Achilles Tendinopathy: Difference between revisions
No edit summary |
mNo edit summary |
||
| Line 6: | Line 6: | ||
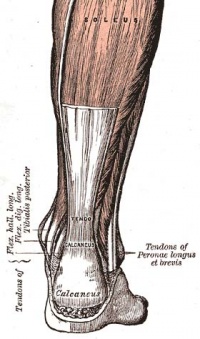
== Clinically Relevant Anatomy<br> == | == Clinically Relevant Anatomy<br> == | ||
[[Image:Achilles tendon.jpg|thumb|right|200px|Achilles Tendon]] | |||
[[ | The [[Achilles Tendon|Achilles tendon]] is the single tendon of the [[Soleus|soleus]] and [[Gastrocnemius|gastrocnemius]] muscles, inserting into the [[Calcaneus|calcaneus]].<ref name="Cook et al">Cook JL, Khan KM, Purdam C. Achilles tendinopathy. Manual Therapy 2002;7(3):121-130.</ref><br> | ||
== Mechanism of Injury / Pathological Process<br> == | == Mechanism of Injury / Pathological Process<br> == | ||
Revision as of 04:07, 23 March 2013
Original Editor - Karolyn Conolty
Lead Editors - Alex Scott
Clinically Relevant Anatomy
[edit | edit source]
The Achilles tendon is the single tendon of the soleus and gastrocnemius muscles, inserting into the calcaneus.[1]
Mechanism of Injury / Pathological Process
[edit | edit source]
Achilles tendonitis is commonly seen in athletes who sustain an increase in training load, and is most often due to overuse. Tendons respond poorly to overuse, therefore healing is slow. This can leave a tendon pathologically defective, which decreases tendon strength and leaves it less able to tolerate load, thus vulnerable to further injury. [1]Extrinsic factors contributing to this condition include training errors and inappropriate footwear. Intrinsic factors include inflexibility, weakness and malalignment. [2]
Clinical Presentation[edit | edit source]
Morning pain is a hallmark symptom because the Achilles tendon must tolerate full range of movement including stretch immediately on rising in the morning. Symptoms are typically localized to the tendon and immediate surrounding area. Swelling and pain at the attachment are less common. The tendon can appear to have subtle changes in outline, becoming thicker in the A-P and M-L planes.[1]
Diagnostic Procedures[edit | edit source]
Imaging studies are not necessary to diagnose Achilles tendonitis, but may be useful with differential diagnosis. US is the imaging modality of first choice as it provides a clear indication of tendon width, changes of water content within the tendon and collagen integrity, as well as bursal swelling. MRI may be indicated if diagnosis is unclear or symptoms are atypical. MRI may show increased signal within the Achilles.[1]
Outcome Measures[edit | edit source]
Robinson et al recommend the VISA-A scale. This is a subjective rating scale that quantifies the symptoms and dysfunction in the Achilles tendon. It is very useful to rate Achilles tendons and to assess progress of recovery during rehabilitation. [1][3]
Management / Interventions
[edit | edit source]
| [4] |
Treatment of Achilles tendinopathy is initially non-operative, including rest, equipment changes, strength and flexibility exercises, anti-inflammatory agents and corticosteroids. The effects of physical therapy on Achilles tendonitis is poorly understood, although musculotendinous strengthening appears essential. Eccentric exercises have been shown to have positive effects of Achilles tendonitis, and remains the gold standard for rehabiliation of this condition.[1][2] A study by Roos et al concluded that eccentric exercises improve function and reduce pain and effects were apparent after 6 weeks of treatment, lasting for 1 year.[3]
Supportive taping can also help manage symptoms:
| [5] | [6] |
Differential Diagnosis
[edit | edit source]
Posterior ankle impingement, medial tendinopathy, retrocalcaneal bursitis, sural nerve, lumbar radiculopathy, ankle OA, DVT, Haglund deformity, partial Achilles tendon rupture.[1]
Resources[edit | edit source]
 |
Achilles Tendinopathy Toolkit
The Achilles Tendinopathy Toolkit is a comprehensive evidence based resource to assist practitioners in clinical decision making for Achilles Tendinopathy. |
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1DeUIcPgNLDEQT17PEJLA26uuKLv4fz4eTsAi9nkGXzfWOXsZF|charset=UTF-8|short|max=10: Error parsing XML for RSS
Presentations[edit | edit source]
 |
Achilles Tendonopathy: Intervention
This presentation, created by Shannon Petersen, Clebert LeBlanc, Amy Lavrich, & Kelly Coleman as part of the Regis University OMPT Fellowship, discusses the current best evidence for interventions for Achilles Tendonopathy. |
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Cook JL, Khan KM, Purdam C. Achilles tendinopathy. Manual Therapy 2002;7(3):121-130.
- ↑ 2.0 2.1 Roos EM, Engstrom M, Lagerquist A, Soderberg B. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy - a randomized trial with 1-year follow-up. Scand J Med Sci Sports. 2004;14:286-295.
- ↑ 3.0 3.1 Robinson JM, Cook JL, Purdam C et al. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. British J of Sports Med. 2001;35:335-341.
- ↑ Robbins Rehabilitations. Eccentric Heel Raises. Available from: http://www.youtube.com/watch?v=8U-xPkW_RAY [last accessed 01/12/12]
- ↑ Jenna Beaudry. Achilles Tendonitis Tape Job. Available from: http://www.youtube.com/watch?v=xzRhIyw85Xk [last accessed 01/12/12]
- ↑ Aaron Tomlinson. Achilles Tape Application. Available from: http://www.youtube.com/watch?v=fQAwpCToR48 [last accessed 01/12/12]