Behcet Disease: Difference between revisions
m (Image caption edit) |
m (Sehriban Ozmen moved page Behcet's Disease to Behcet Disease: The page title includes an apostrophe.) |
||
| (9 intermediate revisions by the same user not shown) | |||
| Line 3: | Line 3: | ||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
| Line 27: | Line 23: | ||
== Pathological Process == | == Pathological Process == | ||
The etiology is unknown <ref name=":0" /> <ref name=":2">Rodríguez-Carrio J, Nucera V, Masala IF, Atzeni F. Behçet disease: from pathogenesis to novel therapeutic options. Pharmacological Research. 2021 May 1;167:105593.</ref> and extensive debate existed on whether to classify it as autoimmune or autoinflammatory but recently classified as the major histocompatibility complex class I (MHC-I) opathy <ref name=":2" />. Genetic factors are thought to play a crucial role since strong association with HLA-B51 antigen is proved <ref>Ohno S, Ohguchi M, Hirose S, Matsuda H, Wakisaka A, Aizawa M. Close association of HLA-Bw51 with Behçet's disease. Archives of ophthalmology. 1982 Sep 1;100(9):1455-8. | The etiology is unknown <ref name=":0" /> <ref name=":2">Rodríguez-Carrio J, Nucera V, Masala IF, Atzeni F. Behçet disease: from pathogenesis to novel therapeutic options. Pharmacological Research. 2021 May 1;167:105593.</ref> and extensive debate existed on whether to classify it as autoimmune or autoinflammatory but recently classified as the major histocompatibility complex class I (MHC-I) opathy <ref name=":2" />. Genetic factors are thought to play a crucial role since strong association with HLA-B51 antigen is proved <ref>Ohno S, Ohguchi M, Hirose S, Matsuda H, Wakisaka A, Aizawa M. Close association of HLA-Bw51 with Behçet's disease. Archives of ophthalmology. 1982 Sep 1;100(9):1455-8.</ref><ref>Ohno S, Aoki K, Sugiura S, Nakayama E, Itakura K, Aizawa M. HL-A5 and Behcet's disease. The Lancet. 1973 Dec 15;302(7842):1383-4.</ref><ref name=":0" /><ref name=":1" /> as well as higher prevalence in specific ethnic populations, and high sibling recurrence rate. <ref name=":1" /> | ||
== Clinical Presentation == | == Clinical Presentation == | ||
[[File:Oral ulcer in Behcet Syndrome.jpg|thumb|Oral ulcer in Behcet Syndrome]] | [[File:Oral ulcer in Behcet Syndrome.jpg|thumb|Oral ulcer in Behcet Syndrome]] | ||
| Line 43: | Line 35: | ||
</ref> | </ref> | ||
* '''Neurologic involvement''': The manifestations include focal or multifocal parenchymal involvement, isolated cerebral venous sinus thrombosis, intracranial hypertension, isolated behavioural syndromes, peripheral nervous system involvement, and secondary neurologic involvement. <ref name=":3" /> The combination of neurologic symptoms and/or signs in patients diagnosed with BD is called Neuro-Behcet's disease (NBD). <ref>Borhani-Haghighi A, Kardeh B, Banerjee S, Yadollahikhales G, Safari A, Sahraian MA, Shapiro L. Neuro-Behcet's disease: an update on diagnosis, differential diagnoses, and treatment. Multiple sclerosis and related disorders. 2020 Apr 1;39:101906. | * '''Neurologic involvement''': The manifestations include focal or multifocal parenchymal involvement, isolated cerebral venous sinus thrombosis, intracranial hypertension, isolated behavioural syndromes, peripheral nervous system involvement, and secondary neurologic involvement. <ref name=":3" /> The combination of neurologic symptoms and/or signs in patients diagnosed with BD is called Neuro-Behcet's disease (NBD). <ref>Borhani-Haghighi A, Kardeh B, Banerjee S, Yadollahikhales G, Safari A, Sahraian MA, Shapiro L. Neuro-Behcet's disease: an update on diagnosis, differential diagnoses, and treatment. Multiple sclerosis and related disorders. 2020 Apr 1;39:101906.</ref> NBD is a serious risk for mortality and usually occurs in males. <ref>Benamour S, Naji T, Alaoui FZ, El Kabli H, El Aidouni S. Manifestations neurologiques de la maladie de Behçet. Revue Neurologique. 2006 Nov 1;162(11):1084-90.</ref><ref name=":1" /> | ||
* '''Pulmonary involvement:''' Pulmonary artery aneurism, pulmonary infection, pulmonary vasculitis, [[Pulmonary Fibrosis|pulmonary fibrosis]], pleuritis, and [[Pulmonary Embolism|pulmonary emboli]]. <ref name=":3" /> | * '''Pulmonary involvement:''' Pulmonary artery aneurism, pulmonary infection, pulmonary vasculitis, [[Pulmonary Fibrosis|pulmonary fibrosis]], pleuritis, and [[Pulmonary Embolism|pulmonary emboli]]. <ref name=":3" /> | ||
| Line 59: | Line 49: | ||
* Skin lesions | * Skin lesions | ||
* Positive pathergy test <ref>Wechsler FB, Davatchi F. Criteria for diagnosis of Behcet's disease. The Lancet. 1990;335(8697):1078-80.</ref> | * Positive pathergy test <ref>Wechsler FB, Davatchi F. Criteria for diagnosis of Behcet's disease. The Lancet. 1990;335(8697):1078-80.</ref> | ||
=== | == Outcome Measures == | ||
A recent study <ref name=":1" /> summarised the outcome measures based on a systematic review by The Outcome Measures in Rheumatology (OMERACT) Vasculitis Working Group <ref>Hatemi G, Merkel PA, Hamuryudan V, Boers M, Direskeneli H, Aydin SZ, Yazici H. [https://www.jrheum.org/content/41/3/599 Outcome measures used in clinical trials for Behçet syndrome: a systematic review]. The Journal of rheumatology. 2014 Mar 1;41(3):599-612. | |||
</ref>: | |||
* Behçet's Disease Current Activity Form (BDCAF) | |||
* Clinical Disease Activity Index | |||
* Clinical Manifestations Index | |||
* Iranian BD Dynamic Activity Measure, | |||
* 1994 Criteria for Disease Activity of BD | |||
* Krause's Total Severity Score | |||
* BD Quality of Life | |||
* Oral Ulcer Composite Index | |||
However, it also indicated that: | |||
* Most of the measures used in the studies were not properly validated, and standard definitions were absent for outcome variables like response, relapse, or remission. | |||
For the disease | * Even though specific outcome measures were developed for BD, they were not widely used in studies. For instance, BDCAF, which is the most commonly used disease activity measure, has been used in only 10% of the studies. | ||
* Internet-based surveys conducted by the OMERACT Vasculitis Working Group among expert physicians from relevant specialities from multiple countries <ref>Hatemi G, Ozguler Y, Direskeneli H, Mahr A, Gul A, Levi V, Aydin SZ, Mumcu G, Sertel-Berk O, Stevens RM, Yazici H. [https://www.jrheum.org/content/42/12/2436 Current status, goals, and research agenda for outcome measures development in Behçet syndrome: report from OMERACT 2014]. The Journal of rheumatology. 2015 Dec 1;42(12):2436-41. | |||
</ref> have emphasized the need for widely acceptable and properly validated outcome measures for BD. | |||
== | == Management / Interventions == | ||
== | === Multidisciplinary Team === | ||
* Treatment and follow-up are ideally coordinated by a paediatrician or adult practice physician with expertise in BD. This is most often an internal medicine specialist, dermatologist, or rheumatologist. The general physician or pediatrician plays a crucial role in optimizing the coordination of the proposed care plan. <ref name=":4">Kone-Paut I, Barete S, Bodaghi B, Deiva K, Desbois AC, Galeotti C, Gaudric J, Kaplanski G, Mahr A, Noel N, Piram M. [https://link.springer.com/article/10.1186/s13023-020-01620-4 French recommendations for the management of Behçet’s disease]. Orphanet journal of rare diseases. 2021 Feb;16:1-28. | |||
</ref> | |||
* Other specialized physicians such as ophthalmologists, neurologists, vascular physicians, gastroenterologists, and pulmonologists may also be involved in patient care. <ref name=":4" /> | |||
* Other health professionals such as those in therapeutic education, dietitians, state-certified nurses, physiotherapists, occupational therapists, psychologists, and social welfare assistants may also be involved upon as necessary. <ref name=":4" /> | |||
=== Medical Management === | |||
* In the treatment and secondary prevention of thrombosis in Behcet's Disease, immunosuppressants are currently preferred over anticoagulants. <ref>Bettiol A, Alibaz-Oner F, Direskeneli H, Hatemi G, Saadoun D, Seyahi E, Prisco D, Emmi G. Vascular Behçet syndrome: from pathogenesis to treatment. Nature Reviews Rheumatology. 2023 Feb;19(2):111-26.</ref> | |||
* Recently, Apremilast has been approved for the treatment of oral ulcers in Behcet's Syndrome in the United States. The efficacy of Apremilast in controlling non-oral ulcer features of the syndrome is still under investigation. <ref name=":5">Yazici Y. Management of Behçet syndrome. Current opinion in rheumatology. 2020 Jan 1;32(1):35-40. | |||
* | </ref> | ||
* Tumor necrosis factor inhibitors have proven to be safe and effective for treating eye disease in Behcet's Syndrome with long-term use. <ref name=":5" /> | |||
* While new treatment options such as ustekinumab, secukinumab, tocilizumab, and others show promising early data, more studies are needed to better understand their role in Behcet's management. <ref name=":5" /> | |||
* | |||
=== Physical Therapy === | |||
To prevent cortisone myopathy, patients should be advised to engage in regular physical activities, such as fast walking for 30 to 45 minutes each day. If they are diagnosed with amyotrophy, they may even need to undergo kinesiology therapy to strengthen their muscles. Engaging in physical activity is also crucial in preventing cortisone-induced [[osteoporosis]]. <ref name=":4" /> | |||
== Differential Diagnosis == | |||
{| class="wikitable" | |||
|+Table 1: The differential diagnoses of BD according to system involvement | |||
!'''System Involvement''' | |||
!'''Differential Diagnoses''' | |||
|- | |||
|Mucocutaneous involvement | |||
|[[Herpes Zoster|Herpes]], [[neutropenia]], pemphigus, Chronic Intestinal Inflammatory Disease (CIID), drugs, vitamin deficiencies <ref name=":4" /> | |||
|- | |||
|Musculoskeletal involvement | |||
|[[Systemic Lupus Erythematosus]], [[Reactive Arthritis]], [[Psoriatic Arthritis]], [[Ankylosing Spondylitis (Axial Spondyloarthritis)|Ankylosing Spondylitis]], [[Juvenile Idiopathic Arthritis]], [[Sarcoidosis]], Inflammatory Bowel Diseases <ref name=":3" /> | |||
|- | |||
|Vascular involvement | |||
|Septic aneurysms, atrophic polychondritis, Takayasu <ref name=":4" /> | |||
|- | |||
|Gastrointestinal involvement | |||
|Inflammatory Bowel Disease, [[Crohn's Disease]], [[Peptic Ulcers|Peptic Ulcer]], Reiter's Syndrome, Ulcerative Colitis, CIID, NSAID toxicity, infectious colitis <ref name=":3" /><ref name=":4" /> | |||
|- | |||
|Neurologic involvement | |||
|[[Multiple Sclerosis (MS)|Multiple Sclerosis]], [[sarcoidosis]], tumoral pathologies, [[Lymphoma|lymphomas]], infectious [[meningoencephalitis]] <ref name=":4" /> | |||
|} | |||
== '''Case Studies''' == | == '''Case Studies''' == | ||
| Line 121: | Line 130: | ||
*John Hopkins: Vasculitis Center: http://www.hopkinsvasculitis.org/types-vasculitis/behcets-disease/ | *John Hopkins: Vasculitis Center: http://www.hopkinsvasculitis.org/types-vasculitis/behcets-disease/ | ||
*An Employer's Guide from the Behçet’s UK organisation: https://behcetsuk.org/wp-content/uploads/2019/06/BUK-Employers-Guide-v2.0-Jun19.pdf | *An Employer's Guide from the Behçet’s UK organisation: https://behcetsuk.org/wp-content/uploads/2019/06/BUK-Employers-Guide-v2.0-Jun19.pdf | ||
*A presentation of Dr. Erkan Demirkaya from the 2nd NIH-WRNMMC Symposium on Autoinflammatory and Immunedysregulatory Diseases, held at NIH on August 22 and 23, 2019: | |||
{{#ev:youtube|DOWOpBVx0k0}}<ref>The National Institute of Allergy and Infectious Diseases (NIAID). Diagnosis and Management of Behçet’s Disease. Available from: https://www.youtube.com/watch?v=DOWOpBVx0k0</ref> | |||
== References == | == References == | ||
Latest revision as of 16:40, 9 September 2023
Top Contributors - Jennifer Edwards, Sehriban Ozmen, Elaine Lonnemann, Admin, Kim Jackson, 127.0.0.1, Laura Ritchie, Wendy Walker, WikiSysop and Lucinda hampton
Definition/Description[edit | edit source]
"Behcet's Disease" (BD) is a chronic disease characterized by inflammation in the blood vessels and relapsing and remitting course. [1] It can also be referred as a "Behcet Syndrome" since it involves different body systems such as skin, mucosa, joints, nervous and gastrointestinal systems. [2]
The video below is a great introduction to the condition provided by the American Behcet's Disease Association (ABDA), featuring educational information and patients' stories.
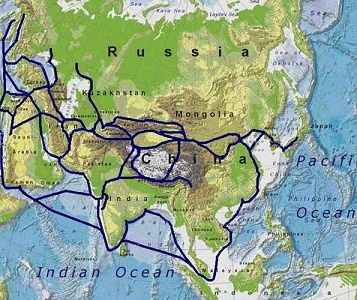
Prevalence[edit | edit source]
The prevalence is variable worldwide [4] but higher in the countries along the Silk Road. [1][4] A recent study calculated the prevalence of BD as 10.3 per 100,000 population globally and 119.8 for Turkey, 31.8 for the Middle East, 4.5 for Asia, 5.3 for Southern Europe, 2.1 for Northern Europe, and 3.8 for North America/Caribbean Islands. [5]
Pathological Process[edit | edit source]
The etiology is unknown [1] [6] and extensive debate existed on whether to classify it as autoimmune or autoinflammatory but recently classified as the major histocompatibility complex class I (MHC-I) opathy [6]. Genetic factors are thought to play a crucial role since strong association with HLA-B51 antigen is proved [7][8][1][4] as well as higher prevalence in specific ethnic populations, and high sibling recurrence rate. [4]
Clinical Presentation[edit | edit source]
Vasculitis in BD can involve any kind and size of vessels, and this explains why the disease can have an effect on multiple systems in the body. [9] So, the patient could present with any of the symptom(s) below:
- Mucocutaneous involvement: Oral aphthosis, genital aphthosis, papulopustular lesions, pathergy phenomenon, erythema-nodosu-like lesions, superficial thrombophlebitis, pyodermagangrenosum-like lesions, erythemamultiforme-like lesions, nailfold capillary abnormalities. [9]
- Ocular involvement: Uveitis, vitritis, retinal infiltrates, sheathing of retinal veins, occlusive vasculitis, neovascularization, secondary cataracts, glaucoma, frosted branch angiitis and macular oedema, conjunctivitis, and conjunctival aphthosis, and scleritis being less common. [9] Ocular involvement is the most common cause of morbidity in people with BD. [10]
- Musculoskeletal involvement: Arthritis, arthralgia, enthesopathy, avascular necrosis, myalgia, and myositis. [9]
- Vascular involvement: Pulmonary, carotid, aortic, iliac, femoral, and popliteal arterial involvement; pulmonary aneurysm; superficial and deep vein thrombosis; Budd-Chiari syndrome; superior and inferior vena cava occlusion; and dural sinus thrombosis. [9]
- Cardiac involvement: Pericarditis, myocarditis, endocarditis with valvular regurgitation, coronary arteritis, coronary artery aneurysms, diastolic dysfunction, atrial septal aneurysm, conduction system disturbances, atrial and ventricular arrhythmias, mitral valve prolapse, intracardiac thrombosis, valvular insufficiency, and myocardial infarction. [9]
- Gastrointestinal (GI) involvement: The most common symptoms are abdominal pain, nausea, vomiting, diarrhoea, and GI bleeding. The GI manifestations of BD are known to cause significant morbidity and mortality. [11] [12]
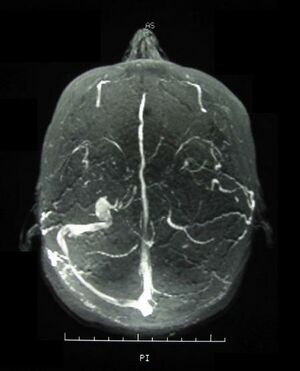
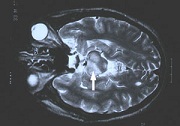
- Neurologic involvement: The manifestations include focal or multifocal parenchymal involvement, isolated cerebral venous sinus thrombosis, intracranial hypertension, isolated behavioural syndromes, peripheral nervous system involvement, and secondary neurologic involvement. [9] The combination of neurologic symptoms and/or signs in patients diagnosed with BD is called Neuro-Behcet's disease (NBD). [13] NBD is a serious risk for mortality and usually occurs in males. [14][4]
- Pulmonary involvement: Pulmonary artery aneurism, pulmonary infection, pulmonary vasculitis, pulmonary fibrosis, pleuritis, and pulmonary emboli. [9]
Diagnostic Procedures[edit | edit source]
Since there is no specific biomarker for BD, the diagnosis process is based on the clinical picture. [4] Although more than fifteen classification criteria have been proposed for BD to date [15], the most frequently used one in studies has been the International Study Group (ISG) Criteria with 92% sensitivity and 97% specificity[16][17], which was set in 1990. Accordingly, the criteria to be met are:
- Oral ulcerations at least three times in one year.
- Plus any two of the following:
- Recurring genital ulceration
- Eye lesions
- Skin lesions
- Positive pathergy test [18]
Outcome Measures[edit | edit source]
A recent study [4] summarised the outcome measures based on a systematic review by The Outcome Measures in Rheumatology (OMERACT) Vasculitis Working Group [19]:
- Behçet's Disease Current Activity Form (BDCAF)
- Clinical Disease Activity Index
- Clinical Manifestations Index
- Iranian BD Dynamic Activity Measure,
- 1994 Criteria for Disease Activity of BD
- Krause's Total Severity Score
- BD Quality of Life
- Oral Ulcer Composite Index
However, it also indicated that:
- Most of the measures used in the studies were not properly validated, and standard definitions were absent for outcome variables like response, relapse, or remission.
- Even though specific outcome measures were developed for BD, they were not widely used in studies. For instance, BDCAF, which is the most commonly used disease activity measure, has been used in only 10% of the studies.
- Internet-based surveys conducted by the OMERACT Vasculitis Working Group among expert physicians from relevant specialities from multiple countries [20] have emphasized the need for widely acceptable and properly validated outcome measures for BD.
Management / Interventions[edit | edit source]
Multidisciplinary Team[edit | edit source]
- Treatment and follow-up are ideally coordinated by a paediatrician or adult practice physician with expertise in BD. This is most often an internal medicine specialist, dermatologist, or rheumatologist. The general physician or pediatrician plays a crucial role in optimizing the coordination of the proposed care plan. [21]
- Other specialized physicians such as ophthalmologists, neurologists, vascular physicians, gastroenterologists, and pulmonologists may also be involved in patient care. [21]
- Other health professionals such as those in therapeutic education, dietitians, state-certified nurses, physiotherapists, occupational therapists, psychologists, and social welfare assistants may also be involved upon as necessary. [21]
Medical Management[edit | edit source]
- In the treatment and secondary prevention of thrombosis in Behcet's Disease, immunosuppressants are currently preferred over anticoagulants. [22]
- Recently, Apremilast has been approved for the treatment of oral ulcers in Behcet's Syndrome in the United States. The efficacy of Apremilast in controlling non-oral ulcer features of the syndrome is still under investigation. [23]
- Tumor necrosis factor inhibitors have proven to be safe and effective for treating eye disease in Behcet's Syndrome with long-term use. [23]
- While new treatment options such as ustekinumab, secukinumab, tocilizumab, and others show promising early data, more studies are needed to better understand their role in Behcet's management. [23]
Physical Therapy[edit | edit source]
To prevent cortisone myopathy, patients should be advised to engage in regular physical activities, such as fast walking for 30 to 45 minutes each day. If they are diagnosed with amyotrophy, they may even need to undergo kinesiology therapy to strengthen their muscles. Engaging in physical activity is also crucial in preventing cortisone-induced osteoporosis. [21]
Differential Diagnosis[edit | edit source]
| System Involvement | Differential Diagnoses |
|---|---|
| Mucocutaneous involvement | Herpes, neutropenia, pemphigus, Chronic Intestinal Inflammatory Disease (CIID), drugs, vitamin deficiencies [21] |
| Musculoskeletal involvement | Systemic Lupus Erythematosus, Reactive Arthritis, Psoriatic Arthritis, Ankylosing Spondylitis, Juvenile Idiopathic Arthritis, Sarcoidosis, Inflammatory Bowel Diseases [9] |
| Vascular involvement | Septic aneurysms, atrophic polychondritis, Takayasu [21] |
| Gastrointestinal involvement | Inflammatory Bowel Disease, Crohn's Disease, Peptic Ulcer, Reiter's Syndrome, Ulcerative Colitis, CIID, NSAID toxicity, infectious colitis [9][21] |
| Neurologic involvement | Multiple Sclerosis, sarcoidosis, tumoral pathologies, lymphomas, infectious meningoencephalitis [21] |
Case Studies[edit | edit source]
- Regional distinction for the clinical severity of Behcet's disease in Korea: four university-based medical centre studies. [24][view article in Clinical and Experimental Rheumatology, 2010]
- Clinical manifestations of Behcet's disease: an analysis of 2147 patients [25] [view article in Yonsei Medical Journal]
- Clinical patterns of neurological involvement in Behçet's disease: evaluation of 200 patients
- Aortic valve replacement in Behcet’s disease: surgical modification to prevent valve detachment
Resources[edit | edit source]
- American Behcet's Disease Association: http://www.behcets.com/site/pp.asp?c=bhJIJSOCJrH&b=260521
- Medicine Net: Bechet's Disease: http://www.medicinenet.com/behcets_syndrome/article.htm
- Mayo Clinic: Behcet's Disease: http://www.mayoclinic.com/health/behcets-disease/DS00822
- John Hopkins: Vasculitis Center: http://www.hopkinsvasculitis.org/types-vasculitis/behcets-disease/
- An Employer's Guide from the Behçet’s UK organisation: https://behcetsuk.org/wp-content/uploads/2019/06/BUK-Employers-Guide-v2.0-Jun19.pdf
- A presentation of Dr. Erkan Demirkaya from the 2nd NIH-WRNMMC Symposium on Autoinflammatory and Immunedysregulatory Diseases, held at NIH on August 22 and 23, 2019:
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Alpsoy E, Bozca BC, Bilgic A. Behçet disease: an update for dermatologists. American Journal of Clinical Dermatology. 2021 Jul;22(4):477-502.
- ↑ Bettiol A, Prisco D, Emmi G. Behçet: the syndrome. Rheumatology. 2020 May 1;59(Supplement_3):iii101-7.
- ↑ Bechet's Disease Explained. Available from http://www.youtube.com/watch?v=Txf7cWW8HwI [accessed 28/98/19]
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Akkoç N. Update on the epidemiology, risk factors and disease outcomes of Behçet's disease. Best Practice & Research Clinical Rheumatology. 2018 Apr 1;32(2):261-70.
- ↑ Maldini C, Druce K, Basu N, LaValley MP, Mahr A. Exploring the variability in Behçet’s disease prevalence: a meta-analytical approach. Rheumatology. 2018 Jan 1;57(1):185-95.
- ↑ 6.0 6.1 Rodríguez-Carrio J, Nucera V, Masala IF, Atzeni F. Behçet disease: from pathogenesis to novel therapeutic options. Pharmacological Research. 2021 May 1;167:105593.
- ↑ Ohno S, Ohguchi M, Hirose S, Matsuda H, Wakisaka A, Aizawa M. Close association of HLA-Bw51 with Behçet's disease. Archives of ophthalmology. 1982 Sep 1;100(9):1455-8.
- ↑ Ohno S, Aoki K, Sugiura S, Nakayama E, Itakura K, Aizawa M. HL-A5 and Behcet's disease. The Lancet. 1973 Dec 15;302(7842):1383-4.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 9.8 9.9 Akdeniz N, Elmas ÖF, Karadağ AS. Behçet syndrome: A great imitator. Clinics in Dermatology. 2019 May 1;37(3):227-39.
- ↑ Davatchi F, Chams-Davatchi C, Shams H, Shahram F, Nadji A, Akhlaghi M, Faezi T, Ghodsi Z, Sadeghi Abdollahi B, Ashofteh F, Mohtasham N. Behcet’s disease: epidemiology, clinical manifestations, and diagnosis. Expert review of clinical immunology. 2017 Jan 2;13(1):57-65.
- ↑ Nguyen A, Upadhyay S, Javaid MA, Qureshi AM, Haseeb S, Javed N, Cormier C, Farooq A, Sheikh AB. Behcet’s disease: an in-depth review about pathogenesis, gastrointestinal manifestations, and management. Inflammatory Intestinal Diseases. 2021 Nov 4;6(4):175-85.
- ↑ Skef W, Hamilton MJ, Arayssi T. Gastrointestinal Behçet's disease: a review. World Journal of Gastroenterology: WJG. 2015 Apr 4;21(13):3801.
- ↑ Borhani-Haghighi A, Kardeh B, Banerjee S, Yadollahikhales G, Safari A, Sahraian MA, Shapiro L. Neuro-Behcet's disease: an update on diagnosis, differential diagnoses, and treatment. Multiple sclerosis and related disorders. 2020 Apr 1;39:101906.
- ↑ Benamour S, Naji T, Alaoui FZ, El Kabli H, El Aidouni S. Manifestations neurologiques de la maladie de Behçet. Revue Neurologique. 2006 Nov 1;162(11):1084-90.
- ↑ Davatchi F, Sadeghi Abdollahi B, Chams‐Davatchi C, Shahram F, Shams H, Nadji A, Faezi T, Akhlaghi M, Ghodsi Z, Mohtasham N, Ashofteh F. The saga of diagnostic/classification criteria in Behcet's disease. International journal of rheumatic diseases. 2015 Jul;18(6):594-605.
- ↑ Wechsler FB, Davatchi F. Criteria for diagnosis of Behcet's disease. The Lancet. 1990;335(8697):1078-80.
- ↑ International Study Group for Behçet's Disease, Wechsler B, Davatchi F, Mizushima Y, Hamza M, Dilsen N, Kansu E, yazici H, Barnes CG, Chamberlain MA, James DG. Evaluation of diagnostic (‘classification’) criteria in Behçet's disease—towards internationally agreed criteria. Rheumatology. 1992 May 1;31(5):299-308.
- ↑ Wechsler FB, Davatchi F. Criteria for diagnosis of Behcet's disease. The Lancet. 1990;335(8697):1078-80.
- ↑ Hatemi G, Merkel PA, Hamuryudan V, Boers M, Direskeneli H, Aydin SZ, Yazici H. Outcome measures used in clinical trials for Behçet syndrome: a systematic review. The Journal of rheumatology. 2014 Mar 1;41(3):599-612.
- ↑ Hatemi G, Ozguler Y, Direskeneli H, Mahr A, Gul A, Levi V, Aydin SZ, Mumcu G, Sertel-Berk O, Stevens RM, Yazici H. Current status, goals, and research agenda for outcome measures development in Behçet syndrome: report from OMERACT 2014. The Journal of rheumatology. 2015 Dec 1;42(12):2436-41.
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 21.6 21.7 Kone-Paut I, Barete S, Bodaghi B, Deiva K, Desbois AC, Galeotti C, Gaudric J, Kaplanski G, Mahr A, Noel N, Piram M. French recommendations for the management of Behçet’s disease. Orphanet journal of rare diseases. 2021 Feb;16:1-28.
- ↑ Bettiol A, Alibaz-Oner F, Direskeneli H, Hatemi G, Saadoun D, Seyahi E, Prisco D, Emmi G. Vascular Behçet syndrome: from pathogenesis to treatment. Nature Reviews Rheumatology. 2023 Feb;19(2):111-26.
- ↑ 23.0 23.1 23.2 Yazici Y. Management of Behçet syndrome. Current opinion in rheumatology. 2020 Jan 1;32(1):35-40.
- ↑ Choe JY, Chung WT, Lee SW, et al. Regional distinction for the clinical severity of Behcet’s disease in Korea: four university-based medical centre studies. Clinical and experimental rheumatology. 2010;28:S20-S26.
- ↑ Gurler A, Boyvat A, Tursen U. Clinical manifestations of Behcet’s disease: an analysis of 2147 patients. Yonsei Medical Journal. 1997; 38:423-427.
- ↑ The National Institute of Allergy and Infectious Diseases (NIAID). Diagnosis and Management of Behçet’s Disease. Available from: https://www.youtube.com/watch?v=DOWOpBVx0k0