Gaming Technology in Neurological Rehabilitation
Introduction[edit | edit source]
The ever increasing population brings with it new challenges for the healthcare system. People are living will illness and disability longer than ever and this places an increasing strain on the healthcare system. In theory by incorporating more telehealth into traditional rehabilitation for individuals with chronic conditions therapists should be able to manage higher caseloads and manage more patients. The use of consoles to supplement therapy is an economically sound means to increase practice opportunities to patients during non-therapy specific time.[1]
Another key element to consider when considering incorporating console based gaming into practice is patient engagement. Research has shown that there is an overall improvement in patient motivation when using consoles and virtual reality for therapy[2]. A study by Deutsch et al found that individuals had an increase in compliance, playfulness, and endurance and were better able to cope with the repetitive nature of rehabilitation.[3][4]
It has been found that consoles are an appropriate means to assist in the ongoing needs of those requiring neurological rehabilitation of all ages.[5][4][3][6][7] By using a console as an adjunct to traditional rehabilitation, patients are able to enhance and self direct the pace of their rehabilitation at home. This is vital for any individual with a neurological condition that must live with long term disability. The rehabilitation process may take months to years before the patient is able to function to their full capacity. Therapy may be necessary for the lifetime of the individual if their condition is chronic.[7][8] With technological and medical advances, individuals who would previously have had a shortened lifespan are surviving longer with a better quality of life.[9][2]
A common issue in rehabilitating neurological conditions is to not only provide sufficient intensity of therapy to regain muscle function and strength of a limb or a joint but also to have transference of skills.[10] A study performed by Deutsch et al.[11] found that the patient population did have some transference of skills when using the Wii as means for rehabilitation. Different games will require different limb activation. Those that require bilateral tasks have been found to improve upper limb function in children with hemiplegic cerebral palsy.[5]It is important that patients not only enjoy partaking in aspects of the rehabilitation process but to also feel they are safe in doing so. Deutsch et al.[3] found that some patient populations require supervision while using the consoles during the rehabilitation process. It was also noted that the patients themselves stated that they felt safe and able to practice within the home setting.
What is a Console-Based Therapy?[edit | edit source]
Console-based therapy is the area of research pertaining to the use of technology within the realm of physiotherapy. Whatever the cause of impairment, the main aim of most neurological rehabilitation is to facilitate learning or relearning of motor skills. The process of gaining motor skills involves repeating the same movement hundreds or even thousands of times. Traditional rehabilitation is time consuming and requires lengthy sessions with therapists that place high demand on personnel and healthcare budgets. Patients often tire of rehabilitation, finding it frustrating or dull. It has been reported that patient adherence to long-term rehabilitation programs involving exercise protocols may be as low as 23% [12].
Integrating console based gaming into rehabilitation protocols has the potential to change the current structure of rehabilitation. Used appropriately game based rehabilitation can be challenging, engaging and fun. No longer is a patient repeatedly flexing and extending their elbow, using a computer game they could be taming a lion, stirring cake batter or shooting multi-coloured balloons. Instead of asking a patient to balance while they reach out and touch a physiotherapy assistant’s hand, patients can work on their balance while playing virtual golf, throwing a strike in the virtual bowling alley or driving a go-kart around a race course on a desert island.
Console based rehabilitation does not seek to replace therapists with computers; rather it is a useful tool that therapists can use to engage with their patients, make rehabilitation fun and exciting, and has the potential to improve compliance rates and thereby improve the functional outcome of these patients.
The need for therapists to integrate games into therapy is further explored in this Ted Talk:
Consoles generally involve:
- A box or equipment which is attached to a television or other medium to transmit information
- May be used with various games both commercially available and rehabilitation specific
- May be deemed a luxurious item or simply one for entertainment only
- Tablets may have a different interface that will require inputs into televisions or other mediums, and have increased portability where the consoles do not
Consoles for Rehabilitation[edit | edit source]
Wii[edit | edit source]
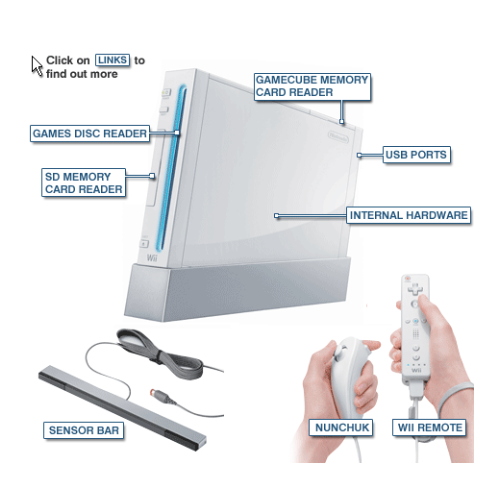
The “Wii” is a computer game console designed to get players moving. The player stands in front of a screen and holds the Wii remote in their hand. A sensor that sits above or below the screen monitors where the player’s hand is (by reading signals sent from the remote in the player’s hand) and translates these signals into movement. It shows the player their progress on the screen.
The Wii was designed for able-bodied users, however Joo et al.[13] found that stroke patients with moderately severe UL impairments could operate the Wii with appropriate strapping and supervision. The therapist may be required to provide encouragement and instructions to compensate for the Wii’s usability limitations.
The role of the Nintendo Wii gaming system has grown in patient rehabilitation since its introduction in November 2006 Henry and Barrett 2010. ‘Wii-habilitation’ incorporates the Wii and its components to help patients fulfil rehabilitation goals. Over 75 million units have been sold worldwide, and it is becoming a popular rehabilitation tool around the world Taylor et al. [14]. Increased use of the Wii for rehabilitation can be attributed to: versatility toward treatment goals, affordability, and increased engagement in therapy.
Nintendo introduced a new style of VR by providing a wireless controller that interacts with the player through a motion detection system. An avatar called Mii[15], (pronounced “me”) represents the player in the game.
Initial interest in the Wii as a therapy tool for upper extremity rehabilitation was due to the console's’ unique wireless controller that allows games to respond to the physical movements of the player, rather than ‘joystick’ movements of traditional gaming systems Halton et al.[16]. Movement is monitored by the components including the Wii remote, “nunchuk”, or balance board.
- Utilises a three-axis accelerometer to translate body movement into onscreen movement.
- Acceleration sensors are responsive to changes in direction, speed, and acceleration that enable participants to interact with games while performing wrist, arm, and hand movements.
- Provides basic audio and visual feedback.
- The nunchuk also incorporates motion-sensing technology and provides additional controls.
The advantages of incorporating the Wii into neurological rehabilitation are plentiful, they include:
- A user friendly interface for both use and set up[17]
- Commercially available system that is safe to use[18]
- A system that does not require a large area allowing patients to use at home[19][20]
- A system that will reduce the number of contact hours promoting patient involvement in rehabilitation[21]
- Attractive graphics with audio feedback creating an enjoyable experience[22]
- Improved compliance and motivation due to entertainment and engaging and nature of games[19][22]
- Positive feedback via awards and badges which are programmed into the games[13]
- Allows patients to socialise with peers and family members thus reduce rates of depression
It is important to note that the Wii may not be suitable for all patient populations some disadvantages include:
- Patients may require assistance and supervision while using the Wii[22].
- Wii-related injuries
- “Wiitus”, acute pain of the supraspinatus[14]
- Hand lacerations were commonly reported
- Wii Tennis was responsible for nearly half (46%) of all injuries reported[14]
- Excessive gameplay may lead to various injuries including musculoskeletal injuries and repetitive strain[14]
- Patients with increased seizure activity may be susceptible to seizure-inducing stimuli[16].
- Patients with pace-makers should keep the Wii remote at least 9 inches away from their chest[16].
What dos the research say:
- Wii games can be feasibly used as an adjunct therapy to conventional therapy[13]
- The Wii cannot replace conventional rehabilitation
- Further research is needed to evaluate if the Wii is independently effective compared to conventional rehabilitation
- Wii games were found to improve UL motor function post-stroke[13][19][23].
Saposnik et al.[24] concluded, when compared to a recreational group therapy (playing cards, bingo, “Jenga”), post-stroke participants showed significant improvement in motor function up to six months post-intervention in the Wii group. A study by McNulty et al.[19] of patients 2-46 months post-stroke found that Wii therapy was as effective as modified constraint-induced movement therapy for improving affected UL movement, and increased independence in activities of daily living. All patients in the Wii therapy group reported increased independence in self-care.
A recent systematic review carried out by Thomson et al.[20] highlights that although there is a trend towards improved UL function and movement, there is insufficient high quality evidence to reach a definitive conclusion about the benefits on activities of daily living or UL function and movement. Larger scale randomised control trials are now needed. There have been no studies showing a negative impact of commercial gaming on therapy. It is therefore likely that the Wii is used complementary to conventional therapy.
A limitation of the Wii technology at present is the fact that it is not sensitive enough to measure some levels of functional ability. One therapist noted: “whether it’s a game for lower functioning individuals…we’re working on just a basic exercise, there need to be maybe 6 different options within that…”[17]. Feedback regarding the:
- Quality of the user’s arm movement
- Parameters including speed and range of motion are not adjustable[25]
- Perceptions that there is a lack of ability to observe and track client progress Tatla et al. study[17]
- Inability to measure change or improvements Tatla et al. study[17]
- The games inability to detect small movements, or muscle activity unlike rehabilitation specific units
- The allowance for ‘cheating’ with compensatory movements
Halton et al.[16] found that the Wii may be too difficult for some patients because it requires a certain level of motor control to progress in the games. A more sensitive system could perhaps overcome these compensatory movements using sensors or vibration to feed back to the patient when they are compensating. However, a limited number of studies have adapted the Wii hardware to turn the Wii into a more useful rehabilitation tool. Matamoros et al. [26] customised the Wii remote and nunchuk so that it could transmit physiological data such as grip strength and finger force while performing therapy. More research is needed in order to design Wii games with a more sensitive rehabilitation focus.
Despite its emerging popularity, current research suggests that the Wii is not a suitable replacement for conventional therapy. Some studies found that Wii practice can lead to benefits on UL function, movement and ADL, but there is insufficient evidence to reach general conclusions. However, commercial gaming can provide high intensity UL practice that is safely tolerated for 180 minutes per week[20]. Stroke rehabilitation is a complex area with gaps in the evidence base on how to promote motor recovery. Some interventions show promise; particularly studies that focus on high-intensity, repetitive task-specific practice[20].
Nintendo Wii encourages high intensity of repetitive arm movements. Over time, patients might find the conventional task-specific exercises monotonous. As discussed earlier, the Wii can potentially motivate patients to spend more time participating in active UL movement because of its fun and interactive approach. Therapists clearly play a key role in selecting and adapting games and activities to meet the needs of patients in the rehabilitation process.
Although the evidence suggests some benefits of using the Wii console in UL rehabilitation, movements by patients playing the Wii are more complex than those in a conventional physiotherapy programme[25]. This can interfere with tailoring a standard treatment plan for a patient because the patient will use different movements with various levels of force.
Further research into the effects and experience of Wii gaming for UL rehabilitation is required, in order to evaluate the efficacy of Wii therapy compared with conventional rehabilitation of the UL. Questions still remain:
- How can we improve the sensitivity of Wii consoles and tailor games to different patient populations?
- How can we improve safety and usability issues for longer-term use at home?
Games[edit | edit source]
Wii Sports - UL Rehab
Nintendo Wii exergames, such as Wii Sports and Wii Fit, are becoming popular in rehabilitation settings. The Wii console’s handheld wireless pointing device has embedded sensors that detect changes in direction and speed in three-dimensions. The games provide immediate audio and visual feedback on progress. The games may be beneficial in:
- Providing encouraging commentaries
- Use of medals and badges
- Allowing bonuses
- Utilising music to aid with improving exercises and repetitively improve performance
- Allow patients to sit or stand while participating
- Providing different levels of difficulty
- Options in the degree in which the limb is used to complete tasks (e.g. swinging a virtual tennis racket or throwing and virtual bowling ball)
Games from the Wii Sports software suitable for UL rehabilitation include:
- Boxing
- Bowling
- Tennis
- Golf
- Baseball
The therapist will pre-select games, taking into consideration an individual’s preferences, and UL functional capacity. Different games or parts of the game will be used for different patients. It is the therapist’s role to monitor for appropriate responses to the game, ensure correct muscles usage, and to be aware of fatigue or pain. The therapist can provide verbal encouragement, support the client’s hand with a cuff to hold the Wii remote if the patient’s grip is inadequate, or even provide hand-over-hand assistance or play with the patient.
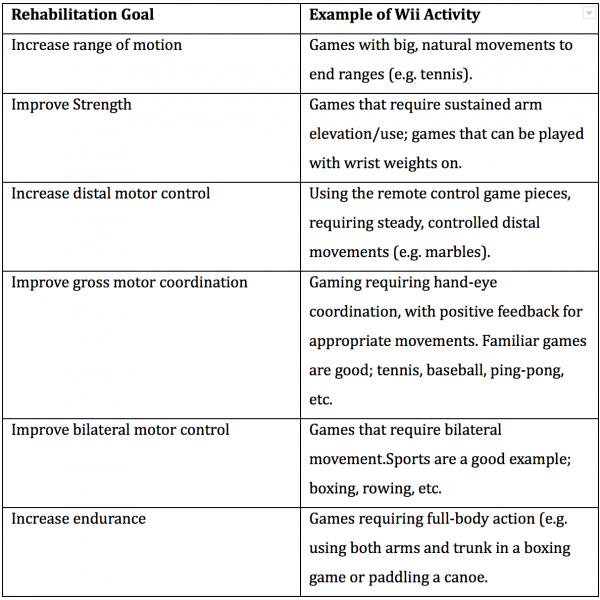
A break-down of how Wii games can be used for specific therapeutic goals [16]
The Wii games described thus far are sold with the Wii console. Although they can be used to assist with rehabilitation goals, Wii games are not designed to do so. Therefore specifically designed games to compliment rehabilitation are needed. Games have been designed for patients with burns, diabetes, asthma, and bladder and bowel dysfunction. Future research should focus on designing more specific games that are suited to the needs of the patient in rehabilitation. The potential of the Wii may improve if games and accessories are designed with rehabilitation in mind.
Kinect[edit | edit source]
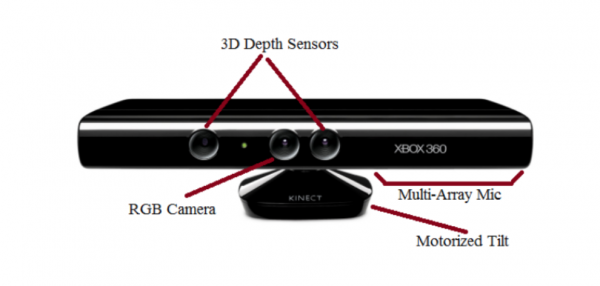
Kinect was released in 2010 and was held as breakthrough in gaming technology. No longer does the player need to hold a remote, instead cameras and motion capture sensors recognise the player and tracks their movement and displays it on the screen.
Kinect began as a revolutionary game platform. It uses an infrared-depth sensing camera [27] manufactured by PrimeSense [28]. The camera captures the users’ full-body movement in 3D space for gaming activities [29]. PrimeSense is used in Microsoft Kinect [28]. Microsoft Kinect sensor can be connected to PC through USB allowing data to be uploaded or downloaded from the server [28].
Kinect enables users to control and interact with the game console by using gestures rather than game controllers [29][30][27], as the Kinect PrimeSense body sensors are not needed as they would in a lab setting [31]. The game 20,000 leaks has the participant use their hands, feet, and head to side step or lunge to plug various leaks that are generated by fish or sharks crashing into a virtual glass bubble [32]. The PrimeSense detects the players’ movements and provides feedback regarding the quality of movement thus determines if the player has succeeded in completing each task.
The PrimeSense utilises a RGB camera and a depth sensor, the combination of these components provide full-body 3D motion capture [29]. The Kinect One is reported to have a 1080p, HD camera that captures video at 30 frames per second [33]. New active-infrared capabilities increase precision, allowing Kinect One to work in various lighting condition with an expanded field of view. Microsoft proprietary ‘Time-of-Flight’ technology measures the time it takes individual photons to rebound off of the player to create unprecedented accuracy and precision. The new noise-isolating multi-microphone array filters ambient sound to recognise natural speaking voices. The camera has greater sensitivity than its predecessors and is able to detect additional data points of articulation including the heartbeat of the player.
Advantages
- Advantages of Kinect include its hands free 3D motion capture capabilities [27]
- Kinect is appropriate for individuals with a wide array of injuries and disorders [30][34][31][35][28][29].
- Patients can complete game-based tasks while standing or seated[35], allowing for greater accessibility to those with disability including wheelchair users[28][34].
- Kinect is commercially available allowing patients to self-manage and complete additional physiotherapy exercises at home.[35][36][28][37][34]
- Current research provides therapists’ with flexibility to prescribe customised rehabilitation programs [32]
- The Kinect will provide feedback on patient performance [27].
- Kinect measures three degrees of freedom of the upper limb, one at the elbow and two at the shoulder[30][37][28].
- The system includes an interactive interface with audio and visual feedback to enhance motivation [31][32][38][30][34], interest, and perseverance to engage in physical activity[35][29].
Disadvantages
- Kinect is unable to discern between supination and pronation of the upper limbs
- Players may not reach a sufficient rate of intensity to acquire sufficient improvements [39].
- The game score is not correspond to motor recovery [36]
- The use of Kinect as an adjunct to traditional physiotherapy may be unknown to health care professionals [32].
Patients have reported Kinect and physiotherapy designed protocols were well accepted, easy to use and safe for use in both home and clinical environments. [31]) No adverse events were reported during testing sessions conducted by Palacios-Navarro et al.[31] who concluding that Kinect games are a safe and feasible means of rehabilitation. VGBT has also been recommended as a complementary strategy to conventional therapy for children with CP[40]. Patents who were recovering from neurological injuries including stroke and spinal cord injuries found using a Kinect prototype to be a valuable rehabilitation tool[28].
When using Kinect in the clinic the rehabilitation area needs to be clear with supervision present. An initial assessment should be conducted within the home environment to ensure the safety of the patient (HCPC Codes of conduct). The PT, carer and pt should review all exercises prior to commencing rehabilitation; the patient should have a carer present when appropriate. There is less risk associated with exercise performed seated when compared to those performed in standing, in populations that have impaired balance and coordination.
The rapidly developing field of VR offers substantial promise in rehabilitation[38]. The VR systems create interactive simulations. MIRA (Medical Interactive Recovery Assistant) has developed software that uses the Kinect interface[27]. Their games aid health care professionals by providing data pertaining to patient performance [29].
Kinect’s validity, reliability, and feasibility have been assessed in Table 3. Kinect is recommended by the current research as an appropriate addition to rehabilitation. Kinect has been found to have acceptable reliability and sensitivity in both recovering and healthy populations [35].
Improvements to neuroplasticity and subsequent recovery of motor function following injury or disease to the nervous system is through intense skillful practice has been observed [35][28]. MRI results indicate activation of the contralateral primary sensorimotor cortex was activated after Kinect-based training in stroke patients [29]. Individuals with access to intensive multidisciplinary rehabilitation programs demonstrate earlier and faster gains on functional independent measures[30]. This would suggest Kinect provides the required intensity needed to investigate neuroplastic changes in sub-acute stroke patients recovering from hemiplegia[29].
Additionally, a large systematic review found the gains from VRBR are attributed to the multisensory feedback provided by the Kinect while influencing motivational aspects of motor performance[38]. Sensory information allows the central nervous system to control body position and orientation allowing adaptations to complex external environments [38]. Effects of VRBR were found to exist at one and three month’s follow-up within the study.
Kinect's low-cost and easy-to-use characteristics make it suitable for the home environment [36][31][40][35][38][37][29]. More research is required as sample sizes were small, some studies did not have control groups while others lacked follow-up.
Due to Kinect’s unique interface, many software companies have been able to develop their own games to target specific clinical outcomes. For this reason, there have been a number of studies conducted without the use of any XBox games. This section will firstly outline some common XBox games used for rehabilitation with the latter section discusses rehabilitation specific software.
Kinect Games[edit | edit source]
Kinect adventure package[32]:
20,000 Leaks:
Player uses arms, legs and head to block leaks in the glass bubble to prevent water from spilling into the bubble. This game requires trunk stability, movement of the upper limbs, lower limbs, trunk and head. The player must make purposeful movements to accurately block the leak.
Space Pop:
The player must side step, squat, flap and raise their arms to move around in outer space. They must hover around to pop bubbles and gain bonuses. The player requires trunk stability and adequate strength in the upper and lower limbs to engaged in hovering. Accuracy of upper limb movement is required as the targets are specific.
Rally Ball:
With the use of the upper limb and head, the player must side step to hit a moving ball that hits a variety of targets. The positioning of the upper limbs is important to hit a specific target. It is equally important to engage the trunk musculature for stabilisation during these movements.
River Rush:
A raft simulation that requires navigation by leaning forward and sideways as well as the use of the upper limbs to target bonuses while on the river. The player engages in jumping and side-stepping to avoid obstacles. Trunk and lower limb stability is required throughout the game. It is also important to have accurate upper limb movement and timing to gain bonuses.
Reflex Ridge:
Player is situated on a rail cart that must avoid obstacles by bending and side-stepping. The upper limbs are used to collect bonuses. Arm movements do not require specific placement as the bonuses are larger scale and easier to obtain.
Kinect Sport Package:
Soccer:
The player must step side to side to act as a defender, kick the ball to act as offense and move side-to-side and lift their arms to act as the goalkeeper.
Volleyball:
For serving, the player must make an upward motion with one arm and a swing motion with the other. The play must also mimic the motions of bumping, setting and spiking the ball.
Bowling:
Requires the player to reach with their left or right arm to grab a ball and then to proceed to swing their arm forward in a bowling action, while maintaining their balance.
Track and Field:
Includes sprinting, javelin, long jump, discus, and hurdles. Players must jog on the spot, jump and use arm movements to throw the discus and javelin.
Boxing:
Player must use both of their arms to punch and block at various heights in response to visual stimuli.
Table Tennis:
Players must reach to their left or right to grab the paddle and swing their arm forward to create topspin, backspin and smash shots. The game also has a “Paddle Panic” setting in which both arms can be used to hit as many balls as possible.
A study by Zoccolillo et al.[40] incorporated the games 20,000 Leaks, Space Pop, and Rally Ball (as well as the boxing, volleyball and bowling games in Kinect Sports package) with the rehabilitation of children with cerebral palsy. They found significant improvements in the quality of movement of the upper limbs, especially for grasping and dissociated movements.
Fruit Ninja
Using the arms as the “blades”, gamers must slice various sized fruit to collect points. This could include shoulder abduction, adduction, flexion, extension, and rotation. The game requires gross dexterity that is timed with the falling fruit. The game’s difficulty increases with more fruit falling at a faster rate. The gamer is positioned at the center of the action, therefore needing to use both arms to slice as many of the fruit falling on either side of them. A study by Bao et al.[29] found that using fruit ninja with patients with subacute stroke for an hour, 5 times a week, improved scores on the Fugl-Meyer Assessment and Wolf Motor Function Test.
DoctorKinetic[41]
Aims to improve range of motion, strength, coordination, activities of daily living, and cognition through enjoyable and engaging games. The games and exercises can be modified to engage the upper limbs, lower limbs, core, and/or back. The therapist is able to prescribe specific exercises to be included in the patient’s program.
The system provides feedback within the game as well as therapist-selected biofeedback. After each session, a report is generated involving gait, balance, range of motion and motor control data. The therapist is able to review the report of the patient’s performance and generates a progress report to detect trends over time.
The system is able to recognise individual patients. This enables the therapist to be in view of the camera without getting included in the virtual reality of the game. This feature also enables quick start up by recognising the patient and bringing up their specifications in the game. This system has implications for neurological musculoskeletal, connective tissue circulatory system, and respiratory system pathologies.
MIRA: Medical Interactive Recovery Assistant [42]
MIRA involves engaging games aimed at rehabilitation of the upper limb. The system originated to help the rehabilitation of orthopaedic impairments and has now branched to involve neurological impairments. Primarily focussed on hemiparesis, tetraparesis, Parkinson’s, dystonia, autism and stroke.
Upper limb movements of the shoulder (flexion, abduction, frontal plane rotation, internal and external rotation, and bilateral arm raises) are used to encourage the player and enable the achievement of treatment goals. These movements involve reflexes, upper limb coordination, flexibility, range of motion, posture, bilateral arm coordination, hand-eye coordination, reaching, and speed constrained movements.
SeeMe Rehab[43]
Aimed to improve coordination, balance, muscle strength, range of motion, reaction times, and memory. The games are easily modified to fit the treatment needs, defined as “deep customisation”. The system generates reports in real time to allow the therapist to analyse compensatory movements, relative angles between limbs, movement times, and range of motions. The reports also allow analysis and quantification of long-term progress.
The developers state their target populations as those who have had a stroke, MS, CP, Parkinson’s disease, extrapyramidal syndromes, brain-tumour operations, spinal cord injury, muscular atrophy and a number of orthopaedic issues. Descriptions of modules are outlined on their website, allowing the therapist to select the appropriate games for their patient’s goals. There is also a real life module that enables the player to undergo activities of daily living in the virtual world. The developers have also introduced a number of games for at home use (with the use of a PC and webcam) that cost under 20 USD.
Jintronix[44]
A system that uses clinically devised exercises to engage patients in their rehabilitation. The system also measures outcomes in real-time and reports it to the clinician. This report enables the therapist to make adjustments to the therapy as well as challenge the patient to improve their scores. Currently, clinician must be monitoring the patient’s participation, not available commercially. The main focus of the system is for the rehabilitation of neurological conditions such as stroke and TBI.
ReflexionHealth- Vera[45]
Is aimed at coaching and motivating patients to perform their exercises. The company is currently focused on musculoskeletal rehabilitation (joint replacement surgery and fall prevention) but has the potential to be used in a broader context, including neurological rehabilitation. Vera has recently received FDA clearance and will be used in a number of clinics as aid to rehabilitation. The system uses an avatar to engage the patient in prescribed exercises at home. The therapist is then able to review the results reported by the system and make adjustments to the program as needed.
KineRehab System
Was developed to assist therapists rehab students in a public school setting. The settings of the game can be adjusted to individualise the game to the student’s rehabilitation needs. The main purpose of the game is to enable students to gauge the accuracy of their movements during rehab. The system provides visual and audio feedback as well as records the student’s progress for the therapist to review. A pilot study[34][30] involving two students with cerebral palsy found an improvement accuracy of upper limb movement. Also, the students reported enjoying the activity and that it promoted better engagement in their therapy regardless of the fact that this is not defined as a “game”.
Virtual Occupational Therapy Assistant (VOTA): [being developed]
VOTA is a virtual reality program that enables participants to practice virtual activities of daily living (ADLs). It incorporates upper limb movements “within integrated, multi-step activities”. The participant manoeuvres around a virtual world and approaches ADLs. The upper limb movement is captured during the execution of the ADLs. This makes it possible to engage both motor and cognitive abilities. The participant is given visual and verbal cues. The system is not recommended for rehabilitating the lower limbs.
A study of hemiparetic stroke patients[46] showed a moderate correlation between the game-embedded assessment of the VOTA system and Wolf Motor Function Test (WMFT) time based assessments. Therefore the VOTA can potentially be used to track the participant's progress.
A randomized controlled clinical trial suggests that virtual reality intervention has positive outcomes on body sway and gross motor function of the children.[47]
Tablets[edit | edit source]
A tablet computer more commonly referred to as a tablet, is a portable computer with a touchscreen display. While a traditional computer will have a separate keyboard, mouse, screen and speakers a tablet combines all of these components into one. The touchscreen display reduces the mouse, and the tablet has a built in camera, speakers and battery.
Despite only being available since 2010, tablets and smart screen technology have had an explosion in popularity and are continuing to grow. The iPad was the first commercially available tablet when it was released in 2010 and since then tablet ownership has steadily grown. The 2015 Ofcom report into the Communications Market reported that 54% of households in the UK now own a tablet. In an audit of current practices in rehabilitation of adults with cervical spine injuries Verdonck and Maye[48] identified the increasingly important role that smartphones and tablets have in activities of daily living and interaction. They recommended that Occupational Therapists integrate smart technology into rehabilitation practices for patients with c-spine injury to allow patient’s greater autonomy.
A tablet is controlled by a touchscreen that reacts to finger movement on the screen. However, it also has a number of other functions that allow the tablet to calculate and react to movement (for example, it can tell if has been placed on it’s side and adjusts the orientation of the screen accordingly). The components of a tablet that allow it to do so include the following:
An Accelerometer: This detects physical movement and orientation of the device. This is used in gaming to allow the user to tilt the device in order to steer a car, for example. A Gyroscope: A gyroscope works alongside the accelerometer to calculate orientation and rotation. A device with both an accelerometer and a gyroscope will have greater accuracy at determining where the player’s hand is. This will therefore allow the tablet to produce a more accurate recording of the work completed. GPS (Global Positioning System): This can tell the user or another person where on the planet the tablet is, accurate to a few meters, providing that the tablet is connected to the internet. This can be useful at measuring distance walked or providing directions to guide a person back home or to the nearest bus stop, hospital or shop. A Camera: This could be used to communicate with the healthcare professional, or to record a patient’s rehab session for playback later.
Advantages
- Tablets are portable and battery operated, which allows the patient to complete their rehabilitation remotely from the clinic. This feature also allows patients to begin using the tablet for rehabilitation in the hospital or clinic and continue the same program after discharge.
- Tablets are relatively cheap. The only piece of hardware needed is the tablet itself, there is no extra equipment needed.
- Anyone can develop a game or app for tablets, and release it on the ‘App Store’ for the iPad or 'Play Store’ for Android devices. When a game is released in these stores, anyone can download and start to use it within a matter of minutes.
- The tablet has a wide range of uses outwit gaming. For instance, if a patient is sent home with a tablet to use for completing their upper limb rehabilitation they could also use the same device to:
- Keep record of their medication
- Remind them when to take their medication,
- Communicate with the department via Skype or e-mail,
- Research their condition
- Join support groups online
- Patients with dysphasia can use the tablet to help them communicate.[49]
- No assistance is required in setting up the tablet; the user can pick up the tablet and start to play immediately. This gives the patient a measure of independence and ownership over their rehab.
- Several of the games described below have a function that allows the therapist to set up an account and monitor their patients’ progress remotely. It can also be used to adjust the difficulty settings of games or to provide feedback or motivation via messages or even short video clips.
Disadvantages
- Compared to the Kinect and Wii the tablet does not have the same level of sensitivity, therefore will not be as good at gathering data on movement
- While the tablet is very good at monitoring fine movement, which is important for improving dexterity at present, it is not useful for rehabilitating gross movements of the upper limb, except as a virtual coach.
- At present the evidence base supporting tablet use in rehabilitation is very limited.
As illustrated by Table 3 the evidence base for tablet-based therapy is still extremely limited. There have been several small scale pilot studies published, however to date no large scale study has evaluated tablet-based rehabilitation, either compared to traditional rehabilitation or other technology. Therefore, we cannot say definitively whether integrating tablet games into neurological rehabilitation would be beneficial. However, several interesting trends emerged:
- All of the studies that looked at patient response reported extremely positive feedback from the patients. Elis et al.[50] reported that patients were highly satisfied with the intervention (rating it 5.6/7 on a Likhert scale). White et al.[49] eported that patients were very satisfied with their tablet based home rehabilitation program, as they felt that their treatment was very modern and cutting-edge.
- Compliance was high across all studies.[51][52][49]
- Participants enjoyed the gaming aspect to their treatment. Hocine et al.[52] reported that participants perceived the sessions to be shorter than they were and one patient likened their game, Prehab to ‘Mario’.
- Age did not appear to influence how participants interacted with the tablet, nor did it appear to influence how participants scored in games. Both Fizzotti et al.[51] and White et al.[49] discussed how elderly patients might be adverse to using a computer or have difficulty adapting to the new technology as a potential barrier to its use. However this was found to be untrue with older participants scoring equally well to younger participants[51] and stroke survivors adapting to the technology well with reassurance and education[49].
The 2013 NICE guidelines[53] /> for rehabilitation after stroke recommend repetitive task training for patients with motor deficits. On rehabilitation wards, physiotherapists often focus on working on gross movements and muscle groups key to maintaining a high a level of function for patients. Dexterity and fine motor skills can often be overlooked.
The inclusion of tablet-based gaming has the potential to help with this. If a ward had several tablets preloaded with several rehabilitation games that patients could use either alone or with assistance from family members, they could safely work on hand movements and dexterity with or without assistance from the healthcare team. The same tablet could in theory also contain information about their condition, advice from members of the healthcare team (in written, audio or video format) and programs that help to combat communication problems post-stroke. The provision of a tablet could also help to bridge the gap between hospital and home, allowing patients to begin therapy in the ward, then take the tablet home and continue the same familiar therapy at home. Patients often feel abandoned and lonely when discharged from hospital and the need to tackle this has been identified. (NICE stroke rehab guidelines). Providing a tablet to improve continuity of care is one possible method that could be used to try and prevent patients from feeling isolated on hospital discharge.
Tablet Games[edit | edit source]
ReHoblet:
An android-based game that utilises an avatar to navigate through a world, defeat enemies and collect bonuses. This game requires gross movements of the upper limb to complete the actions of lifting (up and down) and transporting (left and right). The therapist is able to personalise parameters such as the avatar’s speed, the enemy's’ speed, the size of the world, and the directions that the player will need to move. These modifications allow the therapist to change the game’s difficulty based on the patient’s abilities. For example, increasing the size of the world would require increased magnitude of gross movements. The therapist is also able to log into a web server to track their patient’s data, the game settings, and a list of stats from different sessions (i.e. levels played, scores, the date and time, the number of bonuses counted and the number of enemies hit on different position in the level). This can be used to ensure adherence to the therapy and to quantify where the patient may be struggling.
A pilot study[54] on five MS patients showed good compliance and high enjoyment and engagement with the game.
Ball Strike and Pop Flux:
Ball Strike: an iPad game where the player’s image is projected into the game. The objective of this game is to hit moving colour balls and avoid grey balls. This action engages the trunk, upper limbs, head and shoulders. As the player progresses through the levels of the game, the difficulty increases. The level in which the patient can go to can be manipulated by the therapist.
An iPad game where the player’s image is projected into the game. The player must blow soap bubbles and avoid hitting bombs, rockets, knives etc. This action requires dynamic trunk balance, selectivity, and speed of movement.
A study by Fizzotti et al.[51] on spinal cord injury patients showed significant in game scores and subsequent improvement in Trunk Recovery Scale, which is an indication of trunk control. There was also improved self-reported trunk control and increased satisfaction of treatment.
Fruit Ninja:
Android and iPad based game. Requires goal oriented hand movements to “slice” fruit as it appears on the screen. The player must also avoid missing more than three fruit or slicing a bomb, as this will end the game. Khademi et al.[55] manipulated the game to get rid of the bombs and the three fruit rule and instead use a one-minute time limit. This resulted in a high correlation between the game’s score with Fugl-Meyer Assessment (FMA) and Box-and-Block Test (BBT). Stroke patients were able to increase their scores in the game throughout the study, which resulted in increased FMA and BBT scores.
Dexteria: '
An app that provides therapeutic hand exercises. Dexteria specifically indicates that it is not a game, while their children friendly app “Dexteria Jr.” has games to enable the children to engage in therapeutic hand exercises. The exercises aim to improve strength, control and dexterity in the hands and fingers. Parent’s and therapist are able to track progress with the in-app automatic tracking and reporting feature. Rand et al.[56] found a strong correlation between the Dexteria scores and the Nine Hole Peg Test and with the Box-and-Block Test.
Findex:
Android-based game that uses household and work-related activities to engage the player in finger tapping, dragging and stretching exercises. The aim is to improve finger control, isolation and coordination, and range of motion. The difficulty of the game increases with each level achieved. Carabeo et al.[57] found improved dexterity in a small group of stroke patients. The patients also felt that the game was effective and enjoyed it. It was also reported as being more engaging than standard physiotherapy.
Prehab:
Prehab (or Platform games for Rehabilitation) is a game designed for use on a tablet intended for upper-arm rehabilitation through tasks such as reaching and pointing. The player enters a virtual world where they must collect coins, avoid detection by the enemy and find a gemstone to protect Nature. It has several different settings, for example an underwater environment where the main character is a turtle, a forest and a desert. Each environment is equally challenging, although all of the participants in Hocine et al.[52] study preferred the underwater interface, perceiving it to be easier and more adaptive to the player, which merits further investigation.
Stroke Rehab:
Stroke Rehab was designed by Saposnik et al.[24]. for their ongoing study and is specifically designed for patients with fine motor weakness of the upper limb and/or neglect. It consists of six stages of incremental difficulty and involves moving, popping and stretching balloons that appear on the screen either as stationary items or moving around the screen. [24].
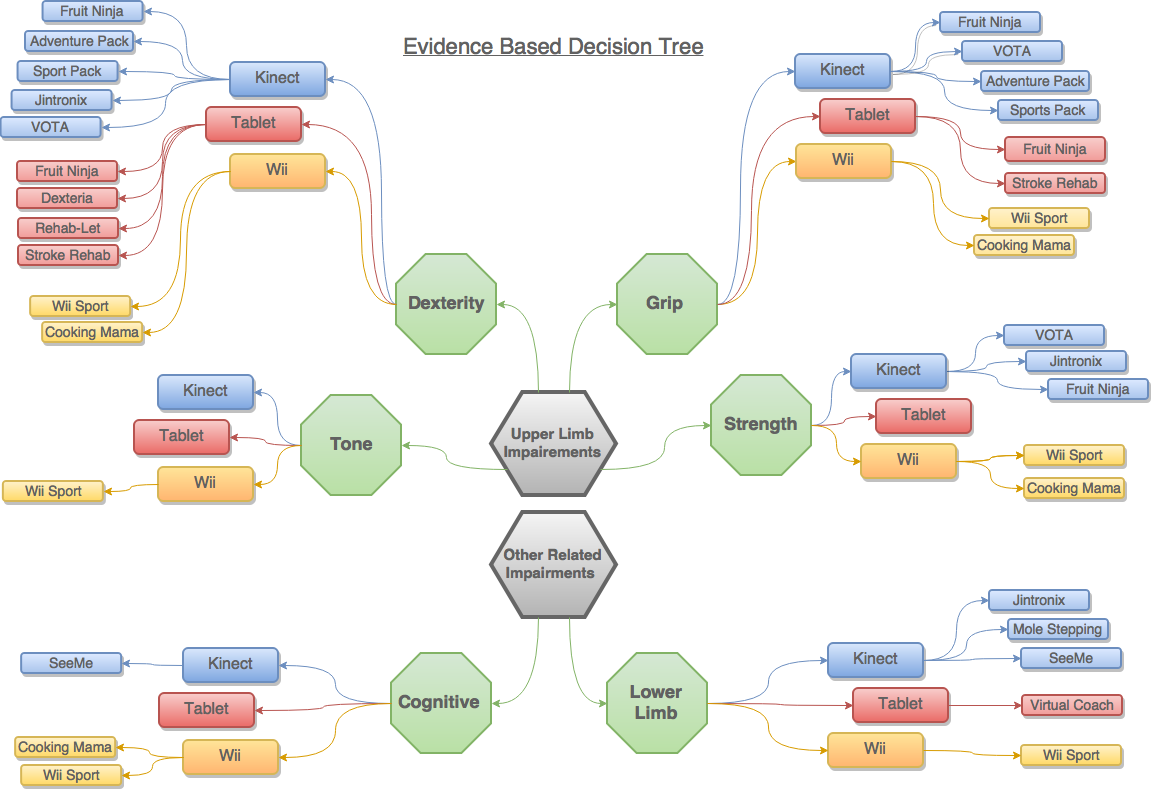
Decision Tree[edit | edit source]
Feeling a bit overwhelmed by all of the information and research? We’ve included a decision tree to help you decide what is best for your patients
This tree strictly includes the games that have reported sufficient research and have demonstrated improvements in their respective impairment. This has no implication on the quality of the games not included in this diagram; the evidence was just not sufficient at the time of the development of this wiki. Please refer back to the “Games” sections to make an informed decision.
The following table outlines the outcome measures used for categorising each subheading in the “Decision Tree”. It also outlines which outcome measures can be used with specific games.
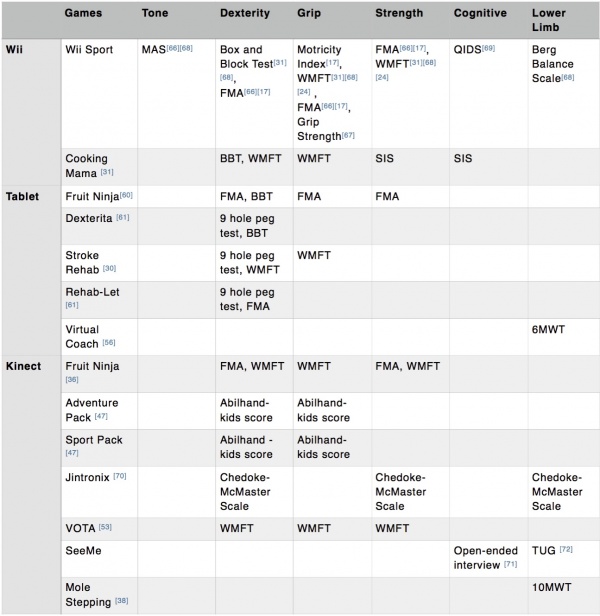
[24][58][13][59][60][19][61][50][56][55][62][63][64]
Conclusions[edit | edit source]
Current research indicates that the use of virtual reality as an adjunct to traditional rehabilitation in neurological patients is promising. Consoles and tablets are commercially available, affordable and safe to use making them a feasible option to supplement rehabilitation of neurological conditions. The variety of games available for the different systems make VR ideal for the vast number of neurological conditions as it will not only cater to specific parts of the body, it is engaging to its audience both young and elderly.
Console based rehabilitation does not seek to replace therapists with computers; rather it is a useful tool that therapists can use as an adjunct to make rehabilitation engaging, thus improving compliance rates to improve the overall functional outcome of patients. The pairing of consoles with traditional therapy is an economically beneficial approach to ensuring optimal rehabilitation of neurological patients. This is particularly important, as neurological pathologies require long periods of rehabilitation with large amounts of repetition. These factors also address barriers including reduced motivation, due to the mundane nature of repetition.
More research is needed in the area of VR in rehabilitation as the data to date consists mainly of small sample groups with a poor use of outcome measures. It would be beneficial to have an increase in longitudinal studies with larger population samples to determine the long-term implications of VR on rehabilitation. Greater use of control groups would also benefit the area, though in some instances there would be ethical considerations to contend with. Additional follow up studies would also improve the robustness of data gathered, providing therapists with a clear picture of the benefits obtained in using VR within the rehabilitation process. More information is needed regarding the optimum prescription in terms of hours per week to reach neuroplasticity. Additionally, there is a lack of data comparing and contrasting the various systems commercially available. There is also a lack of data available pertaining specifically to individuals with disability with few studies discussing how VR may be used with patients that are blind, deaf or wheelchair bound.
The future of rehabilitation is moving toward incorporating VR into therapy. As technology continues to advance, the use of tablets in rehabilitation will grow. This will be ideal due to the portable interactive nature of these devices. Additionally, as the blending of tablets and smartphones continue, individuals everywhere will essentially be able to undergo activities of daily living with a rehabilitation assistant in their pocket.
Studies have examined video gaming as an intervention to various impairments including: balance, mobility, cognition, and upper extremity function. Video game therapy is an emerging area for neurorehabilitation, and recent research has shown that the effectiveness of gaming for upper limb neurological rehabilitation is promising. A systematic review and meta-analysis suggest a positive effect of training with motion-controlled commercial video games on hand and arm function in young people of all ages with cerebral palsy. However, there is a need for high-powered studies on the effectiveness of training with motion-controlled commercial video games for persons with cerebral palsy, especially in adults[65].
References[edit | edit source]
- ↑ Fager SK, Burnfileld, JM. Patients’ experiences with technology during inpatient rehabilitation: opportunities to support independence and therapeutic engagement. Disability and Rehabilitation: Assistive Technology. 2014 9(2):121-127.
- ↑ 2.0 2.1 Fager SK, Burnfileld, JM. Patients’ experiences with technology during inpatient rehabilitation: opportunities to support independence and therapeutic engagement. Disability and Rehabilitation: Assistive Technology. 2014 9(2):121-127.
- ↑ 3.0 3.1 3.2 Deutsch JE, Borbely M, Filler J, Huhn K, Guarrera-Bowlby P. Use of a low-cost, commercially available gaming console (Wii) for rehabilitation of an adolescent with cerebral palsy. Journal of the American Physical Therapy Association. 2008; 88: 1196-1207.
- ↑ 4.0 4.1 Lam MY, Tatla SK, Lohse KR, Shirzad N, Hoens AM, Miller KJ, Holsti L, Virji-Babul N, Van der Loos, M. Perception of technology and its use for therapeutic application for individuals with hemiparesis: findings from adult and pediatric focus groups. JRAT. 2015 2(1):1-13.
- ↑ 5.0 5.1 Brown SH, Lewis CA, McCarthy JM, Doyle ST, Hurvitz. The effects of internet-based home training on upper limb function in adults with cerebral palsy. Neurorehabilitation and Neural Repair. 2010; 24(6):575-583.
- ↑ Fager SK, Burnfileld, JM. Patients’ experiences with technology during inpatient rehabilitation: opportunities to support independence and therapeutic engagement. Disability and Rehabilitation: Assistive Technology. 2014 9(2):121-127.
- ↑ 7.0 7.1 Iosa M, Morone G, Fuso A, Bragoni M, Coiro P, Multiatri M, Venturiero V, De Angelis D, Pratesi L, Paolucci S. Seven capital devices for the future of stroke rehabilitation. Stroke Research and Treatment. 2012. Available from: http://www.hindawi.com/journals/srt/2012/187965/ [Accessed November 4th, 2015]
- ↑ WHO. 2006. Neurological disorders: public health challenge. Available from: http://www.who.int/mental_health/neurology/neurological_disorders_report_web.pdf [Accessed 7th November 2015]
- ↑ WHO. 2006. Neurological disorders: public health challenge. Available from: http://www.who.int/mental_health/neurology/neurological_disorders_report_web.pdf [Accessed 7th November 2015]
- ↑ Iosa M, Morone G, Fuso A, Bragoni M, Coiro P, Multiatri M, Venturiero V, De Angelis D, Pratesi L, Paolucci S. Seven capital devices for the future of stroke rehabilitation. Stroke Research and Treatment. 2012. Available from: http://www.hindawi.com/journals/srt/2012/187965/ [Accessed November 4th, 2015]
- ↑ Deutsch JE, Borbely M, Filler J, Huhn K, Guarrera-Bowlby P. Use of a low-cost, commercially available gaming console (Wii) for rehabilitation of an adolescent with cerebral palsy. Journal of the American Physical Therapy Association. 2008; 88: 1196-1207.
- ↑ Sluijs EM, Kok GJ, van der Zee J. Correlates of exercise compliance in physical therapy. Physical Therapy. 1993; 73 (11):771-786.
- ↑ 13.0 13.1 13.2 13.3 13.4 Joo LY, Yin TS, Xu D, Thia E, Chia PF, Kuah CWK, He KK. A feasibility study using interactive commercial off-the-shelf computer gaming in upper limb rehabilitation in patients after stroke. Journal of Rehabilitation Medicine. 2010; 42:437-441.
- ↑ 14.0 14.1 14.2 14.3 Taylor MJD, McCormick D, Shawis T, Impson R, Griffin M. Activity-promoting gaming systems in exercise and rehabilitation. Journal of Rehabilitation Research and Development. 2011; 48(10):1171-1186.
- ↑ Nintendo News. Mii. 2012. Available from:http://mynintendonews.com/tag/mii/ [Accessed 17th November 2015].
- ↑ 16.0 16.1 16.2 16.3 16.4 Halton J. Rehabilitation with the Nintendo Wii: Experiences at the rehabilitation hospital. Occupational Therapy Now. 2010; 12(3):11-13.
- ↑ 17.0 17.1 17.2 17.3 Tatla S, Shirzad N, Lohse K, Virji-Babul N, Hoens AM, Holsti L, LI L, Miller K, Lam M, Loos M. Therapists’ perceptions of social media and video game technologies in upper limb rehabiltiation. JMIR Serious Games. 2015; 3:1-14.
- ↑ Fung V, So K, Park E. The utility of a video game system in rehabilitation of burn and nonburn patients: a survey among occupational therapy and physiotherapy practitioners. Journal of Burn Care and Research. 2010; 31:768-75.
- ↑ 19.0 19.1 19.2 19.3 19.4 McNulty PA, Thompson-Butel A, Faux SG, Lin G, Katrak PH, Harris L, Ssiner CT. The efficacy of Wii-based movement therapy for upper limb rehabilitation in the chronic poststroke period: a randomised controlled trial. International Journal of Stroke. 2015; 10(8):1253-1260.
- ↑ 20.0 20.1 20.2 20.3 Thomson K, Pollock A, Bugge C, Brady M, Commercial gaming devices for stroke upper limb rehabilitation: a systematic review. International Journal of Stroke. 2014; 9:479-488.
- ↑ Tatla S, Shirzad N, Lohse K, Virji-Babul N, Hoens AM, Holsti L, LI L, Miller K, Lam M, Loos M. Therapists’ perceptions of social media and video game technologies in upper limb rehabiltiation. JMIR Serious Games. 2015; 3:1-14.
- ↑ 22.0 22.1 22.2 Chao YY, Scherer YK, Montgomery CA. Effects of using Nintendo Wii exergames in older adults: a review of the literature. Journal of Aging and Health. 2014; 23:379-402.
- ↑ Saponik G, Chow CM, Gladstone D, Cheung D, Braer E, Thorpe KE, Saldanha A, Dang A, Bayley M, Schweizer TA. iPad technology for home rehabilitation after stroke (iHOME): a proof‐of‐concept randomized trial. International Journal of Stroke. 2014; 9(7):956-962.
- ↑ 24.0 24.1 24.2 24.3 Saposnik G, Teasell R, Hall J, McIlroy W, Cheung D, Thorpe KE, Cohen L, Bayley M. Effectiveness of virtual reality using Wii gaming technology in stroke rehabilitation. Stroke. 2014; 41:1477-1484.
- ↑ 25.0 25.1 Henry A, Barrett A, Wi-habilitation. Royal College of Surgeons in Ireland Student Medical Journal. 2010; 3:70-74.
- ↑ Matamoros M, Negrete M, Leder M. Nintendo Wii remote and nunchuk as a wireless data subsystem for digital acquisition of analog physiological data relevant to motor rehabilitation after stroke. Virtual Rehabilitation International Conference. 2009.
- ↑ 27.0 27.1 27.2 27.3 27.4 Calin A, Cantea A, Dasculu, A, Mihaiu C, Suciu D. MIRA- upper limb rehabilitation system using microsoft kinect. STUDIA UNIV. BABES-BOLYAI . 2011; 56: 63-74. . Available from: http://www.cs.ubbcluj.ro/~studia-i/2011-4/06-Suciu.pdf [Accessed 29th October 2015]
- ↑ 28.0 28.1 28.2 28.3 28.4 28.5 28.6 28.7 28.8 Lange B, Chang C, Suma E, Newman B, Rizzo A, Bolas M. Development and evaluation of low cost game-based balance rehabilitation tool using the Microsoft Kinect sensor. 33rd Annual international conference of IEEE EMBS Online. Boston Massachusetts USA. 2011;1831-1834. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22254685 [Accessed 7th November 2015].
- ↑ 29.0 29.1 29.2 29.3 29.4 29.5 29.6 29.7 29.8 29.9 Bao X, Mao Y, Lin Q, Chen S, LI L, Cates R, Zhou S, Huang D. Mechanism of Kinect-based virtual reality training for motor functional recovery of upper limbs after subacute stroke. Neural regeneration research. 2013; 4:2904-2913 Available: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4146174/ [Accessed 25th September 2015].
- ↑ 30.0 30.1 30.2 30.3 30.4 30.5 Chang Y, Han W, and Tsai Y. A kinect-based upper limb rehabilitation system to assist people with cerebral palsy. Research in Developmental Disabilities. 2013; 34; 3654-3659.
- ↑ 32.0 32.1 32.2 32.3 32.4 Levac, D, Espy D, Fox E, Pradhan S, Deutsch J. Kinect-ing with clinicians: a knowledge translation resource to support decision making about video game use in rehabilitation. Physical Therapy. 2015; 95(3):426-440. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25256741 [Accessed 29th October 2015].
- ↑ Munro D. Microsoft’s new ‘Xbox One’ can measure heart rate. Forbes-Tech. 21st May 2013 Available from: http://www.forbes.com/sites/danmunro/2013/05/21/microsofts-new-xbox-one-can-measure-heart-rate/ [Accessed 16th November 2015].
- ↑ 34.0 34.1 34.2 34.3 34.4 Chang Y, Chen S, Huang J. A kinect-based system for physical rehabilitation: A pilot study for young adults with motor disabilities. Research in Developmental Disabilities. 2011; 32; 2566-2570.http://www.physio-pedia.com/extensions/FCKeditor/plugins/mediawiki/images/tb_icon_ref.gif
- ↑ 35.0 35.1 35.2 35.3 35.4 35.5 35.6 Mobini A, Behzadipour S, Saadat M. Test-retest reliability of kinect’s measurements for the evaluation of upper body recovery of stroke patients. BioMed Central. 2015. 14 . Available from: http://www.biomedical-engineering-online.com/content/14/1/75/ [Accesssed 23rd September 2015].
- ↑ 36.0 36.1 36.2 Pastor I, Hayes H, Bamberg S. A feasibility study of an upper limb rehabilitation system using Kinect and computer games. 34th Annual Conference of the IEEE EMBS Online. 2010; 1286-1289. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23366134 [Accessed 2nd November 2015
- ↑ 37.0 37.1 37.2 Chang C, Lange B, Zhang M, Koenig S, Requejo P, Somboon N, Sawchuk A, Rizzo, A. Towards pervasive physical rehabilitation using Microsoft Kinect. Pervasive computing technologies for healthcare {PervasiveHealth}. 2012; 159-162. Available from: http://ieeexplore.ieee.org/xpl/articleDetails.jsp?reload=true&arnumber=6240377 [Accessed 29th October 2015]
- ↑ 38.0 38.1 38.2 38.3 38.4 Corbetta D, Imeri F, Gatti R. Rehabilitation that incorporates virtual reality is more effective than standard stroke rehabilitation for improving walking speed, balance, and mobility after stroke: a systematic review. Journal of physiotherapy. 2015; 61: 117-124 . Available from: http://www.ncbi.nlm.nih.gov/pubmed/26093805 [Accessed 23rd September 2015]
- ↑ Mellecker R. McManus A. Active video games and physical activity recommendations: a comparison of the gemercize stepper, XBox Kinect, and XaviX J-Mat. Journal of Science and Medicine in Sport. 2014; 17:288-292 . Available from: http://www.ncbi.nlm.nih.gov/pubmed/23777842 [Accessed 7th October 2015]
- ↑ 40.0 40.1 40.2 Zoccolillo L, Morelli D, Cincotti F, Muzzioli L, Gobbetti T, Paolucci S, Iosa M. Video-game based therapy performed by children with cerebral palsy: a cross-over randomized controlled trial and a cross-sectional quantitative measure of physical activity. European Journal of Physical and Rehabilitation Medicine. 2015. Available from: http://www.minervamedica.it/en/journals/europa-medicophysica/article.php?cod=R33Y9999N00A150012 [Accessed 29th October 2015
- ↑ Doctor Kinetic. Doctor Kinetic. Available from: http://doctorkinetic.com [Accessed 8th November 2015].
- ↑ MIRA Rehab Limited. MIRA Rehab. MIRA. Available from: http://www.mirarehab.com [Accessed 8th November 2015].
- ↑ Brontes Processing. SeeMe Rehabilitation. Available from: http://www.virtual-reality-rehabilitation.com/products/seeme/what-is-seeme [Accessed 8th November 2015].
- ↑ Jintronix. Home. Jintronix. Available from: http://www.jintronix.com/ [Accessed 14th November 2015]
- ↑ Reflexion Health. Reflexion Health-Vera. Available from: http://reflexionhealth.com [Acessed 8th November 2015].
- ↑ Adams RJ, Lichter MD, Krepkovich ET, Ellington A, White M, Diamond PT. Assessing upper extremity motor function in practice of virtual activities of daily living. IEEE Transactions on Neural Systems and Rehabilitation Engineering. 2015; 23(2); 287-296.
- ↑ Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Developmental Medicine & Child Neurology. 1997 Apr;39(4):214-23.
- ↑ Verdonck M, Maye F. Enhancing occupational performance in the virtual context using smart technology. British Journal of Occupational Therapy. 2015; 1-6.
- ↑ 49.0 49.1 49.2 49.3 49.4 White J, Janssen H, Jordan L, Pollack M. Tablet technology during stroke recovery: a survivor’s perspective. Disability and Rehabilitation. 2015; 37(13):1186-1192.
- ↑ 50.0 50.1 Ellis T, Latham NK, DeAngelis TR, Thoms CA, Saint-Hilaire M, Bickmore T. Feasibility of a virtual exercise coach to promote walking in community- dwelling persons with Parkinson disease. American Journal of Physical Medicine & Rehabilitation. 2013; 92(6):472-485.
- ↑ 51.0 51.1 51.2 51.3 Fizzotti G, Rognoni C, Imarisoio A, Meneghini A, Pistarini C Quaglini S. Tablet technology for rehabilitation after spinal cord injury: a proof-of-concept. Studies in Health Technology and Informatics. 2014; 210:479-483.
- ↑ 52.0 52.1 52.2 Hocine N, Gouaaich A, Cerri SA, Mottet D, Froger J, Laffont I, Adaptation in serious games for upper-limb rehabilitation: an approach to improve training outcomes. User Modeling and User-Adapted Interaction. 2015; 25(1):65-98.
- ↑ Dworzynski K, Ritchie G, Fenu E, MacDermott K, Playford ED. Rehabilitation after stroke: summary of NICE guidance. Bmj. 2013 Jun 12;346:f3615.
- ↑ Vandermaesen M, Robert K, Luyten K, and Coninx K, 2014. “ReHoblet- a home-based rehabilitation game on the tablet“. IEEE 16th International Conference on e-Health Networking, Applications and Services (Healthcom)(2014). DOI: 10.1109/HealthCom.2014.7001878
- ↑ 55.0 55.1 Khademi M, Hondori HM, McKenzie A, Dodakian L, Lopes CV, Cramer SC. “Free-hand interaction with leap motion controller for stroke rehabilitation”. CHI 2014(2014). DOI: 10.1145/2559206.2581203
- ↑ 56.0 56.1 Rand D, Schejter-Margalit T, Dudkiewicz I, Kizony R, Zeilig G. The use of the iPad for poststroke hand rehabilitation; a pilot study. IEEE(2013). DOI: 978-1-4799-0774-8.13. pp. 109- 113.
- ↑ Carabeo CGG, Dalida CMM, Padilla EMZ, Rodrigo MMT. Stroke patient rehabilitation: a pilot study of an android-based game. Simulation; Gaming(2014). Vol. 45, no. 2. pp. 151-166.
- ↑ Manlapaz DG, Silverio L, Ang M. Effectiveness of using nintendo wii in rehabilitation of chronic stroke patients with upper limb hemiparesis: a pilot study. Univ St Tomas Coll Rehabil Sci Phys Ther DepfckLR2009; 1:1–41.
- ↑ Christie LK, Kennedy S, Brennan K, Ellis G, Barber M. Does stroke wiihab work? Use of nintendo wii for upper limb rehabilitation following stroke. Cerebrovasc Dis 2010; Suppl. 2:1–361, doi: 10.1159/fckLR000315008
- ↑ Mouawad M, Doust CG, Max M, McNulty P. Wii-based movement therapy to promote improved upper extremity function post-stroke: a pilot study. Journal of Rehabilitative Medicine. 2011; 43(6):527-533.
- ↑ Rosenberg D, Depp CA, Vahia IV, Reichstadt J, Palmer BW, Kerr J, Jeste DV. Exergames for subsyndromal depression in older adults: a pilot study of a novel intervention. The American Journal of Geriatric Psychiatry. 2010; 18:221-226.
- ↑ Archambault P, Norouzi-Gheidari N, Tao G, Soloman JM, Kairy D, Levin MF. Use of exergames for upper extremity rehabilitation in stroke patients. Annals of Physical and Rehabilitation Medicine. 2015; 58s: e103-e107.
- ↑ Sugarman H, Weisel-Eichler A, Burstin A, and Brown R. Use of novel virtual reality system for the assessment and treatment of unilateral spatial neglect: a feasibility study. International Conference on Virtual Rehabilitation. 2011.
- ↑ Lauder Y, Korsensky O, Brown R, Burstin A, and Hutzler Y. Rapid stepping time on “virtual” objects correlates with measures of balance and fear of falling in elderly individuals. Physiotherapy Journal Impact Factor and Information. 2015; 101.
- ↑ Johansen T, Strøm V, Simic J, Rike PO. Effectiveness of training with motion-controlled commercial video games on hand and arm function in young people with cerebral palsy: A systematic review and meta-analysis. Journal of rehabilitation medicine. 2019 Dec 3.