Scaphoid Fracture: Difference between revisions
Abbey Wright (talk | contribs) No edit summary |
No edit summary |
||
| (6 intermediate revisions by 2 users not shown) | |||
| Line 45: | Line 45: | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
These diagnoses can be differentiated by the location of tenderness, pain with certain maneuvers, and radiographic abnormalities.<ref name="p3" / | These diagnoses can be differentiated by the location of tenderness, pain with certain maneuvers, and radiographic abnormalities.<ref name="p3" /> | ||
* [https://physio-pedia.com/Distal_Radial_Fractures?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share Distal radius fracture] | * [https://physio-pedia.com/Distal_Radial_Fractures?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share Distal radius fracture] | ||
* Other carpal bone fractures | * Other carpal bone fractures | ||
| Line 54: | Line 54: | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Plain [[X-Rays|X-rays]] are commonly used to diagnose the fracture, but this approach may miss up to 16% of fractures in the absence of clear-cut lucent lines on plain radiographs<ref name=":2">Bäcker HC, Wu CH, Strauch RJ. [https://pubmed.ncbi.nlm.nih.gov/32025360/ Systematic Review of Diagnosis of Clinically Suspected Scaphoid Fractures]. J Wrist Surg. 2020 Feb;9(1):81-89 | Plain [[X-Rays|X-rays]] are commonly used to diagnose the fracture, but this approach may miss up to 16% of fractures in the absence of clear-cut lucent lines on plain radiographs<ref name=":2">Bäcker HC, Wu CH, Strauch RJ. [https://pubmed.ncbi.nlm.nih.gov/32025360/ Systematic Review of Diagnosis of Clinically Suspected Scaphoid Fractures]. J Wrist Surg. 2020 Feb;9(1):81-89. </ref>. Plain radiographs have 64% specificity for scaphoid fractures. | ||
Research has shown that the use of [[MRI Scans|MRI]]<nowiki/> | Research has shown that the use of [[MRI Scans|MRI]] <nowiki/>or [[CT Scans|CT]]<nowiki/>s effective in indeterminate a scaphoid fracture. Both methods have been shown to detect fractures, but the MRI found some significant ligamentous and carpal instabilities in addition to the scaphoid fracture.<ref name=":2" /><ref name="p0">Parvizi J, Wayman J, Kelly P, Moran CG. [https://pubmed.ncbi.nlm.nih.gov/9665518/ Combining the clinical signs improves diagnosis of scaphoid fractures. A prospective study with follow-up]. J Hand Surg Br. 1998 Jun;23(3):324-7. </ref><ref name=":3">Clementson, M., Björkman, A., & Thomsen, N. (2020). [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7047900/ Acute scaphoid fractures: guidelines for diagnosis and treatment.] ''EFORT open reviews'', ''5''(2), 96–103. </ref><br> | ||
== Outcome Measures == | == Outcome Measures == | ||
*[[DASH Outcome Measure|DASH]] or QuickDASH (Disabilities of Arm, Shoulder or Hand) | *[[DASH Outcome Measure|DASH]] or QuickDASH (Disabilities of Arm, Shoulder or Hand) | ||
*[https://physio-pedia.com/PRWE_Score?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share PRWE], a fifteen-item questionnaire was designed to measure wrist pain and disability.<ref name="p4">Mc Dermid, Patient Rating of Wrist Pain and Disability: A Reliable and Valid Measurement Tool, 1998.</ref> | *[https://physio-pedia.com/PRWE_Score?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share PRWE], a fifteen-item questionnaire was designed to measure wrist pain and disability.<ref name="p4">Mc Dermid, Patient Rating of Wrist Pain and Disability: A Reliable and Valid Measurement Tool, 1998.</ref> | ||
*PEM (Patient Evaluation Measure) has a simple layout with questions asked in a visual analog form. Patients are asked to read and comprehend the question alone and not the description of each interval answer.<ref name="p5" /> | *PEM ([[Patient Evaluation Measure]]) has a simple layout with questions asked in a visual analog form. Patients are asked to read and comprehend the question alone and not the description of each interval answer.<ref name="p5" /> | ||
== Assessment == | == Assessment == | ||
| Line 79: | Line 79: | ||
* Pain in the snuffbox with pronation of the wrist followed by ulnar deviation (52% percent positive predictive value, 100% percent negative predictive value)<ref name="p3" /> | * Pain in the snuffbox with pronation of the wrist followed by ulnar deviation (52% percent positive predictive value, 100% percent negative predictive value)<ref name="p3" /> | ||
{{#ev:youtube|v=ElD_Eh9fE9Q&feature=youtu.be}}<ref>Medgeeks. Scaphoid fractures - Don't miss this!. Available from: https://www.youtube.com/watch?v=ElD_Eh9fE9Q&feature=youtu.be [last accessed 02/10/2017]</ref> | |||
== Medical Management == | == Medical Management == | ||
| Line 97: | Line 98: | ||
=== Conservative management === | === Conservative management === | ||
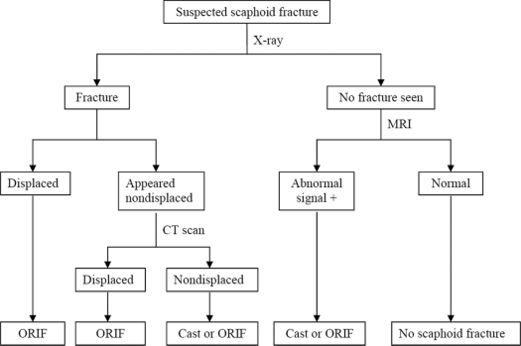
*[[File:Scaphoid fracture algorythm.jpg|thumb|521x521px|<ref>Kawamura, K., & Chung, K. C. (2008). [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4405116/ Treatment of scaphoid fractures and nonunions]. ''The Journal of hand surgery'', ''33''(6), 988–997. </ref>]]Fractures that are non-displaced and within the distal third of the bone can be managed non-operatively with immobilization in a cast. Debate exists as to whether a long or short arm cast is optimal and whether a thumb spica should be included to immobilize the thumb, no evidence currently suggests one option is better than the other. | *[[File:Scaphoid fracture algorythm.jpg|thumb|521x521px|<ref>Kawamura, K., & Chung, K. C. (2008). [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4405116/ Treatment of scaphoid fractures and nonunions]. ''The Journal of hand surgery'', ''33''(6), 988–997. </ref>]]Fractures that are non-displaced and within the distal third of the bone can be managed non-operatively with immobilization in a cast. Debate exists as to whether a long or short arm cast is optimal and whether a thumb spica should be included to immobilize the thumb, no evidence currently suggests one option is better than the other. | ||
Six weeks immobilization is normally required with repeat radiographs taken at this time to assess for the union. | |||
* The relative increase in time to healing while moving from distal to proximal is secondary to the tenuous blood supply and retrograde arterial flow.<ref name=":1" /> | Time to union varies depending on the location of the fracture. | ||
* The distal-third would be expected to heal within 6-8 weeks for approximately 90% of non-displaced or minimally displaced (≤ 0.5 mm) scaphoid waist fractures, | |||
* middle-third within 8-12 weeks | |||
* proximal third within weeks. | |||
* Scaphoid waist fractures with moderate displacement (0.5-1.5 mm) can be treated conservatively, require prolonged cast immobilization for eight to ten weeks.<ref name=":3" /> | |||
The relative increase in time to healing while moving from distal to proximal is secondary to the tenuous blood supply and retrograde arterial flow.<ref name=":1" /> | |||
As a basic rule, in a patient with a clinically suspected scaphoid fracture but negative initial radiographs, it is reasonable to apply a short arm thumb spica and re-evaluate the patient in two weeks. If a cast is not applied, the fracture can worsen over the following months. At the two-week visit, the patient should be free of pain, and a follow-up radiograph should be obtained.<ref name="p3" /> | As a basic rule, in a patient with a clinically suspected scaphoid fracture but negative initial radiographs, it is reasonable to apply a short arm thumb spica and re-evaluate the patient in two weeks. If a cast is not applied, the fracture can worsen over the following months. At the two-week visit, the patient should be free of pain, and a follow-up radiograph should be obtained.<ref name="p3" /> | ||
| Line 125: | Line 126: | ||
<br>Fractures with even small amounts of displacement are prone to nonunion, and operative treatment is recommended<ref name="p1" />. | <br>Fractures with even small amounts of displacement are prone to nonunion, and operative treatment is recommended<ref name="p1" />. | ||
For the fixation, double-threaded headless screws are preferred. Which operative technique to use depends on the fracture morphology.<ref>Schädel-Höpfner, M. | For the fixation, double-threaded headless screws are preferred. Which operative technique to use depends on the fracture morphology.<ref>Schädel-Höpfner M, Bickert B, Dumont C, Laier P, Meier R, Nusche A, Pillukat T, Rosenthal H, Schmitt R, Siemers F, Zach A, Jung M. Die frische Skaphoidfraktur : Management unter Berücksichtigung der neuen S3-Leitlinie [https://pubmed.ncbi.nlm.nih.gov/27725994/ Acute scaphoid fractures : Management under consideration of the new S3-level guideline]. Orthopade. 2016 Nov;45(11):945-950. </ref> Splinting and referral are indicated.<ref name="p3" /> | ||
Traditionally, un-displaced and stable scaphoid fractures are treated by casting in short- or long-arm casts.<ref name="p2" /><ref name="p3" /><br><br> | Traditionally, un-displaced and stable scaphoid fractures are treated by casting in short- or long-arm casts.<ref name="p2" /><ref name="p3" /><br><br> | ||
== Physiotherapy management == | == Physiotherapy management == | ||
After the period of | After the period of immobilization either post-operatively or conservatively, once the fracture is considered stable and cast removed it is likely the hand and wrist will be stiff and have reduced muscle strength. | ||
The primary goals of physiotherapy are: | The primary goals of physiotherapy are: | ||
| Line 139: | Line 140: | ||
=== ROM exercises === | === ROM exercises === | ||
ROM exercises in the initial stages after immobilization should focus on active-assisted ROM as the hand and wrist will be stiff. | ROM exercises in the initial stages after immobilization should focus on active-assisted ROM as the hand and wrist will be stiff.<i><u><ref name="p5" /></u></i> | ||
These exercises should focus on the wrist and thumb, however, the fingers, elbow and shoulder also need to be considered as after immobilization these may also be stiff. | These exercises should focus on the wrist and thumb, however, the fingers, elbow and shoulder also need to be considered as after immobilization these may also be stiff. | ||
| Line 150: | Line 151: | ||
Once a full or functional AROM has been restored it is essential to undergo [[Hand Exercises|strengthening exercises of the wrist and hand]]. | Once a full or functional AROM has been restored it is essential to undergo [[Hand Exercises|strengthening exercises of the wrist and hand]]. | ||
This is an essential step in rehabilitation as without strengthening the hand long standing functional deficits may be present and also put the patient at risk of further injury. | This is an essential step in rehabilitation as without strengthening the hand long standing functional deficits may be present and also put the patient at risk of further injury. | ||
=== Functional restoration === | |||
After full AROM has been restored and a good baseline strength has been regained focus should turn to individualized goals and tasks. | |||
The demographic of scaphoid fractures tend to be younger to middle-aged people therefore it is likely they will be active or have jobs or family to attend to. So specific rehab and exercises need to be individualized to meet these goals and expectations. Full function will eventually be restored if the fracture has been appropriately managed in the initial stages i.e. no missed avascular necrosis. | |||
< | In the sporting population it has been shown that early surgical intervention led to quicker return to play approximately 6-11 weeks versus 4-16 weeks for conservative management. <ref>Goffin JS, Liao Q, Robertson GA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6379737/# Return to sport following scaphoid fractures: A systematic review and meta-analysis]. World J Orthop. 2019 Feb 18;10(2):101-114.</ref> | ||
== Clinical Bottom Line == | |||
The scaphoid bone is the most commonly fractured carpal bone. Stress on the scaphoid, due to a forceful motion, may have a fracture as result (mostly due to a fall on an outstretched arm). | |||
The pain, which often is mild, is aggravated by pinching and gripping. Diagnoses can be differentiated by the location of tenderness, pain with certain maneuvers, and radiographic abnormalities. | |||
The length of immobilization affects negatively the outcomes. Internal fixation provided a satisfactory outcome for control of instability and early functional recovery of the wrist. There are different fractures types classified by Herbert and Fisher's system. To recognize these different fracture types, it is essential that adequate radiographs are taken of both wrists. | |||
== References == | == References == | ||
<references /> <br> | <references /> <br> | ||
[[Category:Assessment]] | [[Category:Assessment]] | ||
[[Category:Hand]] | [[Category:Hand]] | ||
[[Category:Wrist]] | [[Category:Wrist]] | ||
[[Category:Bones]] | [[Category:Bones]] | ||
[[Category:Injury]] | [[Category:Injury]] | ||
[[Category:Musculoskeletal/Orthopaedics]] | [[Category:Musculoskeletal/Orthopaedics]] | ||
[[Category: | [[Category:EIM Student Project 2]] | ||
[[Category:Primary Contact]] | [[Category:Primary Contact]] | ||
[[Category:Sports Medicine]] | [[Category:Sports Medicine]] | ||
| Line 221: | Line 187: | ||
[[Category:Bone - Conditions]] | [[Category:Bone - Conditions]] | ||
[[Category:Fractures]] | [[Category:Fractures]] | ||
[[Category:Winter Sport Injuries]] | |||
Latest revision as of 11:47, 21 February 2022
Original Editor - Dawn Waugh
Top Contributors - Dawn Waugh, Mats Vandervelde, Abbey Wright, Inoa De Pauw, Admin, Chrysolite Jyothi Kommu, Kim Jackson, Evan Thomas, Rachael Lowe, Amanda Ager, Anas Mohamed, Wanda van Niekerk, Lucinda hampton, Johnathan Fahrner, WikiSysop, 127.0.0.1, Nupur Smit Shah, Vanessa Rhule, Naike De Win and Claire Knott
Definition/ Description[edit | edit source]
The scaphoid bone is the most commonly fractured carpal bone. In young children and the elderly population, scaphoid fractures are rare. The scaphoid bone is stronger than the relatively weak distal radius in these age groups.[1][2]
A delay in diagnosis of scaphoid fractures can lead to a variety of adverse outcomes that include nonunion (no consolidation), delayed union, decreased grip strength, and range of motion, along with osteoarthritis of the radiocarpal joint. Timely diagnosis, appropriate immobilization, and referral to surgical opinion when indicated can decrease the likelihood of adverse outcomes.[3][2]
Scaphoid fractures are common, but present unique challenges because of the particular geometry of the fractures and the tenuous vascular pattern of the scaphoid. Delays in diagnosis and inadequate treatment for acute scaphoid fractures can lead to non-unions and subsequent degenerative wrist arthritis.[4]
Clinically Relevant Anatomy[edit | edit source]
The scaphoid is one of the 8 carpal bones of the wrist. It is a boat-shaped carpal bone that articulates with the distal radius, trapezium, and capitate. During the extension and radial deviation of the wrist, the movement is limited by the scaphoid conflicting with the radius.
Anatomically, the scaphoid has proximal and distal poles with a waist between the two. Blood supply to the scaphoid bone is predominantly from branches of the radial artery (dorsal carpal branch). The retrograde nature of the blood supply means that fractures at the waist of the scaphoid leave the proximal pole at a high risk of avascular necrosis.
Epidemiology[edit | edit source]
- Scaphoid fractures predominantly affect young adults, with a mean age of 29 years.
- Higher incidence in males.
- Unusual in the pediatrics population and the elderly population where the physis or distal radius, respectively, are more likely to fracture first.
- Scaphoid fractures account for 15% of acute wrist injuries.[5]
- Scaphoid fractures have a high incidence of nonunion (8-10%), frequent malunion, and late sequelae of carpal instability and post-traumatic arthritis[6].
- No blood vessels enter the proximal pole of the scaphoid, thus a higher incidence of aseptic necrosis and nonunion is noted with fractures on this side of the scaphoid [6].
- Displaced fractures frequently are associated with ligamentus tears in the wrist.[6]
Characteristics/ Clinical Presentation[edit | edit source]
Patients typically present with wrist pain following a fall onto an outstretched hand.
- Axial loading of the wrist with it in forced hyperextension and radial deviation can cause the fracture as the scaphoid impacts on the dorsal rim of the radius.
- Traumatic injury through contact sports and road traffic accidents are also common causes.[5]
Following the traumatic event there will be a massive force of the hand on the arm through the scaphoid bone[1][2][7].
The symptoms will likely be:
- Deep, dull ache in the radial part of the wrist.
- Aggravated pain by pinching and gripping.
- Localised wrist swelling with fullness in the anatomical snuffbox
- Localised bruising
- Tenderness on palpation of the radial side of the wrist
Differential Diagnosis[edit | edit source]
These diagnoses can be differentiated by the location of tenderness, pain with certain maneuvers, and radiographic abnormalities.[2]
- Distal radius fracture
- Other carpal bone fractures
- Scapholunate dissociation
- De Quervain’s tenosynovitis
- Osteoarthritis
- Tendinopathy[5]
Diagnostic Procedures[edit | edit source]
Plain X-rays are commonly used to diagnose the fracture, but this approach may miss up to 16% of fractures in the absence of clear-cut lucent lines on plain radiographs[8]. Plain radiographs have 64% specificity for scaphoid fractures.
Research has shown that the use of MRI or CTs effective in indeterminate a scaphoid fracture. Both methods have been shown to detect fractures, but the MRI found some significant ligamentous and carpal instabilities in addition to the scaphoid fracture.[8][9][10]
Outcome Measures[edit | edit source]
- DASH or QuickDASH (Disabilities of Arm, Shoulder or Hand)
- PRWE, a fifteen-item questionnaire was designed to measure wrist pain and disability.[7]
- PEM (Patient Evaluation Measure) has a simple layout with questions asked in a visual analog form. Patients are asked to read and comprehend the question alone and not the description of each interval answer.[6]
Assessment[edit | edit source]
Subjective assessment[edit | edit source]
- History of trauma i.e. fall onto an outstretched hand
- Dull pain which is aggravated by hand and wrist movements
- Restricted thumb range of movement[4]
Objective exam[edit | edit source]
When examining a patient with a suspected scaphoid injury, it is important to compare the injured wrist with the uninjured wrist.
Presentation may include:
- Anatomical snuffbox tenderness on examination - highly sensitive 90% indication of scaphoid fracture, but it is nonspecific 40%[1]
- Tenderness of the scaphoid tubercle: the physician extends the patient’s wrist with one hand and applies pressure to the tuberosity at the proximal wrist crease with the opposite hand. This provides better diagnostic information; sensitivity 87%, specificity 57%[1]
- Pain with the scaphoid compression test (i.e. axially/longitudinally compressing a patient’s thumb along the line of the first metacarpal) was shown to be helpful in identifying a scaphoid fracture, but in another study[3][2],
- Pain in the snuffbox with pronation of the wrist followed by ulnar deviation (52% percent positive predictive value, 100% percent negative predictive value)[2]
Medical Management[edit | edit source]
Suspected fractures with positive clinical findings on examination but negative radiographs should have a follow-up with films repeated in 7-14 days. If pain persists and radiographs are still normal, then further imaging in the form of MRI or CT should be undertaken. Pain management with the assistance of pharmacists should be considered.
Surgical Management[edit | edit source]
Indications for operative management include:
- Displacement greater than 1mm
- An intrascaphoid angle greater than 35 degrees (humpback deformity)
- A radiolunate angle of more than 15 degrees
- Transcaphoid perilunate dislocation
- Proximal pole fractures
- Comminuted fractures
- Non displaced waist fractures in individuals that need to return quickly to work/sport
- Nonunion or avascular necrosis
Surgical fixation involves the insertion of a single or multiple screws and can be done percutaneously or via an open procedure. The latter is preferable for non-unions and those fractures that exhibit gross displacement with the former for acute, minimally displaced fractures[5].
Conservative management[edit | edit source]
- Fractures that are non-displaced and within the distal third of the bone can be managed non-operatively with immobilization in a cast. Debate exists as to whether a long or short arm cast is optimal and whether a thumb spica should be included to immobilize the thumb, no evidence currently suggests one option is better than the other.
Six weeks immobilization is normally required with repeat radiographs taken at this time to assess for the union.
Time to union varies depending on the location of the fracture.
- The distal-third would be expected to heal within 6-8 weeks for approximately 90% of non-displaced or minimally displaced (≤ 0.5 mm) scaphoid waist fractures,
- middle-third within 8-12 weeks
- proximal third within weeks.
- Scaphoid waist fractures with moderate displacement (0.5-1.5 mm) can be treated conservatively, require prolonged cast immobilization for eight to ten weeks.[10]
The relative increase in time to healing while moving from distal to proximal is secondary to the tenuous blood supply and retrograde arterial flow.[5]
As a basic rule, in a patient with a clinically suspected scaphoid fracture but negative initial radiographs, it is reasonable to apply a short arm thumb spica and re-evaluate the patient in two weeks. If a cast is not applied, the fracture can worsen over the following months. At the two-week visit, the patient should be free of pain, and a follow-up radiograph should be obtained.[2]
Types of fracture[edit | edit source]
The fractured scaphoid exhibits certain behavior that inhibits healing. Fracture fragments are inherently unstable and prone to displacement and require motionless contact to achieve union.[6] As mentioned before, the blood supply of the scaphoid is tenuous.
For therapeutic decision making, the scaphoid is divided into three anatomic sections: proximal, medial, and distal (see image). Fractures are further subdivided into displaced and non-displaced types.[2]
Non-displaced Fractures[edit | edit source]
Non-displaced distal fractures heal well with strict immobilization in a well-molded short arm thumb spica. Controversy exists over whether to use a long arm or a short arm cast. he current treatment for this type of fracture is a thumb spica, but some evidence suggests that the thumb could be omitted from the cast.[13]
Screw fixation may speed recovery to pre-injury activities; referral for surgery may be indicated, depending on the needs of the patient[9].
As the fracture line moves proximally, there is more risk of displacement and nonunion; therefore, it would be appropriate to refer these patients for orthopedic consultation. If conservative treatment is attempted, a long arm cast with thumb immobilization is appropriate.[2][14]
Displaced Fractures[edit | edit source]
Fractures with even small amounts of displacement are prone to nonunion, and operative treatment is recommended[1].
For the fixation, double-threaded headless screws are preferred. Which operative technique to use depends on the fracture morphology.[15] Splinting and referral are indicated.[2]
Traditionally, un-displaced and stable scaphoid fractures are treated by casting in short- or long-arm casts.[3][2]
Physiotherapy management[edit | edit source]
After the period of immobilization either post-operatively or conservatively, once the fracture is considered stable and cast removed it is likely the hand and wrist will be stiff and have reduced muscle strength.
The primary goals of physiotherapy are:
- Restore active range of movement (AROM)
- Reduce swelling
- Increase grip and wrist strength
- Return to functional goals and tasks
ROM exercises[edit | edit source]
ROM exercises in the initial stages after immobilization should focus on active-assisted ROM as the hand and wrist will be stiff.[6]
These exercises should focus on the wrist and thumb, however, the fingers, elbow and shoulder also need to be considered as after immobilization these may also be stiff.
If full ROM is still restricted it may be useful in the therapy session to do manual therapy in the form of joint mobilisations to the radio-carpal joint, radio-ulnar joint and potentially to the carpal joints.
Other forms of manual therapy may also be helpful to reduce any residual swelling or pain such as soft tissue work or massage techniques.
Strengthening exercises[edit | edit source]
Once a full or functional AROM has been restored it is essential to undergo strengthening exercises of the wrist and hand.
This is an essential step in rehabilitation as without strengthening the hand long standing functional deficits may be present and also put the patient at risk of further injury.
Functional restoration[edit | edit source]
After full AROM has been restored and a good baseline strength has been regained focus should turn to individualized goals and tasks.
The demographic of scaphoid fractures tend to be younger to middle-aged people therefore it is likely they will be active or have jobs or family to attend to. So specific rehab and exercises need to be individualized to meet these goals and expectations. Full function will eventually be restored if the fracture has been appropriately managed in the initial stages i.e. no missed avascular necrosis.
In the sporting population it has been shown that early surgical intervention led to quicker return to play approximately 6-11 weeks versus 4-16 weeks for conservative management. [16]
Clinical Bottom Line[edit | edit source]
The scaphoid bone is the most commonly fractured carpal bone. Stress on the scaphoid, due to a forceful motion, may have a fracture as result (mostly due to a fall on an outstretched arm).
The pain, which often is mild, is aggravated by pinching and gripping. Diagnoses can be differentiated by the location of tenderness, pain with certain maneuvers, and radiographic abnormalities.
The length of immobilization affects negatively the outcomes. Internal fixation provided a satisfactory outcome for control of instability and early functional recovery of the wrist. There are different fractures types classified by Herbert and Fisher's system. To recognize these different fracture types, it is essential that adequate radiographs are taken of both wrists.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Gutierrez G, Office management of scaphoid fractures. Phys Sports Med. 1996;24:60–70.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 T. Grant Phillips et al, Diagnosis and Management of Scaphoid Fractures, Am Fam Physician. 2004 Sep 1;70(5):879-884.
- ↑ 3.0 3.1 3.2 Greene WB, Essentials of musculoskeletal care. 2d ed. Rosemont, Ill.: American Academy of Orthopaedic Surgeons, 2001:252–4.
- ↑ 4.0 4.1 Kawamura,K. & Chung, C.C. (2008). Treatment of Scaphoid Fractures and Nonunions. J Hand Surg Am. 2008 Jul-Aug; 33(6): 988–997. doi: 10.1016/j.jhsa.2008.04.026
- ↑ 5.0 5.1 5.2 5.3 5.4 Hayat Z, Varacallo M. Scaphoid Wrist Fracture. InStatPearls [Internet] 2019 Jan 4. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK536907/ (last accessed 23.3.2020)
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Scott R. Laker et al, Scaphoid injury (Epidemiology), Medscape. 2019.
- ↑ 7.0 7.1 Mc Dermid, Patient Rating of Wrist Pain and Disability: A Reliable and Valid Measurement Tool, 1998.
- ↑ 8.0 8.1 Bäcker HC, Wu CH, Strauch RJ. Systematic Review of Diagnosis of Clinically Suspected Scaphoid Fractures. J Wrist Surg. 2020 Feb;9(1):81-89.
- ↑ 9.0 9.1 Parvizi J, Wayman J, Kelly P, Moran CG. Combining the clinical signs improves diagnosis of scaphoid fractures. A prospective study with follow-up. J Hand Surg Br. 1998 Jun;23(3):324-7.
- ↑ 10.0 10.1 Clementson, M., Björkman, A., & Thomsen, N. (2020). Acute scaphoid fractures: guidelines for diagnosis and treatment. EFORT open reviews, 5(2), 96–103.
- ↑ Medgeeks. Scaphoid fractures - Don't miss this!. Available from: https://www.youtube.com/watch?v=ElD_Eh9fE9Q&feature=youtu.be [last accessed 02/10/2017]
- ↑ Kawamura, K., & Chung, K. C. (2008). Treatment of scaphoid fractures and nonunions. The Journal of hand surgery, 33(6), 988–997.
- ↑ Fowler, C., Sullivan, B., Williams, L. et al. A comparison of bone scintigraphy and MRI in the early diagnosis of the occult scaphoid waist fracture. Skeletal Radiol 27, 683–687 (1998).
- ↑ Grewal R, Suh N, MacDermid JC. Is Casting for Non-Displaced Simple Scaphoid Waist Fracture Effective? A CT Based Assessment of Union. Open Orthop J. 2016 Sep 15;10:431-438.
- ↑ Schädel-Höpfner M, Bickert B, Dumont C, Laier P, Meier R, Nusche A, Pillukat T, Rosenthal H, Schmitt R, Siemers F, Zach A, Jung M. Die frische Skaphoidfraktur : Management unter Berücksichtigung der neuen S3-Leitlinie Acute scaphoid fractures : Management under consideration of the new S3-level guideline. Orthopade. 2016 Nov;45(11):945-950.
- ↑ Goffin JS, Liao Q, Robertson GA. Return to sport following scaphoid fractures: A systematic review and meta-analysis. World J Orthop. 2019 Feb 18;10(2):101-114.