Osteopenia: Difference between revisions
Kim Jackson (talk | contribs) (Added One Page Owner and category) |
No edit summary |
||
| (7 intermediate revisions by 3 users not shown) | |||
| Line 2: | Line 2: | ||
'''Original Editors ''' - [[User:Hamelryck Sascha|Hamelryck Sascha]] | '''Original Editors ''' - [[User:Hamelryck Sascha|Hamelryck Sascha]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
Osteopenia is a condition characterised by the loss of bone mineral density (BMD) | Osteopenia is a condition characterised by the loss of [[Bone Density|bone mineral density (BMD]]), this loss of BMD is not as severe as it is in the case of [[osteoporosis]]. By definition from the World Health Organization osteopenia is defined by bone densitometry as a T score -1 to -2.5.<ref>WHO Scientific Group on the Prevention and Management of Osteoporosis (2000 : Geneva, Switzerland) (2003). "Prevention and management of osteoporosis : report of a WHO scientific group" (PDF). Retrieved 2007-05-31.</ref> <ref>Karaguzel G, Holick MF (2010): Diagnosis and treatment of osteopenia. Rev Endocr Metab Disord. 11(4):237-51. doi: 10.1007/s11154-010-9154-0.</ref> | ||
# Osteopenia will not cause any symptoms itself. | |||
# Osteopenia is a severe risk factor for developing osteoporosis. | |||
Watch this 90 second video to get a picture of osteopenia | |||
{{#ev:youtube|dtdEluROrbI|300}}<ref>FW BSI. Fort Worth Brain and Spine Institute - What is Osteopenia?. Available from: http://www.youtube.com/watch?v=dtdEluROrbI [last accessed 30/09/2022]</ref> | |||
== Epidemiology == | == Epidemiology == | ||
* Worldwide, Asia has reported the lowest average t-scores by region. | |||
* Overall, females have a four-fold higher overall prevalence of osteopenia compared to males. | |||
* Australia reported an incidence rate of osteopenia in 42% of men and 51% of women. | |||
* India reported a 52% overall incidence in its population in 2005. | |||
* In the United States, 54% of post[[Menopause|menopausal]] women are osteopenic.<ref name=":0">Varacallo M, Seaman TJ, Jandu JS, Pizzutillo P. Osteopenia. StatPearls.Available:https://www.ncbi.nlm.nih.gov/books/NBK499878/ (accessed 4.12.2022)</ref> | |||
== Etiology == | == Etiology == | ||
Bone mineral accretion from birth to adulthood follows a predictable course for the individual’s age and sex. Peak BMD is achieved typically by age 17 for females and 21 for males, after this point it starts to lower. Failure to achieve peak bone mass as a young adult results in early-onset conditions of decreased bone mass. It is estimated that heritable factors control up to 80% of our ability to gain and maintain optimal bone mineralization levels, modifiable factors credited to the rate of natural bone mass reduction into adulthood include weight-bearing exercises, adequate calcium and vitamin D daily intake, [[Body Composition|body mass]], and [[Hormones|hormonal]] influence.<ref name=":0" /> | |||
== Histopathology == | |||
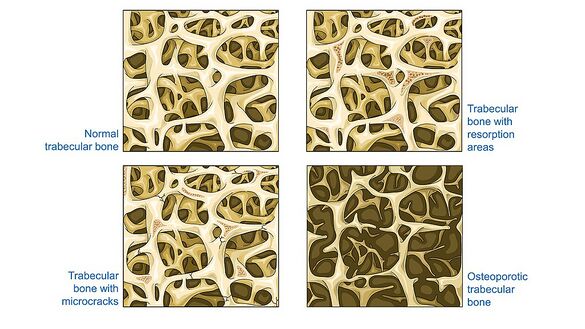
Histologic specimens demonstrate noticeably thinned trabeculae, decreased osteon size, and enlarged haversian and marrow spaces.<ref name=":0" /> | |||
[[File:Cancellous bone - Trabecular bone - Normal trabecular bone Trabecular bone etc -- Smart-Servier (cropped).jpeg|center|frameless|585x585px|Cancellous bone - Trabecular bone - Normal trabecular bone Trabecular bone]] | |||
== | == Diagnosis == | ||
[[File:DEXA scanner in use ALSPAC.jpeg|thumb|239x239px|DEXA scanner]] | |||
Diagnostic procedure usually consists of a [[Dual Energy X-ray Absorptiometry (DEXA Scan)|DEXA]] (dual emission x-ray absorptiometry) scan of the lumbar spine and hip. See link<br>The WHO defines t-scores | |||
= | # t-score between +1 and -1 indicates normal bone density. | ||
# t-score between -1 and -2.5 indicates low bone density or osteopenia. | |||
# t-score of -2.5 or lower is proof of osteoporosis<ref name=":0" />. | |||
== Treatment/Management == | |||
[[File:Dairy-Products.jpg|thumb|Calcium rich foods]] | |||
The main treatment recourse for osteopenic patients involve early education on how to achieve and maintain healthy bone mass levels and extensive education on the relevant social, environmental, and lifestyle risk factors that effect bone health. Medical treatment is generally not given to people with early-stage osteopenia. | |||
All clinicians should educate patients about the morbidity of osteopenia. In particular encourage the patient to | |||
* Eat a healthy diet rich in calcium | |||
* Exercise, cease smoking, and keep alcohol to a minimum.<ref name=":0" /> | |||
== Physiotherapy management == | == Physiotherapy management == | ||
The purpose of the therapy is the same in every case: trying to enhance BMD and slowing/preventing loss of BMD. | The purpose of the therapy is the same in every case: trying to enhance BMD and slowing/preventing loss of BMD. For physiotherapy management see relevant section of [[Osteoporosis]]<ref>Ramos LA, Rodrigues FT, Shirahige L, Barros MD, de Carvalho AG, Guerino MR, de Lima Ferreira AP, Guerra RO, de Araújo MD. [https://www.ncbi.nlm.nih.gov/pubmed/31275877 A single whole body vibration session influences quadriceps muscle strength, functional mobility and balance of elderly with osteopenia and/or osteoporosis? Pragmatic clinical trial.] Journal of Diabetes & Metabolic Disorders. 2019 Jun 1;18(1):73-80.</ref>. | ||
== References == | == References == | ||
| Line 56: | Line 57: | ||
[[Category:Older People/Geriatrics]] | [[Category:Older People/Geriatrics]] | ||
[[Category:Older People/Geriatrics - Conditions]] | [[Category:Older People/Geriatrics - Conditions]] | ||
Latest revision as of 14:58, 16 December 2022
Original Editors - Hamelryck Sascha Top Contributors - Hamelryck Sascha, Kim Jackson, Lucinda hampton, Rotimi Alao, Admin, Vidya Acharya, Claire Knott, Leana Louw, Rishika Babburu, Oyemi Sillo and WikiSysop
Introduction[edit | edit source]
Osteopenia is a condition characterised by the loss of bone mineral density (BMD), this loss of BMD is not as severe as it is in the case of osteoporosis. By definition from the World Health Organization osteopenia is defined by bone densitometry as a T score -1 to -2.5.[1] [2]
- Osteopenia will not cause any symptoms itself.
- Osteopenia is a severe risk factor for developing osteoporosis.
Watch this 90 second video to get a picture of osteopenia
Epidemiology[edit | edit source]
- Worldwide, Asia has reported the lowest average t-scores by region.
- Overall, females have a four-fold higher overall prevalence of osteopenia compared to males.
- Australia reported an incidence rate of osteopenia in 42% of men and 51% of women.
- India reported a 52% overall incidence in its population in 2005.
- In the United States, 54% of postmenopausal women are osteopenic.[4]
Etiology[edit | edit source]
Bone mineral accretion from birth to adulthood follows a predictable course for the individual’s age and sex. Peak BMD is achieved typically by age 17 for females and 21 for males, after this point it starts to lower. Failure to achieve peak bone mass as a young adult results in early-onset conditions of decreased bone mass. It is estimated that heritable factors control up to 80% of our ability to gain and maintain optimal bone mineralization levels, modifiable factors credited to the rate of natural bone mass reduction into adulthood include weight-bearing exercises, adequate calcium and vitamin D daily intake, body mass, and hormonal influence.[4]
Histopathology[edit | edit source]
Histologic specimens demonstrate noticeably thinned trabeculae, decreased osteon size, and enlarged haversian and marrow spaces.[4]
Diagnosis[edit | edit source]
Diagnostic procedure usually consists of a DEXA (dual emission x-ray absorptiometry) scan of the lumbar spine and hip. See link
The WHO defines t-scores
- t-score between +1 and -1 indicates normal bone density.
- t-score between -1 and -2.5 indicates low bone density or osteopenia.
- t-score of -2.5 or lower is proof of osteoporosis[4].
Treatment/Management[edit | edit source]
The main treatment recourse for osteopenic patients involve early education on how to achieve and maintain healthy bone mass levels and extensive education on the relevant social, environmental, and lifestyle risk factors that effect bone health. Medical treatment is generally not given to people with early-stage osteopenia.
All clinicians should educate patients about the morbidity of osteopenia. In particular encourage the patient to
- Eat a healthy diet rich in calcium
- Exercise, cease smoking, and keep alcohol to a minimum.[4]
Physiotherapy management[edit | edit source]
The purpose of the therapy is the same in every case: trying to enhance BMD and slowing/preventing loss of BMD. For physiotherapy management see relevant section of Osteoporosis[5].
References[edit | edit source]
- ↑ WHO Scientific Group on the Prevention and Management of Osteoporosis (2000 : Geneva, Switzerland) (2003). "Prevention and management of osteoporosis : report of a WHO scientific group" (PDF). Retrieved 2007-05-31.
- ↑ Karaguzel G, Holick MF (2010): Diagnosis and treatment of osteopenia. Rev Endocr Metab Disord. 11(4):237-51. doi: 10.1007/s11154-010-9154-0.
- ↑ FW BSI. Fort Worth Brain and Spine Institute - What is Osteopenia?. Available from: http://www.youtube.com/watch?v=dtdEluROrbI [last accessed 30/09/2022]
- ↑ 4.0 4.1 4.2 4.3 4.4 Varacallo M, Seaman TJ, Jandu JS, Pizzutillo P. Osteopenia. StatPearls.Available:https://www.ncbi.nlm.nih.gov/books/NBK499878/ (accessed 4.12.2022)
- ↑ Ramos LA, Rodrigues FT, Shirahige L, Barros MD, de Carvalho AG, Guerino MR, de Lima Ferreira AP, Guerra RO, de Araújo MD. A single whole body vibration session influences quadriceps muscle strength, functional mobility and balance of elderly with osteopenia and/or osteoporosis? Pragmatic clinical trial. Journal of Diabetes & Metabolic Disorders. 2019 Jun 1;18(1):73-80.