Spasticity
Original Editor - Timothy Assi
Top Contributors - Naomi O'Reilly, Sheik Abdul Khadir, Matt Ross, Rhiannon Clement, Kim Jackson, Lucinda hampton, Evan Thomas, Admin, Scott Buxton, Vidya Acharya, Timothy Assi, Garima Gedamkar, Lauren Heydenrych, Oyemi Sillo, George Prudden, WikiSysop, Rachael Lowe, Rania Nasr, Tony Lowe, Shreya Pavaskar, Wendy Walker and Ewa Jaraczewska
Introduction[edit | edit source]
Lesions to the central nervous system (brain or spinal cord) can lead to both positive and/ or negative upper motor neurone syndrome (UMNS) features:
| Positive Component | Negative Component |
|---|---|
| Exaggerated Tendon Reflexes | Spastic Co-Contractions |
| Released Reflexes | Motor Weakness |
| Babinski Sign | Slowed Movements |
| Increased Tone | Loss of Dexterity |
| Clonus | Loss of Selective Motor Control |
| Spastic Dystonia |
Spasticity is seen to be a positive feature of upper motor neuron syndrome. This is because it is due to a loss of inhibition of the lower motor neuron pathways, rather than a loss of connection to the lower motor neuron (or other pathways). This results from disordered sensorimotor control of movement due to a lesion of the upper motor neuron which regulate muscle control. Therefore, there is an imbalance of the signals between the central nervous system (CNS) and muscles, presenting as intermittent or sustained involuntary activation of muscles.
All muscles have some tone to maintain function, for example, activation of antigravity muscles to maintain sitting or standing postures. In an individual with spasticity, there is a velocity-dependent increase in muscle tone to passive movement[1]. This creates an inability to stretch muscles or coordinate movements effectively.
This inhibition can result from central nervous system pathology, such as:
- Cerebral Palsy
- Multiple Sclerosis
- Motor neurone disease
- Stroke
- Hypoxic Brain Injury
- Traumatic Brain Injury
- Parkinson's Disease
- Spinal cord injury
- Spinal cord compression
- Metastesis / tumour
Spasticity can have an impact on an individual's function, affecting upper and lower limbs, as well as trunk. If this is not managed effectively, it can lead to fixed deformity contractures[2] [3](changes to soft tissue), which affect skin care, comfort and hygiene, as well as complications for daily tasks.
The management of spasticity needs to be carefully considered as some patients rely on aspects of spasticity to allow them to maintain enough tone for functions such as standing or walking. Physiotherapy management may include facilitating individuals to utilise this to maintain weight bearing and ambulation to decrease their risk of developing osteoporosis, strengthen muscles, help improve circulation and promote overall mental health[4].
Definition[edit | edit source]
The most well-known and referenced description of spasticity is the physiological definition proposed by Lance in 1980. [5]
'Spasticity is a motor disorder characterised by a velocity-dependent increase in tonic stretch reflexes (muscle tone) with exaggerated tendon jerks, resulting from hyperexcitability of the stretch reflex, as one component of the upper motor neurone syndrome'
More recently, a definition from Pandyan et al (2005) [6] states that spasticity is:
'Disordered sensorimotor control, resulting, resulting from an upper motor neuron lesion (UMN), presenting as an intermittent or sustained involuntary activations of muscles [7]
Classification of Spasticity into various components of spasticity into sub-definitions:[9][10]
- Intrinsic Tonic Spasticity: Exaggeration of the tonic component of the stretch reflex (manifesting as increased tone),
- Intrinsic Phasic Spasticity: Exaggeration of the phasic component of the stretch reflex (manifesting as tendon hyper-reflexia and clonus), and
- Extrinsic Spasticity: Exaggeration of extrinsic flexion or extension spinal reflexes.
Epidemiology[edit | edit source]
Spasticity affects approximately:
- 35% of those with stroke,
- more than 90% with CP
- about 50% of TBI patients
- 40% of SCI patients
- between 37% and 78% of MS patients.[4]
Anatomy and Etiology[edit | edit source]
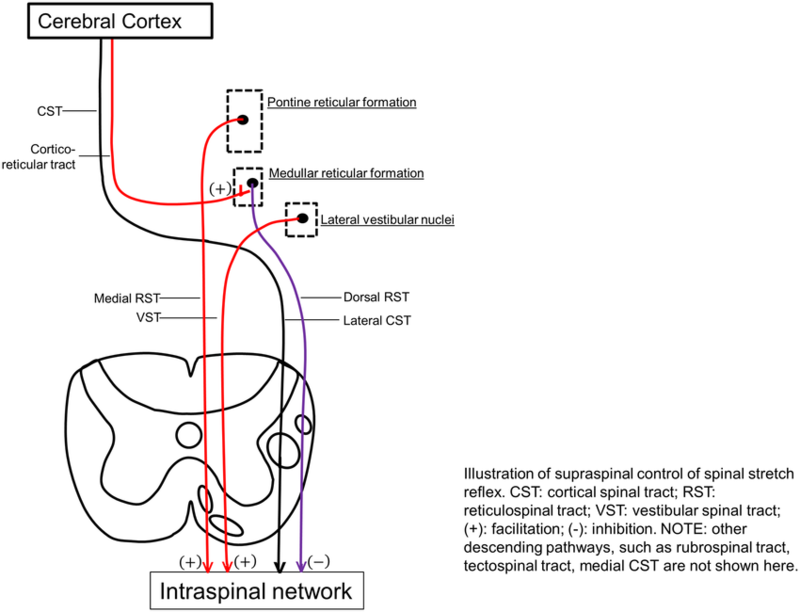
A UMN injury leads to loss of inhibition downstream and hypersensitivity of the reflex arc within the spinal cord.[4] Primary impairments from an upper motor neuron lesion (UMNL) are usually due to the disruption of supraspinal control of descending pathways that control excitatory and inhibitory influences on proprioceptive, cutaneous and nociceptive spinal reflexes.
The Inhibitory System[edit | edit source]
Corticoreticular Spinal Tract: These tracts travel with, but are separate from, the Corticospinal Tract, and are responsible for the facilitation of the inhibitory area within the medulla called the ventromedial reticular formation. Here, the Dorsal Reticulospinal Tract originates, which is responsible for an inhibitory action on both the stretch and flexor reflexes.
The Excitatory System[edit | edit source]
The bulbopontine tegmentum gives rise to the Medial Reticulospinal Tract and, acting weakly with the Vestibulospinal Tract, is excitatory to both stretch and extensor reflexes and like the Dorsal Reticulospinal Tract, is also inhibitory to the flexor reflexes.
Different Lesions and Their Presentations[edit | edit source]
The signs and symptoms between Cortical UMN Lesions and Spinal Cord UMN Lesions vary due to the location of where the disruption has taken place. [11]
Normal[edit | edit source]
Both the inhibitory system (Corticospinal Tract and Dorsoreticulospinal Tract) and excitatory systems (Medial Reticulospinal and Vestibulospinal Tract) are in dynamic balance and therefore the inhibition to the spinal cord is easily adjusted according to demand.
Corticospinal Tract Lesion[edit | edit source]
Although the Corticospinal Tract has an inhibitory influence on stretch and flexor reflex, the main inhibitory system produced by the Dorsal Reticulospinal Tract remains intact and therefore the balance of excitatory and inhibitory influences are maintained.
Internal Capsule Lesion[edit | edit source]
Leads to interruption of both the Corticospinal Tract and Corticoreticular Tract pathways that are responsible for the inhibitory response and some loss of inhibition to stretch and flexor stretches. The excitatory systems from both the Medial Reticulospinal and Vestibulospinal Tract are more dominant which leads to the facilitation of extensor and stretch reflexes but inhibition of flexors.
Incomplete Spinal Cord Lesion[edit | edit source]
Signs and symptoms will vary dependant on site and extent. If the inhibitory system is affected then there will be an unopposed excitatory drive to stretch and extensor reflexes with partial inhibition of flexor reflexes.
Complete Spinal Cord Lesion[edit | edit source]
Spinal reflexes are unopposed due to the complete loss of supraspinal control. Both flexor and extensor reflexes are disinhibited and therefore people may experience both flexor and extensor spasms.
Clinical Presentation[edit | edit source]
On physical exam, hallmark findings include
- high muscle tone in muscle groups such as the shoulder adductors; elbow, wrist, and finger flexors; and forearm pronators. In the lower extremities, the increased tone is especially prominent in the hip adductors, knee flexors and extensors, and plantar flexors and invertors of the ankle. Antigravity muscles are predominantly affected.
- Patients may report difficulty with footwear if their spasticity involves constant, high tone of the extensor hallucis longus or long toe flexors.
- Spasticity varies with speed of movement (velocity dependent); meaning the faster the muscle is moved or stretched, the greater the resistance to stretch or passive elongation is felt.
- Clonus, spastic co-contractions, and spastic dystonia may be evident. i.e., Clonus is defined as an alternating muscle contraction and relaxation of the agonist and antagonist muscles. Spastic co-contractions are abnormal antagonist contractions that present during voluntary agonist effort. Spastic dystonia is a muscle contraction that is present at rest, leading to a constant clinical posture that is highly sensitive to stretch.[4]
- Clasp knife phenomenon: Limb initially resists movement and then suddenly gives way
- Stroking Effect: Stroking the surface of the antagonist muscle may reduce tone in spasticity.
Permanent loss of joint range has been known to occur 3-6 weeks after both stroke and brain injury and therefore it is important that spasticity is identified early on in the assessment in order for it to be monitored and managed as required. In a person with hemiplegia the lower limb pattern is plantar flexion and inversion of the ankle with hamstring tightness limiting knee range of motion as well as adductor spasticity. Upper limb presentation is usually shoulder adduction, internal rotation, elbow flexion, forearm pronation with wrist and elbow flexion. [2][3]
Outcome measures[13][edit | edit source]
Useful objective measures to monitor changes in spasticity can include:
Subjective:
- Pain:
- Numeric Pain Scale (e.g. for pain, comfort, stiffness)
- Observing grimacing / pulling away
- Arm A and Arm B
- LegA
Objective:
- Resting Position: photographs, description, measuring bony landmarks
- Passive range of movement
- Adductor Tone Rating[14]
- Active range of movement
- Muscle strength: Oxford Scale
- Spasms:
- Function
- Walking: 10m times walk
- Transfers: Times up and go
- Upper Limb Function: 9 hole peg test
- Speech: Speech comprehension score [17]
- Walking and Falls Score
- Muscle tone: Ashworth Scale / Modified Ashworth Scale, Tardieu (outlined below)
Ashworth Scale[edit | edit source]
The Ashworth scale is the most widely used assessment tool to measure resistance to limb movement in a clinic setting, although it is unable to distinguish between the neural and non-neural components of increased tone.[18]
The scale is as follows:
| Ashworth Scale | |
|---|---|
| Grade | Description |
| 0 | No increase in muscle tone |
| 1 | Slight increase in tone giving a catch when the limb is moved |
| 2 | More marked increase in tone but limb easily moved |
| 3 | Considerable increase in tone - passive movement difficult |
| 4 | Limb is rigid in flexion or extension |
Modified Ashworth Scale[edit | edit source]
Modified Ashworth Scale' scores exhibited better reliability when measuring upper extremities than lower[19]. The scale is as below:
| Modified Ashworth Scale | |
|---|---|
| Grade | Description |
| 0 | No increase in muscle tone |
| 1 | Slight increase in muscle tone, manifested by a catch and release or by minimal resistance at the end of the range of motion when the affected part(s) is moved in flexion or extension |
| 1
+ |
Slight increase in muscle tone, manifested by a catch, followed by minimal resistance throughout the remainder (less than half) of the ROM |
| 2 | More marked increase in muscle tone through most of the ROM, but affected part(s) easily moved |
| 3 | Considerable increase in muscle tone, passive movement difficult |
| 4 | Affected part(s) rigid in flexion or extension |
Tardieu Scale[edit | edit source]
This scale quantifies muscle spasticity by assessing the response of the muscle to stretch applied at specified velocities. Grading is always performed at the same time of day, in a constant position of the body for a given limb. For each muscle group, reaction to stretch is rated at a specified stretch velocity. [20]
| Tardieu | |
|---|---|
| Velocity to Stretch | |
| V1 | As slow as possible |
| V2 | Speed of the limb segment falling (with gravitational pull) |
| V3 | At a fast rate (>gravitational pull) |
| Quality of Muscle Reaction | |
| 0 | No resistance throughout passive movement |
| 1 | Slight resistance throughout,with no clear catch at a precise angle. |
| 2 | Clear catch at a precise angle followed by release |
| 3 | Fatiguable Clonus (< 10 secs) occurring at a precise angleFatiguable Clonus (< 10 secs) occurring at a precise angle |
| 4 | Unfatiguable Clonus (> 10 secs) occurring at a precise angle |
| 5 | Joint immobile |
| Spasticity Angle | |
| R1 | Angle of catch seen at Velocity V2 or V3 |
| R2 | Full range of motion achieved when muscle is at rest and tested at V1 velocity |
Management[edit | edit source]
It important to consider the triggers of spasticity when planning interventions. There are a number of stimuli which can exacerbate spasticity, some may need multidisciplinary input alongside implementing physiotherapy management[2]. These include:
- Skin: pressure ulcers, ingrown toe nails
- Bladder or bowel: constipation, full bladder
- Pain / discomfort: restrictive clothing, wheelchair straps, catheter straps
- Seating / positioning
- Fatigue
- Infections: UTI, pneumonia, skin
- Stress
- Disease progression
- Menstruation
- Other medical conditions (e.g. kidney stones)
- Ill fitting Introduction to Orthotics
Physiotherapy[edit | edit source]
Spasticity is one of the components of the UMN syndrome but should not be considered in isolation when it comes to management strategies. It is essential that management targets identified impairments to function and is always patient focused rather than aimed at reducing the degree of spasticity[22] Planned interventions should consider a balance between movement and positioning [13]. This includes:
- Standing
- Standing frame
- Treadmill training (body-weight supported if needed)
- Tilt table
- Active exercises
- Passive movements
- Functional electrical stimulation
- 24 hour positioning management
- Splinting and the use of Introduction to Orthotics
- Stretches
Considerations for managing spasticity [23]:
- Client care:
- Preventing or treating contractures
- Monitoring skin to preventing pressure areas
- Positioning of trunk, head and limbs in supine and in chair/ wheel chair
- If possible, standing promotes anti-gravity muscle activity in the trunk and lower limbs. It also maintains or improves soft tissue and joint flexibility and modulation of the neural component of spasticity.
- Introduction to Orthotics to maintain / improve available range
- Movement improvement:
- The unmasking of voluntary movements previously covered by significant spasticity in cases of incomplete lesions
- Accelerating the “spontaneous” recovery process
- Modifying the “immature” motor pattern
- Using new recovery techniques to promote guided neuroplasticity, e.g. robotic rehabilitation
- New functional pattern in moving and walking.
- ADL's and transfers
- Getting around
- Putting on clothes
- Personal hygiene
- Driving, etc.
- Occupation
- Quality of life
- Independent living
- social and professional reintegration[23]
- Task specific activities can have a positive psychological effect
The informative video below outlines some basic treatment strategies ( MS specifically, but can be extrapolated).
Patients should be educated on maintaining a daily stretching and range of motion program. In addition to the patient, the family and caregivers should be educated about proper positioning, daily skin inspection, an adequate and regular bowel/bladder regimen, avoiding noxious stimuli, and identifying signs of infection and pain.[4]
Pharmacological[edit | edit source]
Some individuals may benefit from medications to manage spasticity. These can be generalised, focal or intrathecal interventions.
If the spasticity is widespread then systemic medication is used. This includes:
- Dantrolene (Dantrium)
- Baclofen (Lioresal and others)
- Tizanidine (Zanaflex)
- Diazepam (Vallium)
- Benzodiazepines
- Gabapentin
- Pregabalin
- Canabinoids
If the spasticity is locallised then local medication is used. This includes:
- Botulinum Toxin (Botox)
- Regional Nerve Block
Intrathecal medications can also be used. These include:
- Baclofen
- Phenol
| Medication | ||
|---|---|---|
| Baclofen | The most common systemic agent. Baclofen acts on the receptors of excitatory nerve terminals, in particular the 'GABA B G-Protein receptor. Once the baclofen has attached to this G-Protein on the pre-synaptic terminal, potassium channels open while calcium channels close, hyperpolarising the cell. The inability for calcium to enter the cell means the release of glutamate, an excitatory neurotransmitter, is prohibited. | |
| Tizanidine | Follows the same mechanism as Baclofen, however attaches to the a2 adrenoreceptor on the pre-synaptic cell membrane. | |
| Botulinum Toxin (Botox) | Injected locally into muscle. Prevents the excytotic release of acetylcholine at the level of the neuromuscular junction which further prevents release of calcium from the sarcoplasmic reticulum which leads to excitation-contraction coupling. | |
| Diazepam (Vallium) | Less common. Increases the effect of GABA, an inhibitory neurotransmitter, that is released from inhibitory interneurons which decreases the excitability within the post-synaptic nerve terminal. | |
| Dantrolene | Provided orally. Blocks the release of calcium from the sarcoplasmic reticulum within the muscle which prevents excitation-contraction coupling. | |
Considerations of medication:
- Optimise timings of sessions alongside medications
- Exposing weakness in limbs of trunk
- Monitor effects and when dose may need adjusting
- Side effects, such as fatigue
The Evidence for Interventions[edit | edit source]
- Progressive Resistance Strength Training - No evidence shows that strength training increases spasticity in patients with stroke. Musculoskeletal impairment are significantly reduced after resistance strength training. [25]
- Biofeedback combined with functional electrical stimulation and occupational therapy does not increase the degree of spasticity after treatment. It also showed a greater reduction in spasticity compared to patients who performed functional electrical stimulation and occupational therapy alone. [26]
- Nabiximols (a specific Cannabis extract ) effectiveness in MS-related spasticity combined with a PT program may improve overall response to the reduction in spasticity.[27].
- Shock wave therapy on flexor hypertonic muscles of the forearm and interosseus muscles of the hand in patients with stroke showed significant reduction of muscle tone (>3months). [28]
- Amelio reported significant reduction of muscle tone (>12 weeks) of plantar flexors in children with cerebral palsy. [29]
- Significant reduction of ankle plantar flexor spasticity in patients with stroke after fifteen 10-minute sessions of continuous ultrasound therapy over a 5-week period (frequency 1MHz and intensity 1,5 W/cm2). [30][31]
- Cryotherapy, using cold packs (12°C) for 20-minutes, can lower the muscle temperature to reduce the spasticity. [32]
- Electric Stimulation using agonist stimulation showed a significant improvement in Ashworth Scores, while antagonist stimulation showed an increase of stretch reflex-initiating angle. [33]
- A scoping review (March 2020) summarises management strategies: medication, physical therapy, and other physical rehabilitative strategies, with surgical management techniques used for treating and preventing spasticity after traumatic brain injury in children[34].
- A Systematic Review and Meta-Analysis[35] evaluating the literature about the safety and efficacy of constraint-induced movement therapy combined with Botox in stroke patients with upper limb spasticity shows that the combination of constraint-induced movement therapy and Botox is promising for improving motor function recovery and ADLs; however, long-term, multicenter rigorously designed RCTs with a good sample size are needed to demonstrate the effectiveness of the combination over conventional therapy for improving post-stroke spasticity.
Clinical Guidelines[edit | edit source]
The Royal College of Physicians (RCP) latest clinical guidelines in 2016 recommend the following for the management of spasticity: [36]
- People with motor weakness after stroke should be assessed for spasticity as a cause of pain, as a factor limiting activities or care, and as a risk factor for the development of contractures.
- People with stroke should be supported to set and monitor specific goals for interventions for spasticity using appropriate clinical measures for ease of care, pain and/or range of movement.
- People with spasticity after stroke should be monitored to determine the extent of the problem and the effect of simple measures to reduce spasticity e.g. positioning, passive movement, active movement (with monitoring of the range of movement and alteration in function) and/or pain control.
- People with persistent or progressive focal spasticity after stroke affecting one or two areas for whom a therapeutic goal can be identified (e.g. ease of care, pain) should be offered intramuscular botulinum toxin. This should be within a specialist multidisciplinary team and be accompanied by rehabilitation therapy and/or splinting or casting for up to 12 weeks after the injections. Goal attainment should be assessed 3-4 months after the injections and further treatment planned according to response.
- People with generalised or diffuse spasticity after stroke should be offered treatment with skeletal muscle relaxants (e.g. baclofen, tizanidine) and monitored for adverse effects, in particular sedation and increased weakness. Combinations of antispasticity drugs should only be initiated by healthcare professionals with specific expertise in managing spasticity.
- People with stroke should only receive intrathecal baclofen, intraneural phenol or similar interventions in the context of a specialist multidisciplinary spasticity service.
- People with stroke with increased tone that is reducing passive or active movement around a joint should have the range of passive joint movement assessed. They should only be offered splinting or casting following individualised assessment and with monitoring by appropriately skilled staff.
- People with stroke should not be routinely offered splinting for the arm and hand.
Resources[edit | edit source]
References[edit | edit source]
- ↑ Bhimani R, Anderson L. Clinical understanding of spasticity: implications for practice. Rehabilitation research and practice. 2014;2014. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4168242/ (last accessed 14.10.2019)
- ↑ 2.0 2.1 2.2 Kheder, A. and Nair, K.P.S., 2012. Spasticity: pathophysiology, evaluation and management. Practical neurology, 12(5), pp.289-298.
- ↑ 3.0 3.1 Graham, L.A., 2013. Management of spasticity revisited. Age and ageing, 42(4), pp.435-441.
- ↑ 4.0 4.1 4.2 4.3 4.4 Rivelis Y, Morice K. Spasticity. InStatPearls [Internet] 2019 Mar 6. StatPearls Publishing.Available from: https://www.ncbi.nlm.nih.gov/books/NBK507869/ (last accessed 8.1.20)
- ↑ Lance JW. Symposium synopsis. In: Feldman RG,fckLRYoung RR, Koella WP (eds). Spasticity: Disordered Motor Control. Chicago, IL: Year Book 1980:485–94.
- ↑ Pandyan AD, Gregoric M, Barnes MP et al. Spasticity: clinical perceptions, neurological realities and meaningful measurement. Disabil Rehabil 2005;27:2–6.
- ↑ Lance JW. The control of muscle tone, reflexes, and movement: Robert Wartenberg Lecture. Neurology. 1980;30(12): 1303-13.
- ↑ National stroke association Spasticity Informational Video Available from: https://www.youtube.com/watch?v=TFmSM7SoXDg (last accessed 14.10.2019)
- ↑ Adams MM, Hicks AL. Spasticity after spinal cord injury. Spinal cord. 2005 Oct;43(10):577-86.
- ↑ Oo, Win Min. (2015). Spasticity.
- ↑ Stokes, M. & Stack, E. (2012). Physical Management for Neurological Conditions. 3rd Edition. Elsevier Ltd.
- ↑ Armando Hasudungan. Introduction to Upper and Lower Motor Neuron Lesions. Available from: https://youtu.be/ClXsS7O8seg[last accessed 30/10/18]
- ↑ 13.0 13.1 Valerie L Stevenson, Louise J Lockley and Louise Jarrett, In: Assessment of the individual with spasticity, chapter 2, SPASTICITY MANAGEMENT:A PRACTICAL MULTIDISCIPLINARY GUIDE,Pg-20-21.
- ↑ Snow BJ, Tsui JKC, Bhatt MH et al. Treatment of spasticity with botulinum toxin: a double blind study.Ann Neurol 1990;28:512–15.
- ↑ Penn RD, Savoy SM, Corcos D et al. Intrathecal baclofen for severe spinal spasticity. N Engl J Med 1989;320:1517–21.
- ↑ Smith C, Birnbaum G, Carlter JL et al. Tizanidine treatment of spasticity caused by multiple sclerosis:results of a double-blind, placebo-controlled trial. US Tizanidine Study Group. Neurology 1994;44:S34–42.
- ↑ Wade et al (1987)
- ↑ Ashworth B. Preliminary trial of carisoprodal in multiple sclerosis. Practitioner 1964;192:540–2.
- ↑ Meseguer-Henarejos AB, Sanchez-Meca J, Lopez-Pina JA, Carles-Hernandez R. Inter-and intra-rater reliability of the Modified Ashworth Scale: a systematic review and meta-analysis. European journal of physical and rehabilitation medicine. 2018 Aug;54(4):576-90.
- ↑ Tardieu G, Rondont 0, Mensch J, Dalloz J-C, Monfraix C, Tabary J-C. Responses electromyographiques a l'etirement musculaire chez l'homme normal. Rev Neurol 1957; 97: 60-61.
- ↑ Christchurch Group Managing spasticity following a brain injury Available from: https://www.youtube.com/watch?v=olj6JQ7_ZGs&app=desktop (last accessed 14.10.2019)
- ↑ Thompson AJ, Jarrett L, Lockley L, Marsden J, Stevenson VL. Clinical management of spasticity. Available from: https://jnnp.bmj.com/content/76/4/459 (last accessed 14.10.2019)
- ↑ 23.0 23.1 Petropoulou K. Managing Spasticity with a Focus on Rehabilitation. Available from: https://www.neuromodulation.com/managing-spasticity-with-a-focus-on-rehabilitation (last accessed 14.10.2019)
- ↑ MSgetinvolved Spasticity - Physiotherapy Management Available from: https://www.youtube.com/watch?v=5f0nbadPq8w (last accessed 14.10.2019)
- ↑ Morris SL, Dodd KJ, Morris ME. Outcomes of progressive resistance strength training following stroke: a systematic review. Clin Rehabil. 2004 Feb;18(1):27-39.
- ↑ Lourenção MI, Battistella LR, de Brito CM, Tsukimoto GR, Miyazaki MH. Effect of biofeedback accompanying occupational therapy and functional electrical stimulation in hemiplegic patients. Int J Rehabil Res. 2008 Mar;31(1):33-41
- ↑ Grimaldi, A.E., De Giglio, L., Haggiag, S., Bianco, A., Cortese, A., Crisafulli, S.G., Monteleone, F., Marfia, G., Prosperini, L., Galgani, S. and Mirabella, M., 2019. The influence of physiotherapy intervention on patients with multiple sclerosis–related spasticity treated with nabiximols (THC: CBD oromucosal spray). PloS one, 14(7), p.e0219670. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0219670 (last accessed 14.10.2019)
- ↑ Manganotti P, Amelio E. Long-term effect of shock wave therapy on upper limb hypertonia in patients affected by stroke. Stroke. 2005 Sep;36(9):1967-71. Epub 2005 Aug 18.
- ↑ Amelio E, Manganotti P.Effect of shock wave stimulation on hypertonic plantar flexor muscles in patients with cerebral palsy: a placebo-controlled study. J Rehabil Med. 2010 Apr;42(4):339-43.(B)
- ↑ Ansari NN, Adelmanesh F, Naghdi S, Tabtabaei A.The effect of physiotherapeutic ultrasound on muscle spasticity in patients with hemiplegia: a pilot study. Electromyogr Clin Neurophysiol. 2006 Jul-Aug;46(4):247-52.(B)
- ↑ Ansari NN, Naghdi S, Bagheri H, Ghassabi H. Therapeutic ultrasound in the treatment of ankle plantarflexor spasticity in a unilateral stroke population: a randomized, single-blind, placebo-controlled trial. Electromyogr Clin Neurophysiol. 2007 May-Jun;47(3):137-43. (B)
- ↑ Harlaar J, Ten Kate JJ, Prevo AJ, Vogelaar TW, Lankhorst GJ. The effect of cooling on muscle co-ordination in spasticity: assessment with the repetitive movement test. Disabil Rehabil. 2001 Jul 20;23(11):453-61.
- ↑ Van der Salm A, Veltink PH, Ijzerman MJ, Groothuis-Oudshoorn KC, Nene AV, Hermens HJ. Comparison of electric stimulation methods for reduction of triceps surae spasticity in spinal cord injury. Arch Phys Med Rehabil. 2006 Feb;87(2):222-8.
- ↑ Beynon AM, Hebert JJ, Lebouef-Yde C, Walker BF. Potential risk factors and triggers for back pain in children and young adults. A scoping review, part II: unclear or mixed types of back pain. Chiropractic & manual therapies. 2019 Dec 1;27(1):61.
- ↑ Nasb M, Shah SZ, Chen H, Youssef AS, Li Z, Dayoub L, Noufal A, Allam AE, Hassanien M, El Oumri AA, Chang KV. Constraint-Induced Movement Therapy Combined With Botulinum Toxin for Post-stroke Spasticity: A Systematic Review and Meta-Analysis. Cureus. 2021 Sep;13(9).
- ↑ RCP (2016). National Clinical Guidelines for Stroke. Available at: https://www.strokeaudit.org/Guideline/Full-Guideline.aspx [Accessed 19th June 2018].