Vagus Nerve: Difference between revisions
Kanza Imtiaz (talk | contribs) No edit summary |
No edit summary |
||
| (24 intermediate revisions by 3 users not shown) | |||
| Line 4: | Line 4: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
[[File:Course and distribution of the glossopharyngeal, vagus, and accessory nerves..gif|right|frameless]] | |||
The vagus nerve serves as the body's superhighway, carrying information between the [[Brain Anatomy|brain]] and the internal organs and controlling the body's response in times of rest and relaxation. The large nerve originates in the brain and branches out in multiple directions to the neck and torso, where it's responsible for actions such as carrying sensory information from the skin of the ear, controlling the muscles that you use to swallow and speak and influencing your [[Immune System|immune system]]<ref name=":2">Live science [https://www.livescience.com/vagus-nerve.html Vagus nerve] Available from:https://www.livescience.com/vagus-nerve.html (accessed 2.2.2021)</ref>. | |||
The [[ | The vagus nerve is the tenth [[Cranial Nerves|cranial nerve]] (CN X) and is the longest mixed cranial nerve. Although we refer to the vagus nerve as singular, it's actually a pair of nerves that emerge from the left and right side of the medulla oblongata portion of the brain stem. The literal translation of the vagus is 'wanderer,' which aptly represents its widespread interfacing of [[Cerebral Cortex|cortex]], [[brainstem]], [[hypothalamus]], and the body. Its afferent and efferent pathways comprise about 80% and 20%, respectively<ref>Mandalaneni K, Rayi A. [https://www.ncbi.nlm.nih.gov/books/NBK562175/ Vagus nerve stimulator.] StatPearls [Internet]. 2020 Aug 20.Available from: https://www.ncbi.nlm.nih.gov/books/NBK562175/<nowiki/>(accessed 31.1.2021)</ref>. | ||
[[ | This [[Neurone|nerve]] is the sensory network that tells the [[Brain Anatomy|brain]] what’s going on in our organs, most specially the digestive tract (stomach and intestines), [[Lung Anatomy|lungs]] and [[Anatomy of the Human Heart|heart]], [[Ruptured Spleen|spleen]], [[Liver Disease|liver]] and kidneys, not to mention a range of other nerves that are involved in everything from talking to eye contact to facial expressions and even your ability to tune in to other people’s voices. It is made of thousands upon thousands of fibers, operating far below the level of our conscious mind. It plays a vital role in sustaining overall wellness. It is an essential part of the [[Parasympathetic System|parasympathetic nervous]] system, which is responsible for calming organs after the stressed “fight-or-flight” adrenaline response to danger.<ref>Melt Vagus Nerve Available from: https://www.meltmethod.com/blog/vagus-nerve/<nowiki/>(accessed 31.1.2021)</ref> | ||
The below video gives an anatomical overview{{#ev:youtube|bNPfjLnnJzA|250}}<ref>Kenhub - Learn Human Anatomy. Vagus nerve: location, branches and function (preview) - Neuroanatomy | Kenhub. Available from: https://www.youtube.com/watch?v=bNPfjLnnJzA [last accessed 23/9/2020]</ref> | |||
The | |||
== Functions == | |||
The vagus nerve has a very extensive distribution. | |||
* Sensory: Innervates the [[skin]] of the external acoustic meatus and the internal surfaces of the laryngopharynx and [[Trachea and Larynx|larynx]]. Provides visceral sensation to the heart and abdominal viscera. | |||
* Special Sensory: Provides taste sensation to the epiglottis and root of the tongue. | |||
* Motor: Provides motor innervation to the majority of the muscles of the pharynx, soft palate and larynx. | |||
* Parasympathetic: Innervates the smooth muscle of the [[Trachea and Larynx|trachea]], bronchi and gastro-intestinal tract and regulates heart rhythm. Its cardiac branches act to slow the rate of heartbeat; its bronchial branch acts to constrict the bronchi; and its esophageal branches control involuntary muscles in the esophagus, stomach, gallbladder, pancreas, and small intestine, stimulating peristalsis and gastrointestinal secretions. .<ref name=":0">Britannica [https://www.britannica.com/science/vagus-nerve Vagus Nerve] Available from: https://www.britannica.com/science/vagus-nerve (accessed 31.1.2021)</ref>. | |||
== Course == | == Course == | ||
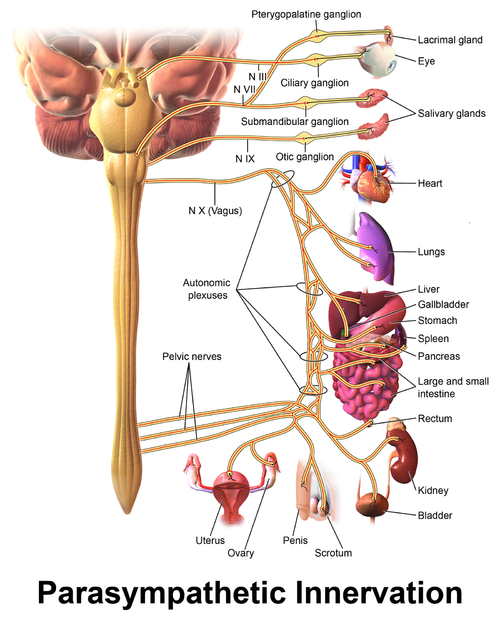
The vagus nerve | [[File:Parasympathetic Innervation.png|right|frameless|625x625px]] | ||
The vagus nerve runs from the brain through the face and thorax to the abdomen. | |||
The right vagus enters the [[Thoracic Anatomy|thorax]] by crossing the first part of the subclavian artery and posterior to the innominate artery; then travels behind the primary right bronchus and esophagus to form the esophageal plexus with the left vagus nerve. <ref name=":1">Yuan H, Silberstein SD. [https://pubmed.ncbi.nlm.nih.gov/26381725/ Vagus nerve and vagus nerve stimulation, a comprehensive review: part II.] Headache: The Journal of Head and Face Pain. 2016 Feb;56(2):259-66.</ref> | * Exits the brain from the [[Brain Anatomy|medulla oblongata]] of the [[brainstem]] and travels laterally exiting the skull through the [[Brain Anatomy|jugular foramen]]. | ||
* It descends within the carotid sheath where it is located posterolateral to the internal and [[Common Carotid Artery|common carotid arteries]], and medial to the internal jugular vein. | |||
[[ | At the base of the neck, the nerve enters the thorax, where the right and left vagus nerve travels on a different path. <ref>Garner DH, Baker S. [https://pubmed.ncbi.nlm.nih.gov/30137861/ Anatomy, Head and Neck, Carotid Sheath.] InStatPearls [Internet] 2019 Feb 6. StatPearls Publishing.</ref> | ||
# The right vagus enters the [[Thoracic Anatomy|thorax]] by crossing the first part of the subclavian artery and posterior to the innominate artery; then travels behind the primary right bronchus and esophagus to form the esophageal plexus with the left vagus nerve. <ref name=":1">Yuan H, Silberstein SD. [https://pubmed.ncbi.nlm.nih.gov/26381725/ Vagus nerve and vagus nerve stimulation, a comprehensive review: part II.] Headache: The Journal of Head and Face Pain. 2016 Feb;56(2):259-66.</ref> | |||
# The left vagus enters the thorax by passing between the left common carotid and left [[Vertebral Artery|subclavian]] arteries, then travels behind the primary left bronchus and into the esophagus.<ref name=":1" /><ref name=":0" /> | |||
The | The [[Accessory Nerve Cranial Nerve 11|accessory nerve (CN XI)]] joins the vagus nerve just distal to the inferior ganglion.<ref>Berthoud HR, Neuhuber WL. [https://pubmed.ncbi.nlm.nih.gov/11189015/ Functional and chemical anatomy of the afferent vagal system. Autonomic Neuroscience]. 2000 Dec 20;85(1-3):1-7.</ref> | ||
[ | |||
== Parasympathetic Actions == | |||
''' | In the thorax and abdomen, the vagus nerve is the main parasympathetic outflow to the heart and gastro-intestinal organs. | ||
# '''The Heart''': Cardiac branches arise in the thorax, conveying parasympathetic innervation to the sino-atrial and atrio-ventricular nodes of the heart. These branches stimulate a reduction in the resting heart rate. They are constantly active, producing a rhythm of 60 – 80 beats per minute. If the vagus nerve was lesioned, the resting heart rate would be around 100 beats per minute. | |||
# '''Gastro-Intestinal System''': The vagus nerve provides parasympathetic innervation to the majority of the abdominal organs. It sends branches to the oesophagus, stomach and most of the intestinal tract – up to the splenic flexure of the large colon. The function of the vagus nerve is to stimulate smooth muscle contraction and glandular secretions in these organs. For example, in the stomach, the vagus nerve increases the rate of gastric emptying, and stimulates acid production<ref>Teach me anatomy [https://teachmeanatomy.info/head/cranial-nerves/vagus-nerve-cn-x/ Vagus Nerve] Available from: https://teachmeanatomy.info/head/cranial-nerves/vagus-nerve-cn-x/<nowiki/>(accessed 31.1.2021)</ref> | |||
== Gut Brain Axis == | |||
The past decade has seen a paradigm shift in our understanding of the [[Gut Brain Axis (GBA)|brain-gut axis]]. The [[Microbiome and Movement|microbiota]], the gut, and the brain communicate through the microbiota-gut-brain axis in a bidirectional way that involves the autonomic nervous system. | |||
The vagus nerve (VN), the principal component of the [[Parasympathetic System|parasympathetic nervous system]], is a mixed nerve composed of 80% afferent and 20% efferent fibers. The VN, because of its role in interoceptive awareness, is able to sense the microbiota metabolites through its afferents, to transfer this gut information to the central nervous system where it is integrated in the central autonomic network, and then to generate a response. | |||
* A cholinergic anti-inflammatory pathway has been described through VN's fibers, which is able to dampen peripheral inflammation and to decrease intestinal permeability, thus very probably modulating microbiota composition. | |||
* [[Stress and Health|Stress]] inhibits the VN and has deleterious effects on the gastrointestinal tract and on the microbiota, and is involved in the pathophysiology of gastrointestinal disorders such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) which are both characterized by a dysbiosis. | |||
* A low vagal tone has been described in IBD and IBS patients thus favoring peripheral inflammation. | |||
* The exponential growth of evidence detailing the bidirectional interactions between the gut microbiome and the brain supports a comprehensive model that integrates the central nervous, gastrointestinal, and immune systems with this newly discovered organ<ref>Bonaz B, Bazin T, Pellissier S. [https://pubmed.ncbi.nlm.nih.gov/29467611/ The vagus nerve at the interface of the microbiota-gut-brain axis]. Frontiers in neuroscience. 2018 Feb 7;12:49.Availabl from: https://pubmed.ncbi.nlm.nih.gov/29467611/<nowiki/>(accessed 1.2.2021)</ref>.<ref>Martin CR, Osadchiy V, Kalani A, Mayer EA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6047317/ The brain-gut-microbiome axis]. Cellular and molecular gastroenterology and hepatology. 2018 Jan 1;6(2):133-48.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6047317/<nowiki/>(last accessed 1.2.2021)</ref> | |||
== | == Anti‐inflammatory properties of the vagus nerve == | ||
[[File:Cytokine release.jpg|right|frameless]] | |||
A low vagal tone, as assessed by heart rate variability, a marker of the sympatho-vagal balance, is observed in functional digestive disorders and [[Irritable Bowel Syndrome|inflammatory bowel diseases]]. To restore a normal vagal tone appears as a goal in such diseases. Among the therapeutic tools, such as drugs targeting the cholinergic system and/or complementary medicine (hypnosis, meditation), deep breathing, [[Physical Activity|physical exercise]], VN stimulation (VNS), either invasive or non-invasive, appears as innovative. There is new evidence supporting the role of VNS in the modulation of gastrointestinal functions<ref>Bonaz B, Sinniger V, Pellissier S. Vagal tone: effects on sensitivity, motility, and inflammation. Neurogastroenterology & motility. 2016 Apr;28(4):455-62.Available from: https://pubmed.ncbi.nlm.nih.gov/27010234/<nowiki/>(accessed 31.1.2021)</ref>. | |||
Brain and viscera interplay within the autonomic nervous system where the vagus nerve (VN), containing approximately 80% afferent and 20% efferent fibres, plays multiple key roles in the homeostatic regulations of visceral functions. Recent data have suggested the anti‐inflammatory role of the VN. This vagal function is mediated through several pathways. The first one is the anti‐inflammatory hypothalamic–pituitary–adrenal axis which is stimulated by vagal afferent fibres and leads to the release of cortisol by the adrenal glands and efferent (activation of the CAP) fibres. Given its position as a key element of the autonomic nervous system in the brain–gut interactions the VN seems to be a good therapeutic target in inflammatory conditions of the digestive tract (e.g. IBD) and also other inflammatory conditions such as RA, and others. | |||
The use of neuromodulation by bioelectronics devices as a treatment is an emerging field in the domain of bioelectronic medicine. It could be an alternative non‐drug therapy to conventional treatment or could be combined with such treatments, but further investigation in a large longitudinal cohort of patients is required.<ref>Bonaz B, Sinniger V, Pellissier S. Anti‐inflammatory properties of the vagus nerve: potential therapeutic implications of vagus nerve stimulation. The Journal of physiology. 2016 Oct 15;594(20):5781-90.Available from:https://physoc.onlinelibrary.wiley.com/doi/full/10.1113/JP271539 (accessed 31,1,2021)</ref> | |||
== Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders == | |||
[[File:Vagus nerve stimulation.jpg|right|frameless|450x450px]]The Vagus nerve constantly sends updated sensory information about the state of the body's organs "upstream" to your brain via afferent nerves. In fact, 80 to 90 percent of the nerve fibers in the vagus nerve are dedicated to communicating the state of your viscera up to your brain.<ref>Psychology today Vagus nerve and the gut<nowiki/>https://www.psychologytoday.com/us/blog/the-athletes-way/201405/how-does-the-vagus-nerve-convey-gut-instincts-the-brain (accessed 1.2.2021)</ref> | |||
Image: Process of medically stimulating vagus nerve. | |||
The vagus nerve represents the main component of the parasympathetic nervous system, which oversees a vast array of crucial bodily functions (including control of mood, [[Immune System|immune response]], digestion, and [[Pulse rate|heart rate]]). It establishes one of the connections between the brain and the gastrointestinal tract and sends information about the state of the inner organs to the brain via afferent fibers. | |||
* There is preliminary evidence that vagus nerve stimulation (VNS) is a promising add-on treatment for treatment-refractory [[depression]], [[Post-traumatic Stress Disorder|posttraumatic stress disorder]], and inflammatory bowel disease. | |||
* Treatments that target the vagus nerve increase the vagal tone and inhibit [[Cytokines|cytokine]] production. Both are important mechanism of resiliency. The stimulation of vagal afferent fibers in the gut influences monoaminergic brain systems in the brain stem that play crucial roles in major psychiatric conditions, such as mood and anxiety disorders. | |||
* There is preliminary evidence for gut bacteria to have beneficial effect on mood and anxiety, partly by affecting the activity of the vagus nerve. Since, the vagal tone is correlated with capacity to regulate [[Stress and Health|stress]] responses and can be influenced by breathing, its increase through meditation and [[yoga]] likely contribute to resilience and the mitigation of mood and anxiety symptoms<ref>Breit S, Kupferberg A, Rogler G, Hasler G. Vagus nerve as modulator of the brain–gut axis in psychiatric and inflammatory disorders. Frontiers in psychiatry. 2018 Mar 13;9:44.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5859128/ (accessed 31.1.2021)</ref>. | |||
* Currently, VNS is a Food and Drug Administration (FDA) approved treatment for various conditions like chronic [[epilepsy]], refractory epilepsy, and depression. It is also being investigated in various other conditions like [[Autoimmune Disorders|autoimmune]] and [[Chronic Disease|chronic]] inflammatory disorders<ref>Mandalaneni K, Rayi A. Vagus nerve stimulator. StatPearls [Internet]. 2020 Aug 20.Available from: https://www.ncbi.nlm.nih.gov/books/NBK562175/<nowiki/>(accessed 31.1.2021)</ref> | |||
The below 4 minute video gives an insight into the Gut Brain Axis{{#ev:youtube|gp67EQhNfj8|250}}<ref>The Art of Living. What Is The Vagus Nerve? | Vagus Nerve Explained | Brain, Mind Body Connect. Available from: https://www.youtube.com/watch?v=gp67EQhNfj8 [last accessed 23/9/2020]</ref> | |||
== Vasovagal Syncope == | |||
When someone faints from heat exposure, standing for a long time or from something surprising such as the sight of blood, the vagus nerve is partly to blame. This occurrence, called vasovagal syncope, happens when the sympathetic division dilates [[Cardiovascular System|blood vessels]] in the legs and the vagus nerve overreacts, causing a significant and immediate decrease in heart rate. Blood pools in the legs, [[Blood Pressure|blood pressure]] drops, and without enough blood flow to the brain, the person loses consciousness momentarily. Unless a person faints frequently, vasovagal syncope does not require treatment<ref name=":2" />. | |||
== Resources == | == Resources == | ||
Latest revision as of 12:20, 11 February 2021
Top Contributors - Kanza Imtiaz, Lucinda hampton and Tony Lowe
Introduction[edit | edit source]
The vagus nerve serves as the body's superhighway, carrying information between the brain and the internal organs and controlling the body's response in times of rest and relaxation. The large nerve originates in the brain and branches out in multiple directions to the neck and torso, where it's responsible for actions such as carrying sensory information from the skin of the ear, controlling the muscles that you use to swallow and speak and influencing your immune system[1].
The vagus nerve is the tenth cranial nerve (CN X) and is the longest mixed cranial nerve. Although we refer to the vagus nerve as singular, it's actually a pair of nerves that emerge from the left and right side of the medulla oblongata portion of the brain stem. The literal translation of the vagus is 'wanderer,' which aptly represents its widespread interfacing of cortex, brainstem, hypothalamus, and the body. Its afferent and efferent pathways comprise about 80% and 20%, respectively[2].
This nerve is the sensory network that tells the brain what’s going on in our organs, most specially the digestive tract (stomach and intestines), lungs and heart, spleen, liver and kidneys, not to mention a range of other nerves that are involved in everything from talking to eye contact to facial expressions and even your ability to tune in to other people’s voices. It is made of thousands upon thousands of fibers, operating far below the level of our conscious mind. It plays a vital role in sustaining overall wellness. It is an essential part of the parasympathetic nervous system, which is responsible for calming organs after the stressed “fight-or-flight” adrenaline response to danger.[3]
The below video gives an anatomical overview
Functions[edit | edit source]
The vagus nerve has a very extensive distribution.
- Sensory: Innervates the skin of the external acoustic meatus and the internal surfaces of the laryngopharynx and larynx. Provides visceral sensation to the heart and abdominal viscera.
- Special Sensory: Provides taste sensation to the epiglottis and root of the tongue.
- Motor: Provides motor innervation to the majority of the muscles of the pharynx, soft palate and larynx.
- Parasympathetic: Innervates the smooth muscle of the trachea, bronchi and gastro-intestinal tract and regulates heart rhythm. Its cardiac branches act to slow the rate of heartbeat; its bronchial branch acts to constrict the bronchi; and its esophageal branches control involuntary muscles in the esophagus, stomach, gallbladder, pancreas, and small intestine, stimulating peristalsis and gastrointestinal secretions. .[5].
Course[edit | edit source]
The vagus nerve runs from the brain through the face and thorax to the abdomen.
- Exits the brain from the medulla oblongata of the brainstem and travels laterally exiting the skull through the jugular foramen.
- It descends within the carotid sheath where it is located posterolateral to the internal and common carotid arteries, and medial to the internal jugular vein.
At the base of the neck, the nerve enters the thorax, where the right and left vagus nerve travels on a different path. [6]
- The right vagus enters the thorax by crossing the first part of the subclavian artery and posterior to the innominate artery; then travels behind the primary right bronchus and esophagus to form the esophageal plexus with the left vagus nerve. [7]
- The left vagus enters the thorax by passing between the left common carotid and left subclavian arteries, then travels behind the primary left bronchus and into the esophagus.[7][5]
The accessory nerve (CN XI) joins the vagus nerve just distal to the inferior ganglion.[8]
Parasympathetic Actions[edit | edit source]
In the thorax and abdomen, the vagus nerve is the main parasympathetic outflow to the heart and gastro-intestinal organs.
- The Heart: Cardiac branches arise in the thorax, conveying parasympathetic innervation to the sino-atrial and atrio-ventricular nodes of the heart. These branches stimulate a reduction in the resting heart rate. They are constantly active, producing a rhythm of 60 – 80 beats per minute. If the vagus nerve was lesioned, the resting heart rate would be around 100 beats per minute.
- Gastro-Intestinal System: The vagus nerve provides parasympathetic innervation to the majority of the abdominal organs. It sends branches to the oesophagus, stomach and most of the intestinal tract – up to the splenic flexure of the large colon. The function of the vagus nerve is to stimulate smooth muscle contraction and glandular secretions in these organs. For example, in the stomach, the vagus nerve increases the rate of gastric emptying, and stimulates acid production[9]
Gut Brain Axis[edit | edit source]
The past decade has seen a paradigm shift in our understanding of the brain-gut axis. The microbiota, the gut, and the brain communicate through the microbiota-gut-brain axis in a bidirectional way that involves the autonomic nervous system.
The vagus nerve (VN), the principal component of the parasympathetic nervous system, is a mixed nerve composed of 80% afferent and 20% efferent fibers. The VN, because of its role in interoceptive awareness, is able to sense the microbiota metabolites through its afferents, to transfer this gut information to the central nervous system where it is integrated in the central autonomic network, and then to generate a response.
- A cholinergic anti-inflammatory pathway has been described through VN's fibers, which is able to dampen peripheral inflammation and to decrease intestinal permeability, thus very probably modulating microbiota composition.
- Stress inhibits the VN and has deleterious effects on the gastrointestinal tract and on the microbiota, and is involved in the pathophysiology of gastrointestinal disorders such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) which are both characterized by a dysbiosis.
- A low vagal tone has been described in IBD and IBS patients thus favoring peripheral inflammation.
- The exponential growth of evidence detailing the bidirectional interactions between the gut microbiome and the brain supports a comprehensive model that integrates the central nervous, gastrointestinal, and immune systems with this newly discovered organ[10].[11]
Anti‐inflammatory properties of the vagus nerve[edit | edit source]
A low vagal tone, as assessed by heart rate variability, a marker of the sympatho-vagal balance, is observed in functional digestive disorders and inflammatory bowel diseases. To restore a normal vagal tone appears as a goal in such diseases. Among the therapeutic tools, such as drugs targeting the cholinergic system and/or complementary medicine (hypnosis, meditation), deep breathing, physical exercise, VN stimulation (VNS), either invasive or non-invasive, appears as innovative. There is new evidence supporting the role of VNS in the modulation of gastrointestinal functions[12].
Brain and viscera interplay within the autonomic nervous system where the vagus nerve (VN), containing approximately 80% afferent and 20% efferent fibres, plays multiple key roles in the homeostatic regulations of visceral functions. Recent data have suggested the anti‐inflammatory role of the VN. This vagal function is mediated through several pathways. The first one is the anti‐inflammatory hypothalamic–pituitary–adrenal axis which is stimulated by vagal afferent fibres and leads to the release of cortisol by the adrenal glands and efferent (activation of the CAP) fibres. Given its position as a key element of the autonomic nervous system in the brain–gut interactions the VN seems to be a good therapeutic target in inflammatory conditions of the digestive tract (e.g. IBD) and also other inflammatory conditions such as RA, and others.
The use of neuromodulation by bioelectronics devices as a treatment is an emerging field in the domain of bioelectronic medicine. It could be an alternative non‐drug therapy to conventional treatment or could be combined with such treatments, but further investigation in a large longitudinal cohort of patients is required.[13]
Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders[edit | edit source]
The Vagus nerve constantly sends updated sensory information about the state of the body's organs "upstream" to your brain via afferent nerves. In fact, 80 to 90 percent of the nerve fibers in the vagus nerve are dedicated to communicating the state of your viscera up to your brain.[14]
Image: Process of medically stimulating vagus nerve.
The vagus nerve represents the main component of the parasympathetic nervous system, which oversees a vast array of crucial bodily functions (including control of mood, immune response, digestion, and heart rate). It establishes one of the connections between the brain and the gastrointestinal tract and sends information about the state of the inner organs to the brain via afferent fibers.
- There is preliminary evidence that vagus nerve stimulation (VNS) is a promising add-on treatment for treatment-refractory depression, posttraumatic stress disorder, and inflammatory bowel disease.
- Treatments that target the vagus nerve increase the vagal tone and inhibit cytokine production. Both are important mechanism of resiliency. The stimulation of vagal afferent fibers in the gut influences monoaminergic brain systems in the brain stem that play crucial roles in major psychiatric conditions, such as mood and anxiety disorders.
- There is preliminary evidence for gut bacteria to have beneficial effect on mood and anxiety, partly by affecting the activity of the vagus nerve. Since, the vagal tone is correlated with capacity to regulate stress responses and can be influenced by breathing, its increase through meditation and yoga likely contribute to resilience and the mitigation of mood and anxiety symptoms[15].
- Currently, VNS is a Food and Drug Administration (FDA) approved treatment for various conditions like chronic epilepsy, refractory epilepsy, and depression. It is also being investigated in various other conditions like autoimmune and chronic inflammatory disorders[16]
The below 4 minute video gives an insight into the Gut Brain Axis
Vasovagal Syncope[edit | edit source]
When someone faints from heat exposure, standing for a long time or from something surprising such as the sight of blood, the vagus nerve is partly to blame. This occurrence, called vasovagal syncope, happens when the sympathetic division dilates blood vessels in the legs and the vagus nerve overreacts, causing a significant and immediate decrease in heart rate. Blood pools in the legs, blood pressure drops, and without enough blood flow to the brain, the person loses consciousness momentarily. Unless a person faints frequently, vasovagal syncope does not require treatment[1].
Resources[edit | edit source]
Vagus nerve stimulation
References[edit | edit source]
- ↑ 1.0 1.1 Live science Vagus nerve Available from:https://www.livescience.com/vagus-nerve.html (accessed 2.2.2021)
- ↑ Mandalaneni K, Rayi A. Vagus nerve stimulator. StatPearls [Internet]. 2020 Aug 20.Available from: https://www.ncbi.nlm.nih.gov/books/NBK562175/(accessed 31.1.2021)
- ↑ Melt Vagus Nerve Available from: https://www.meltmethod.com/blog/vagus-nerve/(accessed 31.1.2021)
- ↑ Kenhub - Learn Human Anatomy. Vagus nerve: location, branches and function (preview) - Neuroanatomy | Kenhub. Available from: https://www.youtube.com/watch?v=bNPfjLnnJzA [last accessed 23/9/2020]
- ↑ 5.0 5.1 Britannica Vagus Nerve Available from: https://www.britannica.com/science/vagus-nerve (accessed 31.1.2021)
- ↑ Garner DH, Baker S. Anatomy, Head and Neck, Carotid Sheath. InStatPearls [Internet] 2019 Feb 6. StatPearls Publishing.
- ↑ 7.0 7.1 Yuan H, Silberstein SD. Vagus nerve and vagus nerve stimulation, a comprehensive review: part II. Headache: The Journal of Head and Face Pain. 2016 Feb;56(2):259-66.
- ↑ Berthoud HR, Neuhuber WL. Functional and chemical anatomy of the afferent vagal system. Autonomic Neuroscience. 2000 Dec 20;85(1-3):1-7.
- ↑ Teach me anatomy Vagus Nerve Available from: https://teachmeanatomy.info/head/cranial-nerves/vagus-nerve-cn-x/(accessed 31.1.2021)
- ↑ Bonaz B, Bazin T, Pellissier S. The vagus nerve at the interface of the microbiota-gut-brain axis. Frontiers in neuroscience. 2018 Feb 7;12:49.Availabl from: https://pubmed.ncbi.nlm.nih.gov/29467611/(accessed 1.2.2021)
- ↑ Martin CR, Osadchiy V, Kalani A, Mayer EA. The brain-gut-microbiome axis. Cellular and molecular gastroenterology and hepatology. 2018 Jan 1;6(2):133-48.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6047317/(last accessed 1.2.2021)
- ↑ Bonaz B, Sinniger V, Pellissier S. Vagal tone: effects on sensitivity, motility, and inflammation. Neurogastroenterology & motility. 2016 Apr;28(4):455-62.Available from: https://pubmed.ncbi.nlm.nih.gov/27010234/(accessed 31.1.2021)
- ↑ Bonaz B, Sinniger V, Pellissier S. Anti‐inflammatory properties of the vagus nerve: potential therapeutic implications of vagus nerve stimulation. The Journal of physiology. 2016 Oct 15;594(20):5781-90.Available from:https://physoc.onlinelibrary.wiley.com/doi/full/10.1113/JP271539 (accessed 31,1,2021)
- ↑ Psychology today Vagus nerve and the guthttps://www.psychologytoday.com/us/blog/the-athletes-way/201405/how-does-the-vagus-nerve-convey-gut-instincts-the-brain (accessed 1.2.2021)
- ↑ Breit S, Kupferberg A, Rogler G, Hasler G. Vagus nerve as modulator of the brain–gut axis in psychiatric and inflammatory disorders. Frontiers in psychiatry. 2018 Mar 13;9:44.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5859128/ (accessed 31.1.2021)
- ↑ Mandalaneni K, Rayi A. Vagus nerve stimulator. StatPearls [Internet]. 2020 Aug 20.Available from: https://www.ncbi.nlm.nih.gov/books/NBK562175/(accessed 31.1.2021)
- ↑ The Art of Living. What Is The Vagus Nerve? | Vagus Nerve Explained | Brain, Mind Body Connect. Available from: https://www.youtube.com/watch?v=gp67EQhNfj8 [last accessed 23/9/2020]