Low Back Pain or a silent killer (AAA)- A case Study
Abstract[edit | edit source]
Low back pain is most commonly caused by a mechanical dysfunction, however, 1-2% of cases of low back pain are caused by non-mechanical spinal disorders or visceral diseases such as a abdominal aortic aneurysm (AAA). This case study outlines how some patients diagnosed with "low back pain" may have an underlying medical condition. Therefore, as physiotherapists/primary care physicians, its crucial to know how to differentiate between back pain and silent killers such as AAA.
Client Characteristics[edit | edit source]
Patient is referred to physiotherapy after a sailing incident (2 weeks ago) where he felt sharp pain in his back whilst leaning forward and pulling on a jib sheet. Patient is a 65 year old male, South African, working in a boat shop (lots of standing and lifting work). The patient reports seeing a massage therapist and then his GP following the incident. He was prescribed some muscle relaxants and Voltaren as required and referred to physiotherapy. The patient has had previous back sprains, which resolved 100% with physiotherapy. He reports his general health has been good, however takes Aspirin due to his "heart".
Examination Findings[edit | edit source]
Subjective Examination[edit | edit source]
Subjectively the patient reports of low back pain which radiate to both hips and bilateral spasms in his legs. These symptoms reportedly are better in the morning and worsen during the day. The patient reports of waking up and night due to his pain. Aggravating activities include standing, twisting, bending activities and sudden movements. Walking and relative rest reportedly eases the patients symptoms. He enjoys fishing and sailing both of which have been difficult to do secondary to his symptoms. He denies any paraesthesia or pain with coughing or sneezing.
Objective Examination[edit | edit source]
Observation[edit | edit source]
The patient mobilises unaided, independently with an antalgic gait. He also has an antalgic movement pattern during sit -> stand. In standing he has no lateral shift of his trunk. Asymmetrical mole in central-left low back- site of patients pain, pt unaware of mole, uneven shade of colour. Increased tone of right Erector Spinae.
Range of motion[edit | edit source]
Active Range Of Motion (AROM):
- Lumbar spine flexion: Bilateral hands to mid-shin, pain with returning to standing,
- Lumbar spine extension: Increased pain, reduced range of motion
- Repeated movements reveal radiating pain to bilateral hips with repeated lumbar extensions.
Strength[edit | edit source]
Reduced strength 4/5 with resisted right knee flexion, ankle dorsiflexion and plantarflexion. Full strength 5/5 in left lower limb.
Neurological tests[edit | edit source]
- Reflexes: Nil Abnormalities detected with patella tendon reflex testing, however, slight reduction in right ankle jerk reflex.
- Slump test: Positive test - pain reproduced in low back.
- Active Straight Leg Raise (ASLR) - negative test, nil pain reproduced, normal range of motion in both legs.
Other tests[edit | edit source]
Spring test: Pain at L4/5 with central posterior-anterior (PA) glide
Clinical Hypothesis[edit | edit source]
Patient is a 65 year old male who presents to the clinic with low back pain. Due to his mechanism of injury, occupation, aggravating factors, objective assessment this patient initially fits the category of discogenic low back pain +/- nerve root impingement. However, with closer observation to his age, his "heart" condition, day/night pattern of pain, skin observation, symptoms in bilateral limbs suggests patient may require further medical screening.
Intervention[edit | edit source]
The patient was initially treated as a "low back pain" patient with physiotherapy. This included manual therapy - joint mobilisations, massage, etc. and an home exercise programme. However, secondary to the patients mole and nil significant changes in his symptoms after approximately 8 weeks of physiotherapy, the patient was referred to a specialist. The patient was advised to wait in the public medical wait list to see this specialist by his GP. During a follow up phone call the patient reports he has been diagnosed with an abdominal aortic aneurysm (AAA) by the specialist. This diagnosis was made after palpating the abdomen and having a follow up scan. This was reportedly causing the patients low back pain.
The Discussion[edit | edit source]
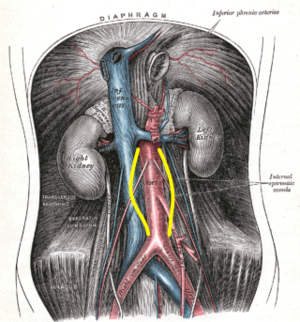
Abdominal Aortic Aneurysm (AAA) is the bulging or widening (50% or more) of the section of the aorta that runs through the abdomen.[1] The abdominal aorta spans between the aortic hiatus and the L4 vertebral level.[1] Here it splits into the right and left common Iliac arteries.[1] AAA is often described as a silent killer as they are clinically silent initially presenting no symptoms at all.[2] However, they can start mimicking low back pain or abdomen pain as the aneurysm enlarges.[2] Risk factors for AAA include age over 55, male sex, genetic/family history of AAA and comorbidities - hypertension and abnormal cholesterol levels.[2] If left untreated ~75% of the victims die before surgery and approximately half make it through surgery.[2] The main symptoms required for onward referral (red flags) include age over 50, patterns of symptoms not compatible with mechanical pain on physical examination, unremitting night pain, etc.[3] Screening for these risk factors, palpating the abdomen +/- referral for an ultrasound of the abdomen are required when AAA is suspected.[2][3][4] As physiotherapists are normally the primary care physicians when treating musculo-skeletal disorders it it therefore crucial the differentiate between "low back pain" and "the silent bombs - AAA".
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Physiopedia. Abdominal Aortic Aneurysm. Avaliable from https://www.physio-pedia.com/Abdominal_Aortic_Aneurysm (accessed 17 February 2019).
- ↑ 2.0 2.1 2.2 2.3 2.4 Harvard Health Publishing. Abdominal aortic aneurysms: Triple A, double trouble. Avaliable from https://www.health.harvard.edu/heart-health/abdominal-aortic-aneurysms-triple-a-double-trouble (accessed 18 February 2019).
- ↑ 3.0 3.1 Sizer Jr PS, Brismée JM, Cook C. Medical screening for red flags in the diagnosis and management of musculoskeletal spine pain. Pain Practice 2007;7(1):53-71.
- ↑ Van Wyngaarden JJ, Ross MD, Hando BR. Abdominal aortic aneurysm in a patient with low back pain. Journal of Orthopaedic & Sports physical therapy 2014;44(7):500-7.