Functional Independence Measure (FIM): Difference between revisions
No edit summary |
Kapil Narale (talk | contribs) No edit summary |
||
| (18 intermediate revisions by 10 users not shown) | |||
| Line 2: | Line 2: | ||
'''Original Editor '''- [[User:Ajay Upadhyay|Ajay Upadhyay]] | '''Original Editor '''- [[User:Ajay Upadhyay|Ajay Upadhyay]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
The Functional Independence Measure (FIM ) is an | == Objective == | ||
[[File:PP Disability Images.jpg|right|frameless|350x350px]] | |||
The Functional Independence Measure (FIM) is an instrument that was developed as a measure of [[International Classification of Functioning, Disability and Health (ICF)|disability]] for a variety of populations and is not specific to any diagnosis. The FIM instrument | |||
* Includes measures of independence for self-care, including sphincter control, transfers, [[Ageing and the Locomotor System|locomotion]], [[Communication in Healthcare|communication]], and social cognition<ref>Cameron MH, Monroe L. Physical Rehabilitation-E-Book: Evidence-based examination, evaluation, and intervention. Elsevier Health Sciences; 2007 Apr 5.Available: https://www.sciencedirect.com/topics/medicine-and-dentistry/functional-independence-measure<nowiki/>(accessed 22.5.2021)</ref>. | |||
* Is an 18-item, seven-level, ordinal scale intended to be sensitive to changes over the course of a comprehensive inpatient medical rehabilitation program. | |||
* Uses the level of assistance an individual needs to grade functional status from total independence to total assistance). | |||
* The tool is used to assess a patient's level of disability as well as a change in patient status in response to [[Introduction to Rehabilitation|rehabilitation]] or medical intervention.<ref name=":0">Linacre JM, Heinemann JW, Wright BD, Granger CV, Hamilton BB. The structure and stability of the functional independence measure. Arch Phys Med Rehabil. 1994. 75: 127-132.</ref><ref name=":1">Heinemann AW, Linacre JM, Wright BD, Hamilton BB, Granger C. Relationships between impairment and physical disability as measured by the functional independence measure. Arch Phys Med Rehabil. 1993. 74: 566-573. </ref> | |||
== | == Intended Population == | ||
Designed to assess areas of dysfunction in activities that commonly occur in subjects with any progressive, reversible or stable [[Neurological Disorders|neurologic]], musculoskeletal, or other disorder ie patients with functional mobility impairments<ref>Elia AE, Graziella F, Albanese A. [https://www.sciencedirect.com/topics/medicine-and-dentistry/functional-independence-measure 12 Clinical Trials of Botulinum Toxin in Adult Spasticity.] Botulinum Toxin E-Book: Therapeutic Clinical Practice and Science. 2009 Feb 18:148.Available from: https://www.sciencedirect.com/topics/medicine-and-dentistry/functional-independence-measure<nowiki/>(accessed 22.5.2021)</ref>. | |||
The FIM | The FIM is used by healthcare practitioners to assess and grade the functional status of a person based on the level of assistance he or she requires. | ||
== Method of Use == | |||
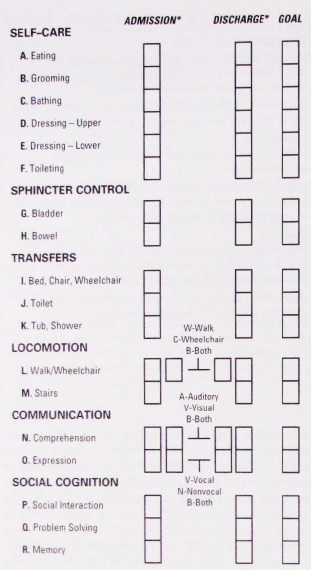
[[Image:Functional Independence Measure.jpg|right|alt=|frameless|570x570px]]Guide for use: Patient function is assessed using the FIM™ instrument at the start of a rehabilitation episode of care and at the end of a rehabilitation episode of care. Admission assessment is collected within 72 hours of the start of a rehabilitation episode. Discharge assessment is collected within 72 hours prior to the end of a rehabilitation episode. | |||
FIM™ is comprised of 18 items, grouped into 2 subscales - motor and cognition. | |||
The | The motor subscale includes: | ||
* Eating | |||
* Grooming | |||
* Bathing | |||
* Dressing, upper body | |||
* Dressing, lower body | |||
* Toileting | |||
* Bladder management | |||
* Bowel management | |||
* Transfers - bed/chair/wheelchair | |||
* Transfers - toilet | |||
* Transfers - bath/shower | |||
* Walk/[[Wheelchair Assessment - Assessment Interview|wheelchair]] | |||
* Stairs | |||
The cognition subscale includes: | |||
* Comprehension | |||
* Expression | |||
* Social interaction | |||
* Problem solving | |||
* [[Memory]] | |||
Each item is scored on a 7 point ordinal scale, ranging from a score of 1 to a score of 7. The higher the score, the more independent the patient is in performing the task associated with that item.<ref name=":2">AIHW FIM Available from:https://meteor.aihw.gov.au/content/index.phtml/itemId/495857 (accessed 22.5.20210</ref> | |||
FIM levels | |||
'''No Helper''' | |||
6. Modified Independence | * 7. Complete Independence (Timely, Safety) | ||
* 6. Modified Independence (Device) | |||
(Device) | |||
'''Helper - Modified Dependence''' | '''Helper - Modified Dependence''' | ||
5. Supervision | * 5. Supervision (Subject = 100%) | ||
* 4. Minimal Assistance (Subject = 75% or more) | |||
(Subject = 100%) | * 3. Moderate Assistance (Subject = 50% or more) | ||
4. Minimal Assistance | |||
(Subject = 75% or more) | |||
3. Moderate Assistance | |||
(Subject = 50% or more) | |||
'''Helper - Complete Dependence''' | '''Helper - Complete Dependence''' | ||
(Subject less than 25%) | * 2. Maximal Assistance (Subject = 25% or more) | ||
* 1. Total Assistance or not Testable (Subject less than 25%) | |||
< | Leave no blanks. Enter 1 if not testable due to risk.<ref name=":0" /> | ||
The total score for the FIM | |||
* motor subscale (the sum of the individual motor subscale items) will be a value between 13 and 91. | |||
* cognition subscale (the sum of the individual cognition subscale items) will be a value between 5 and 35. | |||
= | The total score for the FIM instrument (the sum of the motor and cognition subscale scores) will be a value between 18 and 126.<ref name=":2" /> | ||
== Reliability and Validity == | |||
Inter Rater Reliability ( | # Inter-Rater Reliability of FIM has been established at an acceptable [[Psychometric Properties|psychometric]] performance (Intraclass co-relation coefficients ranging from 0.86 to 0.88) | ||
# The concurrent validity with [[Barthel Index]] (ICC > 0.83) have shown strong construct validity between items on Barthel Index and items on the FIM the measure functional limitations<ref>Gosman-Hedstrom, G, and Svensson, E: Parallel reliability of the Functional Independence Measure and the Barthel index ADLIndex. Psychiatry 73:188, 2000</ref><br> | |||
== References == | == References == | ||
<references /> | |||
[[Category:Outcome Measures]] | |||
[[Category:Older People/Geriatrics]] | |||
[[Category:Activities of Daily Living]] | |||
[[Category:Older People/Geriatrics - Outcome Measures]] | |||
[[Category:Stroke]] | |||
[[Category:Stroke - Assessment and Examination]] | |||
[[Category:Spinal Cord Injuries]] | |||
Latest revision as of 06:04, 7 February 2023
Original Editor - Ajay Upadhyay
Top Contributors - Laura Ritchie, Gayatri Jadav Upadhyay, Ajay Upadhyay, Lucinda hampton, Nikhil Benhur Abburi, Kim Jackson, Kapil Narale, Evan Thomas, WikiSysop, Vidya Acharya, Nicole Hills and Lauren Lopez
Objective[edit | edit source]
The Functional Independence Measure (FIM) is an instrument that was developed as a measure of disability for a variety of populations and is not specific to any diagnosis. The FIM instrument
- Includes measures of independence for self-care, including sphincter control, transfers, locomotion, communication, and social cognition[1].
- Is an 18-item, seven-level, ordinal scale intended to be sensitive to changes over the course of a comprehensive inpatient medical rehabilitation program.
- Uses the level of assistance an individual needs to grade functional status from total independence to total assistance).
- The tool is used to assess a patient's level of disability as well as a change in patient status in response to rehabilitation or medical intervention.[2][3]
Intended Population[edit | edit source]
Designed to assess areas of dysfunction in activities that commonly occur in subjects with any progressive, reversible or stable neurologic, musculoskeletal, or other disorder ie patients with functional mobility impairments[4].
The FIM is used by healthcare practitioners to assess and grade the functional status of a person based on the level of assistance he or she requires.
Method of Use[edit | edit source]
Guide for use: Patient function is assessed using the FIM™ instrument at the start of a rehabilitation episode of care and at the end of a rehabilitation episode of care. Admission assessment is collected within 72 hours of the start of a rehabilitation episode. Discharge assessment is collected within 72 hours prior to the end of a rehabilitation episode.
FIM™ is comprised of 18 items, grouped into 2 subscales - motor and cognition.
The motor subscale includes:
- Eating
- Grooming
- Bathing
- Dressing, upper body
- Dressing, lower body
- Toileting
- Bladder management
- Bowel management
- Transfers - bed/chair/wheelchair
- Transfers - toilet
- Transfers - bath/shower
- Walk/wheelchair
- Stairs
The cognition subscale includes:
- Comprehension
- Expression
- Social interaction
- Problem solving
- Memory
Each item is scored on a 7 point ordinal scale, ranging from a score of 1 to a score of 7. The higher the score, the more independent the patient is in performing the task associated with that item.[5]
FIM levels
No Helper
- 7. Complete Independence (Timely, Safety)
- 6. Modified Independence (Device)
Helper - Modified Dependence
- 5. Supervision (Subject = 100%)
- 4. Minimal Assistance (Subject = 75% or more)
- 3. Moderate Assistance (Subject = 50% or more)
Helper - Complete Dependence
- 2. Maximal Assistance (Subject = 25% or more)
- 1. Total Assistance or not Testable (Subject less than 25%)
Leave no blanks. Enter 1 if not testable due to risk.[2]
The total score for the FIM
- motor subscale (the sum of the individual motor subscale items) will be a value between 13 and 91.
- cognition subscale (the sum of the individual cognition subscale items) will be a value between 5 and 35.
The total score for the FIM instrument (the sum of the motor and cognition subscale scores) will be a value between 18 and 126.[5]
Reliability and Validity[edit | edit source]
- Inter-Rater Reliability of FIM has been established at an acceptable psychometric performance (Intraclass co-relation coefficients ranging from 0.86 to 0.88)
- The concurrent validity with Barthel Index (ICC > 0.83) have shown strong construct validity between items on Barthel Index and items on the FIM the measure functional limitations[6]
References[edit | edit source]
- ↑ Cameron MH, Monroe L. Physical Rehabilitation-E-Book: Evidence-based examination, evaluation, and intervention. Elsevier Health Sciences; 2007 Apr 5.Available: https://www.sciencedirect.com/topics/medicine-and-dentistry/functional-independence-measure(accessed 22.5.2021)
- ↑ 2.0 2.1 Linacre JM, Heinemann JW, Wright BD, Granger CV, Hamilton BB. The structure and stability of the functional independence measure. Arch Phys Med Rehabil. 1994. 75: 127-132.
- ↑ Heinemann AW, Linacre JM, Wright BD, Hamilton BB, Granger C. Relationships between impairment and physical disability as measured by the functional independence measure. Arch Phys Med Rehabil. 1993. 74: 566-573.
- ↑ Elia AE, Graziella F, Albanese A. 12 Clinical Trials of Botulinum Toxin in Adult Spasticity. Botulinum Toxin E-Book: Therapeutic Clinical Practice and Science. 2009 Feb 18:148.Available from: https://www.sciencedirect.com/topics/medicine-and-dentistry/functional-independence-measure(accessed 22.5.2021)
- ↑ 5.0 5.1 AIHW FIM Available from:https://meteor.aihw.gov.au/content/index.phtml/itemId/495857 (accessed 22.5.20210
- ↑ Gosman-Hedstrom, G, and Svensson, E: Parallel reliability of the Functional Independence Measure and the Barthel index ADLIndex. Psychiatry 73:188, 2000