Pudendal Nerve: Difference between revisions
No edit summary |
No edit summary |
||
| Line 10: | Line 10: | ||
The pudendal nerve is the main nerve of perineum, pelvic floor muscles and the external genitalia.<ref name=":0">Rojas-Gómez MF, Blanco-Dávila R, Tobar-Roa V, Gómez-González AM, Ortiz-Zableh AM, Ortiz-Azuero A. https://www.researchgate.net/publication/318085947_Regional_anesthesia_guided_by_ultrasound_in_the_pudendal_nerve_territory Colombian Journal of Anestesiology. 2017 Sep;45(3):200-9.</ref>Benjamin Alcock first described it in 1836 while researching the internal pudendal artery's path. | The pudendal nerve is the main nerve of perineum, pelvic floor muscles and the external genitalia.<ref name=":0">Rojas-Gómez MF, Blanco-Dávila R, Tobar-Roa V, Gómez-González AM, Ortiz-Zableh AM, Ortiz-Azuero A. https://www.researchgate.net/publication/318085947_Regional_anesthesia_guided_by_ultrasound_in_the_pudendal_nerve_territory Colombian Journal of Anestesiology. 2017 Sep;45(3):200-9.</ref>Benjamin Alcock first described it in 1836 while researching the internal pudendal artery's path. | ||
The pudendal nerve is a mixed nerve having sensory, motor, and autonomic functions. It is one of the primary nerve originating from sacral plexus following sciatic nerve. The nerve is paired, meaning that it is found bilaterally, one on the left and one on the right side of the body.<ref name=":1">Kinter KJ, Newton BW. [https://www.ncbi.nlm.nih.gov/books/NBK554736/ Anatomy, abdomen and pelvis, pudendal nerve.] InStatPearls [Internet] 2021 Sep 13. StatPearls Publishing.</ref> | The pudendal nerve is a mixed nerve having sensory, motor, and autonomic functions. It is one of the primary nerve originating from [[Sacral Plexus|sacral plexus]] following sciatic nerve. The nerve is paired, meaning that it is found bilaterally, one on the left and one on the right side of the body.<ref name=":1">Kinter KJ, Newton BW. [https://www.ncbi.nlm.nih.gov/books/NBK554736/ Anatomy, abdomen and pelvis, pudendal nerve.] InStatPearls [Internet] 2021 Sep 13. StatPearls Publishing.</ref> | ||
[[File:Pudendal nerve.svg.png|thumb|Branches of Pudendal nerve in Male]] | [[File:Pudendal nerve.svg.png|thumb|Branches of Pudendal nerve in Male]] | ||
=== Course === | === Course === | ||
* The pudendal nerve receives input from the primary ventral roots of S2–S4 in the sacral plexus, which converge to form the nerve adjacent to the lateral wall of the pelvic cavity. It then forms 1, 2 or three trunks before its final branching; variable contributions from S1 and/or S5. | * The pudendal nerve receives input from the primary ventral roots of S2–S4 in the sacral plexus, which converge to form the nerve adjacent to the lateral wall of the [[Pelvis|pelvic]] cavity. It then forms 1, 2 or three trunks before its final branching; variable contributions from S1 and/or S5. | ||
* Throughout most of its path, the nerve is closely associated with the branches of the internal pudendal artery and vein. | * Throughout most of its path, the nerve is closely associated with the branches of the internal pudendal artery and vein. | ||
* exits the pelvis via the greater sciatic foramen inferior to the piriformis muscle and bends around the posterior aspect of the sacrospinous ligament. | * It then, exits the pelvis via the greater sciatic foramen inferior to the [[piriformis]] muscle and bends around the posterior aspect of the sacrospinous ligament. | ||
* It courses for a very short distance within the gluteal region where it bends around the sacrospinous ligament to enter the perineum through the lesser sciatic foramen. | * It courses for a very short distance within the gluteal region where it bends around the [[Sacrospinous Ligament|sacrospinous ligament]] to enter the perineum through the lesser sciatic foramen. | ||
** While in the gluteal region the pudendal nerve is proximal to the ischial spine where it is the target of a pudendal nerve block.<ref name=":1" /> | ** While in the gluteal region the pudendal nerve is proximal to the ischial spine where it is the target of a pudendal nerve block.<ref name=":1" /> | ||
** Compressive nerve diseases are usually identified at the interligamentous section of its journey, which is when it is dorsal to the sacrospinous ligament and ventral to the sacrotuberous ligament.<ref name=":0" /> | ** Compressive nerve diseases are usually identified at the interligamentous section of its journey, which is when it is dorsal to the sacrospinous ligament and ventral to the [[Sacrotuberous Ligament|sacrotuberous ligament]].<ref name=":0" /> | ||
* After exiting the lesser sciatic foramen and entering the perineum, the nerve passes through a sheath of connective tissue on the medial wall of the obturator internus muscle called the pudendal (Alcock’s) canal. | * After exiting the lesser sciatic foramen and entering the perineum, the nerve passes through a sheath of connective tissue on the medial wall of the [[Obturator Internus|obturator internus]] muscle called the pudendal (Alcock’s) canal. | ||
* It continues to course through the pudendal canal, giving off three consecutive branches on its path towards the pubic symphysis. | * It continues to course through the pudendal canal, giving off three consecutive branches on its path towards the pubic symphysis. | ||
* The pudendal nerve gives rise to the inferior anal nerve as soon as it enters the canal (also called the inferior rectal nerve). | * The pudendal nerve gives rise to the inferior anal nerve as soon as it enters the canal (also called the inferior rectal nerve). | ||
| Line 37: | Line 37: | ||
== Function == | == Function == | ||
The pudendal nerve consists of 70% somatic fibres (50% is sensory and 20% is motor) and 30% autonomic fibers. | |||
* '''Inferior rectal nerve''': carries somatic motor fibers to the external anal sphincter and carries sensations back from the anal canal, inferior to the pectinate line. | |||
* Inferior rectal nerve: carries somatic motor fibers to the external anal sphincter and carries sensations back from the anal canal, inferior to the pectinate line. | * '''Perineal nerve:''' supply motor and sensory fibers to the structures in the urogenital triangle, including the external urethral sphincter, the posterior scrotum in males, and the labia minora, vaginal vestibule, lower one-fifth of the vaginal canal and the posterior aspect of the labia majora in females. | ||
* Perineal nerve: supply motor and sensory fibers to the structures in the urogenital triangle, including the external urethral sphincter, the posterior scrotum in males, and the labia minora, vaginal vestibule, lower one-fifth of the vaginal canal and the posterior aspect of the labia majora in females. | |||
** Deep (muscular) branch: | ** Deep (muscular) branch: | ||
*** In both | *** In both sexes, it innervates the skeletal muscles of the superficial perineal space (pouch), i.e., the ischiocavernosus, superficial transverse perineal, and bulbospongiosus muscles. Thus, it contributes to maximal erectile rigidity, ejaculation, and coordinated contractions of all the perineal muscles and pelvic diaphragm. | ||
*** In either sex, while in the deep perineal space (pouch), the deep perineal nerve innervates the two deep transverse perineal muscles, and more importantly, the external urethral sphincter allowing for the voluntary control of micturition. | *** In either sex, while in the deep perineal space (pouch), the deep perineal nerve innervates the two deep transverse perineal muscles, and more importantly, the external urethral sphincter allowing for the voluntary control of [[Micturition (Urinary) Reflex|micturition.]] | ||
*** In females, the deep perineal nerve also innervates two other skeletal muscles in the deep perineal space: the compressor urethrae and the sphincter urethrovaginalis. | *** In females, the deep perineal nerve also innervates two other skeletal muscles in the deep perineal space: the compressor urethrae and the sphincter urethrovaginalis. | ||
** The superficial branch of the perineal nerve carries somatic sensation from most of the skin overlying the urogenital triangle and are called posterior scrotal or labial nerves. | ** The superficial branch of the perineal nerve carries somatic sensation from most of the skin overlying the urogenital triangle and are called posterior scrotal or labial nerves. | ||
* Dorsal Nerve of the Penis (males) or Dorsal Nerve of the Clitoris (females): | * '''Dorsal Nerve of the Penis (males) or Dorsal Nerve of the Clitoris (females)''': | ||
** This is solely a cutaneous branch of the pudendal nerve and is critical to sexual function since it brings back somatic sensations from the shaft (body) and glans of the penis or clitoris.<ref name=":1" /> | ** This is solely a cutaneous branch of the pudendal nerve and is critical to sexual function since it brings back somatic sensations from the shaft (body) and glans of the penis or clitoris.<ref name=":1" /> | ||
** This branch is also part of an important neuropathway in forming erections. Within the lumbosacral spinal cord, the dorsal nerve afferent fibers communicate with the cavernous nerves (carrying parasympathetic axons) which pierce the perineal membrane to innervate and promote the vasodilation of erectile tissue when stimulated.<ref name=":1" /> | ** This branch is also part of an important neuropathway in forming erections. Within the lumbosacral spinal cord, the dorsal nerve afferent fibers communicate with the cavernous nerves (carrying parasympathetic axons) which pierce the perineal membrane to innervate and promote the vasodilation of erectile tissue when stimulated.<ref name=":1" /> | ||
| Line 57: | Line 56: | ||
#* It is a procedure that involves injecting a local anesthetic in the proximity of the pudendal nerve. This procedure can help in the diagnosis of pudendal nerve entrapment and can be used for pain relief during obstetric procedures, especially during childbirth in women who are unable to undergo spinal anesthesia. <ref name=":1" /> | #* It is a procedure that involves injecting a local anesthetic in the proximity of the pudendal nerve. This procedure can help in the diagnosis of pudendal nerve entrapment and can be used for pain relief during obstetric procedures, especially during childbirth in women who are unable to undergo spinal anesthesia. <ref name=":1" /> | ||
#* The block is performed by administering a single injection adjacent to the pudendal nerve to transiently prevent nerve conduction. In these procedures, the ischial spine is used as a landmark to aid in administering the anesthetic in the correct location.<ref name=":1" /> | #* The block is performed by administering a single injection adjacent to the pudendal nerve to transiently prevent nerve conduction. In these procedures, the ischial spine is used as a landmark to aid in administering the anesthetic in the correct location.<ref name=":1" /> | ||
#* It is also helpful in hemorrhoids, anorectal, vaginal, and perineal surgery, labor, episiotomies, prostate biopsy, prostate brachytherapy, interstitial cystitis, and penile surgery.<ref name=":0" /> | #* It is also helpful in hemorrhoids, anorectal, vaginal, and perineal surgery, labor, [[Episiotomy|episiotomies,]] prostate biopsy, prostate brachytherapy, [[Interstitial Cystitis|interstitial cystitis]], and penile surgery.<ref name=":0" /> | ||
# Iatrogenic damage to the pudendal nerve | # Iatrogenic damage to the pudendal nerve | ||
#* The risk of pudendal nerve injury is of particular importance in obstetrical, perineal, and proctological procedures.<ref name=":1" /> | #* The risk of pudendal nerve injury is of particular importance in obstetrical, perineal, and proctological procedures.<ref name=":1" /> | ||
| Line 68: | Line 67: | ||
* Prolonged sitting (e.g., seamstress, computer operators, judges, concert pianists, locomotive engineers) | * Prolonged sitting (e.g., seamstress, computer operators, judges, concert pianists, locomotive engineers) | ||
* Repetitive hip flexion (sports activities, exercising, jogging, cycling) | * Repetitive hip flexion (sports activities, exercising, jogging, cycling) | ||
* Direct trauma includes falls, motor vehicle accidents, vaginal delivery and pelvic surgeries, especially when using mesh (eg: surgeries for urinary incontinences, total abdominal hysterectomy) | * Direct trauma includes falls, motor vehicle accidents, vaginal delivery and pelvic surgeries, especially when using mesh (eg: surgeries for [[Urinary Incontinence|urinary incontinences]], total abdominal [[hysterectomy]]) | ||
* Radiation therapy especially in males treated for prostate cancer and patients treated for rectal and gynecological cancers<ref>Soon-Sutton TL, Feloney MP, Antolak S. [https://www.ncbi.nlm.nih.gov/books/NBK562246/ Pudendal neuralgia.] InStatPearls [Internet] 2021 Jul 31. StatPearls Publishing.</ref> | * Radiation therapy especially in males treated for [[Prostate Cancer|prostate cancer]] and patients treated for rectal and gynecological cancers<ref>Soon-Sutton TL, Feloney MP, Antolak S. [https://www.ncbi.nlm.nih.gov/books/NBK562246/ Pudendal neuralgia.] InStatPearls [Internet] 2021 Jul 31. StatPearls Publishing.</ref> | ||
=== Pain Assessment === | === Pain Assessment === | ||
* Patient with pelvic pain (especially perineal and genital) with or without concurrent sexual, bladder, or bowel symptoms | * Patient with pelvic [[Pain Assessment|pain (]]<nowiki/>especially perineal and genital) with or without concurrent sexual, bladder, or bowel symptoms | ||
* Gradual onset of pain except for acute trauma | * Gradual onset of pain except for acute trauma | ||
* Pain is less in morning and progress with progression of the day | * Pain is less in the morning and progress with progression of the day | ||
* Type of pain is usually burning pain , but may also experience tingling, aching, stabbing, and shock-like pain | * Type of pain is usually burning pain , but may also experience tingling, aching, stabbing, and shock-like pain | ||
* Pain aggravates while sitting and relieves when standing, lying down, or seated on a toilet. | * Pain aggravates while sitting and relieves when standing, lying down, or seated on a toilet. | ||
* Pain distribution may be limited or extensive and may include the vulva, vagina, clitoris, perineum, and rectum in females; glans penis, scrotum, perineum, and rectum in males | * Pain distribution may be limited or extensive and may include the vulva, vagina, clitoris, perineum, and rectum in females; glans penis, scrotum, perineum, and rectum in males | ||
* Other symptoms associated with PN include urinary frequency, urgency, symptoms mimicking interstitial cystitis, painful ejaculation, dyspareunia, painful nocturnal orgasms, and persistent sexual arousal. | * Other symptoms associated with PN include urinary frequency, urgency, symptoms mimicking interstitial cystitis, painful ejaculation, [[dyspareunia]], painful nocturnal orgasms, and persistent sexual arousal. | ||
* Foreign body sensation<ref>Kaur J, Singh P. [https://www.ncbi.nlm.nih.gov/books/NBK544272/ Pudendal nerve entrapment syndrome.]</ref> | * Foreign body sensation<ref>Kaur J, Singh P. [https://www.ncbi.nlm.nih.gov/books/NBK544272/ Pudendal nerve entrapment syndrome.]</ref> | ||
== Treatment == | |||
Management of Pudendal neuralgia is explained on this page [[Pudendal Neuralgia]] | |||
== References == | == References == | ||
Revision as of 11:01, 1 July 2022
Original Editor - Manisha Shrestha
Top Contributors - Manisha Shrestha, Lucinda hampton, Kim Jackson, Wendy Snyders and Cindy John-Chu
Description[edit | edit source]
The term 'Pudendal' comes from Latin pudenda, meaning “external genitals”, derived from pudendum, meaning "parts to be ashamed of[1]
The pudendal nerve is the main nerve of perineum, pelvic floor muscles and the external genitalia.[2]Benjamin Alcock first described it in 1836 while researching the internal pudendal artery's path.
The pudendal nerve is a mixed nerve having sensory, motor, and autonomic functions. It is one of the primary nerve originating from sacral plexus following sciatic nerve. The nerve is paired, meaning that it is found bilaterally, one on the left and one on the right side of the body.[3]
Course[edit | edit source]
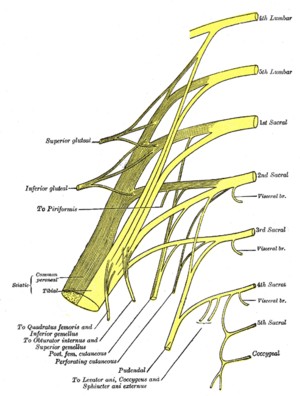
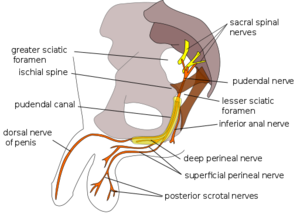
- The pudendal nerve receives input from the primary ventral roots of S2–S4 in the sacral plexus, which converge to form the nerve adjacent to the lateral wall of the pelvic cavity. It then forms 1, 2 or three trunks before its final branching; variable contributions from S1 and/or S5.
- Throughout most of its path, the nerve is closely associated with the branches of the internal pudendal artery and vein.
- It then, exits the pelvis via the greater sciatic foramen inferior to the piriformis muscle and bends around the posterior aspect of the sacrospinous ligament.
- It courses for a very short distance within the gluteal region where it bends around the sacrospinous ligament to enter the perineum through the lesser sciatic foramen.
- While in the gluteal region the pudendal nerve is proximal to the ischial spine where it is the target of a pudendal nerve block.[3]
- Compressive nerve diseases are usually identified at the interligamentous section of its journey, which is when it is dorsal to the sacrospinous ligament and ventral to the sacrotuberous ligament.[2]
- After exiting the lesser sciatic foramen and entering the perineum, the nerve passes through a sheath of connective tissue on the medial wall of the obturator internus muscle called the pudendal (Alcock’s) canal.
- It continues to course through the pudendal canal, giving off three consecutive branches on its path towards the pubic symphysis.
- The pudendal nerve gives rise to the inferior anal nerve as soon as it enters the canal (also called the inferior rectal nerve).
- When it reaches the distal portion of the canal, the nerve bifurcates and gives rise to two more branches: the perineal nerve and the dorsal nerve of the penis/clitoris.
Root[edit | edit source]
S2,S3,S4
Branches[edit | edit source]
There are three main branches of the pudendal nerve. They are:
- Inferior rectal branch
- Perineal branch: which is divided into superficial (cutaneous) and deep (muscular) perineal nerve, which further divides into medial and posterolateral scrotal/labial nerve.
- Dorsal branch of penis/clitoris
Function[edit | edit source]
The pudendal nerve consists of 70% somatic fibres (50% is sensory and 20% is motor) and 30% autonomic fibers.
- Inferior rectal nerve: carries somatic motor fibers to the external anal sphincter and carries sensations back from the anal canal, inferior to the pectinate line.
- Perineal nerve: supply motor and sensory fibers to the structures in the urogenital triangle, including the external urethral sphincter, the posterior scrotum in males, and the labia minora, vaginal vestibule, lower one-fifth of the vaginal canal and the posterior aspect of the labia majora in females.
- Deep (muscular) branch:
- In both sexes, it innervates the skeletal muscles of the superficial perineal space (pouch), i.e., the ischiocavernosus, superficial transverse perineal, and bulbospongiosus muscles. Thus, it contributes to maximal erectile rigidity, ejaculation, and coordinated contractions of all the perineal muscles and pelvic diaphragm.
- In either sex, while in the deep perineal space (pouch), the deep perineal nerve innervates the two deep transverse perineal muscles, and more importantly, the external urethral sphincter allowing for the voluntary control of micturition.
- In females, the deep perineal nerve also innervates two other skeletal muscles in the deep perineal space: the compressor urethrae and the sphincter urethrovaginalis.
- The superficial branch of the perineal nerve carries somatic sensation from most of the skin overlying the urogenital triangle and are called posterior scrotal or labial nerves.
- Deep (muscular) branch:
- Dorsal Nerve of the Penis (males) or Dorsal Nerve of the Clitoris (females):
- This is solely a cutaneous branch of the pudendal nerve and is critical to sexual function since it brings back somatic sensations from the shaft (body) and glans of the penis or clitoris.[3]
- This branch is also part of an important neuropathway in forming erections. Within the lumbosacral spinal cord, the dorsal nerve afferent fibers communicate with the cavernous nerves (carrying parasympathetic axons) which pierce the perineal membrane to innervate and promote the vasodilation of erectile tissue when stimulated.[3]
Clinical relevance[edit | edit source]
- Pudendal Neuralgia
- Pudendal nerve block
- It is a procedure that involves injecting a local anesthetic in the proximity of the pudendal nerve. This procedure can help in the diagnosis of pudendal nerve entrapment and can be used for pain relief during obstetric procedures, especially during childbirth in women who are unable to undergo spinal anesthesia. [3]
- The block is performed by administering a single injection adjacent to the pudendal nerve to transiently prevent nerve conduction. In these procedures, the ischial spine is used as a landmark to aid in administering the anesthetic in the correct location.[3]
- It is also helpful in hemorrhoids, anorectal, vaginal, and perineal surgery, labor, episiotomies, prostate biopsy, prostate brachytherapy, interstitial cystitis, and penile surgery.[2]
- Iatrogenic damage to the pudendal nerve
- The risk of pudendal nerve injury is of particular importance in obstetrical, perineal, and proctological procedures.[3]
Assessment[edit | edit source]
History[edit | edit source]
Common causes for pudendal nerve injury include:
- Prolonged sitting (e.g., seamstress, computer operators, judges, concert pianists, locomotive engineers)
- Repetitive hip flexion (sports activities, exercising, jogging, cycling)
- Direct trauma includes falls, motor vehicle accidents, vaginal delivery and pelvic surgeries, especially when using mesh (eg: surgeries for urinary incontinences, total abdominal hysterectomy)
- Radiation therapy especially in males treated for prostate cancer and patients treated for rectal and gynecological cancers[5]
Pain Assessment[edit | edit source]
- Patient with pelvic pain (especially perineal and genital) with or without concurrent sexual, bladder, or bowel symptoms
- Gradual onset of pain except for acute trauma
- Pain is less in the morning and progress with progression of the day
- Type of pain is usually burning pain , but may also experience tingling, aching, stabbing, and shock-like pain
- Pain aggravates while sitting and relieves when standing, lying down, or seated on a toilet.
- Pain distribution may be limited or extensive and may include the vulva, vagina, clitoris, perineum, and rectum in females; glans penis, scrotum, perineum, and rectum in males
- Other symptoms associated with PN include urinary frequency, urgency, symptoms mimicking interstitial cystitis, painful ejaculation, dyspareunia, painful nocturnal orgasms, and persistent sexual arousal.
- Foreign body sensation[6]
Treatment[edit | edit source]
Management of Pudendal neuralgia is explained on this page Pudendal Neuralgia
References[edit | edit source]
- ↑ Harper, Douglas. "Pudendum". Online Etymology Dictionary.
- ↑ 2.0 2.1 2.2 Rojas-Gómez MF, Blanco-Dávila R, Tobar-Roa V, Gómez-González AM, Ortiz-Zableh AM, Ortiz-Azuero A. https://www.researchgate.net/publication/318085947_Regional_anesthesia_guided_by_ultrasound_in_the_pudendal_nerve_territory Colombian Journal of Anestesiology. 2017 Sep;45(3):200-9.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Kinter KJ, Newton BW. Anatomy, abdomen and pelvis, pudendal nerve. InStatPearls [Internet] 2021 Sep 13. StatPearls Publishing.
- ↑ Causes of Pudendal Neuralgia. Available from: https://www.youtube.com/watch?v=mLvwV_Tfas4 lasted accessed: 27th June 2022
- ↑ Soon-Sutton TL, Feloney MP, Antolak S. Pudendal neuralgia. InStatPearls [Internet] 2021 Jul 31. StatPearls Publishing.
- ↑ Kaur J, Singh P. Pudendal nerve entrapment syndrome.