Spinal Manipulation: Difference between revisions
No edit summary |
No edit summary |
||
| Line 9: | Line 9: | ||
It is a intervention Physiotherapists have been employing since the beginning of physical therapy practice. However, physiotherapists providing spinal manipulations have come under the scrutiny of other professions even though manipulation is not exclusive to any one domain or profession. The APTA has created a page that delineates the difference between physical therapy manipulation and chiropractic manipulation<ref>APTA. [http://www.apta.org/StateIssues/Manipulation/ Manipulation/Mobilisation]. Available online at http://www.apta.org/StateIssues/Manipulation/</ref>. They have also published a manipulation education manual<ref>APTA. [http://www.apta.org/uploadedFiles/APTAorg/Educators/Curriculum_Resources/APTA/Manipulation/ManipulationEducationManual.pdf Manipulation fckLREducation Manual fckLRFor Physical Therapist fckLRProfessional Degree Programs]. Available online at http://www.apta.org/uploadedFiles/APTAorg/Educators/Curriculum_Resources/APTA/Manipulation/ManipulationEducationManual.pdf</ref>. | It is a intervention Physiotherapists have been employing since the beginning of physical therapy practice. However, physiotherapists providing spinal manipulations have come under the scrutiny of other professions even though manipulation is not exclusive to any one domain or profession. The APTA has created a page that delineates the difference between physical therapy manipulation and chiropractic manipulation<ref>APTA. [http://www.apta.org/StateIssues/Manipulation/ Manipulation/Mobilisation]. Available online at http://www.apta.org/StateIssues/Manipulation/</ref>. They have also published a manipulation education manual<ref>APTA. [http://www.apta.org/uploadedFiles/APTAorg/Educators/Curriculum_Resources/APTA/Manipulation/ManipulationEducationManual.pdf Manipulation fckLREducation Manual fckLRFor Physical Therapist fckLRProfessional Degree Programs]. Available online at http://www.apta.org/uploadedFiles/APTAorg/Educators/Curriculum_Resources/APTA/Manipulation/ManipulationEducationManual.pdf</ref>. | ||
== Clinical Prediction Rule for Manipulation == | == Clinical Prediction Rule for Manipulation == | ||
Criteria included in the five factor predictor rule for manipulation<ref>1. Fritz, Julie M. PT, PhD, ATC, Cleland, Joshua A. PT, PhD, OCS, FAAOMPT, and Childs, John D. PT, PhD, MBA, OCS, FAAOMPT, “Subgrouping Patients With Low Back Pain: Evolution of a Classification Approach to Physical Therapy,” Journal of Orthop Sports Physical Therapy 37, no. 6 (June 2007): 290-302.</ref> : | The patients that received the most benefit from spinal manipulation for LBP are those that meet at least four out of the five criteria for spinal manipulation.<ref name="Flynn-CPR">Flynn T, Fritz J, Whitman J, et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine. 2002;27(24):2835-2843.</ref>Criteria included in the five factor predictor rule for manipulation<ref>1. Fritz, Julie M. PT, PhD, ATC, Cleland, Joshua A. PT, PhD, OCS, FAAOMPT, and Childs, John D. PT, PhD, MBA, OCS, FAAOMPT, “Subgrouping Patients With Low Back Pain: Evolution of a Classification Approach to Physical Therapy,” Journal of Orthop Sports Physical Therapy 37, no. 6 (June 2007): 290-302.</ref> : | ||
# Pain lasting less than 16 days | # Pain lasting less than 16 days | ||
| Line 30: | Line 18: | ||
# Internal Rotation of greater than 35 degrees for at least one hip | # Internal Rotation of greater than 35 degrees for at least one hip | ||
# Hypomobility of a least one level of the lumbar spine | # Hypomobility of a least one level of the lumbar spine | ||
Two most important identifiers for manipulation are: Pain lasting less than 16 days; No symptoms distal to the knee<ref name="2 Predictors">Fritz JM, Brennan GP, Leaman H. Does the evidence for spinal manipulation translate into better outcomes in routine clinical care for patients with occupational low back pain? A case-control study. Spine J. 2006;6(3):289-295.</ref> | |||
The following six factors are the criteria for immediate responders to cervical manipulation:<ref name=":0">Tseng Y, Wang W, Chen W, Hou T, Chen T, Lieu F. Predictors for the immediate responders to cervical manipulation in patients with neck pain. Manual Therapy. 2006;11(4):306-315.</ref> | The following six factors are the criteria for immediate responders to cervical manipulation:<ref name=":0">Tseng Y, Wang W, Chen W, Hou T, Chen T, Lieu F. Predictors for the immediate responders to cervical manipulation in patients with neck pain. Manual Therapy. 2006;11(4):306-315.</ref> | ||
| Line 43: | Line 27: | ||
# Feeling better while moving the neck | # Feeling better while moving the neck | ||
# Without feeling worse while extending the neck | # Without feeling worse while extending the neck | ||
# Diagnosis of [[Cervical Spondylosis|Spondylosis]] without Radiculopathy | # Diagnosis of [[Cervical Spondylosis|Spondylosis]] without [[Radiculopathy]] | ||
The presence of four or more of these predictors increased the probability of success with manipulation to 89%<ref name=":0" />. | The presence of four or more of these predictors increased the probability of success with manipulation to 89%<ref name=":0" />. | ||
| Line 53: | Line 37: | ||
Spinal Manipulation: What You Need To Know Available: https://www.nccih.nih.gov/health/spinal-manipulation-what-you-need-to-know (accessed 13.6.2021)</ref> | Spinal Manipulation: What You Need To Know Available: https://www.nccih.nih.gov/health/spinal-manipulation-what-you-need-to-know (accessed 13.6.2021)</ref> | ||
* The NICE guidelines <ref name=":1">Neck pain - non-specific - NICE CKS [Internet]. Cks.nice.org.uk. 2018 [cited 20 May 2020]. Available from: <nowiki>https://cks.nice.org.uk/neck-pain-non-specific#!scenario</nowiki></ref> recommend the use of thoracic spinal manipulation in conjunction with range of movement and strengthening exercises to help relieve neck pain. Their recommendation is based on the American Physical Therapy Association guidelines | * The NICE guidelines <ref name=":1">Neck pain - non-specific - NICE CKS [Internet]. Cks.nice.org.uk. 2018 [cited 20 May 2020]. Available from: <nowiki>https://cks.nice.org.uk/neck-pain-non-specific#!scenario</nowiki></ref> recommend the use of thoracic spinal manipulation in conjunction with range of movement and strengthening exercises to help relieve neck pain. Their recommendation is based on the American Physical Therapy Association guidelines that <ref>Blanpied, R., Gross, R., Elliot, J., Devaney, L., Clewley, D., Walton, D., Spark, C., Robertson, E., Altman, R., Beattie, P., et al. (2017) Neck Pain: Revision 2017. '''Journal of Orthopaedic and Sports Physical Therapy''' [online] Available at: https://www.jospt.org/doi/10.2519/jospt.2017.0302 [Accessed 23 May 2020]</ref> states "For patients with acute neck pain with mobility deficits, there was a benefit compared to control for using multiple sessions of thoracic manipulation for reducing pain over the immediate and short term". | ||
For Headache | For Headache | ||
* For preventing migraines, spinal manipulation may be one of several complementary health approaches (including massage therapy) that’s as helpful as medications used for migraine prevention, but the research isn’t conclusive. | * For preventing [[Migraine Headache|migraines]], spinal manipulation may be one of several complementary health approaches (including massage therapy) that’s as helpful as medications used for migraine prevention, but the research isn’t conclusive. | ||
* A systematic review of noninvasive nonpharmacologic treatment for chronic pain reported spinal manipulation therapy was associated with slight to moderate improvements in function compared to usual care on the Headache Impact Test and the Headache Disability Inventory (scale 0-100) and in pain over the short term (i.e., 1-6 months) in one trial. The standard of evidence was rated as low<ref name=":2" />. | * A systematic review of noninvasive nonpharmacologic treatment for [[Chronic Pain and the Brain|chronic pain]] reported spinal manipulation therapy was associated with slight to moderate improvements in function compared to usual care on the Headache Impact Test and the Headache Disability Inventory (scale 0-100) and in pain over the short term (i.e., 1-6 months) in one trial. The standard of evidence was rated as low<ref name=":2" />. | ||
Cervical spine SMT has been linked to small, potentially dangerous tears in the artery walls in the neck ie [[Cervical Arterial Dysfunction|cervical artery dissections]] (CAD). These tears are rare but can lead to a [[stroke]]. Any kind of sudden neck movement eg playing sports, getting whiplash may also increase the risk of tears. The available evidence suggests that the incidence of CAD in people getting spinal manipulation is low, but patients need to be informed of this potential risk.{{#ev:youtube|tNoE8dPZrCg}} | Cervical spine SMT has been linked to small, potentially dangerous tears in the artery walls in the neck ie [[Cervical Arterial Dysfunction|cervical artery dissections]] (CAD). These tears are rare but can lead to a [[stroke]]. Any kind of sudden neck movement eg playing sports, getting [[Whiplash Associated Disorders|whiplash]] may also increase the risk of tears. The available evidence suggests that the incidence of CAD in people getting spinal manipulation is low, but patients need to be informed of this potential risk.{{#ev:youtube|tNoE8dPZrCg}} | ||
== Thoracic Spine == | == Thoracic Spine == | ||
[[File:Thoracic manip.JPG|right|frameless]] | [[File:Thoracic manip.JPG|right|frameless]] | ||
The thoracic region encompasses the verterbrae T1-T12, and is located in the middle region or thorax of the body. Unlike other areas of the spine, each of the vertebrae present has a rib attached to it, resulting in the the thoracic cage being attached to the Thoracic region of the spine. There is minimal evidence surrounding the use of thoracic manipulations for the relief of thoracic pain, but there is evidence for use in relief of neck pain and increasing respiratory function. | The [[Thoracic Back Pain|thoracic]] region encompasses the verterbrae T1-T12, and is located in the middle region or thorax of the body. Unlike other areas of the spine, each of the [[Thoracic Anatomy|vertebrae]] present has a [[Ribs|rib]] attached to it, resulting in the the thoracic cage being attached to the Thoracic region of the spine. There is minimal evidence surrounding the use of thoracic manipulations for the relief of thoracic pain, but there is evidence for use in relief of neck pain and increasing [[Respiratory Assessment|respiratory]] function. | ||
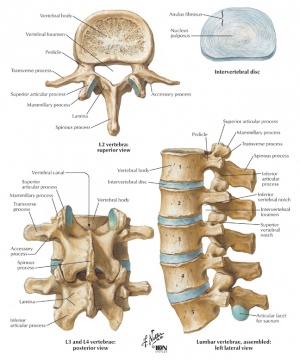
== Lumbar Spine == | == Lumbar Spine == | ||
[[File:Lumbar vertebra.jpg|right|frameless]] | [[File:Lumbar vertebra.jpg|right|frameless]] | ||
Spinal manipulation to the lumbar spine is a common intervention administered for patients with Low Back Pain (LBP). Many noninvasive treatments are available for low-back pain, and these include drugs and nondrug options. In its 2017 clinical guidelines, the American College of Physicians (ACP) suggests that spinal manipulation is one of a number of therapeutic options that may help people with acute or chronic low-back pain (although the ACP says the quality of the evidence is low). <ref>Coronado. R, Gay. C, Bialosky. J, Carnaby. G, Bishop. M and George. S (2012) Changes in Pain sensitivity following spinal manipulation: a systematic review and meta-analysis. '''Journal of Electromyography and Kinesiology.''' 22(5): 752-767</ref> The research on spinal manipulation for acute low-back pain is generally mixed and has many limitations. | Spinal manipulation to the [[Lumbar Anatomy|lumbar]] spine is a common intervention administered for patients with Low Back Pain (LBP). Many noninvasive treatments are available for low-back pain, and these include drugs and nondrug options. In its 2017 clinical guidelines, the American College of Physicians (ACP) suggests that spinal manipulation is one of a number of therapeutic options that may help people with acute or chronic low-back pain (although the ACP says the quality of the evidence is low). <ref>Coronado. R, Gay. C, Bialosky. J, Carnaby. G, Bishop. M and George. S (2012) Changes in Pain sensitivity following spinal manipulation: a systematic review and meta-analysis. '''Journal of Electromyography and Kinesiology.''' 22(5): 752-767</ref> The research on spinal manipulation for acute low-back pain is generally mixed and has many limitations. | ||
* Spinal manipulation is no more effective for acute low-back pain than sham (fake) spinal manipulation, or when added to another treatment such as standard medical care, a 2012 research review of 20 studies found. Spinal manipulation appeared to be safe when compared to other treatment options. | * Spinal manipulation is no more effective for acute low-back pain than sham (fake) spinal manipulation, or when added to another treatment such as standard medical care, a 2012 research review of 20 studies found. Spinal manipulation appeared to be safe when compared to other treatment options. | ||
* A 2017 analysis examined data from 15 randomized controlled trials with almost 1,700 participants. The researchers concluded that spinal manipulative therapy can modestly improve pain and function in people with acute low-back pain<ref name=":2" />. | * A 2017 analysis examined data from 15 randomized controlled trials with almost 1,700 participants. The researchers concluded that spinal manipulative therapy can modestly improve pain and function in people with acute low-back pain<ref name=":2" />. | ||
The best way of using the manipulations is in combination with other therapeutic modalities. There is evidence from a high quality study, that spinal manipulative therapy combined with exercise is more effective than other procedures like spinal manipulation, exercise or physician consultation alone<ref>Rajadurai V, Murugan K. [http://www.ingentaconnect.com/content/maney/ptr/2009/00000014/00000004/art00006 Spinal manipulative therapy for low back pain: A systematic review]. Physical Therapy Reviews. 2009;14;4;260-271.</ref>. A clinical prediction rule was developed in order to identify these patients with LBP who will most likely benefit from spinal manipulation. Spinal manipulation is a sub-group of the [[Treatment_Based_Classification_Approach_to_Low_Back_Pain|Treatment-Based Classification Approach for low back pain]].<ref name="NICE">National Institute of Clinical Excellence. [http://publications.nice.org.uk/low-back-pain-cg88 Low back pain: Early management of persistent non-specific low back pain], May 2009</ref>. | == The best way of using the manipulations is in combination with other therapeutic modalities. == | ||
* There is evidence from a high quality study, that spinal manipulative therapy combined with exercise is more effective than other procedures like spinal manipulation, exercise or physician consultation alone<ref>Rajadurai V, Murugan K. [http://www.ingentaconnect.com/content/maney/ptr/2009/00000014/00000004/art00006 Spinal manipulative therapy for low back pain: A systematic review]. Physical Therapy Reviews. 2009;14;4;260-271.</ref>. | |||
* A clinical prediction rule was developed in order to identify these patients with LBP who will most likely benefit from spinal manipulation. | |||
* Spinal manipulation is a sub-group of the [[Treatment_Based_Classification_Approach_to_Low_Back_Pain|Treatment-Based Classification Approach for low back pain]].<ref name="NICE">National Institute of Clinical Excellence. [http://publications.nice.org.uk/low-back-pain-cg88 Low back pain: Early management of persistent non-specific low back pain], May 2009</ref>. | |||
== Contra-indications== | == Contra-indications== | ||
| Line 81: | Line 67: | ||
The following scenarios are contraindications to low back pain<ref name="Gibbons">Gibbons P., Tehan P. Patient positioning and spinal locking for lumbar spine rotation manipulation. Manual Therapy. 2001;6;3;130±138.</ref> : | The following scenarios are contraindications to low back pain<ref name="Gibbons">Gibbons P., Tehan P. Patient positioning and spinal locking for lumbar spine rotation manipulation. Manual Therapy. 2001;6;3;130±138.</ref> : | ||
*Any pathology that leads to significant bone weakening | *Any pathology that leads to significant bone weakening | ||
*Neurological: cord compression, [[Cauda Equina Syndrome|cauda equina]] compression, nerve root compression with increasing neurological deficit | *[[Neurological Assessment|Neurological]]: cord compression, [[Cauda Equina Syndrome|cauda equina]] compression, nerve root compression with increasing neurological deficit | ||
*Vascular: aortic aneurysm, bleeding into joints | *Vascular: aortic aneurysm, bleeding into joints | ||
*Lack of diagnosis | *Lack of diagnosis | ||
| Line 87: | Line 73: | ||
== Other Conditions == | == Other Conditions == | ||
A 2021 systematic review found no evidence of an effect of SMT for the management of non-musculoskeletal disorders including infantile colic, childhood asthma, hypertension, primary dysmenorrhea, and migraine. This finding challenges the validity of the theory that treating spinal dysfunctions with SMT has a physiological effect on organs and their function.<ref>Côté P, Hartvigsen J, Axén I, Leboeuf-Yde C, Corso M, Shearer H, Wong J, Marchand AA, Cassidy JD, French S, Kawchuk GN. T[https://chiromt.biomedcentral.com/articles/10.1186/s12998-021-00362-9 he global summit on the efficacy and effectiveness of spinal manipulative therapy for the prevention and treatment of non-musculoskeletal disorders: a systematic review of the literature.] Chiropractic & manual therapies. 2021 Dec;29(1):1-23.Available: https://chiromt.biomedcentral.com/articles/10.1186/s12998-021-00362-9<nowiki/>(accessed 13.6.2021)</ref> | A 2021 systematic review found no evidence of an effect of SMT for the management of non-musculoskeletal disorders including infantile colic, childhood [[asthma]], [[hypertension]], primary dysmenorrhea, and migraine. This finding challenges the validity of the theory that treating spinal dysfunctions with SMT has a physiological effect on organs and their function.<ref>Côté P, Hartvigsen J, Axén I, Leboeuf-Yde C, Corso M, Shearer H, Wong J, Marchand AA, Cassidy JD, French S, Kawchuk GN. T[https://chiromt.biomedcentral.com/articles/10.1186/s12998-021-00362-9 he global summit on the efficacy and effectiveness of spinal manipulative therapy for the prevention and treatment of non-musculoskeletal disorders: a systematic review of the literature.] Chiropractic & manual therapies. 2021 Dec;29(1):1-23.Available: https://chiromt.biomedcentral.com/articles/10.1186/s12998-021-00362-9<nowiki/>(accessed 13.6.2021)</ref> | ||
Researchers have studied spinal manipulation for many other conditions, including [[fibromyalgia]], children’s ear infections, chronic obstructive pulmonary disease ([[COPD (Chronic Obstructive Pulmonary Disease)|COPD]]), infant colic, and bedwetting, but there’s too little evidence to know if it helps with these problems.<ref name=":2" /> | |||
== Neurophysiological Effects == | |||
↵An experimental body of evidence exists indicating that spinal manipulation impacts primary afferent neurons from paraspinal tissues, the motor control system and pain processing. Biomechanical changes caused by spinal manipulation are thought to have physiological consequences by means of their effects on the inflow of sensory information to the central nervous system | |||
* [[Muscle spindles|Muscle spindle]] afferents and [[Golgi Tendon Organ|Golgi tendon organ]] afferents are stimulated by spinal manipulation. | |||
* Smaller-diameter sensory nerve fibers are likely activated, although this has not been demonstrated directly. | |||
* Mechanical and chemical changes in the intervertebral foramen caused by a herniated [[intervertebral disc]] can affect the dorsal roots and dorsal root ganglia, but it is not known if spinal manipulation directly affects these changes. | |||
* Individuals with [[Disc Herniation|herniated]] lumbar discs have shown clinical improvement in response to spinal manipulation. | |||
* The phenomenon of central facilitation is known to increase the receptive field of central [[Neurone|neurons]], enabling either subthreshold or innocuous stimuli access to central pain pathways. One mechanism underlying the effects of spinal manipulation may be the manipulation's ability to alter central sensory processing by removing subthreshold mechanical or chemical stimuli from paraspinal tissues. | |||
* Spinal manipulation is also thought to affect reflex neural outputs to both muscle and visceral organs. Substantial evidence demonstrates that spinal manipulation evokes paraspinal muscle reflexes and alters [[Motor Neurone|motoneuron]] excitability. <ref /> | |||
== Key Evidence == | == Key Evidence == | ||
Revision as of 07:06, 13 June 2021
Original Editor - Stacey Jones and Ashley Gunzenhauser. Top Contributors - Admin, Stacey Jones, Ashley Gunzenhauser, Christian Stamou, Eric Robertson, Lucinda hampton, Alistair Husband, Kim Jackson, Rachael Lowe, Rob Dent, Dana Tew, Vidya Acharya, Mariam Hashem, WikiSysop, Anke Jughters, Lisa Pernet, Tarina van der Stockt, Kai A. Sigel and 127.0.0.1
Description[edit | edit source]
Spinal Manipulation Therapy (SMT) is a technique that treats back pain, neck pain and other musculoskeletal conditions via the application of force to the spinal joints, with the idea being that such treatment of dysfunctional areas in the spine can restore the spine’s structural integrity, reduce pain and initiate the body’s natural healing processes[1].
It is a intervention Physiotherapists have been employing since the beginning of physical therapy practice. However, physiotherapists providing spinal manipulations have come under the scrutiny of other professions even though manipulation is not exclusive to any one domain or profession. The APTA has created a page that delineates the difference between physical therapy manipulation and chiropractic manipulation[2]. They have also published a manipulation education manual[3].
Clinical Prediction Rule for Manipulation[edit | edit source]
The patients that received the most benefit from spinal manipulation for LBP are those that meet at least four out of the five criteria for spinal manipulation.[4]Criteria included in the five factor predictor rule for manipulation[5] :
- Pain lasting less than 16 days
- No symptoms distal to the knee
- FABQ score less than 19
- Internal Rotation of greater than 35 degrees for at least one hip
- Hypomobility of a least one level of the lumbar spine
Two most important identifiers for manipulation are: Pain lasting less than 16 days; No symptoms distal to the knee[6]
The following six factors are the criteria for immediate responders to cervical manipulation:[7]
- Initial scores on Neck Disability Index <11.50
- Having bilateral involvement pattern
- Not performing sedentary work >5 h/day
- Feeling better while moving the neck
- Without feeling worse while extending the neck
- Diagnosis of Spondylosis without Radiculopathy
The presence of four or more of these predictors increased the probability of success with manipulation to 89%[7].
Cervical Spine[edit | edit source]
For patients with acute neck pain, either spinal manipulation or home exercises appeared to be more effective than medication in the short and long term, an NCCIH-funded study of 272 patients showed in 2012. A 2015 research review that looked at results from 51 trials with 2,920 participants also reported that there’s weak evidence that spinal manipulation may provide short-term relief from acute or chronic neck pain.[8]
- The NICE guidelines [9] recommend the use of thoracic spinal manipulation in conjunction with range of movement and strengthening exercises to help relieve neck pain. Their recommendation is based on the American Physical Therapy Association guidelines that [10] states "For patients with acute neck pain with mobility deficits, there was a benefit compared to control for using multiple sessions of thoracic manipulation for reducing pain over the immediate and short term".
For Headache
- For preventing migraines, spinal manipulation may be one of several complementary health approaches (including massage therapy) that’s as helpful as medications used for migraine prevention, but the research isn’t conclusive.
- A systematic review of noninvasive nonpharmacologic treatment for chronic pain reported spinal manipulation therapy was associated with slight to moderate improvements in function compared to usual care on the Headache Impact Test and the Headache Disability Inventory (scale 0-100) and in pain over the short term (i.e., 1-6 months) in one trial. The standard of evidence was rated as low[8].
Cervical spine SMT has been linked to small, potentially dangerous tears in the artery walls in the neck ie cervical artery dissections (CAD). These tears are rare but can lead to a stroke. Any kind of sudden neck movement eg playing sports, getting whiplash may also increase the risk of tears. The available evidence suggests that the incidence of CAD in people getting spinal manipulation is low, but patients need to be informed of this potential risk.
Thoracic Spine[edit | edit source]
The thoracic region encompasses the verterbrae T1-T12, and is located in the middle region or thorax of the body. Unlike other areas of the spine, each of the vertebrae present has a rib attached to it, resulting in the the thoracic cage being attached to the Thoracic region of the spine. There is minimal evidence surrounding the use of thoracic manipulations for the relief of thoracic pain, but there is evidence for use in relief of neck pain and increasing respiratory function.
Lumbar Spine[edit | edit source]
Spinal manipulation to the lumbar spine is a common intervention administered for patients with Low Back Pain (LBP). Many noninvasive treatments are available for low-back pain, and these include drugs and nondrug options. In its 2017 clinical guidelines, the American College of Physicians (ACP) suggests that spinal manipulation is one of a number of therapeutic options that may help people with acute or chronic low-back pain (although the ACP says the quality of the evidence is low). [11] The research on spinal manipulation for acute low-back pain is generally mixed and has many limitations.
- Spinal manipulation is no more effective for acute low-back pain than sham (fake) spinal manipulation, or when added to another treatment such as standard medical care, a 2012 research review of 20 studies found. Spinal manipulation appeared to be safe when compared to other treatment options.
- A 2017 analysis examined data from 15 randomized controlled trials with almost 1,700 participants. The researchers concluded that spinal manipulative therapy can modestly improve pain and function in people with acute low-back pain[8].
The best way of using the manipulations is in combination with other therapeutic modalities.[edit | edit source]
- There is evidence from a high quality study, that spinal manipulative therapy combined with exercise is more effective than other procedures like spinal manipulation, exercise or physician consultation alone[12].
- A clinical prediction rule was developed in order to identify these patients with LBP who will most likely benefit from spinal manipulation.
- Spinal manipulation is a sub-group of the Treatment-Based Classification Approach for low back pain.[13].
Contra-indications[edit | edit source]
The following scenarios are contraindications to low back pain[14] :
- Any pathology that leads to significant bone weakening
- Neurological: cord compression, cauda equina compression, nerve root compression with increasing neurological deficit
- Vascular: aortic aneurysm, bleeding into joints
- Lack of diagnosis
- Patient positioning can not be achieved because of pain or resistance.
Other Conditions[edit | edit source]
A 2021 systematic review found no evidence of an effect of SMT for the management of non-musculoskeletal disorders including infantile colic, childhood asthma, hypertension, primary dysmenorrhea, and migraine. This finding challenges the validity of the theory that treating spinal dysfunctions with SMT has a physiological effect on organs and their function.[15]
Researchers have studied spinal manipulation for many other conditions, including fibromyalgia, children’s ear infections, chronic obstructive pulmonary disease (COPD), infant colic, and bedwetting, but there’s too little evidence to know if it helps with these problems.[8]
Neurophysiological Effects[edit | edit source]
↵An experimental body of evidence exists indicating that spinal manipulation impacts primary afferent neurons from paraspinal tissues, the motor control system and pain processing. Biomechanical changes caused by spinal manipulation are thought to have physiological consequences by means of their effects on the inflow of sensory information to the central nervous system
- Muscle spindle afferents and Golgi tendon organ afferents are stimulated by spinal manipulation.
- Smaller-diameter sensory nerve fibers are likely activated, although this has not been demonstrated directly.
- Mechanical and chemical changes in the intervertebral foramen caused by a herniated intervertebral disc can affect the dorsal roots and dorsal root ganglia, but it is not known if spinal manipulation directly affects these changes.
- Individuals with herniated lumbar discs have shown clinical improvement in response to spinal manipulation.
- The phenomenon of central facilitation is known to increase the receptive field of central neurons, enabling either subthreshold or innocuous stimuli access to central pain pathways. One mechanism underlying the effects of spinal manipulation may be the manipulation's ability to alter central sensory processing by removing subthreshold mechanical or chemical stimuli from paraspinal tissues.
- Spinal manipulation is also thought to affect reflex neural outputs to both muscle and visceral organs. Substantial evidence demonstrates that spinal manipulation evokes paraspinal muscle reflexes and alters motoneuron excitability. Cite error: The opening
<ref>tag is malformed or has a bad name
Key Evidence[edit | edit source]
- Fritz, Cleland, and Childs published an article in 2007 entitled "Subgrouping Patients With Low Back Pain: Evolution of a Classification Approach to Physical Therapy" which lays out the Treatment Based Classification Approach and explains the classification critia for the different intervention subgroups.
- Spinal Manipulative Therapy for Low Back Pain (Cochrane Review)
- Spinal Manipulative Therapy for Chronic Low Back Pain (Cochrane Review)
Resources[edit | edit source]
| [16] | [17] |
Manipulation/Mobilisation - Facts about physiotherapy and spinal manipulation from the APTA
References[edit | edit source]
- ↑ Spine Health Spinal Manipulation Available: https://www.spine-health.com/glossary/spinal-manipulation (accessed 13.6.2021)
- ↑ APTA. Manipulation/Mobilisation. Available online at http://www.apta.org/StateIssues/Manipulation/
- ↑ APTA. Manipulation fckLREducation Manual fckLRFor Physical Therapist fckLRProfessional Degree Programs. Available online at http://www.apta.org/uploadedFiles/APTAorg/Educators/Curriculum_Resources/APTA/Manipulation/ManipulationEducationManual.pdf
- ↑ Flynn T, Fritz J, Whitman J, et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine. 2002;27(24):2835-2843.
- ↑ 1. Fritz, Julie M. PT, PhD, ATC, Cleland, Joshua A. PT, PhD, OCS, FAAOMPT, and Childs, John D. PT, PhD, MBA, OCS, FAAOMPT, “Subgrouping Patients With Low Back Pain: Evolution of a Classification Approach to Physical Therapy,” Journal of Orthop Sports Physical Therapy 37, no. 6 (June 2007): 290-302.
- ↑ Fritz JM, Brennan GP, Leaman H. Does the evidence for spinal manipulation translate into better outcomes in routine clinical care for patients with occupational low back pain? A case-control study. Spine J. 2006;6(3):289-295.
- ↑ 7.0 7.1 Tseng Y, Wang W, Chen W, Hou T, Chen T, Lieu F. Predictors for the immediate responders to cervical manipulation in patients with neck pain. Manual Therapy. 2006;11(4):306-315.
- ↑ 8.0 8.1 8.2 8.3 NIH Spinal Manipulation: What You Need To Know Available: https://www.nccih.nih.gov/health/spinal-manipulation-what-you-need-to-know (accessed 13.6.2021)
- ↑ Neck pain - non-specific - NICE CKS [Internet]. Cks.nice.org.uk. 2018 [cited 20 May 2020]. Available from: https://cks.nice.org.uk/neck-pain-non-specific#!scenario
- ↑ Blanpied, R., Gross, R., Elliot, J., Devaney, L., Clewley, D., Walton, D., Spark, C., Robertson, E., Altman, R., Beattie, P., et al. (2017) Neck Pain: Revision 2017. Journal of Orthopaedic and Sports Physical Therapy [online] Available at: https://www.jospt.org/doi/10.2519/jospt.2017.0302 [Accessed 23 May 2020]
- ↑ Coronado. R, Gay. C, Bialosky. J, Carnaby. G, Bishop. M and George. S (2012) Changes in Pain sensitivity following spinal manipulation: a systematic review and meta-analysis. Journal of Electromyography and Kinesiology. 22(5): 752-767
- ↑ Rajadurai V, Murugan K. Spinal manipulative therapy for low back pain: A systematic review. Physical Therapy Reviews. 2009;14;4;260-271.
- ↑ National Institute of Clinical Excellence. Low back pain: Early management of persistent non-specific low back pain, May 2009
- ↑ Gibbons P., Tehan P. Patient positioning and spinal locking for lumbar spine rotation manipulation. Manual Therapy. 2001;6;3;130±138.
- ↑ Côté P, Hartvigsen J, Axén I, Leboeuf-Yde C, Corso M, Shearer H, Wong J, Marchand AA, Cassidy JD, French S, Kawchuk GN. The global summit on the efficacy and effectiveness of spinal manipulative therapy for the prevention and treatment of non-musculoskeletal disorders: a systematic review of the literature. Chiropractic & manual therapies. 2021 Dec;29(1):1-23.Available: https://chiromt.biomedcentral.com/articles/10.1186/s12998-021-00362-9(accessed 13.6.2021)
- ↑ SIJ Mobilization for LBP. Available from: http://www.vimeo.com/9221987, last accessed 21/5/10
- ↑ Maitland Lumbar PAIVM (skeletal model)Available from: https://www.youtube.com/watch?v=t0OCzavA6SY