Sacroiliac Joint Syndrome: Difference between revisions
Kim Jackson (talk | contribs) m (Text replacement - "[[Ankylosing Spondylitis|" to "[[Ankylosing Spondylitis (Axial Spondyloarthritis)|") |
(A recommindation by one researcher) |
||
| (18 intermediate revisions by 3 users not shown) | |||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
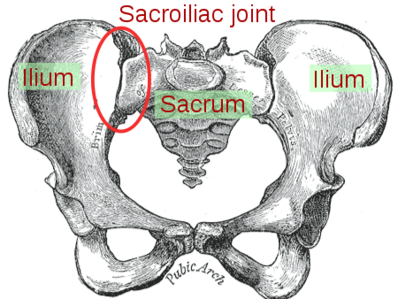
[[File: | [[File:Sacroiliac joint.png|right|frameless|398x398px]] | ||
Sacroiliac joint dysfunction | Sacroiliac joint dysfunction is a term used to describe the pain of the [[Sacroiliac Joint|sacroiliac joint]] (SI joint). It is usually caused by abnormal motion (i.e. hyper- or hypo-mobile) or malalignment of the sacroiliac joint. Sacroiliac joint syndrome is a significant source of pain in 15% to 30% of people with mechanical [[Low Back Pain|low back pain]]. | ||
[[Sacroiliitis]] is not the same as SI joint dysfunction. Sacroiliitis is specific to an inflammatory processes present in the SI joint and the pain sensed is a direct result of those inflammatory processes, whereas sacroiliac joint dysfunction is a condition caused by abnormal motion or slight mispositioning of the SI joint. | |||
Sacroiliac joint syndrome is a condition that is difficult to diagnose and is often overlooked by physicians and physiotherapists.<ref name="bron2">SLIPMAN W.C. Sacroiliac Joint Syndrome. Pain Physician. Vol. 4, N° 2, p 143-152, 2001. ISSN 1533-3159</ref> | Sacroiliac joint syndrome is a condition that is difficult to diagnose and is often overlooked by physicians and physiotherapists.<ref name="bron2">SLIPMAN W.C. Sacroiliac Joint Syndrome. Pain Physician. Vol. 4, N° 2, p 143-152, 2001. ISSN 1533-3159</ref> | ||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
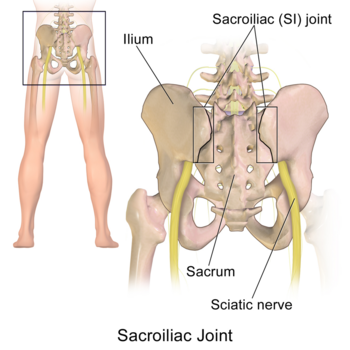
[[Sacroiliac Joint|The sacroiliac joints]] are located on each side of the spine between the two pelvic bones, which attach to the [[sacrum]].<ref name="bron3">OLIVER J., MIDDLEDITCH A. Functional anatomy of the spine. Elsevier Science, p 190-191; 195-198, 2004</ref> | [[File:Sacroiliac Joint human.png|right|frameless|350x350px]] | ||
[[Sacroiliac Joint|The sacroiliac joints]] are located on each side of the spine between the two pelvic bones, which attach to the [[sacrum]].<ref name="bron3">OLIVER J., MIDDLEDITCH A. Functional anatomy of the spine. Elsevier Science, p 190-191; 195-198, 2004</ref> The main function within the [[Biomechanics and Dynamics of the Pelvic Girdle|pelvic girdle]] is to provide shock absorption for the spine and to transmit forces between the upper body and the lower limbs.<ref name="bron6">http://www.orthonc.com/education-research/spine/patient-education-spine-sacroiliac-joint-syndrome (accessed on 22/10/2011)</ref> | |||
The SI joint experiences forces of shearing, torsion, rotation, and tension. Ambulation is heavily impacted by the SI joint, as this is the only orthopedic joint connecting the upper body to our lower body. The joint is a relatively stiff synovial joint filled with synovial fluid. The bones of the sacrum and ilium are coated in hyaline cartilage at their articular surfaces with dense fibrous tissue connecting the ilium and the sacrum. SI joints typically only have a few degrees of motion<ref name=":1">Dydyk AM, Forro SD, Hanna A. Sacroiliac Joint Injury.Available:https://www.ncbi.nlm.nih.gov/books/NBK557881/ (accessed 6.6.2022)</ref>. | |||
== Etiology == | |||
Injuries to the sacroiliac joint can occur from various etiologies. | |||
# 88% of cases of SI joint injury are due to either repetitive microtrauma or acute trauma. There is a high prevalence of SI joint injury in athletes. Trauma in the context of pelvic ring injuries is one example of SI joint injury. [[Pelvic Fractures|Pelvic ring traumatic injuries]] and [[Pelvic Fractures:Low Impact|low impact Pelvic]] fractures can be read about here. | |||
# 20% of cases are pregnancy-related. Female hormones are released during pregnancy, relaxing the sacroiliac ligaments. This stretching in ligaments results in changes to the sacroiliac joints, making them hypermobile.<ref name="bron6" /> After the fifth decade of life, the sacroiliac joint fuses.<ref name=":0">Raj MA, Varacallo M. [https://www.ncbi.nlm.nih.gov/books/NBK470299/ Sacroiliac (SI) Joint Pain.] InStatPearls [Internet] 2019 May 12. StatPearls Publishing Availabe from:.https://www.ncbi.nlm.nih.gov/books/NBK470299/ (last accessed 14.6.2020)</ref> | |||
# 4% are idiopathic.<ref name=":1" /> | |||
# Pain can also be caused by an abnormality of the [[sacrum]] bone, which can be seen on X-rays. | |||
== Epidemiology == | == Epidemiology == | ||
[[File:SI pain.jpg|alt=|thumb|200x200px|Pregnancy]] | |||
Approximately 90% of the population will at some experience or present to the clinic with some form of low back pain/pathology. About 10% to 25% of these patients are thought to be experiencing pain from the SI joint. The majority of SI joint pathologies affect the adult patient population. | Approximately 90% of the population will at some experience or present to the clinic with some form of low back pain/pathology. About 10% to 25% of these patients are thought to be experiencing pain from the SI joint. The majority of SI joint pathologies affect the adult patient population. | ||
* The majority of individuals affected by sacroiliac joint pain are adults. The disorder is most common in individuals who lead a sedentary lifestyle. | * The majority of individuals affected by sacroiliac joint pain are adults. The disorder is most common in individuals who lead a sedentary lifestyle. | ||
* Overall, obese patients are more commonly affected by sacroiliac joint pain. | * Overall, obese patients are more commonly affected by sacroiliac joint pain. | ||
| Line 47: | Line 36: | ||
The most common symptoms include:<ref name="bron6" /> | The most common symptoms include:<ref name="bron6" /> | ||
* | *Pain is usually localized over the buttock | ||
* | *Patients can often complain of sharp, stabbing, and/or shooting pain which extends down the posterior thigh usually not past the knee. | ||
* Pain can frequently mimic and be misdiagnosed as radicular pain | |||
*Difficulty sitting in one place for too long due to pain | *Difficulty sitting in one place for too long due to pain | ||
*Local tenderness of the posterior aspect of the sacroiliac joint (near the PSIS)<ref name="bron7">MONTICONE M., BARBARINO A., TESTI C. Symptomatic efficacy of stabilizing treatment versus laser therapy for sub-acute low back pain with positive tests for sacroiliac dysfunction: a randomized clinical trial with one year follow-up. Europa Medicophysica. Vol. 40, N° 4, p 263-268, 2004</ref><ref name=":0" /> | *Local tenderness of the posterior aspect of the sacroiliac joint (near the PSIS)<ref name="bron7">MONTICONE M., BARBARINO A., TESTI C. Symptomatic efficacy of stabilizing treatment versus laser therapy for sub-acute low back pain with positive tests for sacroiliac dysfunction: a randomized clinical trial with one year follow-up. Europa Medicophysica. Vol. 40, N° 4, p 263-268, 2004</ref><ref name=":0" /> | ||
| Line 54: | Line 44: | ||
*Absence of neurological deficit/nerve root tension signs | *Absence of neurological deficit/nerve root tension signs | ||
*Aberrant sacroiliac movement pattern<ref name="bron8">MORRIS E. C. Low Back Syndromes: integrated clinical management. The McGraw-Hills Companies, 2006.</ref> | *Aberrant sacroiliac movement pattern<ref name="bron8">MORRIS E. C. Low Back Syndromes: integrated clinical management. The McGraw-Hills Companies, 2006.</ref> | ||
* Patients will frequently complain of pain while sitting down, lying on the ipsilateral side of pain, or climbing stairs<ref name=":0" /> | * Patients will frequently complain of pain while sitting down, lying on the ipsilateral side of pain, or climbing stairs<ref name=":0" /> | ||
== | == Treatment == | ||
Initial therapy provided by the primary care provider includes [[Adherence to Home Exercise Programs|home exercise programs,]] over-the-counter [[Pain Medications|pain medications]], bracing, belts, manipulative therapy, and physical therapy. | |||
# Physiotherapy is crucial in the strengthening of the [[Core Strengthening|core muscles]] as well as the [[Gluteal Muscles|gluteus muscles,]] which are needed to help support the SI joint. | |||
#[[Therapeutic Corticosteroid Injection|Corticosteroid injection]] or anesthetic injections can be useful. Radiofrequency ablation (disables nerve fibers that are carrying the pain signal through the spinal cord to the brain) or rhizotomy (surgical procedure in which anterior spinal nerve roots are cut to relieve severe pain) are other options available if warranted. | |||
# Suspected inflammatory SI Joint injury usually requires further assessment, including labs and management by a rheumatologist.<ref name=":1" /> | |||
== Physiotherapy Assessment == | |||
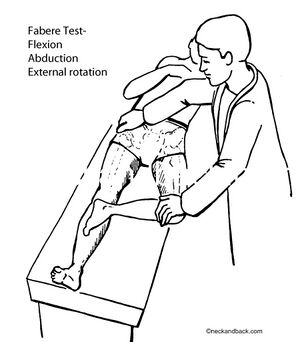
[[File:FABERs test.jpg|right|frameless]] | |||
A comprehensive physical examination for evaluating SI joint dysfunction. | A comprehensive physical examination for evaluating SI joint dysfunction. | ||
* The patients' hips should be evaluated for symptom elicitation, and ROM should be performed and documented. Trendelenburg testing is also helpful. Direct palpation over the SI joints will often elicit discomfort<ref name=":0" />. Leg length discrepancy is also a cause of sacroiliac joint pain. Leg lengths should be measured in all patients with suspected sacroiliac joint dysfunction. | * The patients' hips should be evaluated for symptom elicitation, and ROM should be performed and documented. [[Trendelenburg Sign|Trendelenburg]] testing is also helpful. Direct palpation over the SI joints will often elicit discomfort<ref name=":0" />. [[Leg Length Discrepancy|Leg length discrepancy]] is also a cause of sacroiliac joint pain. Leg lengths should be measured in all patients with suspected sacroiliac joint dysfunction. | ||
Physiotherapists use a variety of orthopaedic [[Posterior pelvic pain provocation test|provocation tests]]. | Physiotherapists use a variety of orthopaedic [[Posterior pelvic pain provocation test|provocation tests]]. | ||
{| class="wikitable" | |||
|Tests | |||
|Description (Positive Findings) | |||
|- | |||
|[[Distraction Test|Distraction]] | |||
|Pt supine. Examiner applies posterolateral directed pressure to bilateral ASIS. (Reproduction of pain) | |||
|- | |||
|[[SI compression test|Compression]] | |||
|Pt sidelying. Examiner compresses pelvis with pressure applied over the iliac crest directed at the opposite iliac crest. (Reproduction of symptoms) | |||
|- | |||
|[[Posterior pelvic pain provocation test|Thigh Thrust]] | |||
|Pt supine. Examiner places hip in 90 deg flexion and adduction. Examiner then applies posteriorly directed force through the femur at varying angles of abduction/adduction. (Reproduction of buttock pain) | |||
|- | |||
|[[Sacral Thrust Test|Sacral Thrust]] | |||
|Pt prone. Examiner delivers an anteriorly directed thrust over the sacrum. (Reproduction of pain) | |||
|- | |||
|[[Gaenslen Test|Gaenslen's]] | |||
|Pt supine with both legs extended. The test leg is passively brought into full knee flexion, while the opposite hip remains in extension. Overpressure is then applied to the flexed extremity. (Reproduction of pain) | |||
|- | |||
|Drop Test | |||
|Pt stands erect with heels raised on both legs while keeping the affected side knee extended. Pt is advised to drop the affected side heel with a bump while bearing the whole body weight alongside keeping the knee exteded, to direct force cranially through the ipsilateral SIJ. | |||
|} | |||
<ref>Physiopedia [[Sacroiliac Joint Special Test Cluster]]</ref>For more testing see [[Sacroiliac Joint Special Test Cluster]] | |||
However, SIJ pain has always been an controversial issue with the low back pain. Is is very important to rule out low back and hip pathologies before concluding to the SIJ involvement otherwise false positive SIJ results can be generated due to low specificity of the above mentioned tests. | |||
SIJ cluster tests has always held questionable due to its compromising Sensitivity and specificity of 91% and 78% respectively when used in cluster of 3 or more positive. Hence, it is not recommended to be rely on single test positive.<ref>Laslett M. Evidence-based diagnosis and treatment of the painful sacroiliac joint. J Man Manip Ther. 2008;16(3):142-52. doi: 10.1179/jmt.2008.16.3.142. PMID: 19119403; PMCID: PMC2582421.</ref> | |||
In a trial of 202 chronic back pain patients, 60% patient were ruled in with SIJ pathology with the presence of 1 positive test. However, after ruling out low back and hip pathology only 17% subjects had 1 positive SIJ test. Moreover, on performing retest on while only looking for the subjects with 3 or more positive tests, 6.5% and 3.5 % were true positive(Laslett,1997).<ref>Laslett M (1997): Pain provocation sacroiliac joint tests: Reliability and prevalence. In Vleeming A and Mooney V (Eds): Movement, Stability and Low Back Pain: The Essential Role of the Pelvis. New York: Churchill Livingstone, pp. 287-295.</ref> | |||
<clinicallyrelevant id="83474654" title="Sacroiliac distraction test" /> | Below are 30 second videos on the distraction and compression tests.<clinicallyrelevant id="83474654" title="Sacroiliac distraction test" /> | ||
<clinicallyrelevant id="83479944" title="Sacroiliac compression test" /> | <clinicallyrelevant id="83479944" title="Sacroiliac compression test" /> | ||
== Physical Therapy Management == | |||
Aims | |||
Stabilization Exercises | # Reduce the inflammation with icepacks and anti-inflammatory medication. If the sacroiliac joint is severely inflamed, a sacroiliac belt can also be used. | ||
# Improve SI joint function and core strength to stabilise the SI joint (using mobilizations, manipulation and exercise therapy).<ref name="bron14">Al-Subahi M. et al, The effectiveness of physiotherapy interventions for sacroiliac joint dysfunction: a systematic review, Journal of physical therapy science, 2017 (LoE 1A)</ref><ref>Zelle, B. A., Gruen, G. S., Brown, S., & George, S. (2005). Sacroiliac joint dysfunction: evaluation and management. The Clinical journal of pain, 21(5), 446-455. (LoA 1A)</ref><br> | |||
[[File:Plank leg lift.jpg|alt=|thumb|Core activation example]]'''1.Core Stability (see also [[Core Stability]])''' | |||
Exercises is a major component of a programme when treating Sacroiliac pain and [[Core Stability]] has been shown to be effective. | |||
Stabilization Exercises (see also [[Exercises for Lumbar Instability]]) | |||
* For the lumbar exercises, awareness is necessary in order to isolate the co-contraction of the local muscle system, which happens without global muscle substitution. It’s necessary to train the specific isometric co-contraction of two important core stabilizers: musculus transversus abdominis and the lumbar multifidi. These muscles have to be trained at low levels of maximal voluntary contraction; it’s important to maintain controlled respiration and neutral lordosis in weight bearing exercises.<ref>P.B. O'Sullivan et al., Masterclass. Lumbar segmental ‘instability’: clinical presentation and specific stabilizing exercise management, Manual therapy, 2000. (Level of evidence 2A)</ref> '' '' It’s really important to take into account the following principles: breathe in and out, tighten the lower abdomen below the umbilicus carefully and slowly without moving the upper stomach, back or pelvis such as a hollowing. Furthermore, a bulging of the multifidus muscle may be felt by the physiotherapist. There is a need of precise palpation of the muscles to ensure effective muscle activation.<ref name="Kumar SP et al.">Kumar SP et al., Efficacy of segmental stabilization exercise for lumbar segmental instability in patients with mechanical low back pain: A randomized placebo controlled crossover study, North American Journal of medical sciences, 2011. . (Level of evidence 1B)</ref> | * For the lumbar exercises, awareness is necessary in order to isolate the co-contraction of the local muscle system, which happens without global muscle substitution. It’s necessary to train the specific isometric co-contraction of two important core stabilizers: musculus transversus abdominis and the lumbar multifidi. These muscles have to be trained at low levels of maximal voluntary contraction; it’s important to maintain controlled respiration and neutral lordosis in weight bearing exercises.<ref>P.B. O'Sullivan et al., Masterclass. Lumbar segmental ‘instability’: clinical presentation and specific stabilizing exercise management, Manual therapy, 2000. (Level of evidence 2A)</ref> '' '' It’s really important to take into account the following principles: breathe in and out, tighten the lower abdomen below the umbilicus carefully and slowly without moving the upper stomach, back or pelvis such as a hollowing. Furthermore, a bulging of the multifidus muscle may be felt by the physiotherapist. There is a need of precise palpation of the muscles to ensure effective muscle activation.<ref name="Kumar SP et al.">Kumar SP et al., Efficacy of segmental stabilization exercise for lumbar segmental instability in patients with mechanical low back pain: A randomized placebo controlled crossover study, North American Journal of medical sciences, 2011. . (Level of evidence 1B)</ref> | ||
Isolated Lumbar Stabilizing Muscle Training | Isolated Lumbar Stabilizing Muscle Training | ||
| Line 124: | Line 118: | ||
'''2. Manipulation''' | '''2. Manipulation''' | ||
* Treatment of Sacroiliac Joint (SIJ) Syndrome is best approached from a multidisciplinary standpoint and it is not uncommon to see modalities such as [[Spinal Manipulation|manipulation]] included in the programme. Conservative treatment consists of exercise therapy and manual therapy. It’s important to determine and address the underlying causes of dysfunction during the treatment.<ref>Pascal Vanelderen et al, Evidence-based Interventional Pain Medicine according to Clinical Diagnoses, ‘13. Sacroiliac Joint Pain’, World Institute of Pain, 2010. (level of evidence 2B)</ref> | * Treatment of Sacroiliac Joint (SIJ) Syndrome is best approached from a multidisciplinary standpoint and it is not uncommon to see modalities such as [[Spinal Manipulation|manipulation]] included in the programme. Conservative treatment consists of exercise therapy and manual therapy. It’s important to determine and address the underlying causes of dysfunction during the treatment.<ref>Pascal Vanelderen et al, Evidence-based Interventional Pain Medicine according to Clinical Diagnoses, ‘13. Sacroiliac Joint Pain’, World Institute of Pain, 2010. (level of evidence 2B)</ref> | ||
* There is evidence for both SIJ manipulation and lumbar manipulation. Following the performance of each of these manual therapy techniques pain and functional disability are significantly improved in patients diagnosed with SIJ syndrome. Manual spinal thrust manipulation may be considered as a component of effective treatment for patients with SIJ syndrome.<ref name="Kamali et al.">Kamali et al., The effect of two manipulative therapy techniques and their outcome in patients with sacroiliac joint syndrome, Journal of bodywork and Movement Therapies, 2013 (Level of evidence 1B)</ref> | * There is evidence for both SIJ manipulation and lumbar manipulation. Following the performance of each of these manual therapy techniques pain and functional disability are significantly improved in patients diagnosed with SIJ syndrome. Manual spinal thrust manipulation may be considered as a component of effective treatment for patients with SIJ syndrome.<ref name="Kamali et al.">Kamali et al., The effect of two manipulative therapy techniques and their outcome in patients with sacroiliac joint syndrome, Journal of bodywork and Movement Therapies, 2013 (Level of evidence 1B)</ref> | ||
* Dr. Abdulsamad Qassem has studided this Manipulation in Yemen and noticed that alot of patients need a specific manipulation after pure Assessment.<br> | |||
[[File:Cleland manip pic.jpg|right|frameless]] | [[File:Cleland manip pic.jpg|right|frameless]] | ||
SIJ Manipulation | SIJ Manipulation | ||
| Line 130: | Line 125: | ||
Lumbar Rotational Manipulation | Lumbar Rotational Manipulation | ||
The patient lies on the unaffected side and the therapist stands opposite the patient, flexing the patient’s hip until the lumbar spine is in flexion. The therapist grasps the patient’s lower shoulder and arm to stabilize him, and moves him into left trunk side bending and right rotation, until motion is felt at the desired segment of the lumbar spine. The arms of the patient are placed above the therapist’s arm. This position is maintained while the patient is rolled toward the therapist. The therapist’s other arm is used to apply a high-velocity low-amplitude thrust to the pelvis in an anterior direction (Cleland et al., 2006).<ref name="Kamali et al." /> | * The patient lies on the unaffected side and the therapist stands opposite the patient, flexing the patient’s hip until the lumbar spine is in flexion. The therapist grasps the patient’s lower shoulder and arm to stabilize him, and moves him into left trunk side bending and right rotation, until motion is felt at the desired segment of the lumbar spine. The arms of the patient are placed above the therapist’s arm. This position is maintained while the patient is rolled toward the therapist. The therapist’s other arm is used to apply a high-velocity low-amplitude thrust to the pelvis in an anterior direction (Cleland et al., 2006).<ref name="Kamali et al." /> | ||
The purpose of this technique is to manipulate an iliac anterior rotation displacement sacroiliac joint dysfunction and to restore posterior rotation of the ilium. The patient lies on his side and toward the therapist. The therapist places his hand on the ASIS and the other is on the ischial tuberosity. The top hip is flexed to 90° and the other leg is relatively extended. Rotate the spine to the level of the L5-S1 segment pull the patient’s bottom arm in an anterior and superior rotation. The hand on the ASIS pushes posteriorly and the other pushes anteriorly. This must be maintained for 10 to 30 seconds.<ref name="K. A. Olson">K. A. Olson, Manuel Physical Therapy of the Spine, Saunders Elsevier, 2009, p 182- 184</ref> | Posterior Iliac Rotation Sacroiliac Joint Manipulation | ||
The aim is to manipulate a posterior iliac rotation displacement to restore anterior rotation of the ilium. The patient lies prone with a pillow under his pelvis. The therapist supports the thigh just above the knee. To stabilize the ilium, the other hand is on the ipsilateral PSIS (Posterior Superior Iliac Spine) pushing in an anterolateral direction. The therapist’s fingers should point toward the patient’s feet. After positioning, the therapist brings the leg above the table into hip extension just enough to take up the slack in the hip flexors. It is recommended to hold this position for 10 seconds with the knee either extended or flexed.<ref name="K. A. Olson" /> <br> | * The purpose of this technique is to manipulate an iliac anterior rotation displacement sacroiliac joint dysfunction and to restore posterior rotation of the ilium. The patient lies on his side and toward the therapist. The therapist places his hand on the ASIS and the other is on the ischial tuberosity. The top hip is flexed to 90° and the other leg is relatively extended. Rotate the spine to the level of the L5-S1 segment pull the patient’s bottom arm in an anterior and superior rotation. The hand on the ASIS pushes posteriorly and the other pushes anteriorly. This must be maintained for 10 to 30 seconds.<ref name="K. A. Olson">K. A. Olson, Manuel Physical Therapy of the Spine, Saunders Elsevier, 2009, p 182- 184</ref> | ||
Anterior Iliac Rotation Sacroiliac Joint Manipulation | |||
* The aim is to manipulate a posterior iliac rotation displacement to restore anterior rotation of the ilium. The patient lies prone with a pillow under his pelvis. The therapist supports the thigh just above the knee. To stabilize the ilium, the other hand is on the ipsilateral PSIS (Posterior Superior Iliac Spine) pushing in an anterolateral direction. The therapist’s fingers should point toward the patient’s feet. After positioning, the therapist brings the leg above the table into hip extension just enough to take up the slack in the hip flexors. It is recommended to hold this position for 10 seconds with the knee either extended or flexed.<ref name="K. A. Olson" /> <br> | |||
'''3. Stabilisation''' | '''3. Stabilisation''' | ||
| Line 146: | Line 145: | ||
== Team Work == | == Team Work == | ||
[[File:Hip exercise 4.png|right|frameless]]Sacroiliac joint pain is a difficult diagnosis to make and best managed by an interprofessional team that includes a physical therapist, pain specialist, nurse practitioner, primary care provider and an orthopedic surgeon. | |||
* The key is to educate the patient on changing lifestyle ie a healthy body weight and regular exercise. | * The key is to educate the patient on changing lifestyle ie a healthy body weight and regular exercise. | ||
* Many other remedies are available for SI joint pain, but their efficacy is dubious. | * Many other remedies are available for SI joint pain, but their efficacy is dubious. | ||
* Surgery is the last resort and is not always associated with good outcomes. Patients who lead a sedentary lifestyle usually have the worst outcomes | * Surgery is the last resort and is not always associated with good outcomes. Patients who lead a sedentary lifestyle usually have the worst outcomes | ||
== Differential Diagnosis == | |||
Sacroiliac joint syndrome is a controversial diagnosis, therefore pain and injury to the sacroiliac joint are commonly overlooked.<ref name="bron9">SEIDENBERG P.H. The Hip and Pelvis in Sports Medicine and Primary Care. Springer, p. 140, 2010.</ref> This condition is often listed under the general term dysfunction, a term that serves as a collective term for different conditions. The differential diagnosis should include: | |||
*[[Radiculopathy|Radicular pain]] | |||
*[[Piriformis Syndrome|Piriformis syndrome]] | |||
*[[Ankylosing Spondylitis (Axial Spondyloarthritis)|Ankylosing spondylitis]]<ref name="bron9" /><ref name="bron10">http://emedicine.medscape.com/article/96054-differential (accessed on 30/10/2011)</ref> | |||
*[[Lumbar Facet Syndrome|Lumbosacral facet syndrome]]<ref name="bron10" /> | |||
*[[Spondyloarthropathy--AS|Spondyloarthropathy]] | |||
*[[Trochanteric Bursitis|Trochanteric bursitis]] | |||
*[[Femoral Neck Hip Fracture|Hip fracture]] | |||
* Hip overuse syndrome | |||
== <u></u>Key Research == | == <u></u>Key Research == | ||
*[https://www.researchgate.net/publication/51922257_The_effect_of_two_manipulative_therapy_techniques_and_their_outcome_in_patients_with_sacroiliac_joint_syndrome Kamali, F., Shokri, E., The effect of two manipulative therapy techniques and their outcome in patients with sacroiliac joint syndrome. Journal of Bodywork & Movement Therapies, 2011.] | *[https://www.researchgate.net/publication/51922257_The_effect_of_two_manipulative_therapy_techniques_and_their_outcome_in_patients_with_sacroiliac_joint_syndrome Kamali, F., Shokri, E., The effect of two manipulative therapy techniques and their outcome in patients with sacroiliac joint syndrome. Journal of Bodywork & Movement Therapies, 2011.] | ||
Sacroiliac joint and lumbar manipulation was more effective for improving functional disability than sacroiliac joint manipulation alone in patients with Sacroiliac Joint Syndrome. Spinal high-velocity low-amplitude manipulation may be a beneficial addition to treatment for patients with SIJ syndrome. | Sacroiliac joint and lumbar manipulation was more effective for improving functional disability than sacroiliac joint manipulation alone in patients with Sacroiliac Joint Syndrome. Spinal high-velocity low-amplitude manipulation may be a beneficial addition to treatment for patients with SIJ syndrome. | ||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
| Line 195: | Line 197: | ||
== References == | == References == | ||
<references /> | <references group="Laslett M(1997). pain provocation sacroiliac joint tests:reliability and prevalence. In Movement, Stability &low Back Pain. The essential role of pelvis, Eds Vleeming A, Mooney V, Dorman T, Sniggers C, Stoeckart R, Churchill Livingstone, New York." /> | ||
[[Category:Sacroiliac_Conditions]] | [[Category:Sacroiliac_Conditions]] | ||
Latest revision as of 00:12, 16 February 2024
Original Editors - Jessie Tourwe
Top Contributors - Jessie Tourwe, Sefora Bakkioui, Lucinda hampton, Kim Jackson, Laura Ritchie, Admin, Dilawar Singh Maan, Elien Lebuf, Wanda van Niekerk, Lauren Lopez, Claire Knott, Kai A. Sigel, Yahya Al-Razi, Rachael Lowe, Tony Lowe, Scott Buxton, Sweta Christian and WikiSysop
Introduction[edit | edit source]
Sacroiliac joint dysfunction is a term used to describe the pain of the sacroiliac joint (SI joint). It is usually caused by abnormal motion (i.e. hyper- or hypo-mobile) or malalignment of the sacroiliac joint. Sacroiliac joint syndrome is a significant source of pain in 15% to 30% of people with mechanical low back pain.
Sacroiliitis is not the same as SI joint dysfunction. Sacroiliitis is specific to an inflammatory processes present in the SI joint and the pain sensed is a direct result of those inflammatory processes, whereas sacroiliac joint dysfunction is a condition caused by abnormal motion or slight mispositioning of the SI joint.
Sacroiliac joint syndrome is a condition that is difficult to diagnose and is often overlooked by physicians and physiotherapists.[1]
Clinically Relevant Anatomy[edit | edit source]
The sacroiliac joints are located on each side of the spine between the two pelvic bones, which attach to the sacrum.[2] The main function within the pelvic girdle is to provide shock absorption for the spine and to transmit forces between the upper body and the lower limbs.[3] The SI joint experiences forces of shearing, torsion, rotation, and tension. Ambulation is heavily impacted by the SI joint, as this is the only orthopedic joint connecting the upper body to our lower body. The joint is a relatively stiff synovial joint filled with synovial fluid. The bones of the sacrum and ilium are coated in hyaline cartilage at their articular surfaces with dense fibrous tissue connecting the ilium and the sacrum. SI joints typically only have a few degrees of motion[4].
Etiology [edit | edit source]
Injuries to the sacroiliac joint can occur from various etiologies.
- 88% of cases of SI joint injury are due to either repetitive microtrauma or acute trauma. There is a high prevalence of SI joint injury in athletes. Trauma in the context of pelvic ring injuries is one example of SI joint injury. Pelvic ring traumatic injuries and low impact Pelvic fractures can be read about here.
- 20% of cases are pregnancy-related. Female hormones are released during pregnancy, relaxing the sacroiliac ligaments. This stretching in ligaments results in changes to the sacroiliac joints, making them hypermobile.[3] After the fifth decade of life, the sacroiliac joint fuses.[5]
- 4% are idiopathic.[4]
- Pain can also be caused by an abnormality of the sacrum bone, which can be seen on X-rays.
Epidemiology[edit | edit source]
Approximately 90% of the population will at some experience or present to the clinic with some form of low back pain/pathology. About 10% to 25% of these patients are thought to be experiencing pain from the SI joint. The majority of SI joint pathologies affect the adult patient population.
- The majority of individuals affected by sacroiliac joint pain are adults. The disorder is most common in individuals who lead a sedentary lifestyle.
- Overall, obese patients are more commonly affected by sacroiliac joint pain.
- The disorder is seen in both genders and people of all races.[5]
Clinical Presentation [edit | edit source]
Symptoms of sacroiliac joint syndrome are often difficult to distinguish from other types of low back pain. This is why making a diagnosis of sacroiliac joint syndrome is very difficult.
The most common symptoms include:[3]
- Pain is usually localized over the buttock
- Patients can often complain of sharp, stabbing, and/or shooting pain which extends down the posterior thigh usually not past the knee.
- Pain can frequently mimic and be misdiagnosed as radicular pain
- Difficulty sitting in one place for too long due to pain
- Local tenderness of the posterior aspect of the sacroiliac joint (near the PSIS)[6][5]
- Pain occurs when the joint is mechanically stressed eg forward bending
- Absence of neurological deficit/nerve root tension signs
- Aberrant sacroiliac movement pattern[7]
- Patients will frequently complain of pain while sitting down, lying on the ipsilateral side of pain, or climbing stairs[5]
Treatment[edit | edit source]
Initial therapy provided by the primary care provider includes home exercise programs, over-the-counter pain medications, bracing, belts, manipulative therapy, and physical therapy.
- Physiotherapy is crucial in the strengthening of the core muscles as well as the gluteus muscles, which are needed to help support the SI joint.
- Corticosteroid injection or anesthetic injections can be useful. Radiofrequency ablation (disables nerve fibers that are carrying the pain signal through the spinal cord to the brain) or rhizotomy (surgical procedure in which anterior spinal nerve roots are cut to relieve severe pain) are other options available if warranted.
- Suspected inflammatory SI Joint injury usually requires further assessment, including labs and management by a rheumatologist.[4]
Physiotherapy Assessment [edit | edit source]
A comprehensive physical examination for evaluating SI joint dysfunction.
- The patients' hips should be evaluated for symptom elicitation, and ROM should be performed and documented. Trendelenburg testing is also helpful. Direct palpation over the SI joints will often elicit discomfort[5]. Leg length discrepancy is also a cause of sacroiliac joint pain. Leg lengths should be measured in all patients with suspected sacroiliac joint dysfunction.
Physiotherapists use a variety of orthopaedic provocation tests.
| Tests | Description (Positive Findings) |
| Distraction | Pt supine. Examiner applies posterolateral directed pressure to bilateral ASIS. (Reproduction of pain) |
| Compression | Pt sidelying. Examiner compresses pelvis with pressure applied over the iliac crest directed at the opposite iliac crest. (Reproduction of symptoms) |
| Thigh Thrust | Pt supine. Examiner places hip in 90 deg flexion and adduction. Examiner then applies posteriorly directed force through the femur at varying angles of abduction/adduction. (Reproduction of buttock pain) |
| Sacral Thrust | Pt prone. Examiner delivers an anteriorly directed thrust over the sacrum. (Reproduction of pain) |
| Gaenslen's | Pt supine with both legs extended. The test leg is passively brought into full knee flexion, while the opposite hip remains in extension. Overpressure is then applied to the flexed extremity. (Reproduction of pain) |
| Drop Test | Pt stands erect with heels raised on both legs while keeping the affected side knee extended. Pt is advised to drop the affected side heel with a bump while bearing the whole body weight alongside keeping the knee exteded, to direct force cranially through the ipsilateral SIJ. |
[8]For more testing see Sacroiliac Joint Special Test Cluster
However, SIJ pain has always been an controversial issue with the low back pain. Is is very important to rule out low back and hip pathologies before concluding to the SIJ involvement otherwise false positive SIJ results can be generated due to low specificity of the above mentioned tests.
SIJ cluster tests has always held questionable due to its compromising Sensitivity and specificity of 91% and 78% respectively when used in cluster of 3 or more positive. Hence, it is not recommended to be rely on single test positive.[9]
In a trial of 202 chronic back pain patients, 60% patient were ruled in with SIJ pathology with the presence of 1 positive test. However, after ruling out low back and hip pathology only 17% subjects had 1 positive SIJ test. Moreover, on performing retest on while only looking for the subjects with 3 or more positive tests, 6.5% and 3.5 % were true positive(Laslett,1997).[10]
Below are 30 second videos on the distraction and compression tests.
Sacroiliac distraction test video provided by Clinically Relevant
Sacroiliac compression test video provided by Clinically Relevant
Physical Therapy Management [edit | edit source]
Aims
- Reduce the inflammation with icepacks and anti-inflammatory medication. If the sacroiliac joint is severely inflamed, a sacroiliac belt can also be used.
- Improve SI joint function and core strength to stabilise the SI joint (using mobilizations, manipulation and exercise therapy).[11][12]
1.Core Stability (see also Core Stability)
Exercises is a major component of a programme when treating Sacroiliac pain and Core Stability has been shown to be effective.
Stabilization Exercises (see also Exercises for Lumbar Instability)
- For the lumbar exercises, awareness is necessary in order to isolate the co-contraction of the local muscle system, which happens without global muscle substitution. It’s necessary to train the specific isometric co-contraction of two important core stabilizers: musculus transversus abdominis and the lumbar multifidi. These muscles have to be trained at low levels of maximal voluntary contraction; it’s important to maintain controlled respiration and neutral lordosis in weight bearing exercises.[13] It’s really important to take into account the following principles: breathe in and out, tighten the lower abdomen below the umbilicus carefully and slowly without moving the upper stomach, back or pelvis such as a hollowing. Furthermore, a bulging of the multifidus muscle may be felt by the physiotherapist. There is a need of precise palpation of the muscles to ensure effective muscle activation.[14]
Isolated Lumbar Stabilizing Muscle Training
- Specifically for stabilization exercises, it’s recommended to begin in a quadruped position. The physiotherapist can manually guide the spine through the full arc of flexion and extension. It’s essential to tuck in the chin and hollow the abdomen by tilting the pelvis posteriorly. Lift one arm slowly while continuing to maintain the neutral position of the spine, without changing the natural curves; return the arm and then continue with the other.
- The lumbar multifidi can be palpated medial to the lumbar facet joints bilaterally; this allows the physiotherapist to avoid changes in muscle activity of the long spinal extensor muscles, ensuring that the patient is performing the exercise correctly.
- Activation of the musculus transversus abdominis and multifidus together in sitting and standing positions, or while performing stepping and balance activities are essential[14] [15]
Integration of Lumbar Stabilization into Light Dynamic Functional Tasks
- Sit on an unstable base of support and co-contract the transverse abdominis and multifidus muscles while performing the following stabilizing exercises individually to improve lumbopelvic control: hip extension, lumbar spine extension, and thoracic spine extension with co-contractions. These co-contractions can also be performed while walking and performing other activities of daily living. [15]
Integration of Lumbar Stabilization into Heavy-Load Dynamic Functional Tasks
- The next exercises are isometric co-contractions to be performed with the addition of heavier external loads to the lumbar spine: bridging and single-leg extension in quadruped.
- Single-leg extension from quadruped can provide further challenge with alternating arm/leg extensions.
- To increase the complexity and the load of these exercises, single-leg bridging and the bilateral bridging exercises can be performed with the lower extremities on an unstable base of support such as a Swiss ball.
- Finally an example of an exercise to improve coordination is single-leg bridging with alternating lower extremities on an unstable base of support. Alternating the stabilizing lower extremity on the Swiss ball further challenges coordination and balance while improving the stabilization capabilities of the core musculature.
- During all these exercises the co-contraction of the musculus transversus abdominus and multifidi are imperative.[15]
2. Manipulation
- Treatment of Sacroiliac Joint (SIJ) Syndrome is best approached from a multidisciplinary standpoint and it is not uncommon to see modalities such as manipulation included in the programme. Conservative treatment consists of exercise therapy and manual therapy. It’s important to determine and address the underlying causes of dysfunction during the treatment.[16]
- There is evidence for both SIJ manipulation and lumbar manipulation. Following the performance of each of these manual therapy techniques pain and functional disability are significantly improved in patients diagnosed with SIJ syndrome. Manual spinal thrust manipulation may be considered as a component of effective treatment for patients with SIJ syndrome.[17]
- Dr. Abdulsamad Qassem has studided this Manipulation in Yemen and noticed that alot of patients need a specific manipulation after pure Assessment.
SIJ Manipulation
- The patient lies on his back with the therapist standing opposite the side to be manipulated. The patient places his hands behind his head and the therapist then moves the patient passively into side bending to end range toward the target side. The therapist then delivers a quick thrust to the Anterior Superior Iliac Spine (ASIS) in a posterior and inferior direction (Cleland et al., 2006; Edmond, 2006).[17]
Lumbar Rotational Manipulation
- The patient lies on the unaffected side and the therapist stands opposite the patient, flexing the patient’s hip until the lumbar spine is in flexion. The therapist grasps the patient’s lower shoulder and arm to stabilize him, and moves him into left trunk side bending and right rotation, until motion is felt at the desired segment of the lumbar spine. The arms of the patient are placed above the therapist’s arm. This position is maintained while the patient is rolled toward the therapist. The therapist’s other arm is used to apply a high-velocity low-amplitude thrust to the pelvis in an anterior direction (Cleland et al., 2006).[17]
Posterior Iliac Rotation Sacroiliac Joint Manipulation
- The purpose of this technique is to manipulate an iliac anterior rotation displacement sacroiliac joint dysfunction and to restore posterior rotation of the ilium. The patient lies on his side and toward the therapist. The therapist places his hand on the ASIS and the other is on the ischial tuberosity. The top hip is flexed to 90° and the other leg is relatively extended. Rotate the spine to the level of the L5-S1 segment pull the patient’s bottom arm in an anterior and superior rotation. The hand on the ASIS pushes posteriorly and the other pushes anteriorly. This must be maintained for 10 to 30 seconds.[18]
Anterior Iliac Rotation Sacroiliac Joint Manipulation
- The aim is to manipulate a posterior iliac rotation displacement to restore anterior rotation of the ilium. The patient lies prone with a pillow under his pelvis. The therapist supports the thigh just above the knee. To stabilize the ilium, the other hand is on the ipsilateral PSIS (Posterior Superior Iliac Spine) pushing in an anterolateral direction. The therapist’s fingers should point toward the patient’s feet. After positioning, the therapist brings the leg above the table into hip extension just enough to take up the slack in the hip flexors. It is recommended to hold this position for 10 seconds with the knee either extended or flexed.[18]
3. Stabilisation
Pelvic Belt
- The tension of a pelvic belt is comparable to the muscle activity of the transversus abdominis (and the obliquus internus abdominis) muscle. Transversus abominis has an anterior attachment on the iliac crest, an ideal place to act on the ilium producing compression of the SIJ in combination with stiff dorsal sacroiliac ligaments.
- A minimum contraction of 30-40% of the maximum voluntary force of the transversus abdominis is sufficient to achieve stability of the pelvis according to Richardson et al. No greater contraction is needed to achieve joint stabilization because the lever arm of the transversus abdominis is almost equal to the lever arm of the pelvic belt. There is also no significant change of stability by increasing belt tension from 50 to 100 N, but if the belt is placed in too low of a position, it may lead to a small decrease of laxity. Greater belt tension isn’t recommended secondary to the potential of skin pressure and discomfort.
- When the pelvic belt is worn there is a decrease of the sacroiliac joint laxity. This difference in laxity is due to the position of the belt. Positioning the pelvic belt just below the anterior superior iliac spines (the high position) is more effective than the low position (at the top of the pubic symphysis). However, the tension of the belt has no significant influence on the stability of the SI-joint. [19]
Sacroiliac Binder
- When the use of the sacroiliac belt for a hypermobile SI-joint is appropriate, it should be worn for 24 hours per day up to 6 to 12 weeks. This belt should be used in combination with physical exercises and manual therapy in the case of joint dysfunction and muscle imbalance. The belt may be removed once the patient has improved control of the lumbopelvic musculature. The location of the sacroiliac belt should be at the superior aspect of the PSIS to assist in stabilizing and supporting the pelvis.[20]
Team Work[edit | edit source]
Sacroiliac joint pain is a difficult diagnosis to make and best managed by an interprofessional team that includes a physical therapist, pain specialist, nurse practitioner, primary care provider and an orthopedic surgeon.
- The key is to educate the patient on changing lifestyle ie a healthy body weight and regular exercise.
- Many other remedies are available for SI joint pain, but their efficacy is dubious.
- Surgery is the last resort and is not always associated with good outcomes. Patients who lead a sedentary lifestyle usually have the worst outcomes
Differential Diagnosis [edit | edit source]
Sacroiliac joint syndrome is a controversial diagnosis, therefore pain and injury to the sacroiliac joint are commonly overlooked.[21] This condition is often listed under the general term dysfunction, a term that serves as a collective term for different conditions. The differential diagnosis should include:
- Radicular pain
- Piriformis syndrome
- Ankylosing spondylitis[21][22]
- Lumbosacral facet syndrome[22]
- Spondyloarthropathy
- Trochanteric bursitis
- Hip fracture
- Hip overuse syndrome
Key Research [edit | edit source]
Sacroiliac joint and lumbar manipulation was more effective for improving functional disability than sacroiliac joint manipulation alone in patients with Sacroiliac Joint Syndrome. Spinal high-velocity low-amplitude manipulation may be a beneficial addition to treatment for patients with SIJ syndrome.
Clinical Bottom Line [edit | edit source]
A Sacroiliac Joint Syndrome is a condition that is often overlooked by physiotherapists. It is often listed under the general term “dysfunction”, but this syndrome has to be differentiated from other sacroiliac joint disorders. To get a clear view of the Sacroiliac Joint Syndrome, further research has to be done in the future.
Presentations[edit | edit source]
 |
Pelvic Physiotherapy - to Kegel or Not?
This presentation was created by Carolyn Vandyken, a physiotherapist who specializes in the treatment of male and female pelvic dysfunction. She also provides education and mentorship to physiotherapists who are similarly interested in treating these dysfunctions. In the Level of Evidence presentation, Carolyn reviews pelvic anatomy, the history of Kegel exercises and what the evidence tells us about when Kegels are and aren't appropriate for our patients. |
References[edit | edit source]
- ↑ SLIPMAN W.C. Sacroiliac Joint Syndrome. Pain Physician. Vol. 4, N° 2, p 143-152, 2001. ISSN 1533-3159
- ↑ OLIVER J., MIDDLEDITCH A. Functional anatomy of the spine. Elsevier Science, p 190-191; 195-198, 2004
- ↑ 3.0 3.1 3.2 http://www.orthonc.com/education-research/spine/patient-education-spine-sacroiliac-joint-syndrome (accessed on 22/10/2011)
- ↑ 4.0 4.1 4.2 Dydyk AM, Forro SD, Hanna A. Sacroiliac Joint Injury.Available:https://www.ncbi.nlm.nih.gov/books/NBK557881/ (accessed 6.6.2022)
- ↑ 5.0 5.1 5.2 5.3 5.4 Raj MA, Varacallo M. Sacroiliac (SI) Joint Pain. InStatPearls [Internet] 2019 May 12. StatPearls Publishing Availabe from:.https://www.ncbi.nlm.nih.gov/books/NBK470299/ (last accessed 14.6.2020)
- ↑ MONTICONE M., BARBARINO A., TESTI C. Symptomatic efficacy of stabilizing treatment versus laser therapy for sub-acute low back pain with positive tests for sacroiliac dysfunction: a randomized clinical trial with one year follow-up. Europa Medicophysica. Vol. 40, N° 4, p 263-268, 2004
- ↑ MORRIS E. C. Low Back Syndromes: integrated clinical management. The McGraw-Hills Companies, 2006.
- ↑ Physiopedia Sacroiliac Joint Special Test Cluster
- ↑ Laslett M. Evidence-based diagnosis and treatment of the painful sacroiliac joint. J Man Manip Ther. 2008;16(3):142-52. doi: 10.1179/jmt.2008.16.3.142. PMID: 19119403; PMCID: PMC2582421.
- ↑ Laslett M (1997): Pain provocation sacroiliac joint tests: Reliability and prevalence. In Vleeming A and Mooney V (Eds): Movement, Stability and Low Back Pain: The Essential Role of the Pelvis. New York: Churchill Livingstone, pp. 287-295.
- ↑ Al-Subahi M. et al, The effectiveness of physiotherapy interventions for sacroiliac joint dysfunction: a systematic review, Journal of physical therapy science, 2017 (LoE 1A)
- ↑ Zelle, B. A., Gruen, G. S., Brown, S., & George, S. (2005). Sacroiliac joint dysfunction: evaluation and management. The Clinical journal of pain, 21(5), 446-455. (LoA 1A)
- ↑ P.B. O'Sullivan et al., Masterclass. Lumbar segmental ‘instability’: clinical presentation and specific stabilizing exercise management, Manual therapy, 2000. (Level of evidence 2A)
- ↑ 14.0 14.1 Kumar SP et al., Efficacy of segmental stabilization exercise for lumbar segmental instability in patients with mechanical low back pain: A randomized placebo controlled crossover study, North American Journal of medical sciences, 2011. . (Level of evidence 1B)
- ↑ 15.0 15.1 15.2 George A Koumantakis et al., Trunk Muscle Stabilization Training Plus General Exercise Versus General Exercise Only: Randomized Controlled Trial of Patients With Recurrent Low Back Pain, Physical Therapy Journal of the American Physical Therapy Association and Royal Dutch Society for Physical Therapy, 2005. . (Level of evidence 1B)
- ↑ Pascal Vanelderen et al, Evidence-based Interventional Pain Medicine according to Clinical Diagnoses, ‘13. Sacroiliac Joint Pain’, World Institute of Pain, 2010. (level of evidence 2B)
- ↑ 17.0 17.1 17.2 Kamali et al., The effect of two manipulative therapy techniques and their outcome in patients with sacroiliac joint syndrome, Journal of bodywork and Movement Therapies, 2013 (Level of evidence 1B)
- ↑ 18.0 18.1 K. A. Olson, Manuel Physical Therapy of the Spine, Saunders Elsevier, 2009, p 182- 184
- ↑ Leonie Damen et al, Does a pelvic belt influence sacroiliac joint laxity?, 2002, Clinical Biomechanics (Level of evidence 2B)
- ↑ K. A. Olson, Manuel Physical Therapy of the Spine, Saunders Elsevier, 2009, p 117- 1118
- ↑ 21.0 21.1 SEIDENBERG P.H. The Hip and Pelvis in Sports Medicine and Primary Care. Springer, p. 140, 2010.
- ↑ 22.0 22.1 http://emedicine.medscape.com/article/96054-differential (accessed on 30/10/2011)