Clavicular Fracture: Difference between revisions
No edit summary |
(text, refs) |
||
| Line 83: | Line 83: | ||
* Only go as far as you can naturally, without doing any trick movements to try and get any further. | * Only go as far as you can naturally, without doing any trick movements to try and get any further. | ||
* The movement should increase over time and should not be forced.<ref>Virtual fracture clinic. [https://www.fracturecare.co.uk/care-plans/shoulder/mid-shaft-clavicle-fracture/clavicle-with-fu-6-52/ Clavicle Fracture]. Available from: https://www.fracturecare.co.uk/care-plans/shoulder/mid-shaft-clavicle-fracture/clavicle-with-fu-6-52/ (last accessed 22.12.2019)</ref> | * The movement should increase over time and should not be forced.<ref>Virtual fracture clinic. [https://www.fracturecare.co.uk/care-plans/shoulder/mid-shaft-clavicle-fracture/clavicle-with-fu-6-52/ Clavicle Fracture]. Available from: https://www.fracturecare.co.uk/care-plans/shoulder/mid-shaft-clavicle-fracture/clavicle-with-fu-6-52/ (last accessed 22.12.2019)</ref> | ||
For people returning to sports or heavy work | |||
Weeks 12 And Beyond | |||
* Start a more aggressive strengthening program as tolerated. | |||
* Increase the intensity of strength and functional training for gradual return to activities and sports. | |||
* Return to specific sports is determined by the physical therapist through functional testing specific to the patient’s demands | |||
* completion of Sports Test for specific initial return to sports and progressive sport-specific training<ref>Stone clinic [https://www.stoneclinic.com/broken-collarbone-rehab-protocol Broken collar bone] Available from: https://www.stoneclinic.com/broken-collarbone-rehab-protocol (last accessed 22.12.2019)</ref> | |||
=== Surgical Treatment === | === Surgical Treatment === | ||
'''Surgical treatment''' is performed to align the bone ends and hold them stable during healing. | |||
It may be considered for | |||
* multiple fractures, | |||
* compound (open) fractures, | |||
* Overlapping of the broken ends of bone (shortened clavicle) | |||
* fractures associated with nerve or blood vessel damage and | |||
* displaced fractures. | |||
=== Clavicle Fracture Surgery === | |||
During this surgical procedure, the broken bone-ends are aligned into their normal position and screws in metal plates are used to hold the bone fragments in place. | |||
These plates and screws are usually left in the bone. If they cause any irritation, they can be removed after fracture healing is complete. | |||
{{#ev:youtube|wbCRHMqZ3yU}} | {{#ev:youtube|wbCRHMqZ3yU}} | ||
= References = | = References = | ||
<references /> | <references /> | ||
Revision as of 07:39, 22 December 2019
Original Editor - Sofie Van Cutsem
Top Contributors - Elvira Muhic, Sofie Van Cutsem, Manisha Shrestha, Lucinda hampton, Kim Jackson, Nupur Smit Shah, WikiSysop, Claire Knott, Tony Lowe, Naomi O'Reilly and Karen Wilson
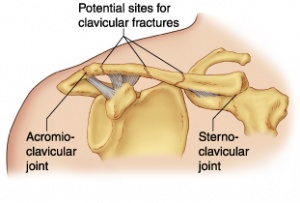
Clinical Anatomy[edit | edit source]
The clavicle is located between the sternum and the scapula, and it connects the arm to the body.[1] The clavicle is the first bone in the human body to begin intramembranous ossification directly from mesenchyme during the fifth week of fetal life. Similar to all long bones, the clavicle has both a medial and lateral epiphysis. The growth plates of the medial and lateral clavicular epiphyses do not fuse until the age of 25 years.Peculiar among long bones is the clavicle’s S-shaped double curve, which is convex medially and concave laterally. This contouring allows the clavicle to serve as a strut for the upper extremity, while also protecting and allowing the passage of the axillary vessels and brachial plexus medially.[2]
Clavicle Fracture[edit | edit source]
A clavicle fracture is also known as a broken collarbone.[1] Clavicle fractures are very common injuries in adults (2–5%) and children (10–15%) and represent the 44–66% of all shoulder fractures. It is the most common fracture of childhood. A fall onto the lateral shoulder most frequently causes a clavicle fracture. Radiographs confirm the diagnosis and aid in further evaluation and treatment. While most clavicle fractures are treated conservatively, severely displaced or comminuted fractures may require surgical fixation[3].
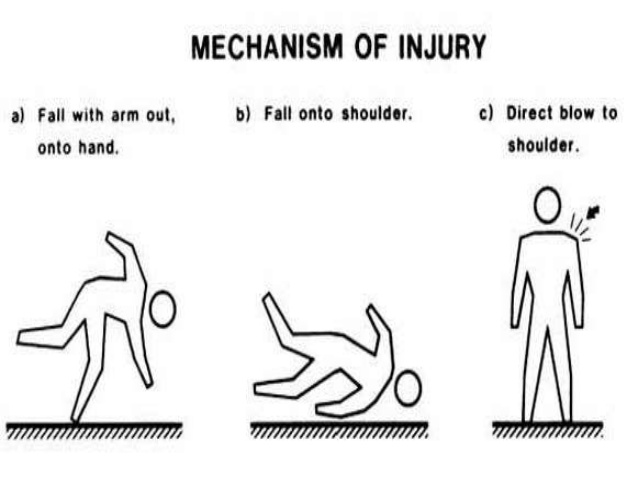
Etiology[edit | edit source]
Younger individuals often sustain these injuries by way of moderate to high-energy mechanisms such as motor vehicle accidents or sports injuries, whereas elderly individuals are more likely to sustain injuries because of the sequela of a low-energy fall. Although a fall onto an outstretched hand was traditionally considered the common mechanism, it has been found that the clavicle most often fails in direct compression from force applied directly to the shoulder.[2]
Epidemiology[edit | edit source]
Clavicle fractures represent 2% to 10% of all fractures. Clavicle fractures[3]
- affect 1 in 1000 people per year
- are the most common fractures during childhood
- approximately two-thirds of all clavicle fractures occurring in males.
- There is a bimodal distribution of clavicle fractures, with the 2 peaks being men younger than 25 (sports injuries) and patients older than 55 years of age (falls).
Classification[edit | edit source]
Fractures of the clavicle or typically described using the Allman classification system, dividing the clavicle into 3 groups based on location.
Fractures of the
middle third or midshaft fractures are in Group I,
distal or lateral third are in Group II
proximal or medial third are in Group III.[3]
- The middle third of the clavicle is fractured in 69% of cases, distal third is fractured in 28% of cases, proximal third is fractured in 3% of cases.
- The middle third of the clavicle represents 90% of fractures seen in children. In children younger than 10, these are frequently nondisplaced, while in children older than 10 the majority are displaced. Clavicle fractures represent 95% of fracture seen during childbirth.
Symptoms[edit | edit source]
Clinical signs and symptoms of clavicle fracture include the following:
- The patient may cradle the injured extremity with the uninjured arm
- The shoulder may appear shortened relative to the opposite side and may droop
- Swelling, ecchymosis, and tenderness may be noted over the clavicle
- Abrasion over the clavicle may be noted, suggesting that the fracture was from a direct mechanism
- Crepitus from the fracture ends rubbing against each other may be noted with gentle manipulation
- Difficulty breathing or diminished breath sounds on the affected side may indicate a pulmonary injury, such as a pneumothorax
- Palpation of the scapula and ribs may reveal a concomitant injury
- Tenting and blanching of the skin at the fracture site may indicate an impending open fracture, which most often requires surgical stabilization
- Nonuse of the arm on the affected side is a neonatal presentation
- Associated distal nerve dysfunction indicates a brachial plexus injury
- Decreased pulses may indicate a subclavian artery injury
Venous stasis, discoloration, and swelling indicate a subclavian venous injury.[4]
Diagnostic procedures and Differential Diagnosis[edit | edit source]
Diagnose can often be made by clients history and physical examination.[5]
The differential diagnosis of a clavicle fracture includes acromioclavicular joint injury, rib fracture, scapular fracture, shoulder dislocation, rotator cuff injury, and sternoclavicular joint injury. Possible complications of clavicle fractures must also be fully evaluated, including pneumothorax, brachial plexus injury, and subclavian vessel injury.[3]
Laboratory studies are ordered in clavicle fractures according to the severity of trauma. With suspected vascular injury, obtain a complete blood count (CBC) to check the hemoglobin and hematocrit values. If a pulmonary injury is suspected or identified, perform an arterial blood gas (ABG) test and obtain an expiration posteroanterior (PA) chest film. Other imaging studies that can be used in the assessment of a clavicle fracture include the following:
- Radiography of the clavicle and shoulder
- Computed tomography (CT) scanning with 3-dimensional (3-D) reconstruction
- Arteriography
- Ultrasonography[4]
Physiotherapy[edit | edit source]
Most clavicle fractures are treated conservatively and nonoperatively. Patients are immobilized in a sling or figure-of-eight brace until the clinical union is achieved. This typically occurs by 6 to 12 weeks in adults and 3 to 6 weeks in children. Patients should perform a range of motion and strengthen exercises under the care physical therapy once immobilization is no longer necessary. Patients typically may resume full daily activity approximately 6 weeks after injury. Requiring 2 to 4 months of rehabilitation, return to full contact sports requires the athlete should demonstrate radiographic evidence of bony healing, no tenderness to palpation, a full range of motion, and normal shoulder strength.[3]
Advice for a new injury and 0-3 weeks post injury
- Cold packs: A cold pack (ice pack or frozen peas wrapped in a damp towel) can provide short term pain relief. Apply this to the sore area for up to 15 minutes, every few hours ensuring the ice is never in direct contact with the skin.
- Rest: Try to rest your shoulder for the first 24-72 hours. However, it is important to maintain movement. Gently move your shoulder following the exercises shown. These should not cause too much pain. This will ensure your shoulder does not become stiff and it will help the healing process.
- Wear the sling during the day, except for exercises and personal hygiene. Clients choice to wear at night or not.
- Client starts Finger and wrist flexion and extension, Elbow Bend to Straighten, Forearm Rotations and Postural awareness instructions and training given
- Do not lift your elbow above shoulder height as this may be painful.
Therapy/advice 3-6 weeks post injury
- Try not to use the sling.
- Begin normal light activities with the arm and shoulder.
- Increase movement: Active assisted Shoulder flexion 4 to 5 times daily, Active assisted External rotation 4 to 5 times daily.
- Avoid heavy lifting for the full 6 weeks.
Therapy/advice 6 weeks post injury
- Start active range of movement shoulder exercises ie Forward flexion, abduction and external rotation
- Perform these exercises 10 times each.
- Only go as far as you can naturally, without doing any trick movements to try and get any further.
- The movement should increase over time and should not be forced.[6]
For people returning to sports or heavy work
Weeks 12 And Beyond
- Start a more aggressive strengthening program as tolerated.
- Increase the intensity of strength and functional training for gradual return to activities and sports.
- Return to specific sports is determined by the physical therapist through functional testing specific to the patient’s demands
- completion of Sports Test for specific initial return to sports and progressive sport-specific training[7]
Surgical Treatment[edit | edit source]
Surgical treatment is performed to align the bone ends and hold them stable during healing.
It may be considered for
- multiple fractures,
- compound (open) fractures,
- Overlapping of the broken ends of bone (shortened clavicle)
- fractures associated with nerve or blood vessel damage and
- displaced fractures.
Clavicle Fracture Surgery[edit | edit source]
During this surgical procedure, the broken bone-ends are aligned into their normal position and screws in metal plates are used to hold the bone fragments in place.
These plates and screws are usually left in the bone. If they cause any irritation, they can be removed after fracture healing is complete.
References[edit | edit source]
- ↑ 1.0 1.1 American Academy of Orthopaedic Surgeons. Clavicle Fracture (Broken Collarbone). www.orthoinfo.aaos.org/topic.cfm?topic=a00072
- ↑ 2.0 2.1 Paladini, P et al. “Treatment of Clavicle Fractures.” Translational Medicine @ UniSa 2 (2012)
- ↑ 3.0 3.1 3.2 3.3 3.4 Bentley TP, Journey JD. Clavicle Fractures. InStatPearls [Internet] 2019 Jan 19. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507892/ (last accessed 22.12.2019)
- ↑ 4.0 4.1 Medscape. Kleinhenz BP, Young CC, Clavicle Fractures. www.emedicine.medscape.com/article/92429-overview#showall
- ↑ M. Pecci, J. Kreher, MD, Boston university, Clavicle fractures, jan. 2008. Level of evidence: 1 Grade of recommendation: B
- ↑ Virtual fracture clinic. Clavicle Fracture. Available from: https://www.fracturecare.co.uk/care-plans/shoulder/mid-shaft-clavicle-fracture/clavicle-with-fu-6-52/ (last accessed 22.12.2019)
- ↑ Stone clinic Broken collar bone Available from: https://www.stoneclinic.com/broken-collarbone-rehab-protocol (last accessed 22.12.2019)