Central Pontine Myelinolysis
Original Editor - Wendy Walker
Top Contributors - Wendy Walker, Laura Ritchie, Kim Jackson, Lucinda hampton, WikiSysop, Admin, Naomi O'Reilly and Aminat Abolade
Introduction[edit | edit source]
Central pontine myelinolysis (CPM) [now termed osmotic demyelination syndrome (ODS)], characterized by damage to regions of the brain (most commonly pontine white matter tracts) after rapid correction of metabolic disturbances such as hyponatremia (low amounts of sodium in the blood)
- Central pontine myelinolysis (CPM) was first described in 1959 by Adams and his colleagues in a report of four patients with pseudobulbar palsy and quadriplegia.
- The initial cases were seen in patients with alcohol use disorder and malnutrition.
- Subsequent cases showed a link with rapid sodium correction.
- CPM has since been reported in cases of severe burns, liver transplantation, anorexia nervosa and hyperemesis gravidarum, and hyperglycemic states.
- Clinical features of CPM typically begin to appear within several days after rapid correction of hyponatremia. Clinical manifestations vary and can range from encephalopathy to coma and death.[1]
Mechanism of Injury / Pathological Process[edit | edit source]
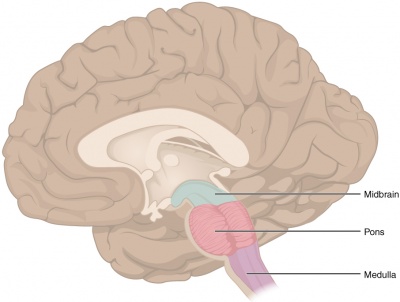
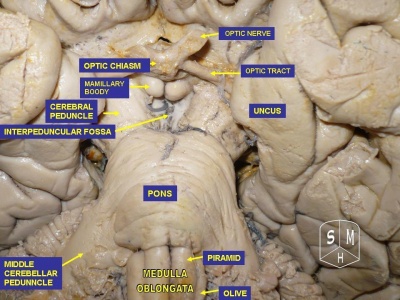
Central pontine myelinolysis is a concentrated, frequently symmetric, noninflammatory demyelination within the pons. The area involved is usually confined to the basal part of the pons but occasionally involves the tegmentum also
The Pons is situated in the brainstem. It lies above the medulla, below the midbrain and anterior to the cerebellum.
It is one of the demyelinating conditions and was first described by Adams et al in 1959.[2] In at least 10% of patients with central pontine myelinolysis, demyelination also occurs in extrapontine regions, including the mid brain, thalamus, basal nuclei and cerebellum. The exact mechanism that strips the myelin sheath is unknown.
Central pontine myelinolysis occurs most often as a complication of treatment of patients with profound, life-threatening hyponatremia (low sodium) and is a consequence of a rapid rise in serum tonicity following treatment in individuals with chronic, severe hyponatremia who have made intracellular adaptations to the prevailing hypotonicity.
In some cases, demyelination occurs outside the pons too; cases which include extrapontine demyelination are labelled "osmotic demyelination syndrome", "extra pontine myelinolysis" or "osmotic myelinolysis".[3]
Microscopically the lesion shows degeneration and loss of oligodendrocytes with preservation of axons unless the lesion is very advanced.
Clinical Presentation[edit | edit source]
Patients more susceptible to CPM include those with a history of
- Malnutrition,
- Alcohol use disorder
- Chronic liver disease
- Hyperemesis gravidarum.
Patients most commonly have a history of rapid sodium correction, greater than 0.5-1.0 mEq/L per hour. The most susceptible patients are those with chronic hyponatremia (>48 hours) or those with severe hyponatremia (Na <120 mEq/L).
The onset of symptoms is usually seen 1 to 14 days after electrolyte correction.
- Clinical features of central pontine myelinolysis reflect damage to upper motor neurons and generally present in a biphasic course.
- Initially, patients present with acute encephalopathy and seizures that typically resolve as normal sodium levels are restored.
- This is later followed by clinical deterioration 3-5 days later.
- Signs and symptoms include dysphagia, dysarthria, spastic quadriparesis, pseudobulbar paralysis, ataxia, lethargy, tremors, dizziness, catatonia, and in the most severe cases, locked-in-syndrome and coma.[5]
Causes[edit | edit source]
Conditions predisposing patients to central pontine myelinolysis include alcoholism, liver disease, malnutrition and hyponatremia (an electrolyte disturbance in which the sodium ion concentration in the plasma is lower than normal).
CPM may occur following liver transplantation surgery.
Burn patients may develop CPM and it can also occur with Wilson disease and neoplasia.
Diagnostic Procedures[edit | edit source]
- Clinical assessment with review of labs with particular attention to the rate of sodium correction is essential in the evaluation and diagnosis of CPM.
- Imaging is not required but can be used to confirm the diagnosis, especially if the diagnosis is uncertain.
- MRI is the most useful imaging technique in these cases. T2-weighted MRI images demonstrate hyperintense or bright areas where demyelination has occurred and has been caused by relatively increased water content in those regions[6].
Management / Prognosis[edit | edit source]
Patients who survive central pontine myelinolysis likely require extensive and prolonged neurorehabilitation. Incorporate occupational, physical, speech, and language therapists early in the care of such patients. Swallowing studies are necessary to evaluate for dysphagia and determine the risk for aspiration pneumonia.
Central pontine myelinolysis was once thought to be fatal, with a mortality of 90% to 100% (possibly because it was initially diagnosed at autopsy). The mortality rate has significantly decreased, with recent retrospective studies showing 94% survival (about 25%-40% make a complete recovery without deficits, and 25%-30% remain incapacitated). [5]
Differential Diagnosis[edit | edit source]
- Demyelination, including multiple sclerosis (MS)
- Infarction from basilar perforators can be central, although more often brainstem infarcts stop at the midline
- Pontine neoplasms including astrocytomas
- hypertensive encephalopathy
- CNS lymphoma
- Acute autoimmune or infectious encephalitis
- Mitochondrial encephalopathies
- CNS vasculitis[5]
Teamwork[edit | edit source]
- The management of central pontine myelinolysis is challenging and requires the coordination of physicians and ancillary staff to have positive outcomes.
- The critical component is the prevention of the condition, which is structured around close monitoring of serum sodium levels.
- Patients being monitored should be under close surveillance in the appropriate setting, such as the intensive care unit.
- Serum sodium levels should be monitored every 4-6 hours, or hourly if there are severe derangements.
- Providers should be aware of this devastating complication.[5]
References[edit | edit source]
- ↑ Danyalian A, Heller D. Central Pontine Myelinolysis. InStatPearls [Internet] 2019 Dec 11. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK551697/ (last accessed 9.2.2020)
- ↑ Adams RD, VICTOR M, MANCALL EL. Central pontine myelinolysis: a hitherto undescribed disease occurring in alcoholic and malnourished patients. AMA Archives of Neurology & Psychiatry. 1959 Feb 1;81(2):154-72.
- ↑ Martin RJ. Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes. Journal of Neurology, Neurosurgery & Psychiatry. 2004 Sep 1;75(suppl 3):iii22-8.
- ↑ Dr A Fazakas Hyponatremia: Osmotic demyelination syndrome Available from: https://www.youtube.com/watch?v=jeF3qw1Z_3E&feature=youtu.be (last accessed 10.2.2020)
- ↑ 5.0 5.1 5.2 5.3 Danyalian A, Heller D. Central Pontine Myelinolysis. InStatPearls [Internet] 2019 Dec 11. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK551697/ (last accessed 10.2.2020)
- ↑ DeWitt LD, Buonanno FS, Kistler JP, Zeffiro T, DeLaPaz RL, Brady TJ, Rosen BR, Pykett IL. Central pontine myelinolysis: demonstration by nuclear magnetic resonance. Neurology. 1984 May 1;34(5):570-.