lyme Disease|Disease]] | |||
* Lyme disease or Lyme borreliosis is the most commonly transmitted tick-borne infection in the United States and among the most frequently diagnosed tick-borne infections worldwide<ref>Skar GL, Simonsen KA. [https://www.ncbi.nlm.nih.gov/books/NBK431066/ Lyme Disease]. InStatPearls [Internet] 2018 Oct 27. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431066/ (last accessed 26.12.2019)</ref>. | * Lyme disease or Lyme borreliosis is the most commonly transmitted tick-borne infection in the United States and among the most frequently diagnosed tick-borne infections worldwide<ref>Skar GL, Simonsen KA. [https://www.ncbi.nlm.nih.gov/books/NBK431066/ Lyme Disease]. InStatPearls [Internet] 2018 Oct 27. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431066/ (last accessed 26.12.2019)</ref>. | ||
4. Brucellosis | 4. Brucellosis | ||
Brucellosis is a bacterial infection that spreads from animals to people. | |||
* Most commonly, people are infected by eating raw or unpasteurized dairy products. Sometimes, the bacteria that cause brucellosis can spread through the air or through direct contact with infected animals. | |||
5. | * Signs and symptoms of brucellosis may include fever, joint pain and fatigue. The infection can usually be treated with antibiotics. However, treatment takes several weeks to months, and the infection can recur. | ||
* Brucellosis affects hundreds of thousands of people and animals worldwide. Avoiding raw dairy products and taking precautions when working with animals or in a laboratory can help prevent brucellosis.<ref>Mayo Clinic [https://www.mayoclinic.org/diseases-conditions/brucellosis/symptoms-causes/syc-20351738 Brucellosis] Available from:https://www.mayoclinic.org/diseases-conditions/brucellosis/symptoms-causes/syc-20351738 (last accessed 6.3.2020)</ref> | |||
5. Ehrlichiosis | |||
The general name used to describe several bacterial diseases that affect animals and humans. | The general name used to describe several bacterial diseases that affect animals and humans. | ||
* Human ehrlichiosis is a disease caused by at least three different ehrlichial species in the United States | * Human ehrlichiosis is a disease caused by at least three different ehrlichial species in the United States. | ||
* Ehrlichiae are transmitted to humans by the bite of an infected tick. | * Ehrlichiae are transmitted to humans by the bite of an infected tick. | ||
* Symptoms usually occur within 1-2 weeks following a tick bite<ref name="CDC Ehrlichiosis" /><ref name="Mayo Ehrlichiosis">Mayo Foundation for Medical Education and Research. Ehrlichiosis. http://www.mayoclinic.com/health/ehrlichiosis/DS00702 (accessed 27 Feb 2011).</ref> and include fever, headache, fatigue, and muscle aches. | * Symptoms usually occur within 1-2 weeks following a tick bite<ref name="CDC Ehrlichiosis" /><ref name="Mayo Ehrlichiosis">Mayo Foundation for Medical Education and Research. Ehrlichiosis. [https://www.mayoclinic.com/health/ehrlichiosis/DS00702 http://www.mayoclinic.com/health/ehrlichiosis/DS00702] (accessed 27 Feb 2011).</ref> and include fever, headache, fatigue, and muscle aches. | ||
* Ehrlichios is is diagnosed based on symptoms, clinical presentation, and later confirmed with specialized laboratory tests. | * Ehrlichios is is diagnosed based on symptoms, clinical presentation, and later confirmed with specialized laboratory tests. | ||
* Treatment for adults and children of all ages is doxycycline.<ref name="CDC Ehrlichiosis">Centers for Disease Control and Prevention. Ehrlichiosis. http://www.cdc.gov/ehrlichiosis/ (accessed 27 Feb 2011).</ref> | * Treatment for adults and children of all ages is doxycycline.<ref name="CDC Ehrlichiosis">Centers for Disease Control and Prevention. Ehrlichiosis. http://www.cdc.gov/ehrlichiosis/ (accessed 27 Feb 2011).</ref> | ||
6. [[Leptospirosis]] | 6. [[Leptospirosis]] | ||
* A bacterial disease that affects humans & animals. | |||
A bacterial disease that affects humans & animals. | * Caused by the bacteria genus Leptospira. | ||
* Spread through urine of infected animals, which can get into water or soil and can survive for weeks to months. | |||
7. Plague ( | * Most common method of transmission is through direct contact with infected urine or other bodily fluids such as saliva, or contaminated water, soil, or food.<ref>World Health Organization [Internet]. [Place unknown]: WHO; Prepared for World Day 2001 [ cited 2016 March 31]. Available from: http://www.who.int/water_sanitation_health/diseases/leptospirosis/en/</ref> | ||
7. Plague (Yersinia enterocolitica, Yersinia pestis) | |||
Plague is a zoonotic infection that has affected humans for thousands of years. In humans, the primary plague syndromes are bubonic, septicemic, and pneumonic. All of these result from infection with the gram-negative bacillus ''Yersinia pestis''. The typical life-cycle of ''Y. Pestis'' starts within an insect vector followed by transmission to a mammalian host, typically rodents or other wild animals. Humans are only affected as incidental hosts. Despite this, ''Y. pestis'' is arguably one of the most important microbes in human history. It has caused three documented pandemics, with the “black death” in 14th century Europe leading to the death of up to 30% of the population. The most recent pandemic began in the late 19th century in Asia and India, and it continues today in Africa. Outside of this, the bacterium remains endemic in the Americas and Asia and also exists as a potential bioterrorism threat, spurring ongoing vaccine development[[Image:Yersinia swollen axillary lymph node.jpg|200x190px|Swollen axillary lymph node associated with yersinia pestis. Image from http://pathmicro.med.sc.edu/ghaffar/zoonoses.htm|right|frameless]] | Plague is a zoonotic infection that has affected humans for thousands of years. In humans, the primary plague syndromes are bubonic, septicemic, and pneumonic. All of these result from infection with the gram-negative bacillus ''Yersinia pestis''. The typical life-cycle of ''Y. Pestis'' starts within an insect vector followed by transmission to a mammalian host, typically rodents or other wild animals. Humans are only affected as incidental hosts. Despite this, ''Y. pestis'' is arguably one of the most important microbes in human history. It has caused three documented pandemics, with the “black death” in 14th century Europe leading to the death of up to 30% of the population. The most recent pandemic began in the late 19th century in Asia and India, and it continues today in Africa. Outside of this, the bacterium remains endemic in the Americas and Asia and also exists as a potential bioterrorism threat, spurring ongoing vaccine development[[Image:Yersinia swollen axillary lymph node.jpg|200x190px|Swollen axillary lymph node associated with yersinia pestis. Image from http://pathmicro.med.sc.edu/ghaffar/zoonoses.htm|right|frameless]] | ||
''<br>''8. Rickettsia ([[Rocky Mountain Spotted Fever|Rocky Mountain Spotted Fever]])[[Image:Rocky Mountain Spotted Fever rash.jpg|200x160px|Rash associated with Rocky Mountain Spotted Fever. Image can be found at http://commons.wikimedia.org/wiki/File:Rocky_Mountain_spotted_fever_PHIL_1962_lores.jpg|right|frameless]] | ''<br>''8. Rickettsia ([[Rocky Mountain Spotted Fever|Rocky Mountain Spotted Fever]])[[Image:Rocky Mountain Spotted Fever rash.jpg|200x160px|Rash associated with Rocky Mountain Spotted Fever. Image can be found at [https://commons.wikimedia.org/wiki/File:Rocky_Mountain_spotted_fever_PHIL_1962_lores.jpg http://commons.wikimedia.org/wiki/File:Rocky_Mountain_spotted_fever_PHIL_1962_lores.jpg]|right|frameless]] | ||
* A disease caused by the bacterium Rickettsia rickettsii, which is carried by ticks. | * A disease caused by the bacterium Rickettsia rickettsii, which is carried by ticks. | ||
* People usually start having fevers and feeling nauseous about a week after being bitten by a tick. | * People usually start having fevers and feeling nauseous about a week after being bitten by a tick. | ||
| Line 132: | Line 134: | ||
9. [[Methicillin-Resistant Staphylococcus Aureus|Methicillin Resistant Staphylococcus Aureus]] (MRSA) | 9. [[Methicillin-Resistant Staphylococcus Aureus|Methicillin Resistant Staphylococcus Aureus]] (MRSA) | ||
Methicillin-Resistant Staphylococcus Aureus (MRSA) is defined as a type of bacterial staph infection that is non-responsive to antibiotics normally prescribed to treat such infections.<ref>Mayo Clinic Staff. MRSA infection - Mayo Clinic [Internet]. Mayoclinic.org. 2016.[https://www.mayoclinic.org/diseases-conditions/mrsa/basics/definition/con-20024479 http://www.mayoclinic.org/diseases-conditions/mrsa/basics/definition/con-20024479] (accessed 1 April 2016).</ref> | Methicillin-Resistant Staphylococcus Aureus (MRSA) is defined as a type of bacterial staph infection that is non-responsive to antibiotics normally prescribed to treat such infections.<ref>Mayo Clinic Staff. MRSA infection - Mayo Clinic [Internet]. Mayoclinic.org. 2016.[https://www.mayoclinic.org/diseases-conditions/mrsa/basics/definition/con-20024479 http://www.mayoclinic.org/diseases-conditions/mrsa/basics/definition/con-20024479] (accessed 1 April 2016).</ref> | ||
* MRSA was first described in 1961-1962 in a patient whose infection was resistant to the drug Methicillin, which was discovered in 1960. | |||
The bacteria from which MRSA arises, staphylococcus aureus, is found in the skin and in the nostrils of one third of all people and do not show any symptoms of having been exposed to the bacteria. These carriers of the bacteria are then exposing the bacteria to all of the items that they touch as well as expelling it into the air where it will remain until the item is next cleaned. | * The incidence of MRSA greatly increased in the United States in the 1980s and was especially emerging in patients who used intravenous drugs<ref>Millar B, Loughrey A, Elborn J, Moore J. Proposed definitions of community-associated meticillin-resistant Staphylococcus aureus (CA-MRSA). Journal of Hospital Infection. 2007;67(2):109-113. http://eds.b.ebscohost.com.libproxy.bellarmine.edu/ehost/detail/detail?vid=14&sid=71ee6b7e-199d-4adc-8e31-bc94eca59a09%40sessionmgr113&hid=112&bdata=JmxvZ2luLmFzcCZzaXRlPWVob3N0LWxpdmUmc2NvcGU9c2l0ZQ%3d%3d#AN=105828672&db=cin20 (accessed 2 April 2016).</ref>. | ||
* The bacteria from which MRSA arises, staphylococcus aureus, is found in the skin and in the nostrils of one third of all people and do not show any symptoms of having been exposed to the bacteria. | |||
10. Streptococcus suis is a zoonotic pathogen that infects pigs and can occasionally cause serious infections in humans. S. suis infections occur sporadically in humans throughout Europe and North America, but a recent major outbreak has been described in China with high levels of mortality. The mechanisms of S. suis pathogenesis in humans and pigs are poorly understood.<ref>Holden et al. Rapid evolution of virulence and drug resistance in the emerging zoonotic pathogen streptococcus suis. PLoS One. 2009; 4(7). e6072. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2705793/(accessed 8 March 2011).</ref> | * These carriers of the bacteria are then exposing the bacteria to all of the items that they touch as well as expelling it into the air where it will remain until the item is next cleaned. | ||
10. Streptococcus suis is a zoonotic pathogen that infects pigs and can occasionally cause serious infections in humans. | |||
* S. suis infections occur sporadically in humans throughout Europe and North America, but a recent major outbreak has been described in China with high levels of mortality. | |||
* The mechanisms of S. suis pathogenesis in humans and pigs are poorly understood.<ref>Holden et al. Rapid evolution of virulence and drug resistance in the emerging zoonotic pathogen streptococcus suis. PLoS One. 2009; 4(7). e6072. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2705793/(accessed http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2705793/(accessed] 8 March 2011).</ref> | |||
=== Fungal Zoonoses === | === Fungal Zoonoses === | ||
| Line 142: | Line 147: | ||
Fungal infections associated with zoonotic transmission are an important public health problem worldwide . A number of these infections are among the group of the most common fungal diseases, such as: dermatophytosis, sporotrichosis , and histoplasmosis.<ref>Seyedmousavi S, Guillot J, Tolooe A, Verweij PE, De Hoog GS. [https://www.sciencedirect.com/science/article/pii/S1198743X15003250 Neglected fungal zoonoses: hidden threats to man and animals]. Clinical Microbiology and Infection. 2015 May 1;21(5):416-25. Available from:https://www.sciencedirect.com/science/article/pii/S1198743X15003250 (last accessed 5.3.2020)</ref> | Fungal infections associated with zoonotic transmission are an important public health problem worldwide . A number of these infections are among the group of the most common fungal diseases, such as: dermatophytosis, sporotrichosis , and histoplasmosis.<ref>Seyedmousavi S, Guillot J, Tolooe A, Verweij PE, De Hoog GS. [https://www.sciencedirect.com/science/article/pii/S1198743X15003250 Neglected fungal zoonoses: hidden threats to man and animals]. Clinical Microbiology and Infection. 2015 May 1;21(5):416-25. Available from:https://www.sciencedirect.com/science/article/pii/S1198743X15003250 (last accessed 5.3.2020)</ref> | ||
1.Dermatomycoses | 1.Dermatomycoses - infections of the skin, hair and nails, which are caused in most cases by dermatophytes, and in rarer cases by yeasts and moulds. | ||
Fungal infections of the skin are the most frequently occurring infectious diseases, with a worldwide prevalence of 20% to 25% and high and growing relapse rates. | |||
* Clinical image of dermatomycoses very heterogeneous and cannot always be differentiated from other dermatoses. | |||
* Further, a simultaneous bacterial infection of the damaged skin, pretreatment with corticosteroid-containing preparations or secondary contact allergy hinder identification of dermatomycoses. | |||
* Dermatomycoses must always be treated. | |||
* The choice of antimycotic therapy (therapeutic, duration, dose) depends on the pathogen and on the severity and type of infection, and treatment is either local and/or systemic. | |||
* A fast diagnosis and pathogen typing are for successful therapy of fungal diseases<ref>Euroimmune [https://www.euroimmun.com/products/indications/molekulare-diagnostik/molekulare-infektionsdiagnostik/dermatomycosis.html Dermatomycosis] Available from:https://www.euroimmun.com/products/indications/molekulare-diagnostik/molekulare-infektionsdiagnostik/dermatomycosis.html (last accessed 6.3.2020)</ref> | |||
| [[File:Histoplasmosis.jpg|right|frameless]] | ||
2. Histoplasmosis is a fungal disease associated with bat guano (stool).<ref name="CDC" /> and is a type of lung infection. | |||
* It is caused by inhaling ''Histoplasma capsulatum'' fungal spores. | |||
* These spores are found in soil and in the droppings of bats and birds. | |||
* This fungus mainly grows in the central, southeastern, and mid-Atlantic states. | |||
* Most cases of histoplasmosis don’t require treatment. | |||
* People with weaker immune systems may experience serious problems. | |||
* The disease may progress and spread to other areas of the body. | |||
* Skin lesions have been reported in 10 to 15 percent of cases of histoplasmosis that has spread throughout the body.<ref>Healthline [https://www.healthline.com/health/histoplasmosis Histoplasmosis] Available from:https://www.healthline.com/health/histoplasmosis (last accessed 6.3.2020)</ref> | |||
3. Coccidioidomycosis ( is an infection usually caused by inhaling the spores (“seeds”) of either Coccidioides immitis or Coccidioides posadasii fungi). | |||
* These spores are found in the soil in certain geographic areas (called endemic), and get into the air when the soil is disturbed. | |||
* This can happen with construction, gardening, farming, windy weather, dirt biking or driving all-terrain vehicles (ATV’s) in these areas. | |||
* Coccidioidomycosis cannot be passed from person-to-person. | |||
* The most common states for people to be infected with coccidioidomycosis are Arizona and California, followed by Nevada, New Mexico, Texas, and Utah <ref>American Thoracic Society [https://www.thoracic.org/patients/patient-resources/resources/coccidioidomycosis.pdf Coccidioidomycosos] Available from: https://www.thoracic.org/patients/patient-resources/resources/coccidioidomycosis.pdf (last accessed 6.3.2020)</ref> | |||
| |||
=== Parasitic Zoonoses === | === Parasitic Zoonoses === | ||
==== 3 Common Parasitic Zoonoses ==== | ==== 3 Common Parasitic Zoonoses ==== | ||
1, | 1, Toxocara Canis (Roundworm) | ||
A parasitic disease associated with cats, dogs and their environment.<ref name="CDC" /> | |||
* Toxocara canis is an infection transmitted from animals to humans caused by the parasitic roundworms commonly found in the intestine of dogs (Toxocara canis) and cats (T. cati). | |||
* The most common Toxocara parasite of concern to humans is T. canis, which puppies usually contract from the mother before birth or from her milk. The larvae mature rapidly in the puppy’s intestine; when the pup is 3 or 4 weeks old, they begin to produce large numbers of eggs that contaminate the environment through the animal’s stool. The eggs soon develop into infective larvae. | |||
* Humans can become infected after accidentally ingesting infective Toxocara eggs in soil or other contaminated surfaces. In most cases, | |||
* Toxocara infections are not serious. | |||
* The most severe cases are rare, but are more likely to occur in young children, who often play in dirt, or eat dirt (pica) contaminated by dog or cat stool.<ref name="CDC Toxocariasis">Centers for Disease Control and Prevention. Parasites. Toxocariasis. http://www.cdc.gov/parasites/toxocariasis/gen_info/faqs.html (accessed 8 March 2011).</ref> | |||
2. Hookworm: Ancylostoma caninum is a parasitic disease associated with dogs and their environment.<ref name="CDC" /> | |||
* Animals can indirectly pass hookworm to humans. Animals that are infected pass hookworm eggs in their stools. | |||
* The eggs can hatch into larvae, and both eggs and larvae may be found in dirt where animals have been and can get into the human body through direct contact with the dirt.eg if a child is walking barefoot or playing in an area where dogs or cats have been. | |||
* If a person contracts animal hookworm eggs, the larvae that hatch out of the eggs reaching the intestine and cause bleeding, inflammation (swelling), and abdominal pain. | |||
* People can get painful and itchy skin infections when animal hookworm larvae move through their skin.<ref name="CDC Hookworm">Centers for Disease Control and Prevention. Healthy Pets Healthy People. Hookworm Infection and Animals. http://www.cdc.gov/healthypets/diseases/hookworm.htm (accessed 8 March 2011).</ref> | |||
[[File:Tapeworm lifecycle.jpg|right|frameless]] | |||
3. Echinococcosis (tapeworm) | 3. Echinococcosis (tapeworm) | ||
Tapeworms are flat, segmented worms that live in the intestines of some animals. Animals can become infected with these parasites when grazing in pastures or drinking contaminated water. | |||
Eating undercooked meat from infected animals is the main cause of tapeworm infection in people. Although tapeworms in humans usually cause few symptoms and are easily treated, they can sometimes cause serious, life-threatening problems<ref>WebMD [https://www.webmd.com/digestive-disorders/tapeworms-in-humans#1 Tapeworm in humans] Available from:https://www.webmd.com/digestive-disorders/tapeworms-in-humans#1 (last accessed 6.3.2020)</ref> | |||
== References == | == References == | ||
| Line 174: | Line 199: | ||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
[[Category:Communicable Diseases]] | |||
Latest revision as of 09:06, 5 January 2022
Original Editors - Kristy Rizzo from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Kristine Rizzo, Lucinda hampton, Elaine Lonnemann, Admin, Tony Lowe, Kim Jackson, WikiSysop, 127.0.0.1 and Nupur Smit Shah
Introduction[edit | edit source]
A zoonotic disease is any disease or infection that is transmissible from vertebrate animals to humans. [1],[2] Recently emerged zoonotic diseases include globally devastating diseases such as:
- Coronaviruses (CoV), a large family of viruses that cause illness ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS-CoV),Severe Acute Respiratory Syndrome (SARS-CoV) and COVID 19[3]
- Ebola virus disease
- Highly pathogenic avian influenza
- Bovine spongiform encephalopathy [4]
Key Points
- Nearly two-thirds of human infectious diseases arise from pathogens shared with wild or domestic animals
- Endemic and enzootic zoonoses cause about a billion cases of illness in people and millions of deaths every year, and emerging zoonoses are a rising threat to global health, having caused hundreds of billions of US dollars of economic damage in the past 20 years
- Ecological and evolutionary perspectives can provide valuable insights into pathogen ecology and can inform zoonotic disease-control programmes
- Anthropogenic practices (ie those caused by humans or their practices) eg. changes in land use, animal production systems, and widespread antimicrobial applications, affect zoonotic disease transmission
- Risks are to all countries; as global trade and travel expands, zoonoses are increasingly posing health concerns for the global medical community
- Multisectoral collaboration, including clinicians, public health scientists, ecologists and disease ecologists, veterinarians, economists, and others is necessary for effective management of the causes and prevention of zoonotic diseases[5]
How do Zoonoses spread[edit | edit source]
Because of the close connection between people and animals, it’s important to be aware of the common ways people can get infected with germs that can cause zoonotic diseases. These can include:
- Direct contact: Coming into contact with the saliva, blood, urine, mucous, feces, or other body fluids of an infected animal. Examples include petting or touching animals, and bites or scratches.
- Indirect contact: Coming into contact with areas where animals live and roam, or objects or surfaces that have been contaminated with germs. Examples include aquarium tank water, pet habitats, chicken coops, barns, plants, and soil, as well as pet food and water dishes.
- Vector-borne: Being bitten by a tick, or an insect like a mosquito or a flea.
- Foodborne: Each year, 1 in 6 Americans get sick from eating contaminated food. Eating or drinking something unsafe, such as unpasteurized (raw) milk, undercooked meat or eggs, or raw fruits and vegetables that are contaminated with feces from an infected animal. Contaminated food can cause illness in people and animals, including pets.
- Waterborne: Drinking or coming in contact with water that has been contaminated with feces from an infected animal.[6]
Approaches for Zoonotic Disease Control[edit | edit source]
Mitigating the impact of endemic and emerging zoonotic diseases of public health importance requires multisectoral collaboration and interdisciplinary partnerships. Collaborations across sectors relevant to zoonotic diseases, particularly among human and animal (domestic and wildlife) health disciplines, are essential for quantifying the burden of zoonotic diseases, detecting and responding to endemic and emerging zoonotic pathogens, prioritizing the diseases of greatest public health concern, and effectively launching appropriate prevention, detection, and response strategies.
These structures must be in place before an outbreak, epidemic, or pandemic occurs to have an effective, coordinated public- and animal-health response. Countries that lack a well-functioning coordination mechanism could fail to rapidly detect and effectively respond to emerging health threats, which could spread to other countries and threaten global health security.[4]
Prevention[edit | edit source]
On a personal level
The best way to protect oneself from many of these zoonotic diseases is to practice good hygiene after handling animals or their waste. Washing hands thoroughly with hot, soapy water after any contact will help prevention contraction of zoonotic diseases.[2] In addition screening newly received animals, conducting a routine sanitization of the contaminated environment, equipment, and caging, wearing gloves and protective clothing will help decrease the possiblity of contracting a zoonotic disease.[7]
The four principal means of preventing spread of zoonoses are[1]
1. parasite recognition and control
2. vaccination programs
3. sanitation methods
4. behavior training to prevent bites and scratches
On a world wide level
Preventing zoonotic diseases requires coordinated actions by government authorities responsible for human and animal health.
- The prevention and control of zoonotic diseases impose a unique, often heavy burden on public health services, particularly in resource-limited settings.
- Because zoonotic diseases can deeply affect animals and humans, for many zoonotic infections, medical and veterinary health agencies have a large stake in disease surveillance and control activities.
- Collaboration between agencies is pivotal but takes time, requiring dedicated planning and well-exercised coordination of activities. Achieving this level of collaboration can be daunting in many real-world situations where resource disparities, differences in institutional culture and priorities, disparate legal authorizations, and many other factors can impede development of the formal structures needed to ensure effective implementation of disease prevention and control programs.
- Field observations and anecdotal reports suggest ongoing risks to human health, to the preservation of wildlife, and, in many cases, to livestock production—the last of which can compound human hardships by negatively affecting livelihoods—in the absence of formal structures that enable intersectoral collaboration.[8]
Classes of Zoonoses[edit | edit source]
Including viruses, bacteria, parasites, and fungi.
Viral Zoonoses - 6 Common Viral Zoonoses[edit | edit source]
- Coronaviruses (CoV) are a large family of viruses that cause illness ranging from the common cold
- 3 strains of corana virus are Middle East Respiratory Syndrome (MERS-CoV), Severe Acute Respiratory Syndrome (SARS-CoV, Covid19 - a new strain that has not been previously identified in humans.
- Detailed investigations found that SARS-CoV was transmitted from civet cats to humans and MERS-CoV from dromedary camels to humans.
- Several known coronaviruses are circulating in animals that have not yet infected humans.
2. Ehrlichiosis - Ehrlichiosis is the general name used to describe diseases caused by the bacteria Ehrlichia chaffeensis, E. ewingii, or E. muris eauclairensis in the United States. These bacteria are spread to people primarily through the bite of infected ticks including the lone star tick (Amblyomma americanum) and the blacklegged tick (Ixodes scapularis).
People with ehrlichiosis will often have fever, chills, headache, muscle aches, and sometimes upset stomach. Doxycycline is the treatment of choice for adults and children of all ages with ehrlichiosis.[9]
3. Rocky Mountain Spotted Fever (Rickettsia ) Rocky Mountain Spotted Fever is a tick borne disease, due to an intracellular pathogen known as Rickettsia rickettsi
4. Rabies - Rabies is an infectious, zoonotic disease that destroys brain cells and can lead to death if left untreated before symptoms appear. It is caused by a virus that lives in the saliva of a host or carrier and can be transmitted by being bitten by the carrier or if the infected saliva enters an open wound or mucous membranes. Rabies has been reported as being transmitted to people after breathing in air from caves that contained millions of bats and through organ transplants from an infected person. The most common sources of infections for humans are from wild animals and dogs.[10]
5. West Nile Virus - West Nile virus (WNV) is the leading cause of mosquito-borne disease in the continental United States.
- It is most commonly spread to people by the bite of an infected mosquito.
- Cases of WNV occur during mosquito season, which starts in the summer and continues through fall.
- There are no vaccines to prevent or medications to treat WNV in people.
- Fortunately, most people infected with WNV do not feel sick.
- About 1 in 5 people who are infected develop a fever and other symptoms.
- About 1 out of 150 infected people develop a serious, sometimes fatal, illness.
- You can reduce your risk of WNV by using insect repellent and wearing long-sleeved shirts and long pants to prevent mosquito bites.[11]
6. Equine Encephalitis - A mosquito borne infection normally maintained in nature by a cycle from an arthropod vector to a vertebrate reservoir host.[1]
- Some people experience it only as a mild illness for others it is fatal (fatal in about one-third of the cases).
- Symptoms of eastern equine encephalitis usually appear three to 10 days after a bite by an infected mosquito.[12]
- No vaccine exists for humans.[1]
- Personal protective measures are the primary way to avoid contracting the virus.[1]
Bacterial Zoonoses - 10 Common Bacterial Zoonoses[edit | edit source]
- Anthrax
Anthrax is an acute infectious disease caused by the spore-forming bacterium Bacillus anthracis[13], a microbe that lives in the soil.[14]
- A serious infectious disease caused by gram-positive, rod-shaped bacteria known as Bacillus anthracis.
- Anthrax can be found naturally in soil and commonly affects domestic and wild animals around the world.
- Rare in the United States - people can get sick with anthrax if they come in contact with infected animals or contaminated animal products.
- Contact with anthrax can cause severe illness in both humans and animals.
- Anthrax is not contagious, which means you can’t catch it like the cold or flu.
- Anthrax can occur in three forms: cutaneous, inhalation, and gastrointestinal.[13][14]
2. Bartonella (Cat Scratch Fever) - bacterial disease caused by Bartonella henselae.
- Most people with CSD have been bitten or scratched by a cat and developed a mild infection at the point of injury.
- Lymph nodes, especially those around the head, neck, and upper limbs, become swollen.
- Person with CSD may experience fever, headache, fatigue, and a poor appetite.[15]
- Bartonella will begin in the human as a pustule that will gradually progress to regional lymphadenopathy which can last for months (or become a systemic illness in immunocompromised patients).
- Can also be transmitted through the feces of fleas.[1]
- Lyme disease or Lyme borreliosis is the most commonly transmitted tick-borne infection in the United States and among the most frequently diagnosed tick-borne infections worldwide[16].
4. Brucellosis
Brucellosis is a bacterial infection that spreads from animals to people.
- Most commonly, people are infected by eating raw or unpasteurized dairy products. Sometimes, the bacteria that cause brucellosis can spread through the air or through direct contact with infected animals.
- Signs and symptoms of brucellosis may include fever, joint pain and fatigue. The infection can usually be treated with antibiotics. However, treatment takes several weeks to months, and the infection can recur.
- Brucellosis affects hundreds of thousands of people and animals worldwide. Avoiding raw dairy products and taking precautions when working with animals or in a laboratory can help prevent brucellosis.[17]
5. Ehrlichiosis
The general name used to describe several bacterial diseases that affect animals and humans.
- Human ehrlichiosis is a disease caused by at least three different ehrlichial species in the United States.
- Ehrlichiae are transmitted to humans by the bite of an infected tick.
- Symptoms usually occur within 1-2 weeks following a tick bite[18][19] and include fever, headache, fatigue, and muscle aches.
- Ehrlichios is is diagnosed based on symptoms, clinical presentation, and later confirmed with specialized laboratory tests.
- Treatment for adults and children of all ages is doxycycline.[18]
- A bacterial disease that affects humans & animals.
- Caused by the bacteria genus Leptospira.
- Spread through urine of infected animals, which can get into water or soil and can survive for weeks to months.
- Most common method of transmission is through direct contact with infected urine or other bodily fluids such as saliva, or contaminated water, soil, or food.[20]
7. Plague (Yersinia enterocolitica, Yersinia pestis)
Plague is a zoonotic infection that has affected humans for thousands of years. In humans, the primary plague syndromes are bubonic, septicemic, and pneumonic. All of these result from infection with the gram-negative bacillus Yersinia pestis. The typical life-cycle of Y. Pestis starts within an insect vector followed by transmission to a mammalian host, typically rodents or other wild animals. Humans are only affected as incidental hosts. Despite this, Y. pestis is arguably one of the most important microbes in human history. It has caused three documented pandemics, with the “black death” in 14th century Europe leading to the death of up to 30% of the population. The most recent pandemic began in the late 19th century in Asia and India, and it continues today in Africa. Outside of this, the bacterium remains endemic in the Americas and Asia and also exists as a potential bioterrorism threat, spurring ongoing vaccine development
8. Rickettsia (Rocky Mountain Spotted Fever)
- A disease caused by the bacterium Rickettsia rickettsii, which is carried by ticks.
- People usually start having fevers and feeling nauseous about a week after being bitten by a tick.
- A few days after the fever begins people will often have a rash, usually on the arms or ankles. They also may have pain in their joints, stomach pain, and diarrhea.[15]
- When you remove ticks from any animal, the crushed tick or its parts can also pass this disease through any cuts or scrapes on your skin.[15]
9. Methicillin Resistant Staphylococcus Aureus (MRSA)
Methicillin-Resistant Staphylococcus Aureus (MRSA) is defined as a type of bacterial staph infection that is non-responsive to antibiotics normally prescribed to treat such infections.[21]
- MRSA was first described in 1961-1962 in a patient whose infection was resistant to the drug Methicillin, which was discovered in 1960.
- The incidence of MRSA greatly increased in the United States in the 1980s and was especially emerging in patients who used intravenous drugs[22].
- The bacteria from which MRSA arises, staphylococcus aureus, is found in the skin and in the nostrils of one third of all people and do not show any symptoms of having been exposed to the bacteria.
- These carriers of the bacteria are then exposing the bacteria to all of the items that they touch as well as expelling it into the air where it will remain until the item is next cleaned.
10. Streptococcus suis is a zoonotic pathogen that infects pigs and can occasionally cause serious infections in humans.
- S. suis infections occur sporadically in humans throughout Europe and North America, but a recent major outbreak has been described in China with high levels of mortality.
- The mechanisms of S. suis pathogenesis in humans and pigs are poorly understood.[23]
Fungal Zoonoses[edit | edit source]
Fungal infections associated with zoonotic transmission are an important public health problem worldwide . A number of these infections are among the group of the most common fungal diseases, such as: dermatophytosis, sporotrichosis , and histoplasmosis.[24]
1.Dermatomycoses - infections of the skin, hair and nails, which are caused in most cases by dermatophytes, and in rarer cases by yeasts and moulds.
Fungal infections of the skin are the most frequently occurring infectious diseases, with a worldwide prevalence of 20% to 25% and high and growing relapse rates.
- Clinical image of dermatomycoses very heterogeneous and cannot always be differentiated from other dermatoses.
- Further, a simultaneous bacterial infection of the damaged skin, pretreatment with corticosteroid-containing preparations or secondary contact allergy hinder identification of dermatomycoses.
- Dermatomycoses must always be treated.
- The choice of antimycotic therapy (therapeutic, duration, dose) depends on the pathogen and on the severity and type of infection, and treatment is either local and/or systemic.
- A fast diagnosis and pathogen typing are for successful therapy of fungal diseases[25]
2. Histoplasmosis is a fungal disease associated with bat guano (stool).[15] and is a type of lung infection.
- It is caused by inhaling Histoplasma capsulatum fungal spores.
- These spores are found in soil and in the droppings of bats and birds.
- This fungus mainly grows in the central, southeastern, and mid-Atlantic states.
- Most cases of histoplasmosis don’t require treatment.
- People with weaker immune systems may experience serious problems.
- The disease may progress and spread to other areas of the body.
- Skin lesions have been reported in 10 to 15 percent of cases of histoplasmosis that has spread throughout the body.[26]
3. Coccidioidomycosis ( is an infection usually caused by inhaling the spores (“seeds”) of either Coccidioides immitis or Coccidioides posadasii fungi).
- These spores are found in the soil in certain geographic areas (called endemic), and get into the air when the soil is disturbed.
- This can happen with construction, gardening, farming, windy weather, dirt biking or driving all-terrain vehicles (ATV’s) in these areas.
- Coccidioidomycosis cannot be passed from person-to-person.
- The most common states for people to be infected with coccidioidomycosis are Arizona and California, followed by Nevada, New Mexico, Texas, and Utah [27]
Parasitic Zoonoses[edit | edit source]
3 Common Parasitic Zoonoses[edit | edit source]
1, Toxocara Canis (Roundworm)
A parasitic disease associated with cats, dogs and their environment.[15]
- Toxocara canis is an infection transmitted from animals to humans caused by the parasitic roundworms commonly found in the intestine of dogs (Toxocara canis) and cats (T. cati).
- The most common Toxocara parasite of concern to humans is T. canis, which puppies usually contract from the mother before birth or from her milk. The larvae mature rapidly in the puppy’s intestine; when the pup is 3 or 4 weeks old, they begin to produce large numbers of eggs that contaminate the environment through the animal’s stool. The eggs soon develop into infective larvae.
- Humans can become infected after accidentally ingesting infective Toxocara eggs in soil or other contaminated surfaces. In most cases,
- Toxocara infections are not serious.
- The most severe cases are rare, but are more likely to occur in young children, who often play in dirt, or eat dirt (pica) contaminated by dog or cat stool.[28]
2. Hookworm: Ancylostoma caninum is a parasitic disease associated with dogs and their environment.[15]
- Animals can indirectly pass hookworm to humans. Animals that are infected pass hookworm eggs in their stools.
- The eggs can hatch into larvae, and both eggs and larvae may be found in dirt where animals have been and can get into the human body through direct contact with the dirt.eg if a child is walking barefoot or playing in an area where dogs or cats have been.
- If a person contracts animal hookworm eggs, the larvae that hatch out of the eggs reaching the intestine and cause bleeding, inflammation (swelling), and abdominal pain.
- People can get painful and itchy skin infections when animal hookworm larvae move through their skin.[29]
3. Echinococcosis (tapeworm)
Tapeworms are flat, segmented worms that live in the intestines of some animals. Animals can become infected with these parasites when grazing in pastures or drinking contaminated water.
Eating undercooked meat from infected animals is the main cause of tapeworm infection in people. Although tapeworms in humans usually cause few symptoms and are easily treated, they can sometimes cause serious, life-threatening problems[30]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Van Dyke JB. Veterinary zoonoses, what you need to know before you treat that puppy! American Physical Therapy Association Combined Sections Meeting; 2011 Feb 11; New Orleans, Louisianna.
- ↑ 2.0 2.1 Oregon Veterinary Medical Association. Zoonotic Diseases and Horses.fckLRhttp://oregonvma.org/care-health/zoonotic-diseases-horses. (accessed 8 March 2011).
- ↑ WHO Corona virus Available from:https://www.who.int/health-topics/coronavirus (last accessed 5.3.2020)
- ↑ 4.0 4.1 Belay ED, Kile JC, Hall AJ, Barton-Behravesh C, Parsons MB, Salyer S, Walke H. Zoonotic disease programs for enhancing global health security. Emerging infectious diseases. 2017 Dec;23(Suppl 1):S65. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5711319/ (last accessed 5.3.2020)
- ↑ Karesh WB, Dobson A, Lloyd-Smith JO, Lubroth J, Dixon MA, Bennett M, Aldrich S, Harrington T, Formenty P, Loh EH, Machalaba CC. Ecology of zoonoses: natural and unnatural histories. The Lancet. 2012 Dec 1;380(9857):1936-45. Available from:https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(12)61678-X/fulltext (last accessed 5.3.2020)
- ↑ CDC Zoonotic diseases Available from:https://www.cdc.gov/onehealth/basics/zoonotic-diseases.html (last accessed 5.3.2020)
- ↑ Iowa State University. Institutional Biosafety Committee. Guidance & Education. Zoonotic Disease Fact Sheets: dermatomycoses. http://compliance.iastate.edu/ibc/guide/zoonoticfactsheets/Dermatomycoses.pdf (accessed 8 March 2011).
- ↑ Shiferaw ML, Doty JB, Maghlakelidze G, Morgan J, Khmaladze E, Parkadze O, Donduashvili M, Wemakoy EO, Muyembe JJ, Mulumba L, Malekani J. Frameworks for preventing, detecting, and controlling zoonotic diseases. Emerging Infectious Diseases. 2017 Dec;23(Suppl 1):S71. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5711328 / (last accessed 6.3.30)
- ↑ CDC Ehrlichiolis Available from:https://www.cdc.gov/ehrlichiosis/ (last accessed 6.3.2020)
- ↑ RABIES. (n.d.), [cited March 17, 2011]; Available from: Funk & Wagnalls New World Encyclopedia
- ↑ CDC West Nile Virus Available from:https://www.cdc.gov/westnile/index.html (last accessed 6.3.2020)
- ↑ Mayo Foundation for Medical Education and Research. Encephalitis. http://www.mayoclinic.com/health/encephalitis/DS00226/DSECTION=causes (accessed 27 Feb 2011).
- ↑ 13.0 13.1 Centers for Disease Control and Prevention. Emergency Preparedness and Response. Questions and Answers about Anthrax. http://www.bt.cdc.gov/agent/anthrax/faq/ (accessed 2 March 2011)
- ↑ 14.0 14.1 U.S. National Library of Medicine. National Institute of Health. Medline Plus. Anthrax.http://www.nlm.nih.gov/medlineplus/anthrax.html (accessed 2 March 2011).
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 Centers for Disease Control and Prevention. Healthy Pets Healthy People. http://www.cdc.gov/healthypets/browse_by_diseases.htm (accessed 26 Feb 2011).
- ↑ Skar GL, Simonsen KA. Lyme Disease. InStatPearls [Internet] 2018 Oct 27. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431066/ (last accessed 26.12.2019)
- ↑ Mayo Clinic Brucellosis Available from:https://www.mayoclinic.org/diseases-conditions/brucellosis/symptoms-causes/syc-20351738 (last accessed 6.3.2020)
- ↑ 18.0 18.1 Centers for Disease Control and Prevention. Ehrlichiosis. http://www.cdc.gov/ehrlichiosis/ (accessed 27 Feb 2011).
- ↑ Mayo Foundation for Medical Education and Research. Ehrlichiosis. http://www.mayoclinic.com/health/ehrlichiosis/DS00702 (accessed 27 Feb 2011).
- ↑ World Health Organization [Internet]. [Place unknown]: WHO; Prepared for World Day 2001 [ cited 2016 March 31]. Available from: http://www.who.int/water_sanitation_health/diseases/leptospirosis/en/
- ↑ Mayo Clinic Staff. MRSA infection - Mayo Clinic [Internet]. Mayoclinic.org. 2016.http://www.mayoclinic.org/diseases-conditions/mrsa/basics/definition/con-20024479 (accessed 1 April 2016).
- ↑ Millar B, Loughrey A, Elborn J, Moore J. Proposed definitions of community-associated meticillin-resistant Staphylococcus aureus (CA-MRSA). Journal of Hospital Infection. 2007;67(2):109-113. http://eds.b.ebscohost.com.libproxy.bellarmine.edu/ehost/detail/detail?vid=14&sid=71ee6b7e-199d-4adc-8e31-bc94eca59a09%40sessionmgr113&hid=112&bdata=JmxvZ2luLmFzcCZzaXRlPWVob3N0LWxpdmUmc2NvcGU9c2l0ZQ%3d%3d#AN=105828672&db=cin20 (accessed 2 April 2016).
- ↑ Holden et al. Rapid evolution of virulence and drug resistance in the emerging zoonotic pathogen streptococcus suis. PLoS One. 2009; 4(7). e6072. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2705793/(accessed 8 March 2011).
- ↑ Seyedmousavi S, Guillot J, Tolooe A, Verweij PE, De Hoog GS. Neglected fungal zoonoses: hidden threats to man and animals. Clinical Microbiology and Infection. 2015 May 1;21(5):416-25. Available from:https://www.sciencedirect.com/science/article/pii/S1198743X15003250 (last accessed 5.3.2020)
- ↑ Euroimmune Dermatomycosis Available from:https://www.euroimmun.com/products/indications/molekulare-diagnostik/molekulare-infektionsdiagnostik/dermatomycosis.html (last accessed 6.3.2020)
- ↑ Healthline Histoplasmosis Available from:https://www.healthline.com/health/histoplasmosis (last accessed 6.3.2020)
- ↑ American Thoracic Society Coccidioidomycosos Available from: https://www.thoracic.org/patients/patient-resources/resources/coccidioidomycosis.pdf (last accessed 6.3.2020)
- ↑ Centers for Disease Control and Prevention. Parasites. Toxocariasis. http://www.cdc.gov/parasites/toxocariasis/gen_info/faqs.html (accessed 8 March 2011).
- ↑ Centers for Disease Control and Prevention. Healthy Pets Healthy People. Hookworm Infection and Animals. http://www.cdc.gov/healthypets/diseases/hookworm.htm (accessed 8 March 2011).
- ↑ WebMD Tapeworm in humans Available from:https://www.webmd.com/digestive-disorders/tapeworms-in-humans#1 (last accessed 6.3.2020)