|
|
| (14 intermediate revisions by 3 users not shown) |
| Line 4: |
Line 4: |
| '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} |
| </div> | | </div> |
| == Definition/Description == | | == Introduction == |
| “Pneumonia is an infection of the lung tissue. When a person has pneumonia the air sacs in their lungs become filled with microorganisms, fluid and inflammatory cells and their lungs are not able to work properly. Diagnosis of pneumonia is based on symptoms and signs of an acute lower respiratory tract infection, and can be confirmed by a chest X-ray showing new shadowing that is not due to any other cause (such as pulmonary oedema or infarction)." <ref name="NICE 2">http://www.nice.org.uk/guidance/cg191/resources/cg191-pneumonia-costing-statement2</ref> (NICE clinical guidelines 2014)
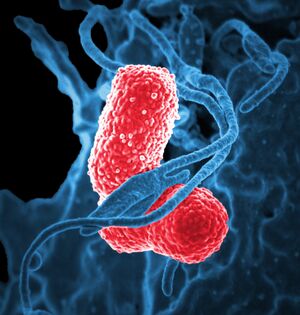
| | [[File:Multidrug-resistant Klebsiella pneumoniaeand neutrophil.jpeg|thumb|Multidrug-resistant bacteria and WBC]] |
| | Hospital-acquired [[pneumonia]] (HAP) is defined as pneumonia that occurs 48 hours or more after hospital admission and is not incubating at hospital admission. |
|
| |
|
| '''Hospital-acquired pneumonia'''
| | # Early-onset (occurring within 4 days of admission) HAP is usually caused by the same [[Bacterial Infections|bacteria]] and [[Viral Infections|viruses]] as community-acquired pneumonia and has a good prognosis. |
| | | # Late-onset (starting 5 days or more after admission) HAP has a worse prognosis and is usually caused by micro-organisms that are acquired from the hospital environment. MRSA, Pseudomonas aeruginosa and other non-pseudomonal Gram-negative bacteria are the most common causes."<ref>NICE [https://www.nice.org.uk/advice/esnm44 Hospital-acquired pneumonia caused by methicillin-resistant Staphylococcus aureus: telavancin] Available:http://www.nice.org.uk/advice/esnm44/chapter/full-evidence-summary (accessed 25.12.2022)</ref> |
| "Hospital-acquired pneumonia is defined as pneumonia that occurs 48 hours or more after hospital admission and is not incubating at hospital admission. Early-onset (occurring within 4 days of admission) hospital-acquired pneumonia is usually caused by the same bacteria and viruses as community-acquired pneumonia and has a good prognosis. Late-onset (starting 5 days or more after admission) hospital-acquired pneumonia has a worse prognosis and is usually caused by micro-organisms that are acquired from the hospital environment. MRSA, Pseudomonas aeruginosa and other non-pseudomonal Gram-negative bacteria are the most common causes."<ref>http://www.nice.org.uk/advice/esnm44/chapter/full-evidence-summary</ref> (NICE Guidelines. Published: 15 July 2014)
| | HAP is the second most common hospital acquired infection (see [[Healthcare-Associated Infections]]), catheter-associated [[Urinary Tract Infection|urinary tract infections]] being the most common.<ref name=":1">American [https://www.myamericannurse.com/preventing-hospital-acquired-pneumonia/ Nurse Preventing hospital-acquired pneumonia]Available:https://www.myamericannurse.com/preventing-hospital-acquired-pneumonia/ (accessed 25.12.20220</ref> |
|
| |
|
| == Epidemiology == | | == Epidemiology == |
|
| |
|
| “At any time 1.5% of hospital inpatients in England have a hospital-acquired respiratory infection, more than half of which are hospital-acquired pneumonia and are not associated with intubation. Hospital-acquired pneumonia is estimated to increase hospital stay by about 8 days and has a reported mortality rate that ranges from 30–70%. Variations in clinical management and outcome occur across the UK.”<ref name="NICE 2" /> HAP and VAP together are the second most common cause of hospital-acquired infection and have been associated with a higher mortality than any other nosocomial infection.<ref name=":0">Rotstein C, Evans G, Born A, Grossman R, Light RB, Magder S, McTaggart B, Weiss K, Zhanel GG. Clinical practice guidelines for hospital-acquired pneumonia and ventilator-associated pneumonia in adults. Canadian Journal of Infectious Diseases and Medical Microbiology. 2008;19(1):19-53.</ref> HAP is the second most common nosocomial infection with a crude overall rate of 6.1 per 1000 discharges<ref>Nosocomial infection rates for interhospital comparison: Limitations and possible solutions. A report from the National Nosocomial Infections Surveillance (NNIS) System. Infect Control Hosp Epidemiol. 1991;12:609–21.</ref>
| | # HAP is a common cause of pneumonia in those admitted to [[Physiotherapists Role in ICU|intensive care units]] (ICU) or on mechanical [[Ventilation and Weaning|ventilation]]. 9/10 cases of HAP develope in ICUs occur in patients who are intubated and mechanically ventilated. |
| | | # The elderly are more are risk of developing HAP.<ref>Radiopedia [https://radiopaedia.org/articles/hospital-acquired-pneumonia-1?lang=us Hospital-acquired pneumonia] Available:https://radiopaedia.org/articles/hospital-acquired-pneumonia-1?lang=us (accessed 24.12.2022)</ref> |
| Ventilator-acquired pneumonia (VAP) has been studied more comprehensively than HAP. A clear reason for this is VAP is responsible for 86% of the HAP reported<ref name="masterton">Masterton, R. G., Galloway, A., French, G., Street, M., Armstrong, J., Brown, E., & Wilcox, M. (2008). Guidelines for the management of hospital-acquired pneumonia in the UK: report of the working party on hospital-acquired pneumonia of the British Society for Antimicrobial Chemotherapy. Journal of Antimicrobial Chemotherapy, 62(1), 5-34.</ref>. <br>The incidence rate of HAP is between 3 and 10 per 1000 hospital admissions<ref name="kieninger">Kieninger, A. N., & Lipsett, P. A. (2009). Hospital-acquired pneumonia: pathophysiology, diagnosis, and treatment. Surgical Clinics of North America, 89(2), 439-461.</ref><ref name="stolbrink">Stolbrink, M., McGowan, L., Saman, H., Nguyen, T., Knightly, R., Sharpe, J., ... & Turner, A. M. (2014). The Early Mobility Bundle: a simple enhancement of therapy which may reduce incidence of hospital-acquired pneumonia and length of hospital stay. Journal of Hospital Infection, 88(1), 34-39.</ref>.
| |
| | |
| Mortality rates from VAP are between 24 and 50% but it is reported to jump to 76% if it is caused my multi drug resistant pathogens that are often linked to later stage pneumonia (> 5days in hospital)<ref name="masterton" />. Although it is difficult to determine the exact cause of death in critically ill patients, which will cause discrepancies in any date, Accurate antibiotics taken at the right time has shows to lower mortality rate for HAP.<br>The chance of infection is estimated to be 3%/day during the first 5 days of ventilation, followed by 2%/day up to day 10 of ventilation and there- after 1%/day.<ref>American Thoracic Society, & Infectious Diseases Society of America. (2005). Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med, 171, 388-416.</ref>
| |
| == Aetiology ==
| |
| | |
| The most common cause is an accumulation of bacteria, most ordinarily gram-negative bacilli and staphlycoccus aureus, which inhabit the oropharynx and upper airways in seriously ill and ventilated patients<ref name="luna">Luna, Carlos M., Angela Famiglietti, Rubén Absi, Alejandro J. Videla, Facundo J. Nogueira, Alejandro Diaz Fuenzalida, and Ricardo J. Gené. "Community-acquired pneumonia: etiology, epidemiology, and outcome at a teaching hospital in Argentina." CHEST Journal 118, no. 5 (2000): 1344-1354.</ref>. A less common cause is seeding of the lung due to bacteremia; a bacterium that originates in the patients’ blood supply and can transferred to the lungs during gas exchange. Finally inhalation of bacterially contaminated aerosols which transport airborne particles containing Legionella sp, Aspergillus sp, or influenza virus, although this is a relatively unfamiliar form of contracting hospitalized pneumonia<ref name="luna" />.<br>Endotracheal intubation with mechanical ventilation poses the greatest overall risk<ref name="Ntoumenopoulos">Ntoumenopoulos, G., J. Presneill, M. McElholum, and J. Cade. "Chest physiotherapy for the prevention of ventilator-associated pneumonia." Intensive care medicine 28, no. 7 (2002): 850-856.</ref>. Ventilation Associated Pneumonia is a subcategory of hospitalized and contributes more than 85% of all cases, with pneumonia occurring in up to 27% of ventilated patients<ref name="Ntoumenopoulos" />. Endotracheal intubation related bacteria embed themselves deep into the endotracheal tube cuff enabling them to avoid the body' nature immune response while also providing a biofilm of protection from antibiotics<ref name="luna" />.<br>In non-intubated patients, risk factors include previous antibiotic treatment, high gastric pH, resulting from cardiac, pulmonary, hepatic, or renal deficiencies<ref name="luna" />. Major risk factors for postoperative pneumonia are patients older than 70, abdominal or thoracic surgery, and cardiorespiratory functional depletion<ref name="luna" />.
| |
| | |
| Many patients at risk for HAP and VAP have underlying medical conditions that put them at higher risk for acquiring antibiotic-resistant organisms (AROs).<ref name=":0" />
| |
| == Investigations ==
| |
| | |
| HAP or VAP should be suspected in all patients, whether ventilated or not, if two or more of the following clinical features are present: temperature greater than 38°C or less than 36°C; leukopenia or leukocytosis; purulent tracheal secretions and decreased partial pressure of oxygen in arterial blood (PaO2).<ref name=":0" />
| |
| | |
| General investigations are not necessary for the majority of patients who are managed in the community. Pulse oximeters allow for simple assessment of oxygenation. When a patient is admitted to hospital:<br>
| |
| | |
| '''FBC with differential white cell count: '''<br>Total white blood cells: All the white cell types are given as a percentage, and as an absolute number per liter. A high WBC is often an indicator of infection<ref name="osei">Osei‐Bimpong, A., R. McLean, E. Bhonda, and S. M. Lewis. "The use of the white cell count and haemoglobin in combination as an effective screen to predict the normality of the full blood count." International journal of laboratory hematology 34, no. 1 (2012): 91-97.</ref>.<br>CRP (to aid diagnosis and as a baseline measure). The C-reactive protein (CRP) test is a diagnostic tool that identifies regions of inflammation<ref name="tracy">Tracy, Russell P., Rozenn N. Lemaitre, Bruce M. Psaty, Diane G. Ives, Rhobert W. Evans, Mary Cushman, Elaine N. Meilahn, and Lewis H. Kuller. "Relationship of C-reactive protein to risk of cardiovascular disease in the elderly results from the Cardiovascular Health Study and the Rural Health Promotion Project." Arteriosclerosis, thrombosis, and vascular biology 17, no. 6 (1997): 1121-1127.</ref>. CRP is a protein manufactured in the liver before dispersal into the blood which occurs a few hours after any form of tissue injury, an acute manifestation of infection, or inflammation caused by another source<ref name="tracy" />. The CRP test can be used in adjunction with signs, symptoms and other tests in order to fully evaluate patients with HAP<ref name="tracy" />.<br>'''Blood cultures: '''<br>Blood culture is a microbiological culture of blood. It is employed to detect infections that are spreading through the bloodstream (such as bacteremia, septicemia amongst others).<br>'''Pneumococcal and legionella urinary antigen tests: '''<br>Urine tests are administered and designed to locate the presence of both Streptococcus pneumoniae and Legionella species<ref name="marcos">Marcos, M. A., MT Jimenez de Anta, J. P. De La Bellacasa, J. González, E. Martinez, E. Garcia, J. Mensa, A. De Roux, and A. Torres. "Rapid urinary antigen test for diagnosis of pneumococcal community-acquired pneumonia in adults." European Respiratory Journal 21, no. 2 (2003): 209-214.</ref>. Two major pathogens in HAP, which also play a key role in community acquired Pneumonia. The tests are usually in conjunction with both sputum examination and blood testing due to their high specificity<ref name="marcos" />.<br>'''CXR: '''<br> HAP may deliver signs of abnormal opacity in specific areas of the lungs, or even clear consolidation due to inflammation causing abnormal positioning of structures, such as the trachea and mediastinum<ref name="pugin">Pugin, Jérôme, Raymond Auckenthaler, Nabil Mili, Jean-Paul Janssens, P. Daniel Lew, and Peter M. Suter. Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and nonbronchoscopic blind bronchoalveolar lavage fluid. American Review of Respiratory Disease 143, no. 5_pt_1 (1991): 1121-1129.</ref>.
| |
| | |
| '''Sputum examination and culture. ''' <br>Sputum Examination is a diagnostic tool used to identify bacteria and fungi located in the pulmonary facet<ref name="musher">Musher, Daniel M., Roberto Montoya, and Anna Wanahita. "Diagnostic value of microscopic examination of Gram-stained sputum and sputum cultures in patients with bacteremic pneumococcal pneumonia." Clinical infectious diseases 39, no. 2 (2004): 165-169.</ref>. Samples are often obtained through expectorating or in some cases an induced saline can produce the required volumes from lab testing. HAP normally produces sputum in a thick and purulent form, which is common in more cases of infection<ref name="musher" />.<br>'''Blood gases: '''<br>Blood gases will demonstrate how well both the respiratory and the renal systems are functioning<ref name="marc">Marc A. Rodger, Marc Carrier, Gwynne N. Jones, Pasteur Rasuli, Francois Raymond, Helene Djunaedi, and Philp S. Wells. "Diagnostic Value of Arterial Blood Gas Measurement in Suspected Pulmonary Embolism", American Journal of Respiratory and Critical Care Medicine, Vol. 162, No. 6 (2000), pp. 2105-2108.</ref>. In terms of HAP ABG’s can be used to gain insight into the patient’s oxygen saturation levels as well as demonstrate incidences of both acidosis and alkalosis, both of which can occur due to poor ventilation<ref name="marc" />.<br>'''Aspiration of pleural fluid (for biochemistry and culture). '''<br>Chest aspiration is a diagnostic tool used to investigate the cause of pleural fluid or to improve respiration rates that have dropped due to accumulated fluid<ref name="blackmore" />. Samples of the pleural fluid are sent for analysis which includes cytology for malignant cells and bacteriology for identification of foreign bacteria<ref name="blackmore">Blackmore CC, Black WC, Dallas RV, et al. Pleural fluid volume estimation: a chest radiograph prediction rule. Acad Radiol 1996;3:103–9.</ref>. <br>
| |
| == Clinical Manifestations ==
| |
| | |
| A patient that develops new or extra pulmonary infiltrates and a fever are signs of HAP. In order to differentiate HAP and other pathologies diagnosis should be based on a radiographic x-ray. To diagnose HAP radiological opacity with alveolar condensation must be present.<ref name="Rello, J.">Rello, J., Vidaur, L., Díaz, E., & Rodríguez, A. (2007). Management of Hospital-Associated Pneumonia in the Intensive Care Unit. In Infectious Diseases in Critical Care (pp. 449-455). Springer Berlin Heidelberg.</ref><br>
| |
|
| |
|
| '''The time of onset of HAP is a large determinate of the type of bacteria causing the infection:'''
| | == Clinical Manifestations == |
|
| |
|
| '''Early-onset HAP''' ''occurring in the first 4 days of hospitalization) is often caused by community-acquired pathogens such as'': <br>Haemophilus influenzae, <br>Streptococcus pneumoniae, or <br>methicillin-susceptible S aureus (MSSA). <br>In this context, pathogens with strong intrinsic or acquired antimicrobial resistances are rarely causative.
| | # Symptoms of HAP: includes cough, expectoration, [[Fever|a rise in body temperature]], chest pain or [[Dyspnoea|dyspnea]]. |
| | | # Signs include of HAP include: fever, tachypnea, consolidations or crackles.<ref name=":2">Shebl E, Gulick PG. Nosocomial Pneumonia. InStatPearls [Internet] 2021 Jul 21. StatPearls Publishing.Available;https://www.ncbi.nlm.nih.gov/books/NBK535441/#!po=22.7273 (accessed 25.12.2022)</ref> |
| '''Late-onset HAP''' ''developing ≥ 5 days after hospitalization is often caused by aerobic Gram-negative bacilli such as:''<br>P aeruginosa, <br>Enterobacteriaceae, or <br>Acinetobacter) or <br>Methicillin-resistant Staphylococcus aureus (MRSA) Late-onset pneumonia is due to P aeruginosa, Acinetobacter, or MRSA in 30 to 71% of cases.
| |
|
| |
|
| | For more see [[Pneumonia]] |
| == Physiotherapy and Other Management == | | == Physiotherapy and Other Management == |
|
| |
|
| Other health professionals will be treating your patient. What is their input?When addressing HAP, respiratory physiotherapy interventions should be individually tailored around the patient’s symptoms, observing aspects such as degree of pain, mobility capabilities and an array of complex factors<ref name="denehy">Denehy L, Berney S. Physiotherapy in the intensive care unit. Physical Therapy Reviews. 2006;11(1):49.</ref>. Therefore techniques may include positional manipulations (addressing V/A matching and attempting to uses gravity to potentially enable drainage), manual hyperinflation, percussion, shaking, vibrations, suctioning (if huffing or cough promoting techniques are proving ineffective in regards to sputum extraction), breathing exercises including thoracic expansion and relaxing tidal volumes, while also engaging sputum reduction through active cycle and autogenic drainage techniques) as well as mobilization<ref name="denehy" />. The later of course demonstrating great importance not only in terms of improving the patients’ respiratory distress, but also in reducing overall hospitalization.<br>Published substantial evidence very much supports the role of physiotherapy in the respiratory managing HAF, demonstrating both short-term and longer term benefits<ref name="denehy" />. However, its essential to promote physiotherapy treatment as part of a multi-disciplinary approach as aspects including pharmaceutical interventions play an integral part in controlling bacterial diseases, promoting lung function and reducing problematic symptoms<ref>Berney S, Denehy L. A comparison of the effects of manual and ventilator hyperinflation on static lung compliance and sputum production in intubated and ventilated intensive care patients. Physiotherapy Research International. 2002;7(2):100.</ref>. | | Other health professionals will be treating your patient. What is their input? When addressing HAP, respiratory physiotherapy interventions should be individually tailored around the patient’s symptoms, observing aspects such as degree of pain, mobility capabilities and an array of complex factors<ref name="denehy">Denehy L, Berney S. [https://www.researchgate.net/publication/233585155_Denehy_L_Berney_S_Physiotherapy_in_the_intensive_care_unit_Phys_Ther_Rev_20061149-56 Physiotherapy in the intensive care unit.] Physical Therapy Reviews. 2006;11(1):49. Available: https://www.researchgate.net/publication/233585155_Denehy_L_Berney_S_Physiotherapy_in_the_intensive_care_unit_Phys_Ther_Rev_20061149-56 (accessed 25.12.2022)</ref>. |
| | |
| == Prevention ==
| |
|
| |
|
| Three European societies, (European Respiratory Society (ERS), European, Society of Clinical Microbiology and Infectious Diseases (ESCMID) and European Society of Intensive Care Medicine (ESICM), in 2008 produced a report to further the clinical guidelines of HAP and VAP. Within these guidelines they outline several measures that can have proven to reduce the likelihood of HAP.
| | Substantial evidence supports the role of physiotherapy in the respiratory managing HAP, demonstrating both short-term and longer term benefits<ref name="denehy" />. |
|
| |
|
| '''Generally recommended general measures:'''
| | Techniques may be found here [[Respiratory Physiotherapy]] and [[Respiratory Physiotherapy for ICU Patients]] Examples include: |
|
| |
|
| *Alcohol-based hand disinfection | | * [[Manual Hyperinflation|Manual hyperinflation]] |
| *Use of microbiologic surveillance | | * Percussion, shaking, vibrations, |
| *Monitoring and early removal of invasive devices | | * [[Suctioning]] (if huffing or cough promoting techniques are proving ineffective in regards to sputum extraction), |
| *Programs to reduce antimicrobial prescriptions
| | * [[Breathing Exercises|Breathing exercises]] |
| *Generally recommended specific measures
| | * Mobilization<ref name="denehy" />. <br> |
| *Avoidance of endotracheal intubation
| |
| *Avoidance of reintubation
| |
| *Preference of noninvasive ventilation (NIV)
| |
| *Preference of orotracheal intubation and orogastric tubes | |
| *Maintenance of the ET cuff pressure at approximately 20 cmH2O | |
| *Avoidance of flushing the condensate into the lower airway or to in-line medication nebulizers Patient positioning (semirecumbent position)<ref name="Torres">Torres, A., Ewig, S., Ruhrgebiet, T., und Augusta-Kranken, E. K. H., Bochum, A., Lode, H., ... & Saint Joseph, G. H. P. DIAGNOSING, TREATING AND PREVENTING HOSPITAL ACQUIRED PNEUMONIA: A EUROPEAN PERSPECTIVE. Intensive Care Med (2009) 35:9–29</ref>
| |
|
| |
|
| '''Additional measures which might be helpful in distinct settings and populations:'''
| | == Prognosis == |
| | HAP is linked with increased death rates. The death rates associated with VAP ranges from 20% to 50% in different studies.<ref name=":2" /> |
|
| |
|
| *Continuous aspiration of subglottic secretions
| | == Prevention == |
| *Endotracheal tubes coated with antiseptics or silver
| | Several basic nursing interventions are associated with reducing HAP risk— |
| *Preference of heat-moisture exchangers (HMEs) over heater humidifiers (HH)
| |
| *Oral decontamination
| |
| *Selective decontamination of the digestive tract (SDD)<ref name="Torres" /><br>
| |
| '''The VAP Guidelines Committee and the Canadian Critical Care Trials group in 2008 recommended several approaches to encourage a reduction in incidences<ref>Muscedere, J., Dodek, P., Keenan, S., Fowler, R., Cook, D., Heyland, D., ... & Canadian Critical Care Trials Group. (2008). Comprehensive evidence-based clinical practice guidelines for ventilator-associated pneumonia: prevention. Journal of critical care, 23(1), 126-137.</ref>:'''
| |
|
| |
|
| *The orotracheal route of intubation should be used when intubation is necessary | | * Following infection prevention standards |
| *There should be no scheduled ventilator circuit changes but new circuits for each patient, and changes if the circuits become soiled or damaged | | * Elevating the head of the bed 30 to 45 degrees to prevent aspiration |
| *Changes of heat and moisture exchangers with each patient, also every 5-7 days and as clinically indicated
| | * Seeing to good oral hygiene (cleaning teeth, gums, tongue, dentures) |
| *Closed endotracheal suctioning system, and that the system is changed for each patient and as clinically indicated.
| | * Increasing patient mobility with ambulation to eg three times a day (as appropriate) |
| *The use of subglottic secretion drainage in patients expected to be mechanically ventilated for > 72hrs | | * Educating patient re coughing and deep breathing, and use of incentive spirometry.<ref name=":1" /> |
| *Bed head to be elevated to 45°. If this angle is not possible then as much elevation as possible is recommended | |
| *The use of oral antiseptic chlorhexidine | |
| *The use of oral antiseptic povidone-iodione should be considered with patients with severe head injury
| |
| *Rotating beds should be considered
| |
| == Resources ==
| |
|
| |
|
| '''NHS website'''<br>http://www.nhs.uk/conditions/pneumonia/Pages/Introduction.aspx
| | For more see [[Infection Prevention and Control]] |
|
| |
|
| '''Patient website'''<br>http://www.patient.co.uk/health/pneumonia-leaflet
| |
| == References == | | == References == |
|
| |
|
| Line 95: |
Line 59: |
| [[Category:Cardiopulmonary]] | | [[Category:Cardiopulmonary]] |
| [[Category:Older People/Geriatrics]] | | [[Category:Older People/Geriatrics]] |
| | [[Category:Acute Respiratory Disorders - Conditions]] |
| | [[Category:Older People/Geriatrics - Conditions]] |