Resisted Exercise Initiative (RExI): Difference between revisions
Kim Jackson (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| Line 44: | Line 44: | ||
A statement from National Strength and Conditioning Association highlighted the benefits of resistance exercise to older people (Fragala et al .2019).<ref name=":0">Fragala MS, Cadore EL, Dorgo S, Izquierdo M, Kraemer WJ, Peterson MD, Ryan ED. Resistance training for older adults: position statement from the national strength and conditioning association. The Journal of Strength & Conditioning Research. 2019 Aug 1;33(8).</ref> Also Fragala et al .2019 recommended the resisted exercise training programme should be matched appropriately to the individual's abilities and goals. A properly designed resistance training programme can | A statement from National Strength and Conditioning Association highlighted the benefits of resistance exercise to older people (Fragala et al .2019).<ref name=":0">Fragala MS, Cadore EL, Dorgo S, Izquierdo M, Kraemer WJ, Peterson MD, Ryan ED. Resistance training for older adults: position statement from the national strength and conditioning association. The Journal of Strength & Conditioning Research. 2019 Aug 1;33(8).</ref> Also Fragala et al .2019 recommended the resisted exercise training programme should be matched appropriately to the individual's abilities and goals. A properly designed resistance training programme can:<ref>Ratamess N. ACSM's foundations of strength training and conditioning. Lippincott Williams & Wilkins; 2021 Mar 15.</ref> | ||
# | # Counteract the age related changes in contractile function, atrophy and morphology of aging human skeletal muscle. | ||
# Enhance the muscular strength, power and neuromuscular functioning of older adults. | # Enhance the muscular strength, power and neuromuscular functioning of older adults. | ||
# Improve older adults resistance to injuries and catastrophic events like [[Falls in elderly|falls.]] | # Improve mobility, physical functioning, performance in [[ADLs|activities of daily living]] (ADL), and preserve the independence of olcdf adults. | ||
# Improve an older adults' resistance to injuries and catastrophic events like [[Falls in elderly|falls.]] | |||
# Help | # Help improve the psychosocial well-being of older adults. | ||
# | # | ||
| Line 120: | Line 120: | ||
== Principles of Strength and Conditioning == | == Principles of Strength and Conditioning == | ||
[[ | [[Strength and Conditioning]] is the selection and development of dynamic /static exercises used to improve physical performance. Whilst it originally benefited athletes it is now widely used in both the sporting world and the wider population, including older people. | ||
==== Principle 1 - Individuality ==== | |||
Each person will have unique responses to the same training stiumulus, due to individual characteristics, such as biological age, training age, gender, genetics, body size and shape, past injuries, etc. Training should be adjusted to the individual's characteristics and needs. [ref] | |||
==== Principle 2 - Specificity ==== | |||
Physiological adaptations to training are specific to the muscle groups trained, the intensity of the exercise, the metabolic demands of the exercise and specific movements and activities.[ref] | |||
==== Principle 3 - Progressive Overload ==== | |||
Certain adaptations require training with greater stimulus than that to which the body is accustomed. | |||
This could be done by increasing the intensity, duration or frequency of training. [ref]Overloading should occur at an optimal level and time frame to maximize performance. | |||
Overloading too quickly may lead to poor technique or injury, while very slow overloading may result in little or no improvement. [ref] | |||
To continue to gain benefits, strength training activities need to be done to the point where it is difficult to do another repetition (close to maximal force generating capacity). | |||
Overload leads to muscle hypertrophy via activation of satellite cells. [ref] | |||
==== Principle 4 - Diminishing Returns ==== | |||
An individual's level of training determines how much improvement in performance is achieved due to the training. | |||
A novice will see large and relatively quick gains in performance when they begin training. However, the gains become smaller, and come about slower, as the individual becomes more experienced. [ref] | |||
==== Principle 5 - Reversibility ==== | |||
The effects of training will be lost if a training stimulus is removed for an extended period of time: "Use it or lose it." [ref] | |||
For more information you can read the Physiopedia [[Strength and Conditioning|strength and conditioning]] article. | For more information you can read the Physiopedia [[Strength and Conditioning|strength and conditioning]] article. | ||
Revision as of 09:24, 19 April 2022
Top Contributors - Shaimaa Eldib, Kim Jackson, Oyemi Sillo and Aminat Abolade
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (19/04/2022)
Introduction[edit | edit source]
The current volume and level of acuity of elderly patients in acute care settings challenges physical therapists to address all needs. One related aspect of practice that is receiving increasing attention is the optimal prescription of resistance exercise in these settings. To support best practice and assist in the use of resisted exercise by physical therapists for elderly patients the PT Knowledge Broker facilitated project, started in April 2019, created the Resisted Exercise Initiative (RExI)
Objectives:
- To determine existing practice.
- To identify opportunities to support enhanced practice.
- To undertake knowledge translation (KT) strategies to target barriers to enhance using of resisted exercise.
- To evaluate effect of introduction of the KT strategies.
Definition and Benefits[edit | edit source]
Resistance Exercise is defined as movement using body weight or external resistance that improves muscular strength, power, endurance and it may positively impact mobility, function and independence.[1]
Benefits of resistance exercise:[2][3]
- Improves muscle strength and tone
- Maintain flexibility and balance
- Weight management and increased muscle to fat ratio
- May help to prevent or reduce cognitive decline in older people
- Greater stamina (people will not tire as easily due to improved body strength)
- Prevention or control of chronic conditions eg (back pain, heart disease, arthritis, obesity &depression)
- Pain management
- Improves posture and decreases the risk of injury
- Increases bone density
- Decreases risk of osteoporosis
- Improves sense of wellbeing, boosts confidence and self-esteem
A statement from National Strength and Conditioning Association highlighted the benefits of resistance exercise to older people (Fragala et al .2019).[4] Also Fragala et al .2019 recommended the resisted exercise training programme should be matched appropriately to the individual's abilities and goals. A properly designed resistance training programme can:[5]
- Counteract the age related changes in contractile function, atrophy and morphology of aging human skeletal muscle.
- Enhance the muscular strength, power and neuromuscular functioning of older adults.
- Improve mobility, physical functioning, performance in activities of daily living (ADL), and preserve the independence of olcdf adults.
- Improve an older adults' resistance to injuries and catastrophic events like falls.
- Help improve the psychosocial well-being of older adults.
Considerations and Flags[edit | edit source]
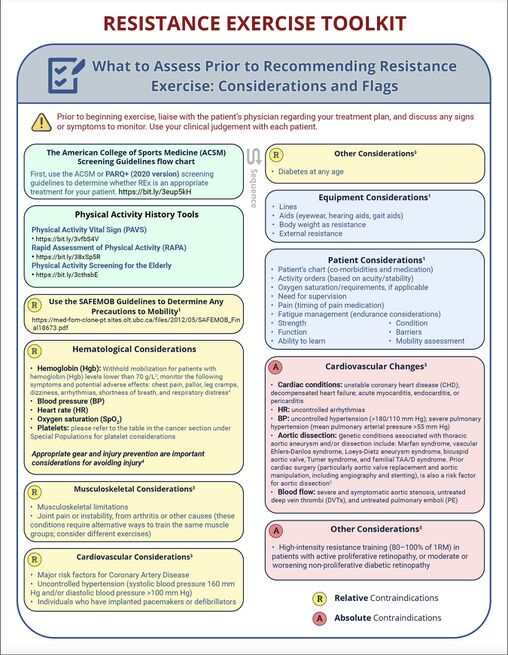
Prior to beginning exercise, liaise with the patient's physician regarding your treatment plan and discuss any signs or symptoms to monitor. You can also refer to the American College of Sports Medicine (ACSM) screening guidelines flow chart to determine if REx is appropriate treatment for your patient.
Relative Contraindications[edit | edit source]
If a patient has any of the following caution should be used when considering including resistance exercises in your treatment plan.
Absolute Contraindications[edit | edit source]
Patients with the following conditions should not exercise until their condition is stable or controlled. It is important to assess each patient and to use your clinical judgement of a patient's suitability to participate in a resistance exercise programme. See the image below for considerations and flags :[6][7][8]
Exercise Physiology Foundation[edit | edit source]
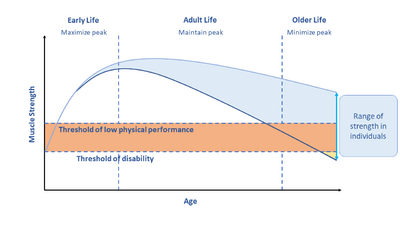
Muscle strength decreases through the adult years and into older life. The decreases in strength are associated with increased disability, falls and mortality.
Loss in strength can be moderated through maximizing muscle in early adulthood, maintaining strength in middle age and minimizing loss in older age. This can be achieved through resistance exercise training.
While resisted exercise is more impactful if done earlier in life, it can still have positive effects if done later in life.
Muscle Strength and Life Course[edit | edit source]
Muscle strength decreases through adult years and life course. There is a strong link between decreased muscle strength and falls, immobility and mortality.[4]
Loss in strength can be moderated by maximizing muscle in early adulthood, maintaining strength in middle age and minimizing loss in older age. This can be achieved through resistance exercise training.[4] [9] *(diagram)
Muscle Atrophy[edit | edit source]
Hospitalized older adults may experience some problems from immobility for example - muscle atrophy, sarcopenia, [9]cachexia. Muscle Atrophy can be categorised into 3 types - Disuse or physiologic Atrophy; Neurogenic Atrophy[10] [11]and Myogenic Atrophy[11]
Disuse or Physiologic Atrophy[edit | edit source]
Caused by bed rest and/or immobility. It results in the same number of muscle fibers, but reduced volume/diameter with associated reduction in muscle mass; decrease in protein synthesis; Type 1 antigravity muscles most affected. Susceptible to sarcomere damage when reloading.
Neurogenic Atrophy[edit | edit source]
Caused by injury or disease of nerve supplying muscle (upper or lower motor neuron); generally more sudden than in disuse atrophy, for example:
- Amyotrophic lateral sclerosis (ALS or Lou Gehrig's disease)
- Spinal muscular atrophy
- Damage to a single nerve, such as axillary nerve
- Spinal cord injury
- Guillain-Barre syndrome
- Nerve damage caused by injury, diabetes, toxins, or alcohol;
- Polio
This results in atrophy of Type I and Type II fibers. Hypertrophy of Type I fibers can occur with re-innervation of denervated fibers by surviving collateral nerves. A shift of fiber type typically occurs from Type I to Type II[ref]
Myogenic Atrophy[edit | edit source]
Muscle diseases such as muscular dystrophy, polymyositis, dermatomyositis, metabolic myopathy, congential myopathy, myotonia[ref]
This results in simultaneous occurence of atrophic and hypertrophic Type I and Type II fibers in most myopathies. Atrophy of Type II fibers is a non-specific event, and occurs in many myopathic disorders. Selective Type I atrophy happens in various congenital myopathies and myotonic dystrophy[ref]
Sarcopenia[edit | edit source]
Sarcopenia is defined as a progressive and generalized skeletal muscle disorder that is associated with an increased likelihood of adverse outcomes like falls, fractures, physical disability and mortality.[9] Sarcopenia is considered a muscle disease ( muscle failure ) with the following 3 criteria:
- Low muscle strength
- Low muscle quantity and quality
- Low physical performance
- Probable sarcopenia is identified by criteria 1.
- Diagnosis is confirmed by additional documentation of criteria 2.
- Sarcopena is considered severe if the 1, 2, and 3 criteria are met.
For more information on Sarcopenia and resisted exercise visit the RExI Toolkit
Cachexia[edit | edit source]
Cachexia is a complex metabolic syndrome associated with underlying illness and characterized by loss of muscle with or without loss of fat mass. The prominent clinical feature of cachexia is weight loss in adults (corrected for fluid retention) or growth failure in children (excluding endocrine disorders). Anorexia, inflammation, insulin resistance, and increased muscle protein breakdown are frequently associated with cachexia. Cachexia is distinct from starvation, age-related loss of muscle mass, primary depression, malabsorption, and hyperthyroidism and is associated with increased morbidity. Sarcopenia is one of the factors that may cause cachexia.[12][13]
Regeneration of Injured Skeletal Muscle[edit | edit source]
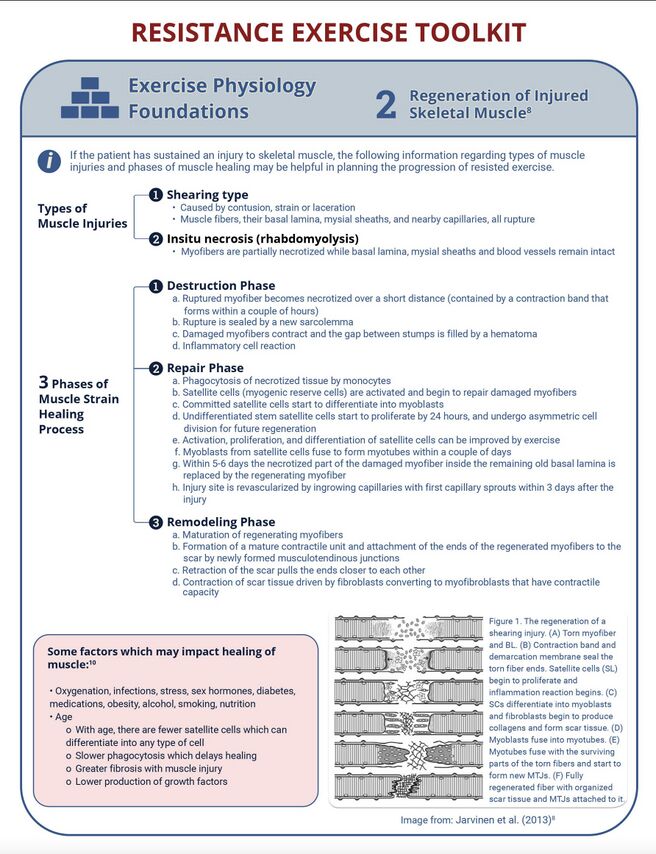
If the patient has sustained an injury to skeletal muscle, the following information regarding types of muscle injuries and phases of muscle healing may be helpful in planning the progression of resisted exercise.[14]
Principles of Strength and Conditioning[edit | edit source]
Strength and Conditioning is the selection and development of dynamic /static exercises used to improve physical performance. Whilst it originally benefited athletes it is now widely used in both the sporting world and the wider population, including older people.
Principle 1 - Individuality[edit | edit source]
Each person will have unique responses to the same training stiumulus, due to individual characteristics, such as biological age, training age, gender, genetics, body size and shape, past injuries, etc. Training should be adjusted to the individual's characteristics and needs. [ref]
Principle 2 - Specificity[edit | edit source]
Physiological adaptations to training are specific to the muscle groups trained, the intensity of the exercise, the metabolic demands of the exercise and specific movements and activities.[ref]
Principle 3 - Progressive Overload[edit | edit source]
Certain adaptations require training with greater stimulus than that to which the body is accustomed.
This could be done by increasing the intensity, duration or frequency of training. [ref]Overloading should occur at an optimal level and time frame to maximize performance.
Overloading too quickly may lead to poor technique or injury, while very slow overloading may result in little or no improvement. [ref]
To continue to gain benefits, strength training activities need to be done to the point where it is difficult to do another repetition (close to maximal force generating capacity).
Overload leads to muscle hypertrophy via activation of satellite cells. [ref]
Principle 4 - Diminishing Returns[edit | edit source]
An individual's level of training determines how much improvement in performance is achieved due to the training.
A novice will see large and relatively quick gains in performance when they begin training. However, the gains become smaller, and come about slower, as the individual becomes more experienced. [ref]
Principle 5 - Reversibility[edit | edit source]
The effects of training will be lost if a training stimulus is removed for an extended period of time: "Use it or lose it." [ref]
For more information you can read the Physiopedia strength and conditioning article.
The Effects of Resistance Exercise on Muscle[edit | edit source]
Key terms:[15]
- Strength The ability to produce force
- Power The ability to produce force at a high speed of movement (force x distance/time)
- Motor Unit[15] Consists of an alpha motor neuron and the muscle fibres innervated by it
- Fibre Types[18][10]
- Type I muscle fibres are considered slower but more fatigue-resistant fibres (e.g. beneficial for long distance runners).
- Type II fibres are considered the faster, more powerful fibres, but are also more susceptible to fatigue (e.g. more beneficial for sprinters and lifters)
- Henneman's Size Principle[19]
- As levels of activation increase (either through increased load or speed), larger motor units are recruited (i.e. Type I, Type IIa, and Type IIb in succession).
How to Increase Hypertrophy, Strength and Power[edit | edit source]
The number of motor units is one of the most important determinants of power, strength, and muscle size. Two ways of accomplishing higher motor unit recruitment are:
- Heavier resistance: Henneman's size principle
- Low resistance, high reps to momentary muscle failure or near failure.[ref15]
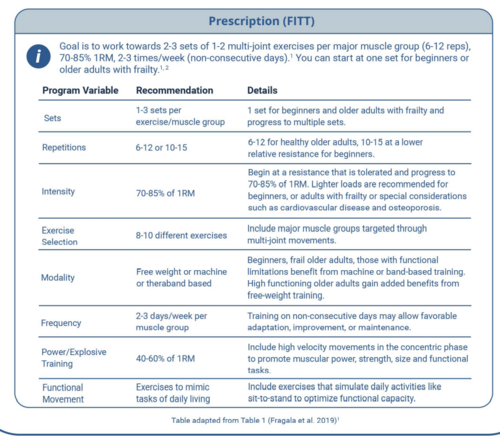
Prescription Principles (Older Adults)[edit | edit source]
Where possible, resistance exercise should be prescribed in combination with aerobic training because both types of exercise elicit distinct benefits. To optimize functional capacity, resistance training programs should include familiarization to training in which the patient's body mass is used for resistance and in which daily activities are simulated (like sit-to-stand).[20] High speed motion (at low to moderate intensity 30-60% 1 RM) can also be incorporated to promote greater improvements in the functional task performance of older adults. For more information about resistance training in the frail older adult, see the "Special Population " section on frailty.
Grip strength is a robust proxy indicator of overall strength. Grip strength of <26kg in men and <16 kg in women have been established as a biomarker of age related disability and early mortality and have been strongly related to incident mobility limitations and mortality.
Assessment[edit | edit source]
- Screen for contraindications
- Resistance exercise has been shown to be safe in the frail, elderly population, but if you have any questions or are unsure of medical stability for resistance exercises, check with the primary care provider, or use the Physical Activity Readiness Questionnaire for Everyone (PAR-Q+) and electronic Physical Activity Readiness Medical Examination (ePARmed-X+) programs
Prescription (FITT)[edit | edit source]
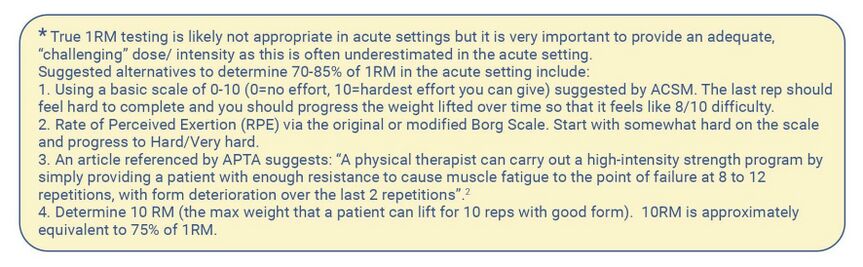
Goal is to work towards 2-3 sets of 1-2 multi-joint exercises per major muscle group (6-12 reps), 70-85% 1RM, 2-3 times/week (non-consecutive days). You can start at one set for beginners or older adults with frailty.[4][1]
Appropriate Intensity[edit | edit source]
- Free weights, machines, or bands or body weight can be used. Beginners, frail older adults, or those with functional limitations, benefit from machine-based resistance training, training with resistance bands and isometric training to help simplify and/or stabilize movements. High functioning older adults gain added benefit from free-weight resistance training as these exercises may engage additional muscles for support and stability and are more similar to movements used in activities of daily living. [4][21]
- Lift and lower the weight in a controlled manner with a focus on good form.[22]
- Rest 1.5-3 min between sets. The greater the intensity, the longer rest period is needed. The rest allows the muscles energy stores to be restored and therefore you can maximize the intensity of each set. Exercises done with the muscles in a fatigued state can lead to poor form and injury.[4][23]
- Primary attention should be given to lower body exercises as age-related reductions are more pronounced in the lower body.[21]
- In general, larger muscle groups should be worked before smaller muscle groups and multi-joint exercises (encouraged) should be done before uni-joint.[4]
Muscle Groups[edit | edit source]
The specific muscle groups targeted can be based on manual muscle testing, dynamometer testing, or functional muscle testing. Exercise selection should include major muscle groups targeted through multi-joint movements. Some examples of exercises that may be included in a whole-body resistance exercise session for general weakness or prevention of decline/deconditioning (if there is not a targeted area of weakness) include:
(see standardized exercise programs for more specifics)
Basic
- Squat (leg press if unable to do squat)
- Knee extension
- Knee flexion (leg curl or Romanian deadlift; deadlift with caution in elderly patients with spine issues)
- Chest press
- Seated low row
Complementary
- Hip adduction/abduction
- Hip flexion/extension
- Calf raise (standing or seated)
- Elbow flexion/extension
- Core/abdominals
One multi-joint exercise should be prescribed for major muscle groups although lower limbs may respond better to exercise.
Monitoring and Progression[edit | edit source]
Progression should follow general exercise principles of individualization, periodization, and progression.[1][24][25][21]
For progression of intensity, continue to use the method utilized for your initial strength testing prescription.
Progression[edit | edit source]
The following summarizes simple progression recommendations:
- Volume - manipulate sets, reps, weight
- Equipment - Body weight, bands, machine, free weight
- Stability - Lying, seated, kneeling, standing both feet on flat surface, standing single leg on flat surface, standing both legs on unstable surface, standing single leg on unstable surface[26]
- Complexity - Single joint + single exercise, multi-joint + single exercise, combined exercises
It is important to explain to patients that, with resistance training, they should expect some delayed onset muscle soreness.
For patients with medical issues, continue to monitor as per clinical judgement (e.g. SpO2 with patients with COPD; Borg for patients who are short of breath; heart rate for patients with a cardiac condition; or blood sugar for patients with diabetes.
Behaviour Change[edit | edit source]
It is important to support your patient to participate in strength training.[27] A well-supported behaviour change strategy to develop SMART goals and a plan that your client is confident that they can do:
Special Populations[edit | edit source]
Patients with COPD[edit | edit source]
COPD Key Points:[28]
- Performing pursed lip breathing and diaphragmatic breathing can increase breathing efficiency.[29]
- Increasing oxygen therapy during exercise may help to prevent exercise-induced hypoxemia.
- Instruct the patient to avoid extreme weather conditions and schedule exercise sessions during mid-late morning hours.
- Exercise frequency, duration, intensity as well as a list of exercises are included in the document AECOPD-Mob: Clinical Decision-Making Tool for Safe and Effective Mobilization of Hospitalized Patients with AECOPD.
Cardiac Patients[edit | edit source]
Cardiac Key Points:[29]
- Patients with left ventricular outflow, decompensated chronic heart failure or unstable dysrhythmias should not exercise.
- Patients with significant aortic stenosis should avoid strength training.
- Patients who have had a myocardial infarction should closely monitor intensity level and stay within the patient's recommended exercise heart rate range.
- Patients with congestive heart failure should closely monitor the intensity level and adjust workout if feeling fatigued. Instruct patient to stop exercising if they experience chest pain/angina.
- Patients with atrial fibrillation should adjust how hard and how long exercises are performed based on how they feel.
- Exercise should be performed without Valsalva maneuver (i.e. exhaling against a closed glottis).
- Instruct the patient to stop exercising immediately if experiencing angina.
- Upper body exercises may precipitate angina more readily than lower body exercises because of a higher pressor response.
- An extended warm up and cool down may reduce the risk of angina or other cardiovascular complications following exercise.
- If nitroglycerin has been prescribed, instruct the patient to carry it when exercising.
- Instruct the patient to avoid exercising in extreme weather conditions.
Stroke Patients[edit | edit source]
- Add task-oriented circuit training to improve transfer skills, mobility and ADLs/functional tasks.
- Avoid putting the most challenging or complex exercises at the end of an exercise program as the patient might be tired-potentially increasing risk of falls, injury and/or undue fatigue.[31]
- Encourage frequent rest breaks or reduce exercise intensity to decrease fatigue.
- Be mindful of use of compensatory strategies (drop foot, knee hyperextension, circumduction.
- Cue patients to be aware of neglected side, adjust movements and integrate exercises at midline for patients with neglect.
- Encourage bilateral movements with safe mechanics if the patient has a painful shoulder. (e.g. during arm raises, hold on to paretic arm, avoid pulling on paretic arm).
- Keep arm movements at or below shoulder level if the arm that is most affected by the stroke is weak and has decreased ROM. Arm movements above shoulder height can cause shoulder impingement and other injuries.
- Incorporate task related activities such as sit to stand, heel raises, step-ups, squats, and lunges.
- Avoid exercises that overload the joints or increase risk of falling. Begin each exercise in a stable position.
- Instruct the patient to avoid holding their breath during strength training because this can cause large fluctuations in blood pressure.
Patients with Parkinson's[edit | edit source]
Parkinson's Key Points:
- Choose the time of day for exercise that is best for the patient. It may be more effective to time exercises with medications. If fatigue is an issue, instruct the patient to try exercising first thing in the morning.[32]
- Patients may enjoy doing the exercises to music.[32]
- Consider exercising with supervision for those at risk of falls or who have had a recent change in medications (e.g. Levodopa/Carbidopa may produce exercise bradycardia).[33]
- If the patient is at risk of falling or freezing (becoming rigid), instruct them to hold on to a chair when performing standing exercises or do chair-based exercises instead.[29]
Patients with Multiple Sclerosis (MS)[edit | edit source]
Multiple Sclerosis (MS) Key Points:
- As MS patients lack endurance, increase the number of repetitions rather than the weight or resistance to help improve endurance.
- Instruct patients to avoid exercising in high temperatures and during the hottest part of the day.
- Encourage the patient to drink cool fluids before, during and after your exercise session.
- Avoid exercises/activities that may increase risk of falling.
- Set reasonable expectations for progression; i.e. some patients may not see improvements in strength over time depending on their disease progression, but resistance exercise is still beneficial in prevention of deterioration.
Patients with a Spinal Cord Injury[edit | edit source]
Spinal Cord Injury Key Points:
- An individual with a SCI should do at least 20 minutes of moderate to vigorous physical activity plus 3 sets of strength training exercises for each major functional muscle group at a moderate to vigorous intensity, 2x/week to reach a minimum threshold for improving cardiorespiratory health (cardiorespiratory fitness).
- Patients with cervical or high thoracic injury (i.e. T6 and above) should be aware of the symptoms of autonomic dysreflexia before beginning.[34] If a patient is experiencing autonomic dysreflexia, keep them sitting upright, address the suspected cause (e.g. full bladder, kinked catheter, or other stimulus below the level of injury). If symptoms persist, seek medical attention.
Patients with Arthritis[edit | edit source]
Osteoarthritis[edit | edit source]
- Combining exercise to increase to strength, flexibility, and aerobic capacity is the most effective management of lower limb osteoarthritis.
- Proper alignment is essential during loading with osteoarthritis of lower limb.
Rheumatoid Arthritis[edit | edit source]
- Schedule exercise each day when pain is lowest and pain medication most effective medication.
- Continue being physical active during flare and inflammation period, but avoid vigorous exercise and repetitive activities.
- Instruct patient to avoid over stretching.
Patients with Chronic Pain[edit | edit source]
- Gentle exercises help distract patients from pain.
- Advice patients to be persistent and patient.
Patients with Osteoporosis[edit | edit source]
- Resistance training machines should be avoided.
- Avoid unstable surfaces.
- Begin at lower intensity, exert effort to prevent falls.
- Strength and resistance exercises are recommended (weight bearing aerobic exercises & multicomponent exercise).
- Advise patient to focus on form and good alignment over intensity.
Patients with Diabetes[edit | edit source]
- Instruct patient to drink plenty of fluids before and after exercise.
- Always watch for signs of low blood sugar.
- Instruct patient to check with their physician if they felt signs of low blood sugar more than 2 or 3 times in one week with exercise. The medication or insulin dose may need to be changed.
Patients with Cancer[edit | edit source]
- Instruct patient to start with short periods of exercise.[2][38][39]
- Encourage patients to be as active as best as they can.
- Always ask patients to listen to their bodies.
Frail Patients[edit | edit source]
- Patients with frailty can follow the general guidelines but for intensity, start at a lower level (20%-30% 1RM() and progress to 80%.[36]
- Patients may be susceptible to dehydrationand insulin insenstivity - be alert to the warning signs of these conditions.[29]
- Avoid exercises that over-load joints or increase risk of falling. [29]
Patients with Poor Vision[edit | edit source]
- Consider using weight machines (as opposed to free weights).[29]
Patients with Poor Balance[edit | edit source]
- Consider using weight machines (as opposed to free weights).[29]
Patients with Back Pain[edit | edit source]
- Delay exercises that target the trunk region until at least 2 weeks after the first sign of symptoms.[29]
- Consider using weight machines (as opposed to free weights).[29]
Standardized Exercise Programme[edit | edit source]
Below are some sample resistance exercise programs target general strengthening of the major muscle groups (you can select the exercises that are most appropriate for your patient):
- Chest (Pectorals)
- Shoulder (Deltoids, Rotator Cuff, Scapula)
- Arms (Biceps, Triceps, Forearm)
- Back (Latissimus Darsi, Erector Spinae)
- Abdominals (Rectus Abdominus, Obliques)
- Legs (Hip Flexors, Gluteals, Quadriceps, Hamstrings)
There is one exercise set for supine/seated exercises and one for standing exercises. The programs can be modified if your patient has a specific area of weakness. Start with 1 set for beginners or patients with frailty with the goal of working towards 2-3 sets of 6-12 reps at 70-85% of 1 RM*.[40]Including power exercises (higher velocity with moderate intensity like 40-60% 1RM) can be effective, especially when the goal is to improve ADLs.
You can progress exercises by:
- Increasing volume and intensity (sets, reps, weight)
- Changing equipment (body weight, bands, machine, free weight)
- Changing position relative to gravity
- Decreasing stability or increasing complexity (single joint & single exercise, multi-joint & single exercise, combined exercises)
Some special populations have more specific restrictions around resisted exercise. For example, for an individual with osteoporosis, consider which factors increase compressive forces through the spine, and potentially increase the risk for compression fractures. You may consider changing the position (i.e. lying or standing instead of sitting) or changing the range of motion (i.e. avoid overhead lifting and end range/combined spinal flexion/rotation/side flexion) for these individuals. Please see the special populations section or the REx Toolkit for more information.
Resistance Exercise ( Lying down / Sitting )[edit | edit source]
- To get health benefits from resistance exercises, they need to feel at least somewhat hard to do.
- Progress the weight lifted over time so that it feels like an 8 out of 10 difficulty (where O=no effort, 1 O=hardest effort you can give).
- The last repetition of each exercise should be difficult to complete. If it is easy to complete, you need to make the exercise harder by adding more weight or increasing the number of repetitions that you are doing.
- Remember to lift and lower the weight with control.
- Try to do these exercises at least 2x/week.
- Rest 1.5-3 minutes between your exercise sets to allow your muscles to recover.
- These exercises are shown with a band but your physiotherapist may modify them to use weights instead of a band.
- With resistance exercise, you should expect some muscle soreness. Taking a 2 day break between exercise sessions is a good idea.
Resistance Exercise (Standing position )[edit | edit source]
- To get health benefits from resistance exercises, they need to feel at least somewhat hard to do.
- Progress the weight lifted over time so that it feels like an 8 out of 10 difficulty (where O=no effort, 1 O=hardest effort you can give).
- The last repetition of each exercise should be difficult to complete. If it is easy to complete, you need to make the exercise harder by adding more weight or increasing the number of repetitions that you are doing.
- Remember to lift and lower the weigtht with control.
- Try to do these exercises at least 2x/week.
- Rest 1.5-3 minutes between your exercise sets to allow your muscles to recover.
- With resistance exercise, you should expect some muscle soreness. Taking a 2 day break between exercise sessions is a good idea.
Case Study and Integration into Practice[edit | edit source]
For more information on how to use and integrate this toolkit into your practice refer to the REx Toolkit
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Loveless MS, Ihm JM. Resistance exercise: how much is enough?. Current sports medicine reports. 2015 May 1;14(3):221-6.
- ↑ 2.0 2.1 Exercise prescription principles - Exercise.trekeducation.org https://exercise.trekeducation.org/2021
- ↑ American Physical Therapy Association | Choosing Wisely Choosing Wisely | Promoting conversations between providers and patients https://www.choosingwisely.org/societies/american-physical-therapy-association/
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Fragala MS, Cadore EL, Dorgo S, Izquierdo M, Kraemer WJ, Peterson MD, Ryan ED. Resistance training for older adults: position statement from the national strength and conditioning association. The Journal of Strength & Conditioning Research. 2019 Aug 1;33(8).
- ↑ Ratamess N. ACSM's foundations of strength training and conditioning. Lippincott Williams & Wilkins; 2021 Mar 15.
- ↑ Kim J, Fanola C, Ouzounian M, Hughes GC, Pyeritz RE, Gleason TG, Evangelista-Masip A, Braverman AC, Montgomery DG, Ehrlich M, Schermerhorn M. Acute Aortic Dissection in Patients With Mitral Valve Disease. Journal of the American College of Cardiology. 2020 Mar 24;75(11_Supplement_1):2255-.
- ↑ Jeevanantham D, Rajendran V, McGillis Z, Tremblay L, Larivière C, Knight A. Mobilization and exercise intervention for patients with multiple myeloma: clinical practice guidelines endorsed by the Canadian Physiotherapy Association. Physical therapy. 2021 Jan;101(1):pzaa180.
- ↑ Stiller K, Phillips A. Safety aspects of mobilising acutely ill inpatients. Physiotherapy theory and practice. 2003 Jan 1;19(4):239-57.
- ↑ 9.0 9.1 9.2 Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinková E. Sarcopenia: European consensus on definition and diagnosis Report of the European Working Group on Sarcopenia in Older PeopleA. J. Cruz-Gentoft et al. Age and ageing. 2010 Jul 1;39(4):412-23.
- ↑ 10.0 10.1 Dumitru A, Radu BM, Radu M, Cretoiu SM. Muscle changes during atrophy. Muscle Atrophy. 2018:73-92.
- ↑ 11.0 11.1 He N, Ye H. Exercise and muscle atrophy. Physical Exercise for Human Health. 2020:255-67.
- ↑ Evans WJ, Morley JE, Argilés J, Bales C, Baracos V, Guttridge D, Jatoi A, Kalantar-Zadeh K, Lochs H, Mantovani G, Marks D. Cachexia: a new definition. Clinical nutrition. 2008 Dec 1;27(6):793-9.
- ↑ Ding S, Dai Q, Huang H, Xu Y, Zhong C. An overview of muscle atrophy. Muscle Atrophy. 2018:3-19.
- ↑ Järvinen TA, Järvinen M, Kalimo H. Regeneration of injured skeletal muscle after the injury. Muscles, ligaments and tendons journal. 2013 Oct;3(4):337.
- ↑ 15.0 15.1 Kraemer WJ, Looney DP. Underlying mechanisms and physiology of muscular power. Strength & Conditioning Journal. 2012 Dec 1;34(6):13-9.
- ↑ Phillips SM. A brief review of critical processes in exercise-induced muscular hypertrophy. Sports Medicine. 2014 May;44(1):71-7.
- ↑ Khan KM, Scott A. Mechanotherapy: how physical therapists’ prescription of exercise promotes tissue repair. British journal of sports medicine. 2009 Apr 1;43(4):247-52.
- ↑ Deschenes MR. Effects of aging on muscle fibre type and size. Sports medicine. 2004 Oct;34(12):809-24.
- ↑ Schoenfeld BJ, Grgic J, Ogborn D, Krieger JW. Strength and hypertrophy adaptations between low-vs. high-load resistance training: a systematic review and meta-analysis. The Journal of Strength & Conditioning Research. 2017 Dec 1;31(12):3508-23.
- ↑ Alley DE, Shardell MD, Peters KW, McLean RR, Dam TT, Kenny AM, Fragala MS, Harris TB, Kiel DP, Guralnik JM, Ferrucci L. Grip strength cutpoints for the identification of clinically relevant weakness. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences. 2014 May 1;69(5):559-66.
- ↑ 21.0 21.1 21.2 Ribeiro AS, Nunes JP, Schoenfeld BJ. Selection of resistance exercises for older individuals: The forgotten variable. Sports Medicine. 2020 Jun;50(6):1051-7.
- ↑ Fiataraone Singh M, Hackett D, Schoenfeld B, Vincent HK, Wescott W. ACSM Guidelines for Strength Training: Resistance Training for Health. AC o. S. Medicine (Ed.). 2019.
- ↑ Scudese E, Willardson JM, Simão R, Senna G, de Salles BF, Miranda H. The effect of rest interval length on repetition consistency and perceived exertion during near maximal loaded bench press sets. The Journal of Strength & Conditioning Research. 2015 Nov 1;29(11):3079-83.
- ↑ Cheung K, Hume PA, Maxwell L. Delayed onset muscle soreness. Sports medicine. 2003 Feb;33(2):145-64.
- ↑ Tomasone JR, Flood SM, Latimer-Cheung AE, Faulkner G, Duggan M, Jones R, Lane KN, Bevington F, Carrier J, Dolf M, Doucette K. Knowledge translation of the Canadian 24-Hour Movement Guidelines for Adults aged 18–64 years and Adults aged 65 years or older: a collaborative movement guideline knowledge translation process. Applied Physiology, Nutrition, and Metabolism. 2020;45(10):S103-24.
- ↑ McLean RR, Shardell MD, Alley DE, Cawthon PM, Fragala MS, Harris TB, Kenny AM, Peters KW, Ferrucci L, Guralnik JM, Kritchevsky SB. Criteria for clinically relevant weakness and low lean mass and their longitudinal association with incident mobility impairment and mortality: the foundation for the National Institutes of Health (FNIH) sarcopenia project. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences. 2014 May 1;69(5):576-83.
- ↑ AuYoung M, Linke SE, Pagoto S, Buman MP, Craft LL, Richardson CR, Hutber A, Marcus BH, Estabrooks P, Gorin SS. Integrating physical activity in primary care practice. The American journal of medicine. 2016 Oct 1;129(10):1022-9.
- ↑ Camp PG, Reid WD, Chung F, Kirkham A, Brooks D, Goodridge D, Marciniuk DD, Hoens AM. Clinical decision-making tool for safe and effective prescription of exercise in acute exacerbations of chronic obstructive pulmonary disease: results from an interdisciplinary Delphi survey and focus groups. Physical therapy. 2015 Oct 1;95(10):1387-96.
- ↑ 29.00 29.01 29.02 29.03 29.04 29.05 29.06 29.07 29.08 29.09 29.10 Exercise is Medicine: Your Prescription for Health Series. Available from https://exerciseismedicine.org/assets/page_documents/YPH_All.pdf [Accessed 21 March 2022]
- ↑ Brown G, Brunton K, French E, Gilmore P, Gregor T, Howe JA, Kelloway L, Levy J, Matthews J, McCullough C, McNorgan C. Post Stroke Community-Based Exercise Guidelines. InINTERNATIONAL JOURNAL OF STROKE 2016 Sep 1 (Vol. 11, pp. 64-64). 1 OLIVERS YARD, 55 CITY ROAD, LONDON EC1Y 1SP, ENGLAND: SAGE PUBLICATIONS LTD.
- ↑ Eng JJ. Fitness and Mobility Exercise (FAME) program for stroke. Topics in geriatric rehabilitation. 2010;26(4):310
- ↑ 32.0 32.1 Parkinson Canada. Exercises for People with Parkinson's. Available from https://www.parkinson.ca/wp-content/uploads/Exercises_for_people_with_Parkinsons.pdf. [Accessed 21 March 2022]
- ↑ Riebe D, Ehrman JK, Liguori G, Magal M, American College of Sports Medicine, editors. ACSM's guidelines for exercise testing and prescription. Wolters Kluwer; 2018. BibTeXEndNoteRefManRefWorks
- ↑ ICORD. Exercise Guidelines for Individuals with SCI. Available from https://icord.org/2019/02/exercise-guidelines-for-individuals-with-sci/ [Accessed 21 March 2022]
- ↑ Tips for Exercising Safely When You Have Diabetes | HealthLink BC https://www.healthlinkbc.ca/illnesses-conditions/diabetes/tips-exercising-safely-when-you-have-diabetes Sep 23, 2021
- ↑ 36.0 36.1 Symptoms of Low Blood Sugar | HealthLink BC https://www.healthlinkbc.ca/illnesses-conditions/diabetes/symptoms-low-blood-sugar
- ↑ Carbohydrate Foods | HealthLink BC https://www.healthlinkbc.ca/healthy-eating-physical-activity/food-and-nutrition/nutrients/carbohydrate-foods
- ↑ Jeevanantham D, Rajendran V, McGillis Z, Tremblay L, Larivière C, Knight A. Mobilization and exercise intervention for patients with multiple myeloma: clinical practice guidelines endorsed by the Canadian Physiotherapy Association. Physical therapy. 2021 Jan;101(1):pzaa180
- ↑ Understanding How Bone Cancer Is Staged and Graded | CTCA https://www.cancercenter.com/cancer-types/bone-cancer/stages Sep 21, 2021
- ↑ Fragala MS, Cadore EL, Dorgo S, Izquierdo M, Kraemer WJ, Peterson MD, Ryan ED. Resistance training for older adults: position statement from the national strength and conditioning association. The Journal of Strength & Conditioning Research. 2019 Aug 1;33(8).