Femoral Neck Hip Fracture: Difference between revisions
No edit summary |
m (Lucinda hampton moved page Hip Fracture/Femoral Neck Fracture to Femoral Neck Hip Fracture: More appropriate ) |
||
| (148 intermediate revisions by 17 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox">'''Original Editor '''- [[User: Delmoitie Giovanni|Delmoitie Giovanni]] | |||
'''Original | |||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} </div> | ||
</div> | == Introduction == | ||
== | [[File:Fig5.png|thumb|Garden classification, NOF]] | ||
Hip fractures are one of the most frequent fractures presenting to the emergency department and orthopedic trauma teams. | |||
# The terms hip fracture and femoral neck fracture both relate to the same type of injury. | |||
# Both terms describe a fracture of the proximal femur between the femoral head and 5 cm distal to the lesser trochanter.<ref name=":2">Emmerson BR, Varacallo M, Inman D. Hip Fracture Overview. InStatPearls [Internet] 2022 Feb 12. StatPearls Publishing.Available;https://www.statpearls.com/articlelibrary/viewarticle/22890/ (accessed 9.12.2022)</ref> | |||
A hip fracture occurs just below the head of femur (HOF), the region of the femur called the femoral neck. A femoral neck fracture disconnects the HOF from the rest of the femur. Click [[Hip Anatomy]] for more details | |||
== Etiology == | |||
Most commonly: | |||
* Falls in the elderly: Account for the majority of hip fractures. Risk factors for falls in the elderly population are many, those strongly associated with these fractures are a previous history of falls, gait abnormalities, the use of walking aids, vertigo, Parkinson disease, and antiepileptic medications. A lot of patients have multiple risk factors, and this, combined with age-associated reduced bone quality, is the underpinning cause of most hip fractures.<ref name=":2" /> The majority of fragility hip fractures occurred inside the home<ref name=":3">Dhibar DP, Gogate Y, Aggarwal S, Garg S, Bhansali A, Bhadada SK. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6683687/ Predictors and outcome of fragility hip fracture: a prospective study from North India]. Indian Journal of Endocrinology and Metabolism. 2019 May;23(3):282.</ref> | |||
* Significant trauma (e.g. motor vehicle collisions) in younger patients | |||
* About 3% of hip fractures are related to localized bone weakness at the fracture site, secondary to tumour, followed by bone cysts, or [[Paget's Disease|Paget’s disease]]. | |||
== | ==Epidemiology == | ||
The incidence of femoral neck fractures is increasing as the proportion of the elderly population in many countries increases. Between 1990 and 2000, there was nearly a 25% increase in hip fractures worldwide.<ref name=":0">Radiopedia Neck of femur fracture Available:https://radiopaedia.org/articles/neck-of-femur-fracture-1?lang=us (accessed 9.12.2022)</ref> | |||
The hip | * The peak number of hip fractures occurred at 75-79 years of age for both sexes, with most occuring in women. In white women, the lifetime risk of hip fracture is 1 in 6. | ||
* Up to 20% of patients die in the first year following hip fractures, mostly due to pre-existing medical conditions. Less than half of those who survive the hip fracture regain their previous level of function<ref>IOF [https://www.iofbonehealth.org/facts-statistics#category-16 Facts and stats] Available from:https://www.iofbonehealth.org/facts-statistics#category-16 (last accessed 14.10.2020)</ref> | |||
== | == Classification of Hip Fractures == | ||
[[File:Hip fracture classification.png|350x350px|alt=|thumb|Hip fracture classification]] | |||
Hip fractures is classified into intracapsular and extracapsular fractures<ref name=":7">Zuckerman JD. [https://www.nejm.org/doi/full/10.1056/NEJM199606063342307 Hip fracture]. New England journal of medicine. 1996 Jun 6;334(23):1519-25.</ref> | |||
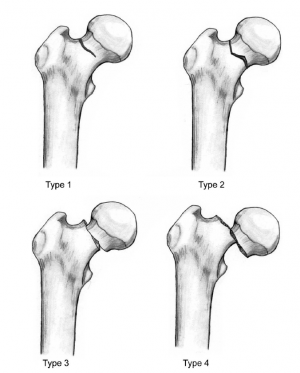
# '''Intracapsular fractures''' (femoral neck fractures): Occurs within the hip capsule; accounts for 45% of all acute hip fractures in the elderly<ref>Canale ST. ''Campbell's Operative Orthopaedics''. St. Louis, MO: Mosby;; 1998. pp. 2181–2223.</ref>; susceptible to malunion/[https://physio-pedia.com/Avascular_Necrosis avascular necrosis] of the HOF because of the limited blood supply to the area. The [[Femoral Neck Fractures, Garden Classification]] is the most commonly classification system. This splits into four categories depending on the severity of the fracture and the degree of displacement. | |||
# '''Extracapsular fractures''': Intertrochanteric fracture: occurs between the greater and the lesser trochanter<ref name=":7" />, intertrochanteric region has a good blood supply, [https://physio-pedia.com/Avascular_Necrosis avascular necrosis] or nonunion is rare; Subtronchanteric fracture: occurs below the lesser trochanter, approximately 2.5 inches below. | |||
== Risk factors == | |||
Risk factors for hip fracture include<ref>Grisso JA, Kelsey JL, Strom BL, Ghiu GY, Maislin G, O'Brien LA, Hoffman S, Kaplan F. [https://www.nejm.org/doi/full/10.1056/NEJM199105093241905 Risk factors for falls as a cause of hip fracture in women]. New England journal of medicine. 1991 May 9;324(19):1326-31. </ref><ref>http://www.mayoclinic.com/health/hip-fracture/DS00185/DSECTION=risk-factors (visited on april 2016)</ref>: | |||
*Gender: prevalent in women; post[[Menopause|menopausal]] twice as likely as premenopausal to have hip fracture<ref>Banks E, Reeves GK, Beral V, Balkwill A, Liu B, Roddam A, [https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1000181 Million Women Study Collaborators. Hip fracture incidence in relation to age, menopausal status, and age at menopause: prospective analysis]. PLoS medicine. 2009 Nov 10;6(11):e1000181.</ref> | |||
*Reduced Bone density<ref>Angthong C, Suntharapa T, Harnroongroj T. [https://dergipark.org.tr/en/pub/aott/issue/18213/191450 Major risk factors for the second contralateral hip fracture in the elderly.] Acta orthopaedica et traumatologica turcica. 2009 May 1;43(3):193-8.</ref> | |||
*Falls<ref>Yang Y, Komisar V, Shishov N, Lo B, Korall AM, Feldman F, Robinovitch SN. [https://asbmr.onlinelibrary.wiley.com/doi/abs/10.1002/jbmr.4048 The Effect Of Fall Biomechanics On Risk For Hip Fracture In Older Adults: A Cohort Study Of Video‐Captured Falls In Long‐Term Care.] Journal of bone and mineral research. 2020 May 13.</ref> | |||
*[[Medication and Falls|Medications]]: Some medications can cause a decrease in bone density like cortisone. | |||
* | *[[Nutrition]]: It is well known that calcium and vitamin D increase bone mass, so a lack of it can cause several fractures, including hip fractures. | ||
*Age: the older you get, the higher the risk is for hip fractures. 90% of these fractures occur in persons over 70 years old. | |||
*[[Alcoholism|Alcohol]] and tobacco: These products can reduce bone mass, causing a higher risk to have a hip fracture | |||
*Medical problems: Endocrine disorders can cause fragility of the bones | |||
*[[Physical Inactivity|Physical inactivity]]: [[Physical Activity|Physical activity]] is very important for muscle mass and bone mass | |||
*[[Stroke]] increases the risk factor for falls which can cause a hip fracture. | |||
*[[Parkinson's|Parkinson’s]] disease increases the risk factor for falls which can cause a hip fracture. | |||
== Characteristics/Clinical Presentation == | |||
*Dull ache in the groin and/or hip region<ref name=":8">Rao SS, Cherukuri M. [https://www.aafp.org/afp/2006/0615/p2195.html Management of hip fracture: the family physician's role]. American family physician. 2006 Jun 15;73(12):2195-200. </ref> | |||
*Inability to put weight on the injured leg causing immobility right after the fall<ref name=":9" /> | |||
*Shorter leg on the side of the injured hip | |||
*Dull ache in the groin and/or hip region <ref name=" | *External rotation of the injured leg<ref name=":9" /> | ||
*Inability to put weight on the injured leg causing immobility right after the fall <ref name=" | *Stiffness, bruising and swelling in and around the hip | ||
* | |||
* | |||
* | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
The diagnosis of a hip fracture is established based on patient history, physical examination and radiography. <ref name=" | The diagnosis of a hip fracture is established based on patient history, physical examination, and radiography.<ref name=":9">Dinçel VE, Şengelen M, Sepici V, Çavuşoğlu T, Sepici B. [https://onlinelibrary.wiley.com/doi/abs/10.1002/ca.20680 The association of proximal femur geometry with hip fracture risk]. Clinical Anatomy: The Official Journal of the American Association of Clinical Anatomists and the British Association of Clinical Anatomists. 2008 Sep;21(6):575-80. | ||
</ref> | |||
* Plain [[X-Rays|radiograph]]<nowiki/>s (sensitivity 93-98%) is the first-line investigation for suspected Neck of Femur(NOF) fractures. | |||
* In patients with a suspected occult NOF fracture, [[MRI Scans|MRI]] (sensitivity 99-100%) is recommended by many institutions as the second-line test if available within 24 hours, with CT or nuclear medicine bone scan third-line<ref name=":1">Radiopedia [https://radiopaedia.org/articles/femoral-neck-fracture NOF fractures] Available from:https://radiopaedia.org/articles/femoral-neck-fracture (last accessed 14.10.2020)</ref> | |||
== Outcome Measures == | |||
* [https://physio-pedia.com/Functional_Independence_Measure_(FIM) Functional Independence Measure] | |||
* [[Berg Balance Scale|Berg Balance Scale]] | |||
* [https://physio-pedia.com/Timed_Up_and_Go_Test_(TUG) Timed Up and Go Test (TUG)] | |||
* [[Patient Specific Functional Scale]] | |||
* [[Falls Risk Assessment Tool (FRAT): An Overview to Assist Understanding and Conduction|Falls Risk Assessment Tool]] | |||
== Treatment == | |||
Serious complications (for example avascular necrosis and non-union) are very common without surgical intervention. | |||
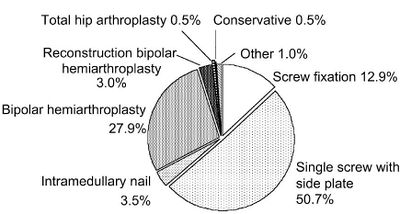
In general, Garden stage I and II are stable fractures and can be treated with internal fixation (head-preservation) eg dymanic hip screw, and stage III and IV are unstable fractures and hence treated with arthroplasty (either hemi- or total arthroplasty. Internal fixation can be performed with multiple pins, intramedullary hip screw, crossed screw-nails or compression with a dynamic screw and plate. | |||
== | The high morbidity and mortality assoc<span class="reference" id="cite_ref-11"></span>iated with hip and pelvic fractures after trauma is well reported. | ||
Prognosis varies but is complicated by older age, as hip fractures increase the risk of death and major morbidity in the elderly.<ref name=":0" /> | |||
== Rehabilitation == | |||
[[Image:Figure4.jpg|right|frameless|400x400px]]The postoperative rehabilitation is as important as the initial surgery. Surgery aims to restore mobility, and commence early mobilization. Patients who have undergone arthroplasty or fixation of an extracapsular fracture can usually mobilize immediately after surgery without weight restrictions. Following fixation of an intracapsular fracture protected weight bearing is often recommended to reduce the risk of subsequent fracture displacement. | |||
= | Regular intensive physiotherapy is needed to encourage the rapid progression of mobility, aiming to restore the patient’s pre-morbid mobility status. Sadly, many patients do not regain their previous level of mobility or independence and therefore require social care input<ref name=":2" />. | ||
== Physical Examination == | |||
== | On physical examination, findings on the patient with a hip fracture may include the following: | ||
* limited and painful hip range of motion, especially in internal rotation. | |||
* the injured leg is shortened, externally rotated, and abducted in the supine position | |||
* Pain is noted upon attempted passive hip motion. | |||
* Ecchymosis may or may not be present. | |||
* An antalgic gait pattern may be present. | |||
* Tenderness to palpation around the inguinal area, over the femoral neck. This area may also be swollen. | |||
* Increased pain on the extremes of hip rotation, an abduction lurch, and an inability to stand on the involved leg | |||
For more on details, Click [[Hip Examination]] | |||
== Physical Therapy Management == | |||
[[File:Hip exercise 6.png|right|frameless]] | |||
Rehabilitation begins promptly. | |||
'''Two to three days postoperative''' | |||
* Instruct patient in deep breathing and cough. '''Goal:''' Prevent postoperative pneumonia and [[atelectasis]]. | |||
* Initiate isometrics and ankle pumps with involved extremity. '''Goal:''' Prepare patient for active exercise program. | |||
* Initiate bedside sitting once physician has cleared patient for this activity. '''Goal:''' Prepare patient to begin transfer and progressive gait training processes.<ref>Luciani D, Cadossi M, Mazzotti A, Chiarello E, Giannini S. [https://link.springer.com/article/10.1007/s40520-013-0079-9 The importance of rehabilitation after lower limb fractures in elderly osteoporotic patients.] Aging clinical and experimental research. 2013 Oct;25(1):113-5. | |||
</ref> | |||
'''Three to five days postoperative''' | |||
* Gait train patient, observing weight-bearing precautions. Progress to walker or crutches. '''Goal:''' Establish independent gait with assistive device, using proper gait pattern on all surfaces and stairs. | |||
* Initiate training in activities of daily living, including bed mobility and transfers to and from bed and toilet. '''Goal:''' Achieve independence with all transfers. | |||
* Initiate active range of motion/strengthening program. Individualize exercise programs according to each patient's needs, but generally include the following. '''Goals:''' Increase strength of involved extremity; increase independence with exercise program. | |||
** Supine: hip abduction and adduction, gluteal sets, quadriceps sets, straight leg raise, hip and knee flexion, short arc quadriceps, internal and external rotation. | |||
** Sitting: Long arc quadriceps, hip flexion, ankle pumps<ref>Physio treatment Hip Protocol Available from:https://www.physiotherapy-treatment.com/Femoral-Neck-Fracture-Physiotherapy.html (last accessed 15.10.2020)</ref>. | |||
* When internal fixation is performed, partial weight-bearing is recommended for a period of 8–10 weeks (according to the radiological evaluation of fracture healing), and after 3 months full weight-bearing should be allowed. | |||
* The patient can also begin strengthening exercises based on the surgeon's orders (typically six weeks post-op). | |||
Patients should also undergo [[Balance Training|balance]] and [[Proprioception|proprioceptive]] rehab and these abilities are quickly lost with inactivity. Rehabilitation classes for balance and [[Falls and Exercise|falls prevention]] are recommended. | |||
Weight-bearing exercises are very important for mobility, balance, activities of daily living and quality of life<ref>LeBlanc KE, Muncie Jr HL, LeBlanc LL. [https://www.aafp.org/afp/2014/0615/p945 Hip fracture: diagnosis, treatment, and secondary prevention]. American family physician. 2014 Jun 15;89(12):945-51. | |||
</ref>, examples: stepping in different directions, standing up and sitting down, tapping the foot and stepping onto and off a block. | |||
[[File:Hip Abduction with IR.JPG|right|frameless]] | |||
For patients who underwent a prosthetic replacement have to avoid the following for approximately 12 weeks: | |||
*Hip flexion greater than 70–90° | |||
*External rotation of the leg | |||
*Adduction of the leg past midline | |||
*Should not bend forward from the waist more than 90° | |||
'''Rehabilitation program components'''<ref>Latham NK, Harris BA, Bean JF, Heeren T, Goodyear C, Zawacki S, Heislein DM, Mustafa J, Pardasaney P, Giorgetti M, Holt N. [https://jamanetwork.com/journals/jama/article-abstract/1829991 Effect of a home-based exercise program on functional recovery following rehabilitation after hip fracture: a randomized clinical trial]. Jama. 2014 Feb 19;311(7):700-8. | |||
</ref>: | |||
*Hip extension (theraband and manual exercise) | |||
*Heel raises onto toes (theraband and manual exercise) | |||
*Resisted rowing (double arm lifting) (theraband and manual exercise) | |||
*Standing diagonal reach (theraband and manual exercise) | |||
*Modified get up and go (theraband and manual exercise) | |||
*Overhead arm extensions (theraband and manual exercise) | |||
*Repeated chair stands (vest and manual exercise) | |||
*Lunges - forward and back (vest and manual exercise) | |||
*Stepping up and down step (vest, manual exercise and plyometric step) | |||
*Calf raises - both legs and one leg (manual exercise) | |||
'''Importance of rehabilitation/home exercise program''': | |||
* Moderate to large improvements in physical performance and quality of life was found in patients who had a 10- week home-based progressive resistance exercise program<ref>Mangione KK, Craik RL, Palombaro KM, Tomlinson SS, Hofmann MT. [https://agsjournals.onlinelibrary.wiley.com/doi/abs/10.1111/j.1532-5415.2010.03076.x Home‐based leg‐strengthening exercise improves function 1 year after hip fracture: a randomized controlled study]. Journal of the American Geriatrics Society. 2010 Oct;58(10):1911-7.</ref> | |||
* A meta-analysis, showed that balance training within 6 months improves a person with hip fracture's physical functioning, gait, lower limb strength, performance task, and activity of daily living.<ref>Wu JQ, Mao LB, Wu J. [https://josr-online.biomedcentral.com/articles/10.1186/s13018-019-1125-x Efficacy of balance training for hip fracture patients: a meta-analysis of randomized controlled trials]. Journal of orthopaedic surgery and research. 2019 Dec;14(1):1-1.</ref> | |||
* Among patients who had completed standard rehabilitation after hip fracture, the use of a home-based functionally oriented exercise program resulted in modest improvement in physical function at 6 months after randomization.<ref>Latham NK, Harris BA, Bean JF, Heeren T, Goodyear C, Zawacki S, Heislein DM, Mustafa J, Pardasaney P, Giorgetti M, Holt N. [https://jamanetwork.com/journals/jama/article-abstract/1829991 Effect of a home-based exercise program on functional recovery following rehabilitation after hip fracture: a randomized clinical trial]. Jama. 2014 Feb 19;311(7):700-8. | |||
</ref> | |||
Education and prevention are also important issues to address. | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
== References == | == References == | ||
<references /> <br> | |||
[[Category:Vrije_Universiteit_Brussel_Project]] | |||
[[Category:Primary Contact]] | |||
[[Category:Older People/Geriatrics]] | |||
[[Category:Acute Care]] | |||
[[Category: | [[Category:Older People/Geriatrics - Conditions]] | ||
[[Category:Fractures]] | |||
[[Category:Conditions]] | |||
Latest revision as of 08:32, 14 December 2022
Introduction[edit | edit source]
Hip fractures are one of the most frequent fractures presenting to the emergency department and orthopedic trauma teams.
- The terms hip fracture and femoral neck fracture both relate to the same type of injury.
- Both terms describe a fracture of the proximal femur between the femoral head and 5 cm distal to the lesser trochanter.[1]
A hip fracture occurs just below the head of femur (HOF), the region of the femur called the femoral neck. A femoral neck fracture disconnects the HOF from the rest of the femur. Click Hip Anatomy for more details
Etiology[edit | edit source]
Most commonly:
- Falls in the elderly: Account for the majority of hip fractures. Risk factors for falls in the elderly population are many, those strongly associated with these fractures are a previous history of falls, gait abnormalities, the use of walking aids, vertigo, Parkinson disease, and antiepileptic medications. A lot of patients have multiple risk factors, and this, combined with age-associated reduced bone quality, is the underpinning cause of most hip fractures.[1] The majority of fragility hip fractures occurred inside the home[2]
- Significant trauma (e.g. motor vehicle collisions) in younger patients
- About 3% of hip fractures are related to localized bone weakness at the fracture site, secondary to tumour, followed by bone cysts, or Paget’s disease.
Epidemiology[edit | edit source]
The incidence of femoral neck fractures is increasing as the proportion of the elderly population in many countries increases. Between 1990 and 2000, there was nearly a 25% increase in hip fractures worldwide.[3]
- The peak number of hip fractures occurred at 75-79 years of age for both sexes, with most occuring in women. In white women, the lifetime risk of hip fracture is 1 in 6.
- Up to 20% of patients die in the first year following hip fractures, mostly due to pre-existing medical conditions. Less than half of those who survive the hip fracture regain their previous level of function[4]
Classification of Hip Fractures[edit | edit source]
Hip fractures is classified into intracapsular and extracapsular fractures[5]
- Intracapsular fractures (femoral neck fractures): Occurs within the hip capsule; accounts for 45% of all acute hip fractures in the elderly[6]; susceptible to malunion/avascular necrosis of the HOF because of the limited blood supply to the area. The Femoral Neck Fractures, Garden Classification is the most commonly classification system. This splits into four categories depending on the severity of the fracture and the degree of displacement.
- Extracapsular fractures: Intertrochanteric fracture: occurs between the greater and the lesser trochanter[5], intertrochanteric region has a good blood supply, avascular necrosis or nonunion is rare; Subtronchanteric fracture: occurs below the lesser trochanter, approximately 2.5 inches below.
Risk factors[edit | edit source]
Risk factors for hip fracture include[7][8]:
- Gender: prevalent in women; postmenopausal twice as likely as premenopausal to have hip fracture[9]
- Reduced Bone density[10]
- Falls[11]
- Medications: Some medications can cause a decrease in bone density like cortisone.
- Nutrition: It is well known that calcium and vitamin D increase bone mass, so a lack of it can cause several fractures, including hip fractures.
- Age: the older you get, the higher the risk is for hip fractures. 90% of these fractures occur in persons over 70 years old.
- Alcohol and tobacco: These products can reduce bone mass, causing a higher risk to have a hip fracture
- Medical problems: Endocrine disorders can cause fragility of the bones
- Physical inactivity: Physical activity is very important for muscle mass and bone mass
- Stroke increases the risk factor for falls which can cause a hip fracture.
- Parkinson’s disease increases the risk factor for falls which can cause a hip fracture.
Characteristics/Clinical Presentation[edit | edit source]
- Dull ache in the groin and/or hip region[12]
- Inability to put weight on the injured leg causing immobility right after the fall[13]
- Shorter leg on the side of the injured hip
- External rotation of the injured leg[13]
- Stiffness, bruising and swelling in and around the hip
Diagnostic Procedures[edit | edit source]
The diagnosis of a hip fracture is established based on patient history, physical examination, and radiography.[13]
- Plain radiographs (sensitivity 93-98%) is the first-line investigation for suspected Neck of Femur(NOF) fractures.
- In patients with a suspected occult NOF fracture, MRI (sensitivity 99-100%) is recommended by many institutions as the second-line test if available within 24 hours, with CT or nuclear medicine bone scan third-line[14]
Outcome Measures[edit | edit source]
- Functional Independence Measure
- Berg Balance Scale
- Timed Up and Go Test (TUG)
- Patient Specific Functional Scale
- Falls Risk Assessment Tool
Treatment[edit | edit source]
Serious complications (for example avascular necrosis and non-union) are very common without surgical intervention. In general, Garden stage I and II are stable fractures and can be treated with internal fixation (head-preservation) eg dymanic hip screw, and stage III and IV are unstable fractures and hence treated with arthroplasty (either hemi- or total arthroplasty. Internal fixation can be performed with multiple pins, intramedullary hip screw, crossed screw-nails or compression with a dynamic screw and plate.
The high morbidity and mortality associated with hip and pelvic fractures after trauma is well reported. Prognosis varies but is complicated by older age, as hip fractures increase the risk of death and major morbidity in the elderly.[3]
Rehabilitation[edit | edit source]
The postoperative rehabilitation is as important as the initial surgery. Surgery aims to restore mobility, and commence early mobilization. Patients who have undergone arthroplasty or fixation of an extracapsular fracture can usually mobilize immediately after surgery without weight restrictions. Following fixation of an intracapsular fracture protected weight bearing is often recommended to reduce the risk of subsequent fracture displacement.
Regular intensive physiotherapy is needed to encourage the rapid progression of mobility, aiming to restore the patient’s pre-morbid mobility status. Sadly, many patients do not regain their previous level of mobility or independence and therefore require social care input[1].
Physical Examination[edit | edit source]
On physical examination, findings on the patient with a hip fracture may include the following:
- limited and painful hip range of motion, especially in internal rotation.
- the injured leg is shortened, externally rotated, and abducted in the supine position
- Pain is noted upon attempted passive hip motion.
- Ecchymosis may or may not be present.
- An antalgic gait pattern may be present.
- Tenderness to palpation around the inguinal area, over the femoral neck. This area may also be swollen.
- Increased pain on the extremes of hip rotation, an abduction lurch, and an inability to stand on the involved leg
For more on details, Click Hip Examination
Physical Therapy Management[edit | edit source]
Rehabilitation begins promptly.
Two to three days postoperative
- Instruct patient in deep breathing and cough. Goal: Prevent postoperative pneumonia and atelectasis.
- Initiate isometrics and ankle pumps with involved extremity. Goal: Prepare patient for active exercise program.
- Initiate bedside sitting once physician has cleared patient for this activity. Goal: Prepare patient to begin transfer and progressive gait training processes.[15]
Three to five days postoperative
- Gait train patient, observing weight-bearing precautions. Progress to walker or crutches. Goal: Establish independent gait with assistive device, using proper gait pattern on all surfaces and stairs.
- Initiate training in activities of daily living, including bed mobility and transfers to and from bed and toilet. Goal: Achieve independence with all transfers.
- Initiate active range of motion/strengthening program. Individualize exercise programs according to each patient's needs, but generally include the following. Goals: Increase strength of involved extremity; increase independence with exercise program.
- Supine: hip abduction and adduction, gluteal sets, quadriceps sets, straight leg raise, hip and knee flexion, short arc quadriceps, internal and external rotation.
- Sitting: Long arc quadriceps, hip flexion, ankle pumps[16].
- When internal fixation is performed, partial weight-bearing is recommended for a period of 8–10 weeks (according to the radiological evaluation of fracture healing), and after 3 months full weight-bearing should be allowed.
- The patient can also begin strengthening exercises based on the surgeon's orders (typically six weeks post-op).
Patients should also undergo balance and proprioceptive rehab and these abilities are quickly lost with inactivity. Rehabilitation classes for balance and falls prevention are recommended.
Weight-bearing exercises are very important for mobility, balance, activities of daily living and quality of life[17], examples: stepping in different directions, standing up and sitting down, tapping the foot and stepping onto and off a block.
For patients who underwent a prosthetic replacement have to avoid the following for approximately 12 weeks:
- Hip flexion greater than 70–90°
- External rotation of the leg
- Adduction of the leg past midline
- Should not bend forward from the waist more than 90°
Rehabilitation program components[18]:
- Hip extension (theraband and manual exercise)
- Heel raises onto toes (theraband and manual exercise)
- Resisted rowing (double arm lifting) (theraband and manual exercise)
- Standing diagonal reach (theraband and manual exercise)
- Modified get up and go (theraband and manual exercise)
- Overhead arm extensions (theraband and manual exercise)
- Repeated chair stands (vest and manual exercise)
- Lunges - forward and back (vest and manual exercise)
- Stepping up and down step (vest, manual exercise and plyometric step)
- Calf raises - both legs and one leg (manual exercise)
Importance of rehabilitation/home exercise program:
- Moderate to large improvements in physical performance and quality of life was found in patients who had a 10- week home-based progressive resistance exercise program[19]
- A meta-analysis, showed that balance training within 6 months improves a person with hip fracture's physical functioning, gait, lower limb strength, performance task, and activity of daily living.[20]
- Among patients who had completed standard rehabilitation after hip fracture, the use of a home-based functionally oriented exercise program resulted in modest improvement in physical function at 6 months after randomization.[21]
Education and prevention are also important issues to address.
Clinical Bottom Line[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Emmerson BR, Varacallo M, Inman D. Hip Fracture Overview. InStatPearls [Internet] 2022 Feb 12. StatPearls Publishing.Available;https://www.statpearls.com/articlelibrary/viewarticle/22890/ (accessed 9.12.2022)
- ↑ Dhibar DP, Gogate Y, Aggarwal S, Garg S, Bhansali A, Bhadada SK. Predictors and outcome of fragility hip fracture: a prospective study from North India. Indian Journal of Endocrinology and Metabolism. 2019 May;23(3):282.
- ↑ 3.0 3.1 Radiopedia Neck of femur fracture Available:https://radiopaedia.org/articles/neck-of-femur-fracture-1?lang=us (accessed 9.12.2022)
- ↑ IOF Facts and stats Available from:https://www.iofbonehealth.org/facts-statistics#category-16 (last accessed 14.10.2020)
- ↑ 5.0 5.1 Zuckerman JD. Hip fracture. New England journal of medicine. 1996 Jun 6;334(23):1519-25.
- ↑ Canale ST. Campbell's Operative Orthopaedics. St. Louis, MO: Mosby;; 1998. pp. 2181–2223.
- ↑ Grisso JA, Kelsey JL, Strom BL, Ghiu GY, Maislin G, O'Brien LA, Hoffman S, Kaplan F. Risk factors for falls as a cause of hip fracture in women. New England journal of medicine. 1991 May 9;324(19):1326-31.
- ↑ http://www.mayoclinic.com/health/hip-fracture/DS00185/DSECTION=risk-factors (visited on april 2016)
- ↑ Banks E, Reeves GK, Beral V, Balkwill A, Liu B, Roddam A, Million Women Study Collaborators. Hip fracture incidence in relation to age, menopausal status, and age at menopause: prospective analysis. PLoS medicine. 2009 Nov 10;6(11):e1000181.
- ↑ Angthong C, Suntharapa T, Harnroongroj T. Major risk factors for the second contralateral hip fracture in the elderly. Acta orthopaedica et traumatologica turcica. 2009 May 1;43(3):193-8.
- ↑ Yang Y, Komisar V, Shishov N, Lo B, Korall AM, Feldman F, Robinovitch SN. The Effect Of Fall Biomechanics On Risk For Hip Fracture In Older Adults: A Cohort Study Of Video‐Captured Falls In Long‐Term Care. Journal of bone and mineral research. 2020 May 13.
- ↑ Rao SS, Cherukuri M. Management of hip fracture: the family physician's role. American family physician. 2006 Jun 15;73(12):2195-200.
- ↑ 13.0 13.1 13.2 Dinçel VE, Şengelen M, Sepici V, Çavuşoğlu T, Sepici B. The association of proximal femur geometry with hip fracture risk. Clinical Anatomy: The Official Journal of the American Association of Clinical Anatomists and the British Association of Clinical Anatomists. 2008 Sep;21(6):575-80.
- ↑ Radiopedia NOF fractures Available from:https://radiopaedia.org/articles/femoral-neck-fracture (last accessed 14.10.2020)
- ↑ Luciani D, Cadossi M, Mazzotti A, Chiarello E, Giannini S. The importance of rehabilitation after lower limb fractures in elderly osteoporotic patients. Aging clinical and experimental research. 2013 Oct;25(1):113-5.
- ↑ Physio treatment Hip Protocol Available from:https://www.physiotherapy-treatment.com/Femoral-Neck-Fracture-Physiotherapy.html (last accessed 15.10.2020)
- ↑ LeBlanc KE, Muncie Jr HL, LeBlanc LL. Hip fracture: diagnosis, treatment, and secondary prevention. American family physician. 2014 Jun 15;89(12):945-51.
- ↑ Latham NK, Harris BA, Bean JF, Heeren T, Goodyear C, Zawacki S, Heislein DM, Mustafa J, Pardasaney P, Giorgetti M, Holt N. Effect of a home-based exercise program on functional recovery following rehabilitation after hip fracture: a randomized clinical trial. Jama. 2014 Feb 19;311(7):700-8.
- ↑ Mangione KK, Craik RL, Palombaro KM, Tomlinson SS, Hofmann MT. Home‐based leg‐strengthening exercise improves function 1 year after hip fracture: a randomized controlled study. Journal of the American Geriatrics Society. 2010 Oct;58(10):1911-7.
- ↑ Wu JQ, Mao LB, Wu J. Efficacy of balance training for hip fracture patients: a meta-analysis of randomized controlled trials. Journal of orthopaedic surgery and research. 2019 Dec;14(1):1-1.
- ↑ Latham NK, Harris BA, Bean JF, Heeren T, Goodyear C, Zawacki S, Heislein DM, Mustafa J, Pardasaney P, Giorgetti M, Holt N. Effect of a home-based exercise program on functional recovery following rehabilitation after hip fracture: a randomized clinical trial. Jama. 2014 Feb 19;311(7):700-8.