Pregnancy Related Pelvic Pain
Original Editors - Marlies Verbruggen
Top Contributors - Marlies Verbruggen, Nicole Hills, Rotimi Alao, Andeela Hafeez, Lara Lagrange, Vanwymeersch Celine, Kim Jackson, Admin, Laura Ritchie, Simisola Ajeyalemi, Rachael Lowe, WikiSysop, Wanda van Niekerk, Evan Thomas and Fasuba Ayobami
[See also Chronic Pelvic Pain]
Introduction[edit | edit source]
According to the European guidelines created by Vleeming and colleagues,[1] “Pelvic girdle pain (PGP) generally arises in relation to pregnancy, trauma, arthritis and osteoarthritis. Pain is experienced between the posterior iliac crest and the gluteal fold, particularly in the vicinity of the sacroiliac joints (SIJ). The pain may radiate in the posterior thigh and can also occur in conjunction with/or separately in the symphysis. The endurance capacity for standing, walking, and sitting is diminished. The diagnosis of PGP can be reached after exclusion of lumbar causes. The pain or functional disturbances in relation to PGP must be reproducible by specific clinical tests”[1]
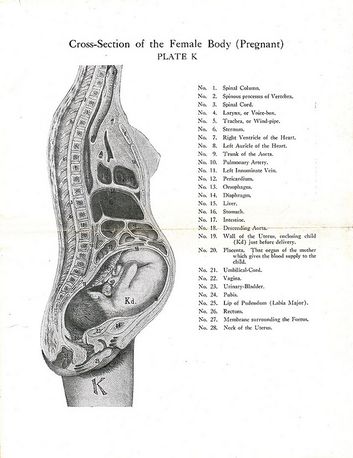
Clinically Relevant Anatomy[edit | edit source]
The pelvis is composed of the sacrum, ilium, ischium and pubis. The pelvic bone consists the pubic symphysis and the sacroiliac joint.
Sacroiliac Joints
The sacroiliac joints allow for the transfer of forces between the spine and the lower extremity.[2] To read more about the function of the sacroiliac joints review: Force and Form Closure
Pelvic Floor
The pelvic floor muscles have two primary functions in females. The muscles:[3]
- support the abdominal viscera (bladder, intestines, uterus) and the rectum
- control the mechanism for continence for the urethral, anal and vaginal orifices[3]
Etiology[edit | edit source]
The etiology of pregnancy-related pelvic girdle pain has not been clearly established in the literature.[4] However, the cause of this pain is believed to be multi-factorial and may be related to hormonal, biomechanical, traumatic, metabolic, genetic and degenerative factors.[5] [6] [7]
Hormonal[edit | edit source]
Women produce increased quantities of the hormone relaxin during their pregnancy. Relaxin increases ligament laxity in the pelvic girdle (and in other parts of the body) in preparation for the labour process. Increased ligament laxity may cause a small increase in the range of motion at the pelvis. If this increase in motion is not complimented by a change in neuromotor control (e.g., muscles around the pelvis act to improve stability), it is possible that pain may occur.[1] However, the link between relaxin and pelvic girdle pain during pregnancy has not been established in the literature.[6][7] Research to date also does not support the idea that an increase in the range of motion at the pelvis causes pain.[1][8] [9]
Biomechanical[edit | edit source]
As pregnancy progresses, the gravid uterus increases load on the spine and pelvis. To accommodate for the growth of the uterus the pubic symphysis must soften and laxity in the pelvic ligaments increases. The uterus shifts forward which changes the maternal centre of gravity and the orientation of pelvis.[10] This change in centre of gravity may cause stress or a change in load on the lower back and pelvic girdle.[6][11][7] This change in load can result in compensatory postural changes (e.g., an increase in lumbar lordosis).[6][11][7]
Risk Factors[edit | edit source]
The risk factors for developing pregnancy-related pelvic girdle pain are:
- a previous history of low back pain or pelvic girdle pain.[12][7]
- a previous trauma to the pelvis or back.[12][7]
- physical demanding work (e.g., twisting and bending the back several times per hour per day).[1][13][14][15][16]
- multiparity - may play a causal role in the development of pregnancy-related pelvic girdle pain[17]
Epidemiology[edit | edit source]
Pelvic girdle pain may begin around the 18th week of pregnancy and appears to peak between the 24th and 36th week.[18] Pelvic pain affects approximately 50% of women during pregnancy.[13] 25% of the women who experience pelvic girdle pain report having severe pain and 8% report pain that causes severe disability.[19]
Clinical Presentation[edit | edit source]
The clinical presentation of pregnancy-related pelvic girdle pain can vary from patient to patient and can change over the course of the patient's pregnancy.[13] Since the cause of pregnancy related pelvic girdle pain is multifactorial it is important to incorporate a biopsychosocial approach to the diagnosis and treatment of this pain.
Subjective History[edit | edit source]
Common symptoms related to pregnancy-related pelvic pain include:
- a difficulty walking quickly and covering long distances[1][20][13]
- pain/discomfort/difficulty during sexual intercourse[20][13]
- pain/discomfort during sleep and/or a difficulty turning over in bed[13][21]
- decreased ability to perform housework[13][21]
- decreased ability to engage in activities with children[13]
- difficulty sitting[21]
- difficulty standing for 30 minutes or longer[21]
- pain in single leg stance i.e., climbing stairs[21]
- inability or difficulty running (postnatal) due to pain[21]
- decreased ability for mother-child interactions[14]
- pain/discomfort with weight bearing activities[11]
Pain[edit | edit source]
The onset of pain may occur around the 18th week of pregnancy and reaches peak intensity between the 24th and 36th week of pregnancy. The pain typically resolves by the third month in the postpartum period.[22][7]
Location[edit | edit source]
Pelvic girdle pain typically presents near the sacroiliac joints and/or gluteal area or anteriorly near the symphysis pubis[13]. The reported pain may radiate into the patient's groin, perineum or posterior thigh but does not mimic a typically sciatic nerve root distribution.[23][24] The location of the pain may vary throughout the course of the pregnancy.[25] A pain distribution diagram can be a useful tool in diagnosing the patient's pain and to help distinguish pregnancy-related pelvic girdle pain from pregnancy related low back pain.[26]
Nature and intensity of pain[edit | edit source]
Pelvic girdle pain may be described as a stabbing[27][28], dull, shooting or burning sensation.[28] The intensity of pain on a 100 mm visual analogue scale averages around 50-60 mm.[25][24]
Muscle Function and Perception[edit | edit source]
- postpartum women may present with reduced hip abduction and adduction force[29] which may be related to fear of pain/movement.[29]
- women may reported a feeling of "catching" in their upper leg during ambulation[28] and/or report feeling the lack the ability to move their legs during the active straight leg test[30] which may suggest nervous system involvement.[13]
- altered gait coordination- women with postpartum pelvic girdle pain can present with a coupling between pelvic and thoracic rotations during gait (pelvic and thoracic rotations in the same direction occur at the same time) which has been proposed as a nervous system strategy used to cope with motor problems.[31]
Pelvic Girdle Pain Examination[edit | edit source]
Before a diagnosis of pelvic girdle pain is reached potential lumbar spine pain and/or dysfunction should be ruled out.[1] Once the lumbar spine is ruled out the sacroiliac joint, the symphysis pubis, and the pelvis should be assessed.
Sacroiliac joint[edit | edit source]
- Posterior pelvic pain provocation test (P4)[1][20][32] [33] This is a pain provocation test used to determine the presence of sacroiliac dysfunction. It is used to distinguish between pregnancy-related pelvic pain (PRPP) and low back pain
- Patrick ‘s Faber test [1][20]
- Palpation of the long dorsal SIJ ligament [1][20][32][33]
- Gaenslen’s test [1][20]
- For more information on the tests listed above see SIJ Special Test Cluster
Symphysis Pubis[edit | edit source]
- Palpation of symphysis[1][20][32]
- Modified trendelenburg’s test of the pelvic girdle [1][20][32]
Functional Pelvic Test[edit | edit source]
- Active straight leg raise test (ASLR test) [1][20][32][33]
Diagnostic Procedures[edit | edit source]
During pregnancy diagnostic imaging using radiation is contraindicated.[26] Ultrasound imaging and/or MRIs may be used for certain interventions and/or surgical planning or to rule out the presence of serious medical conditions.[34]
Outcome Measures[edit | edit source]
The Pelvic Girdle Questionnaire (PGQ)[35] was developed to evaluate impairments and/or the functional limitations caused my pelvic girdle pain during pregnancy and in the postpartum period.[35] The PGQ has been found to significantly discriminated participants who were pregnant from participants who were not pregnant.[36]
Clinton and colleagues[26] recommend using the Pain Catastrophizing Scale (PCS) and the Fear-Avoidance Beliefs Questionnaire (FABQ), using these scales in your clinical practice can help to provide a broader picture of your patient's ability to mental processing of the pain and how their pain is affecting their daily activities. Currently only the Fear-Avoidance Beliefs Questionnaire-Physical Activity sub-scale has been validated for use during pregnancy.[36]
Differential Diagnosis[edit | edit source]
Patient-reported pelvic girdle pain can be associated with signs and symptoms of inflammatory, infectious, traumatic, neoplastic, degenerative, or metabolic disorders.[26] Therefore, it is important to take a detailed subjective history and refer to the appropriate medical professional as indicated. Pelvic girdle pain can be a symptom of uterine abruption or referred pain due to urinary tract infection to the lower abdomen/pelvic or sacral region.[37] A referral to a medical professional is warranted if the patient reports any of the following:[26]
- a history of trauma
- unexplained weight loss
- a history of cancer
- steroid use or drug abuse
- human immunodeficiency virus or immunosuppressed state
- neurological symptoms/signs,
- a fever, and/or feeling systemically unwell
- severe pain that does not improve with rest [26]
[edit | edit source]
When assessing a patient who presents with pregnancy related pelvic girdle pain the presence of pelvic floor muscle, hip, and lumbar spine dysfunction should be ruled out.[26]
Hip dysfunction
- possible femoral neck stress fracture due to transient osteoporosis[38] [39][40]
- bursitis/tendonitis, chondral damage/loose bodies, capsular laxity, femoral acetabular impingement, labral irritations/tears, muscle strains
- referred pain from L2,3 radiculopathy[41]
- osteonecrosis of the femoral head[41]
- Paget’s disease[41]
- rheumatoid, and psoriatic and septic arthritis[41]
Lumbar spine dysfunctions and pregnancy-related low back pain[26]
- spondylolisthesis
- discal patterns of symptoms that fail to centralize, and
Bowel/bladder dysfunction[26]
- cauda equina syndrome
- large lumbar disc, or
- other space-occupying lesions around the spinal cord or nerve roots
Physical Therapy Management[edit | edit source]
Physical therapy for pelvic girdle pain during pregnancy[edit | edit source]
According to the European guidelines by Vleeming and colleagues[1] exercises are recommended during pregnancy. These exercises should focus on adequate advice concerning activities of daily living and avoid maladaptive movement patterns.[1] It is important to follow an individualized program, focusing specifically on stabilizing exercises for a greater control.
Physical therapy for pelvic girdle pain after pregnancy[edit | edit source]
After pregnancy, it is also important to focus on specific stabilizing exercises. It has been proven that this type of exercises have a positive effect on pain, functional status and health-related quality of life.[1][15]
The treatment program actually includes several important factors like [32] :
- Advice and education: Informing the patient about body awareness. The purpose of information is mainly to reduce fear and to encourage patients to take an active part in their treatment and/or rehabilitation. General information on PGP needs to be presented (anatomy, biomechanics, motor control) and the patients need to be reassured that their problems are not dangerous to them or their child and that they will probably improve/recover. Ergonomic advice in real life situations can also be helpful, these situations can be really specific like carrying or lifting a child. The patient needs to be encouraged to enjoy physical activity and manage and combine this with periods of rest in order to recuperate.[1]
- Joint mobilization, massage, relaxation and stretching can be executed when indicated. Manipulation or joint mobilization may be used to test for symptomatic relief, but should only be applied for a few treatments. Adjusting asymmetrical motion of the SIJs prior to exercising with joint mobilization may influence optimal form closure and enhance the possibility to exercise without pain. Massage might be helpful, but it must be given as part of a multifactorial individualized treatment program.[17] Manual therapy could be applied even though the evidence is conflicting.[42][43]
- Exercises to retrain motor control and strength of abdominal, spinal, pelvic girdle, hip and pelvic floor muscles.[42] Giving the patients specific stabilizing exercises can reduce pain intensity, lower disability and higher quality of life.[44]
- Pain control: Exercise in water can help.[42] Conflicting evidence shows that acupuncture could relieve pain.[45] Massage and osteo manipulative therapy can also help to reduce pain during pregnancy but further research is required.[46][47] Craniosacral therapy has small pain-relieving effects. If it’s used in combination with standard treatment it diminishes morning pain and gives less deteriorated function. But it’s not recommended for pregnant women since the effect are clinically very small.[48] TENS is a safe way to help patients with pain relief.[49]
The program, for exercise and training, consists of:[15]
- Specific training of the abdominal muscles, which are transversely oriented. This must be performed with co-activation of the lumbar multifidus at the lumbosacral region.
- The following muscles will be trained: Gluteus maximus, latissimus dorsi, blique abdominal muscles, erector spinae, quadratus lumborum and the hip adductors and abductors.
In the initial stage, the treatment program focuses on the training of specific contractions of the deep muscle system, independently from the superficial muscle. The deep muscle system consists of transversus abdominis, obliquus internus, multifidus, pelvic floor and the diaphragm. During all exercises and daily activities they emphasize the importance of activating these muscles before adding the superficial muscles. Depending on clinical findings this focus was combined with information, ergonomic advice, body awareness training, relaxation of global muscles and mobilization.[15][44] Exercises for the superficial muscles were gradually added to the program, when low force contractions of the transversely oriented abdominal muscles were achieved.[44]
The Therapy Master, which is an exercise device, can be utilized to facilitate the exercise progression for most of the exercises.[15][44] In literature, the patients performed these exercises 30 to 60 minutes, 3 days a week, and this for 18 to 20 weeks. They also started with three series of ten repetitions of each exercise.[15] The quality of the execution of the exercise determined the number of exercises and number of repetitions. Each patient received specific stabilizing exercises out of a fixed menu (see photo). The patients may have muscle soreness, but the exercises may not provoke pain at any time. It’s also very important that the patient maintains lumbopelvic control during the performance of these exercises.[15][44] The exercises for enhancing the lumbopelvic control and stability should involve the entire spinal musculature. Focusing on only global muscles seems insufficient.[17]
Patients often have a flare-up of pain when exercising, but this is likely from progressing the exercise load too quickly. This study used an exercise diary so the patient could describe her progression, and seemed to be effective in avoiding flare-ups.[15] It is well documented that exercise supervision is critical for improving quality of exercise performance.[15][44]
Prognosis[edit | edit source]
Pregnancy-related pelvic girdle pain appears to be a self-limiting condition that typically resolves by 3 months postpartum in a majority of women.[7] However, due to the complexity of the condition it has been recommended that a biopsychosocial approach aimed at improving the individual's self-knowledge and self-efficacy be used in the management of pelvic girdle pain to help minimize disability.[50]
Clinical Bottom Line[edit | edit source]
We can conclude that pregnancy related pelvic girdle pain often is caused by instability of the pelvis or sacroiliac joint. Biomechanical (the wedge shape of the sacrum, the additional compression forces which are generated by the muscles, fascia and ligaments) and hormonal (relaxin, progesterone) factors have an impact on the dynamic stability. These factors can cause an increased motion of the pelvic joints which leads to a stabbing pain deep in the sacral/gluteal region. Patients who suffer from pelvic girdle pain, have difficulty during walking, running, climbing stairs, sexual intercourse and also during sitting and sleeping.
To make the diagnosis of pelvic girdle pain the following tests are recommended for the clinical examination: posterior pelvic pain provocation test , Patrick ‘s Faber test, palpation of the long dorsal SIJ ligament , Gaenslen’s test, palpation of symphysis, modified Trendelenburg’s of the pelvic girdle and the active straight leg raise test (ASLR test). It’s also very important to ask the patient about his pain history.
During and after pregnancy it is important to follow an individualized program, in which stabilization exercises are very important. During this program it is important to focus on adequate advice concerning activities of daily living and to avoid maladaptive movement patterns. The following muscles need to be trained during the exercise program: the abdominal muscles, M. gluteus maximus, M. latissimus dorsi, M. oblique abdominal muscles, M. erector spinae, M. quadrates lumborum end the hip adductors and abductors.
Resources[edit | edit source]
Vleeming A, Albert HB, Östgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. European Spine Journal. 2008 Jun 1;17(6):794-819.
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 Vleeming A, Albert HB, Östgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. European Spine Journal Jun 2008; 17(6) : 794-819.
- ↑ Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. Journal of anatomy. 2012 Dec 1;221(6):537-67.
- ↑ 3.0 3.1 Raizada V, Mittal RK. Pelvic floor anatomy and applied physiology. Gastroenterology Clinics of North America. 2008 Sep 1;37(3):493-509.
- ↑ Aldabe D, Milosavljevic S, Bussey MD. Is pregnancy related pelvic girdle pain associated with altered kinematic, kinetic and motor control of the pelvis? A systematic review. European Spine Journal. 2012 Sep 1;21(9):1777-87.
- ↑ Homer C, Oats J. Clinical practice guidelines: Pregnancy care. Canberra: Australian Government Department of Health, 2018; p. 355–57
- ↑ 6.0 6.1 6.2 6.3 Bhardwaj A, Nagandla K. Musculoskeletal symptoms and orthopaedic complications in pregnancy: Pathophysiology, diagnostic approaches and modern management. Postgrad Med J
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 Kanakaris NK, Roberts CS, Giannoudis PV. Pregnancy-related pelvic girdle pain: An update. BMC Med 2011;9:15. doi: 10.1186/1741-7015-9-15.
- ↑ Damen L, Buyruk HM, Güler-Uysal F, Lotgering FK, Snijders CJ, Stam HJ. Pelvic pain during pregnancy is associated with asymmetric laxity of the sacroiliac joints. Acta obstetricia et gynecologica Scandinavica. 2001 Jan 1;80(11):1019-24.
- ↑ Sturesson B, Selvik G, UdÉn A. Movements of the sacroiliac joints. A roentgen stereophotogrammetric analysis. Spine. 1989 Feb;14(2):162-5.
- ↑ Ritchie JR. Orthopedic considerations during pregnancy. Clinical obstetrics and gynecology. 2003 Jun 1;46(2):456-66.
- ↑ 11.0 11.1 11.2 Robinson H.S., Clinical course of pelvic girdle pain postpartum - impact of clinic findings in late pregnancy, Manual therapy 19 (2014) 190-196
- ↑ 12.0 12.1 Pierce H, Homer CS, Dahlen HG, King J. Pregnancy-related lumbopelvic pain: listening to Australian women. Nursing research and practice. 2012;2012.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 13.7 13.8 13.9 Wu WH, Meijer OG, Uegaki K, Mens JMA, Van Dieën JH, Wuisman PIJM, Östgaard HC. Pregnancy-related pelvic girdle pain (PPP), I : Terminology, clinical presentation, and prevalence. European Spine Journal Nov 2004; 13(7) : 575-589.
- ↑ 14.0 14.1 Elden H., Predictors and consequences of long-term pregnancy-related pelvic girdle pain: a longitudinal follow-up study,BMC Musculoskelet Disord. 2016; 17: 276.doi: 10.1186/s12891-016-1154-0
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 15.7 15.8 Danielle Casagrande et al., Low Back Pain and Pelvic Girdle Pain in Pregnancy, J Am Acad Orthop Surg 2015;00:1-11
- ↑ Ostgaard HC, Andersson GB. Postpartum low-back pain. Spine. 1992 Jan;17(1):53-5.
- ↑ 17.0 17.1 17.2 Bjelland EK. et al., Hormonal contraception and pelvic girdle pain during pregnancy: a population study of 91.721 pregnancies in the norwegian mother and child cohort, Human reproduction. vol 0, No.0 pp1-7, 2013
- ↑ Bergstrom et al., Pregnancy-related low back pain and pelvic girdle pain approximately 14 months after pregnancy – pain status, self-rated health and family situation, BMC Pregnancy and Childbirth 201414:48, DOI: 10.1186/1471-2393-14-48
- ↑ Albert H, Godskesen M, Westergaard J. Prognosis in four syndromes of pregnancy‐related pelvic pain. Acta obstetricia et gynecologica Scandinavica. 2001 Jun 1;80(6):505-10.
- ↑ 20.0 20.1 20.2 20.3 20.4 20.5 20.6 20.7 20.8 Kanakaris NK, Roberts CS, Giannoudis PV. Pregnancy-related pelvic girdle pain: un update. BMC Medicine Feb 2011; 9: 1-15.
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 Nielsen LL. Clinical findings, pain descriptions and physical complaints reported by women with post-natal pregnancy-related pelvic girdle pain. Acta Obstetricia et Gynecologica 2010: 89; 1187-1191.
- ↑ Oätgaard HC, Andersson GB, Wennergren M. The impact of low back and pelvic pain in pregnancy on the pregnancy outcome. Acta obstetricia et gynecologica Scandinavica. 1991 Jan;70(1):21-4.
- ↑ Fast A, Shapiro D, Ducommun EJ, Friedmann LW, Bouklas T, Floman Y. Low-back pain in pregnancy. Spine. 1987 May;12(4):368-71.
- ↑ 24.0 24.1 Ostgaard HC, Zetherström G, Roos-Hansson E, Svanberg B. Reduction of back and posterior pelvic pain in pregnancy. Spine. 1994 Apr;19(8):894-900.
- ↑ 25.0 25.1 Kristiansson P, Svärdsudd K, von Schoultz B. Back pain during pregnancy: a prospective study. Spine. 1996 Mar 15;21(6):702-8.
- ↑ 26.0 26.1 26.2 26.3 26.4 26.5 26.6 26.7 26.8 Clinton SC, Newell A, Downey PA, Ferreira K. Pelvic Girdle Pain in the Antepartum Population: Physical Therapy Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability, and Health From the Section on Women's Health and the Orthopaedic Section of the American Physical Therapy Association. Journal of Women's Health Physical Therapy. 2017 May 1;41(2):102-25.
- ↑ Östgaard HC, Roos-Hansson E, Zetherström G. Regression of back and posterior pelvic pain after pregnancy. Spine. 1996 Dec 1;21(23):2777-80.
- ↑ 28.0 28.1 28.2 Sturesson et al; Pain pattern in pregnancy and" catching" of the leg in pregnant women with posterior pelvic pain; Spine; 1997; PP 1880-1883
- ↑ 29.0 29.1 Mens JM, Vleeming A, Snijders CJ, Ronchetti I, Stam HJ. Reliability and validity of hip adduction strength to measure disease severity in posterior pelvic pain since pregnancy. Spine. 2002 Aug 1;27(15):1674-9.
- ↑ Mens JM, Vleeming A, Snijders CJ, Koes BW, Stam HJ. Reliability and validity of the active straight leg raise test in posterior pelvic pain since pregnancy. Spine. 2001 May 15;26(10):1167-71.
- ↑ Wu W, Meijer OG, Jutte PC, Uegaki K, Lamoth CJ, de Wolf GS, van Dieën JH, Wuisman PI, Kwakkel G, de Vries JI, Beek PJ. Gait in patients with pregnancy-related pain in the pelvis: an emphasis on the coordination of transverse pelvic and thoracic rotations. Clinical biomechanics. 2002 Nov 1;17(9-10):678-86.
- ↑ 32.0 32.1 32.2 32.3 32.4 32.5 Stuge B, Laerum E, Kirkesola G, Vollestad N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: A randomized controlled trial. Spine Feb 2004 : 29(4) ; 351-359.
- ↑ 33.0 33.1 33.2 Vollestad NK, Stuge B. Prognostic factors for recovery from postpartum pelvic girdle pain. European Spine Journal Feb 2009: 18; 718-726.
- ↑ American College of Obstetricians and Gynecologists, Committee on Obstetric Practice. Guidelines for diagnostic imaging during pregnancy. Obstet Gynecol. 2004;104:647-51.
- ↑ 35.0 35.1 Stuge. B., The pelvic girdle questionnaire: a condition-specific instrument for assessing activity limitations and symptoms in people with pelvic girdle pain. phys ther 2011; 91:1096-1108
- ↑ 36.0 36.1 Grotle M, Garratt AM, Krogstad Jenssen H, Stuge B. Reliability and construct validity of self-report questionnaires for patients with pelvic girdle pain. Physical therapy. 2012 Jan 1;92(1):111-23.
- ↑ Boissonnault JS, Klestinski JU, Pearcy K. The role of exercise in the management of pelvic girdle and low back pain in pregnancy: A systematic review of the literature. Journal of Women’s Health Physical Therapy. 2012 May 1;36(2):69-77.
- ↑ Boissonnault WG, Boissonnault JS. Transient osteoporosis of the hip associated with pregnancy. Journal of Women’s Health Physical Therapy. 2005 Dec 1;29(3):33-9.
- ↑ Møller UK, við Streym S, Mosekilde L, Rejnmark L. Changes in bone mineral density and body composition during pregnancy and postpartum. A controlled cohort study. Osteoporosis International. 2012 Apr 1;23(4):1213-23.
- ↑ Oliveri B , Parisi MS , Zeni S , Mautalen C . Mineral and bone mass changes during pregnancy and lactation . Nutrition . 2004 ; 20 ( 2 ): 235 – 240.
- ↑ 41.0 41.1 41.2 41.3 Tibor LM, Sekiya JK. Differential diagnosis of pain around the hip joint. Arthroscopy. 2008;24(12): 1407–1421.
- ↑ 42.0 42.1 42.2 Pelvic Obstretic & Gyneacological Physiotherapy. Guidance for health professionals, pregnancy- related pelvic girdle pain.
- ↑ Hall H. et al., The effectiveness of complementary manual therapies for pregnancy-related back and pelvic pain. Medicine (Baltimore). 2016 Sep; 95(38): e4723.
- ↑ 44.0 44.1 44.2 44.3 44.4 44.5 Mens JM, Pool- Goudzwaard A, Stam HJ. Mobility of the pelvic joints in pregnancy-related lumbopelvic pain : a systematic review. Obstetrical Gynecological Survey Mar 2009; 64(3) : 200-208. (Level of evidence 1B)
- ↑ Kaj Wedenberg et al; A prospective randomized study comparing acupuncture with physiotherapy for low‐back and pelvic pain in pregnancy; AOGS; 2000 May; 331-335
- ↑ Helen Hall et al., The effectiveness of complementary manual therapies for pregnancy-related back and pelvic pain, Medicine (Baltimore). 2016 Sep; 95(38): e4723.
- ↑ Pennick V. et al., Interventions for preventing and treating low-back and pelvic pain during pregnancy (Review), Cochrane Database Syst Rev. 2013 Aug 1;(8):CD001139.
- ↑ Elden H. et al., Effects of craniosacral therapy as adjunct to standard treatment for pelvic girdle pain in pregnant women: a multicenter, single blind, randomized controlled trial, ELDEN H. et al., Januari 2013 AOGS, DOI: 10.1111/aogs.12096
- ↑ Qiuttan M. et al.,Transcutaneous Electrical Nerve stimulation (TENS) in patients with pregnancy- induced low back pain and/ or pelvic girdle pain, phys. med rehab kuror 2016:26: 91-95. ISSN 0940-6689
- ↑ E.H. Verstraete, G. Vanderstraeten, W. Parewijck. Pelvic Girdle Pain during or after Pregnancy: a review of recent evidence and a clinical care path proposal: a systematic review. Pubmed 2013; 5(1); 33-43