Hyperthyroidism: Difference between revisions
m (Text replace - ''''Lead Editors'''' to ''''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}') |
Kim Jackson (talk | contribs) m (Text replacement - "[[Hip Fracture|" to "[[Femoral Neck Hip Fracture|") |
||
| (21 intermediate revisions by 5 users not shown) | |||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
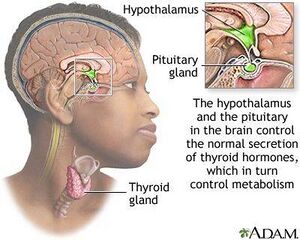
[[File:Thyroid and release.jpeg|thumb]] | |||
The term "hyperthyroidism" defines a syndrome associated with excess thyroid [[Hormones|hormone]] production<ref name=":1">Mathew P, Rawla P, Fortes K. Hyperthyroidism (Nursing).Available: https://www.ncbi.nlm.nih.gov/books/NBK537053/ (accessed 24.2.2022)</ref>. The [[Thyroid Gland|thyroid]] gland controls important metabolic processes such as growth and energy expenditure. In hyperthyroidism the thyroid gland is overactive. An [[Immune System|immune system]] abnormality called [[Graves' Disease|Graves' disease]] is the most common cause of hyperthyroidism. People treated for hyperthyroidism normally end up with an underactive thyroid ie [[hypothyroidism]]<ref name=":0">Better health channel Available: Thyroid hyperactivity<nowiki/>https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/thyroid-hyperthyroidism<nowiki/>(accessed 24.2.2022)</ref>. | |||
== Epidemiology == | |||
The prevalence of hyperthyroidism differs according to the ethnic group, while in Europe, the frequency is affected by dietary intake of Iodine, and some cases are due to autoimmune disease. | |||
= | * Subclinical hyperthyroidism occurs more in women older than 65 than in men | ||
* Overt hyperthyroidism rates are 0.4 per 1000 women and 0.1 per 1000 men and vary with age.<ref name=":1" /> | |||
* Women between the ages of 20-40 are even more prone to developing this disease. <ref name="Goodman and Fuller">Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. St. Louis, Missouri: Saunders Elsevier; 2009.</ref>. | |||
== Etiology == | |||
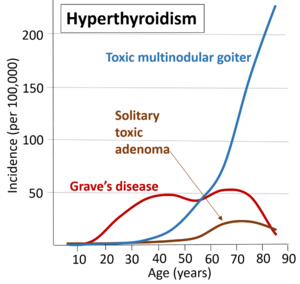
[[File:Causes of hyperthyroidism.png|thumb|Most common causes of hyperthyroidism by age in Denmark]] | |||
The most common cause of hyperthyroidism is [[Graves' Disease|Grave’s disease]], which accounts for approximately 85 percent of cases. It is an autoimmune disease in which an antibody that works against the thyroid stimulating hormone (TSH) receptor causes an increase in T4 production <ref name="aafp" /><ref name="Goodman and Fuller" />. Other causes of Hyperthyroidism include: | |||
*Toxic multinodular goiter: Accounts for approximately 5% of cases in the U.S. It is much more common in countries where iodine deficiency is more prevalent. This condition usually occurs in people over age 40 that have had a goiter for an extended period of time. | |||
*Toxic adenoma: This condition also occurs rarely in the U.S. It is common in the younger population in iodine-deficient countries. | |||
*Thyroiditis: Inflammation of the thyroid gland | |||
*Subacute thyroiditis often occurs following a viral illness. Symptoms usually resolve in eight months, and may occur repeatedly in some people. | |||
*Tumors <ref name="aafp" /> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
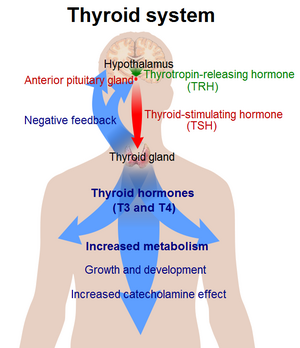
[[File:Thyroid system.png|thumb|Thyroid system]] | |||
People with hyperthyroidism may present with a variety of symptoms depending on the person’s age, the quantity of excess hormones, the period of time the person has been sick, and the presence of a comorbid condition <ref name="aafp">Reid J, Wheeler S. Hyperthyroidism: diagnosis and treatment. American Family Physician 2005 Aug 15; 72(4): 623. Available at http://www.aafp.org/afp/2005/0815/p623.html (accessed 24 Feb 2010).</ref>. Typical symptoms include: Accelerated heart rate or palpitations; Muscle weakness and trembling; Unexplained weight loss; Sensitivity to heat; Diarrhoea; Sleeping difficulties; Sweating; Irritability; Nervousness, agitation and anxiety<ref name=":0" /> | |||
* Older Persons: It is often difficult to detect the disease in older adults because they do not present with many of the typical signs and symptoms. Instead, they will often appear to have other illnesses, such as heart disease, depression, or dementia. Older people also tend to act more apathetic than hyperactive, and are more likely to have cardiovascular problems <ref name="Goodman and Fuller" />. | |||
* Under 70: In addition to tachycardia, fatigue and weight loss which are commonly seen in adults over 70, people younger than age 50 will also typically display hyperactive reflexes, increased perspiration, heat intolerance, tremor, nervousness, polydipsia, weakness, increased appetite, dyspnea, and weight loss despite normal food intake <ref>Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis, Missouri: Saunders Elsevier, 2007.</ref>. | |||
* Women may also notice a change in their menstrual cycles <ref name="mayo">Mayo Clinic. Symptoms. http://www.mayoclinic.com/health/graves-disease/DS00181/DSECTION=symptoms (accessed 24 Feb 2010).</ref>. Emotions can also become affected, causing a person’s moods to cycle between a euphoric state and acting hyperactive to feeling depressed and acting delusional <ref name="Goodman and Fuller" />. | |||
'''Graves' Disease | === Graves' Disease === | ||
[[File:Proptosis and lid retraction from Graves' Disease.jpeg|thumb|Proptosis and lid retraction - Graves' Disease]] | |||
In addition to the signs and symptoms previously mentioned, two key features of people with [[Graves' Disease|Graves’ disease]] are an enlarged thyroid gland (goiter) and exophthalmos which occurs in approximately 50% of people with the disease <ref name="aafp" />. See link | |||
=== Thyroid Storm === | |||
In a patient with untreated, incorrectly treated, or undiagnosed hyperthyroidism an acute episode of thyroid overactivity may occur. This event is known as [[Thyroid Storm (Thyroid Crisis)|thyroid storm]], a rare complication of hyperthyroidism that is characterized by a high fever, tachycardia, dehydration, delirium, and extreme irritability <ref name="Goodman and Fuller" />.<br> See link. | |||
In a patient with untreated, incorrectly treated, or undiagnosed hyperthyroidism | |||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
*Congestive heart failure | *[[Congestive Heart Failure|Congestive heart failure]] | ||
*Coronary artery disease | *[[Coronary Artery Disease (CAD)|Coronary artery disease]] | ||
*Sjogren’s syndrome | *[[Sjogren's Syndrome|Sjogren’s syndrome]] | ||
*Rheumatoid arthritis | *[[Rheumatoid Arthritis|Rheumatoid arthritis]] | ||
*Psoriatic arthritis | *[[Psoriatic Arthritis|Psoriatic arthritis]] | ||
*Chronic periarthritis | *Chronic periarthritis | ||
* | *[[Myasthenia Gravis|Myasthenia gravis]]<ref name="Goodman and Fuller" /> | ||
== Etiology == | |||
' | The most common cause of hyperthyroidism is [[Graves' Disease|Grave’s disease]], which accounts for approximately 85 percent of cases. It is an autoimmune disease in which an antibody that works against the thyroid stimulating hormone (TSH) receptor causes an increase in T4 production <ref name="aafp" /><ref name="Goodman and Fuller" />. Other causes of Hyperthyroidism include: | ||
* | *Toxic multinodular goiter: Accounts for approximately 5% of cases in the U.S. It is much more common in countries where iodine deficiency is more prevalent. This condition usually occurs in people over age 40 that have had a goiter for an extended period of time. | ||
* | *Toxic adenoma: This condition also occurs rarely in the U.S. It is common in the younger population in iodine-deficient countries. | ||
* | *Thyroiditis: Inflammation of the thyroid gland | ||
*Subacute thyroiditis often occurs following a viral illness. Symptoms usually resolve in eight months, and may occur repeatedly in some people. | |||
* | *Lymphocyctic and Postpartum are both types of thyroiditis that last for a short duration of time. Postpartum thyroiditis occurs in around 5-10% of women in the first 3-6 weeks after delivery. It is common for a person to experience hypothyroidism briefly before the condition resolves. | ||
*Treatment-induced: Iodine, Amiodarone, Thyroid hormone | |||
*Tumors <ref name="aafp" /> | |||
== | == Treatment == | ||
The treatment of HD has not changed substantially for many years and remains a choice between antithyroid drugs, radioiodine or surgery. However: | |||
* Antithyroid drug use can cause drug-induced embryopathy in pregnancy, | |||
* Surgery can result in hypoparathyroidism or laryngeal nerve damage. | |||
Future studies should focus on improved drug management, and a number of important advances are on the horizon. | |||
# Antithyroid drugs: These medications work to reduce the amount of hormone that the thyroid makes. This is one of the simplest approaches hyperthyroidism<span class="reference" id="cite_ref-:1_2-3"></span>. | |||
# Radioiodine therapy: involves taking radioactive iodine orally, either in capsule or liquid form. It targets the thyroid gland and destroys the cells that produce thyroid hormone. This means that most people who have radioiodine therapy go on to develop hypothyroidism. This is much easier to manage and does not cause as many long-term health issues as hyperthyroidism<ref>Physiopedia [[Graves' Disease|Graves]] Available: [[Graves' Disease|Graves Disease]] Accessed 24.2.2022)</ref>. | |||
== | == Physical Therapy Management == | ||
[[File:Older adult exercise with tin can..jpg|thumb|Exercise]] | |||
Hyperthyroidism has key elements that will cause a decreased tolerance to [[Physical Activity|physical activity]]. Therapists should be sensitive to patient complaints and symptoms to note an exacerbation if the patient is already diagnosed or be able to recognize symptoms in order to refer to a physician. | |||
What Should I Monitor During Treatment Session? | |||
* | *[[Vital Signs|Vital Signs:]] This is especially important if the patient is an older adult, has CAD or previous hx of heart disease, or presents with signs of dyspnea, fatigue, tachycardia, and/or arrhythmia. | ||
* | *Watch for signs of hypoparathyroidism such as muscular twitching, tetany, numbness, and tingling around mouth, fingertips, or toes if patient is post thyroidectomy. Hypoparathryoidism may result 1-7 days after thyroidectomy if there are complications during the surgery resulting in unintentional removal of part of the parathyroid glands.<ref name="Goodman and Fuller" /> | ||
Safety Precautions for Therapist | |||
*When working with patients who have been given RAI, be aware their saliva is radioactive for 24 hours following their treatment. When working with these patients it is important to take the necessary precautions if the patient is coughing or expectorating.<ref name="Goodman and Fuller" /> | |||
[[File:Hydrotherapy Pool Exercises.jpg|thumb|Monitor for heat stress]] | |||
Hyperthyroidism and Exercise | |||
*Some patients with Graves’ disease suffer from heat intolerance, making exercising in a hot pool a contraindication to therapy. This patient would still be able to participate in aquatic therapy in a warm pool; given the patient’s body temperature is being monitored. Typically heat intolerance is associated with thyroid storm, and will normally not occur in clients attending therapy in outpatient settings. | |||
*Hyperthyroidism is associated with exercise intolerance and reduced exercise capacity. | |||
*Many patients with hyperthyroidism suffer from cardiopulmonary complications often leading to [[Atrial Fibrillation|atrial fibriliation]], [[Heart Failure|CHF,]] and increased risk of a [[Myocardial Infarction|MI]]. | |||
*70% of people with hyperthyroidism develop proximal muscle weakness as a result of treatment, most often affecting the pelvis and thigh muscles | |||
*Graves’ disease is associated with a low bone mineral density (BMD) and has also been shown to be a risk factor for [[Femoral Neck Hip Fracture|hip fractures.]][http://www.physio-pedia.com/images/f/fa/Osteoarticular_disorders_of_endocrine_origin.pdf <ref name="Lioté F">Lioté F, Orcel P. Osteoarticular disorders of endocrine origin. Baillière's Best Practice & Research. Clinical Rheumatology [serial on the Internet]. (2000, June), [cited April 18, 2010]; 14(2): 251-276. Available from: MEDLINE.</ref>][[Hyperthyroidism#cite%20note-Liot%C3%A9%20F-8|<span class="mw-reflink-text">[8]</span>]][[Hyperthyroidism#cite%20note-Liot%C3%A9%20F-8|<span class="mw-reflink-text">[8]</span>]][[Hyperthyroidism#cite%20note-Liot%C3%A9%20F-8|<span class="mw-reflink-text">[8]</span>]][[Hyperthyroidism#cite%20note-Liot%C3%A9%20F-8|<span class="mw-reflink-text">[8]</span>]][[Hyperthyroidism#cite%20note-Liot%C3%A9%20F-8|<span class="mw-reflink-text">[8]</span>]][[Hyperthyroidism#cite%20note-Liot%C3%A9%20F-7|<span class="mw-reflink-text">[7]</span>]][[Hyperthyroidism#cite%20note-Liot%C3%A9%20F-8|<span class="mw-reflink-text">[8]</span>]][[Hyperthyroidism#cite%20note-Liot%C3%A9%20F-6|<span class="mw-reflink-text">[6]</span>]][[Hyperthyroidism#cite%20note-Liot%C3%A9%20F-7|<span class="mw-reflink-text">[7]</span>]][[Hyperthyroidism|<span class="mw-reflink-text">[10]</span>]] [http://www.physio-pedia.com/images/7/71/Subclinical_Hyperthyroidism_features_and_treatment.pdf <ref name="Aly">Aly N. Subclinical hyperthyroidism: features and treatment. Geriatric Medicine [serial on the Internet]. (2007, Nov), [cited April 18, 2010]; 37(11): 17. Available from: CINAHL with Full Text.</ref>][[Hyperthyroidism#cite%20note-Aly-9|<span class="mw-reflink-text">[9]</span>]][[Hyperthyroidism#cite%20note-Aly-9|<span class="mw-reflink-text">[9]</span>]][[Hyperthyroidism#cite%20note-Aly-9|<span class="mw-reflink-text">[9]</span>]][[Hyperthyroidism#cite%20note-Aly-9|<span class="mw-reflink-text">[9]</span>]][[Hyperthyroidism#cite%20note-Aly-9|<span class="mw-reflink-text">[9]</span>]][[Hyperthyroidism#cite%20note-Aly-8|<span class="mw-reflink-text">[8]</span>]][[Hyperthyroidism#cite%20note-Aly-9|<span class="mw-reflink-text">[9]</span>]][[Hyperthyroidism#cite%20note-Aly-7|<span class="mw-reflink-text">[7]</span>]][[Hyperthyroidism#cite%20note-Aly-8|<span class="mw-reflink-text">[8]</span>]][[Hyperthyroidism|<span class="mw-reflink-text">[11]</span>]] | |||
== Case Reports == | == Case Reports == | ||
# [http://www.physio-pedia.com/images/9/93/Myositis_Associated_with_the_Decline_of_Thyroid_Hormone_Levels_in_Thyrotoxicosis.pdf '''Myositis Associated with the Decline of Thyroid Hormone Levels in Thyrotoxicosis: A Syndrome?'''] <ref name="Duha">Duha S, Caroline S. K. Myositis Associated with the Decline of Thyroid Hormone Levels in Thyrotoxicosis: A Syndrome?. Thyroid [serial on the Internet]. (2009, Dec), [cited April 18, 2010]; 19(12): 1413-1417. Available from: Academic Search Premier.</ref> Case Report of a 24 y/o women with Graves’ disease who developed myalgias after a total thyroidectomy. The study concluded myositis after correction of thyrotoxicosis may constitute a syndrome that should be assessed for in<br>hyperthyroid patients complaining of myalgias after starting treatment. | |||
# '''[http://journals.lww.com/ajnonline/Abstract/2009/10000/Treatment_for_Graves__Disease_Poses_Risk_of_Liver.25.aspx Treatment for Graves' Disease Poses Risk of Liver Failure]<ref name="Aschenbrenner">Aschenbrenner D.. TREATMENT FOR GRAVES' DISEASE POSES RISK OF LIVER FAILURE. The American Journal of Nursing [serial online]. 2009;109:33. Available from: Research Library Core. Accessed March 28, 2010, Document ID: 1937632561.</ref>'''<br>The FDA has issued an alert regarding the risk of liver failure with the use of propylthiouracil, a popular antithyroid drug. The alert is based on 32 case reports of 22 adults and 10 children--12 of the adults died and five needed liver transplantation; one of the children died and six needed liver transplantation.Resources | |||
== References == | |||
== References | |||
<references /> | <references /> | ||
[[Category:Bellarmine_Student_Project]] | [[Category:Bellarmine_Student_Project]] | ||
[[Category:Conditions]] | |||
[[Category:Autoimmune Disorders]] | |||
Latest revision as of 12:04, 19 December 2022
Original Editors - Dana Johnston from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Dana Johnston, Lucinda hampton, Admin, Kim Jackson, WikiSysop, 127.0.0.1, Dave Pariser, Erin Shinkle, Wendy Walker and Elaine Lonnemann
Introduction[edit | edit source]
The term "hyperthyroidism" defines a syndrome associated with excess thyroid hormone production[1]. The thyroid gland controls important metabolic processes such as growth and energy expenditure. In hyperthyroidism the thyroid gland is overactive. An immune system abnormality called Graves' disease is the most common cause of hyperthyroidism. People treated for hyperthyroidism normally end up with an underactive thyroid ie hypothyroidism[2].
Epidemiology[edit | edit source]
The prevalence of hyperthyroidism differs according to the ethnic group, while in Europe, the frequency is affected by dietary intake of Iodine, and some cases are due to autoimmune disease.
- Subclinical hyperthyroidism occurs more in women older than 65 than in men
- Overt hyperthyroidism rates are 0.4 per 1000 women and 0.1 per 1000 men and vary with age.[1]
- Women between the ages of 20-40 are even more prone to developing this disease. [3].
Etiology[edit | edit source]
The most common cause of hyperthyroidism is Grave’s disease, which accounts for approximately 85 percent of cases. It is an autoimmune disease in which an antibody that works against the thyroid stimulating hormone (TSH) receptor causes an increase in T4 production [4][3]. Other causes of Hyperthyroidism include:
- Toxic multinodular goiter: Accounts for approximately 5% of cases in the U.S. It is much more common in countries where iodine deficiency is more prevalent. This condition usually occurs in people over age 40 that have had a goiter for an extended period of time.
- Toxic adenoma: This condition also occurs rarely in the U.S. It is common in the younger population in iodine-deficient countries.
- Thyroiditis: Inflammation of the thyroid gland
- Subacute thyroiditis often occurs following a viral illness. Symptoms usually resolve in eight months, and may occur repeatedly in some people.
- Tumors [4]
Characteristics/Clinical Presentation[edit | edit source]
People with hyperthyroidism may present with a variety of symptoms depending on the person’s age, the quantity of excess hormones, the period of time the person has been sick, and the presence of a comorbid condition [4]. Typical symptoms include: Accelerated heart rate or palpitations; Muscle weakness and trembling; Unexplained weight loss; Sensitivity to heat; Diarrhoea; Sleeping difficulties; Sweating; Irritability; Nervousness, agitation and anxiety[2]
- Older Persons: It is often difficult to detect the disease in older adults because they do not present with many of the typical signs and symptoms. Instead, they will often appear to have other illnesses, such as heart disease, depression, or dementia. Older people also tend to act more apathetic than hyperactive, and are more likely to have cardiovascular problems [3].
- Under 70: In addition to tachycardia, fatigue and weight loss which are commonly seen in adults over 70, people younger than age 50 will also typically display hyperactive reflexes, increased perspiration, heat intolerance, tremor, nervousness, polydipsia, weakness, increased appetite, dyspnea, and weight loss despite normal food intake [5].
- Women may also notice a change in their menstrual cycles [6]. Emotions can also become affected, causing a person’s moods to cycle between a euphoric state and acting hyperactive to feeling depressed and acting delusional [3].
Graves' Disease[edit | edit source]
In addition to the signs and symptoms previously mentioned, two key features of people with Graves’ disease are an enlarged thyroid gland (goiter) and exophthalmos which occurs in approximately 50% of people with the disease [4]. See link
Thyroid Storm[edit | edit source]
In a patient with untreated, incorrectly treated, or undiagnosed hyperthyroidism an acute episode of thyroid overactivity may occur. This event is known as thyroid storm, a rare complication of hyperthyroidism that is characterized by a high fever, tachycardia, dehydration, delirium, and extreme irritability [3].
See link.
Associated Co-morbidities[edit | edit source]
- Congestive heart failure
- Coronary artery disease
- Sjogren’s syndrome
- Rheumatoid arthritis
- Psoriatic arthritis
- Chronic periarthritis
- Myasthenia gravis[3]
Etiology[edit | edit source]
The most common cause of hyperthyroidism is Grave’s disease, which accounts for approximately 85 percent of cases. It is an autoimmune disease in which an antibody that works against the thyroid stimulating hormone (TSH) receptor causes an increase in T4 production [4][3]. Other causes of Hyperthyroidism include:
- Toxic multinodular goiter: Accounts for approximately 5% of cases in the U.S. It is much more common in countries where iodine deficiency is more prevalent. This condition usually occurs in people over age 40 that have had a goiter for an extended period of time.
- Toxic adenoma: This condition also occurs rarely in the U.S. It is common in the younger population in iodine-deficient countries.
- Thyroiditis: Inflammation of the thyroid gland
- Subacute thyroiditis often occurs following a viral illness. Symptoms usually resolve in eight months, and may occur repeatedly in some people.
- Lymphocyctic and Postpartum are both types of thyroiditis that last for a short duration of time. Postpartum thyroiditis occurs in around 5-10% of women in the first 3-6 weeks after delivery. It is common for a person to experience hypothyroidism briefly before the condition resolves.
- Treatment-induced: Iodine, Amiodarone, Thyroid hormone
- Tumors [4]
Treatment[edit | edit source]
The treatment of HD has not changed substantially for many years and remains a choice between antithyroid drugs, radioiodine or surgery. However:
- Antithyroid drug use can cause drug-induced embryopathy in pregnancy,
- Surgery can result in hypoparathyroidism or laryngeal nerve damage.
Future studies should focus on improved drug management, and a number of important advances are on the horizon.
- Antithyroid drugs: These medications work to reduce the amount of hormone that the thyroid makes. This is one of the simplest approaches hyperthyroidism.
- Radioiodine therapy: involves taking radioactive iodine orally, either in capsule or liquid form. It targets the thyroid gland and destroys the cells that produce thyroid hormone. This means that most people who have radioiodine therapy go on to develop hypothyroidism. This is much easier to manage and does not cause as many long-term health issues as hyperthyroidism[7].
Physical Therapy Management[edit | edit source]
Hyperthyroidism has key elements that will cause a decreased tolerance to physical activity. Therapists should be sensitive to patient complaints and symptoms to note an exacerbation if the patient is already diagnosed or be able to recognize symptoms in order to refer to a physician.
What Should I Monitor During Treatment Session?
- Vital Signs: This is especially important if the patient is an older adult, has CAD or previous hx of heart disease, or presents with signs of dyspnea, fatigue, tachycardia, and/or arrhythmia.
- Watch for signs of hypoparathyroidism such as muscular twitching, tetany, numbness, and tingling around mouth, fingertips, or toes if patient is post thyroidectomy. Hypoparathryoidism may result 1-7 days after thyroidectomy if there are complications during the surgery resulting in unintentional removal of part of the parathyroid glands.[3]
Safety Precautions for Therapist
- When working with patients who have been given RAI, be aware their saliva is radioactive for 24 hours following their treatment. When working with these patients it is important to take the necessary precautions if the patient is coughing or expectorating.[3]
Hyperthyroidism and Exercise
- Some patients with Graves’ disease suffer from heat intolerance, making exercising in a hot pool a contraindication to therapy. This patient would still be able to participate in aquatic therapy in a warm pool; given the patient’s body temperature is being monitored. Typically heat intolerance is associated with thyroid storm, and will normally not occur in clients attending therapy in outpatient settings.
- Hyperthyroidism is associated with exercise intolerance and reduced exercise capacity.
- Many patients with hyperthyroidism suffer from cardiopulmonary complications often leading to atrial fibriliation, CHF, and increased risk of a MI.
- 70% of people with hyperthyroidism develop proximal muscle weakness as a result of treatment, most often affecting the pelvis and thigh muscles
- Graves’ disease is associated with a low bone mineral density (BMD) and has also been shown to be a risk factor for hip fractures.[8][8][8][8][8][8][7][8][6][7][10] [9][9][9][9][9][9][8][9][7][8][11]
Case Reports[edit | edit source]
- Myositis Associated with the Decline of Thyroid Hormone Levels in Thyrotoxicosis: A Syndrome? [10] Case Report of a 24 y/o women with Graves’ disease who developed myalgias after a total thyroidectomy. The study concluded myositis after correction of thyrotoxicosis may constitute a syndrome that should be assessed for in
hyperthyroid patients complaining of myalgias after starting treatment. - Treatment for Graves' Disease Poses Risk of Liver Failure[11]
The FDA has issued an alert regarding the risk of liver failure with the use of propylthiouracil, a popular antithyroid drug. The alert is based on 32 case reports of 22 adults and 10 children--12 of the adults died and five needed liver transplantation; one of the children died and six needed liver transplantation.Resources
References[edit | edit source]
- ↑ 1.0 1.1 Mathew P, Rawla P, Fortes K. Hyperthyroidism (Nursing).Available: https://www.ncbi.nlm.nih.gov/books/NBK537053/ (accessed 24.2.2022)
- ↑ 2.0 2.1 Better health channel Available: Thyroid hyperactivityhttps://www.betterhealth.vic.gov.au/health/conditionsandtreatments/thyroid-hyperthyroidism(accessed 24.2.2022)
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. St. Louis, Missouri: Saunders Elsevier; 2009.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Reid J, Wheeler S. Hyperthyroidism: diagnosis and treatment. American Family Physician 2005 Aug 15; 72(4): 623. Available at http://www.aafp.org/afp/2005/0815/p623.html (accessed 24 Feb 2010).
- ↑ Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis, Missouri: Saunders Elsevier, 2007.
- ↑ Mayo Clinic. Symptoms. http://www.mayoclinic.com/health/graves-disease/DS00181/DSECTION=symptoms (accessed 24 Feb 2010).
- ↑ Physiopedia Graves Available: Graves Disease Accessed 24.2.2022)
- ↑ Lioté F, Orcel P. Osteoarticular disorders of endocrine origin. Baillière's Best Practice & Research. Clinical Rheumatology [serial on the Internet]. (2000, June), [cited April 18, 2010]; 14(2): 251-276. Available from: MEDLINE.
- ↑ Aly N. Subclinical hyperthyroidism: features and treatment. Geriatric Medicine [serial on the Internet]. (2007, Nov), [cited April 18, 2010]; 37(11): 17. Available from: CINAHL with Full Text.
- ↑ Duha S, Caroline S. K. Myositis Associated with the Decline of Thyroid Hormone Levels in Thyrotoxicosis: A Syndrome?. Thyroid [serial on the Internet]. (2009, Dec), [cited April 18, 2010]; 19(12): 1413-1417. Available from: Academic Search Premier.
- ↑ Aschenbrenner D.. TREATMENT FOR GRAVES' DISEASE POSES RISK OF LIVER FAILURE. The American Journal of Nursing [serial online]. 2009;109:33. Available from: Research Library Core. Accessed March 28, 2010, Document ID: 1937632561.