Total Knee Arthroplasty: Difference between revisions
Claire Knott (talk | contribs) mNo edit summary |
Claire Knott (talk | contribs) mNo edit summary |
||
| Line 29: | Line 29: | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
In order to assess the gravity of wear or injury the orthopedic surgeon carries out external tests, and the patient is likely to undergo imaging. Patients co-morbidities also need to be considered<ref>Lee, Qunn Jid, Wai Ping Mak, and Yiu Chung Wong. "Risk factors for peri-prosthetic joint infection in total knee arthroplasty." Journal of Orthopaedic Surgery 23.3 (2015).</ref> Obesity is an important factor that needs to be considered prior to surgery as evidence suggests a correlation between higher body mass index (BMI) and poorer post-operative functional outcomes.<br> | In order to assess the gravity of wear or injury the orthopedic surgeon carries out external tests, and the patient is likely to undergo imaging. Patients co-morbidities also need to be considered<ref>Lee, Qunn Jid, Wai Ping Mak, and Yiu Chung Wong. "Risk factors for peri-prosthetic joint infection in total knee arthroplasty." Journal of Orthopaedic Surgery 23.3 (2015).</ref> Obesity is an important factor that needs to be considered prior to surgery as evidence suggests a correlation between higher body mass index (BMI) and poorer post-operative functional outcomes <ref>Polat, Ceylan, Sayar, Kucukdurmaz, Erdil and Tuncay. "Effect of body mass index on functional outcomes following arthroplasty procedures." World Journal of Orthopedics. 6.11 (2015). doi:10.5312/wjo.v6.i11.991.</ref><br> | ||
[[Image:Stages Knee OA.jpg]] | [[Image:Stages Knee OA.jpg]] | ||
Revision as of 08:23, 18 July 2018
Original Editors - Lynn Wright
Top Contributors - Safiya Naz, Loes Verspecht, Kim Jackson, Lucinda hampton, Kun Man Li, Jess Bell, Ellen Wynant, Lisa Ingenito, Claire Knott, George Prudden, Karolien Van Melkebeke, Lynn Wright, Tarina van der Stockt, Lauren Lopez, Daniele Barilla, WikiSysop, Karen Wilson, Famke Coosemans, Leana Louw, 127.0.0.1, Evan Thomas, Ewa Jaraczewska and Greg Walding
Definition/Description[edit | edit source]
Total knee arthoplasty (TKA) or total knee replacement (TKR) is a orthopaedic surgical procedure where the articular surfaces of the knee, the femoral condyles and tibial plateau, are replaced. There is at least one polyethylene piece, placed between the tibia and the femur, as a shock absorber.[1] In 50% of the cases the patella is also replaced. Reasons for a patella replacement are osteolysis, maltracking of the patella, failure of the implant,... The aim of the patella reconstruction is to restore the extensor mechanism. The level of bone loss will dictate which kind of patella prosthesis is placed. The main clinical reason for the operation is osteoarthritis with the goal of reducing an individuals pain and increasing function..[2]
Clinically Relevant Anatomy[edit | edit source]
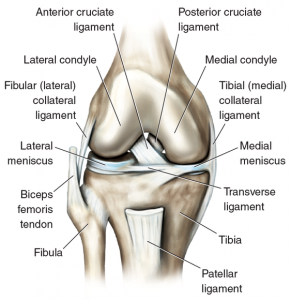
The Knee is a modified hinge joint, allowing motion through flexion and extension, but also a slight amount of internal and external rotation. There are three bones that form the knee joint: the upper part of the Tibia , the lower part of the Femur and the Patella. The bones are covered with a thin layer of cartilage, which ensures that friction is limited. On both the lateral and medial sides of the knee, there is a meniscus, which adheres the tibia to the femur, but is also a shock absorber. The three bones are kept together by the ligaments and are surrounded by a capsule.
Epidemiology /Etiology[edit | edit source]
When all the compartments of the knee are damaged, a total knee prosthesis may be necessary. The main cause of need for a total knee prosthesis is Osteoarthritis [3]. Osteoarthritis causes the cartilage of the joint to become damaged and no longer able to absorb shock. There are a lot of external risk factors that can cause knee osteoarthritis. For example: being overweight, previous knee injuries or partial removal of a meniscus, [4] rheumatoid arthritis, fractures and congenital factors. There might also be some genetic factors the contribute to the development of osteoarthritis, but more research is necessary. Total knee arthroplasty is more commonly performed on women and incidence increases with age.[4]
Characteristics/Clinical Presentation[edit | edit source]
Pain is the main complaint of patients' with degenerated knee joints. At first, pain is felt only after rest periods; this is also called ‘starting pain’; after a couple of minutes the pain slowly fades away. When the knee joint degeneration increases, the pain can also occur during rest periods and it can affect sleep at night. Individuals' can also complain of knee stiffness and crepitus. Due to pain and stiffness, function can decline and is manifests as reduced exercise tolerance, difficulty climbing stairs or slopes, reduced gait speed and increased risk of falls.
Complications[edit | edit source]
Stiffness is the most common complaint following primary total knee replacement, affecting approximately 6 to 7% of patients undergoing surgery.[5] In addition to stiffness, the following complications can impact on function following this surgery:
- Loosening or fracture of the prosthesis components
- Joint instability and dislocation
- Infection
- Component misalignment and breakdown
- Nerve damage
- Bone fracture (intra or post operatively)
- Swelling and joint pain
Diagnostic Procedures[edit | edit source]
In order to assess the gravity of wear or injury the orthopedic surgeon carries out external tests, and the patient is likely to undergo imaging. Patients co-morbidities also need to be considered[6] Obesity is an important factor that needs to be considered prior to surgery as evidence suggests a correlation between higher body mass index (BMI) and poorer post-operative functional outcomes [7]
These are the different stages of osteoarthritis that you can see at a MRI.
Outcome Measures[edit | edit source]
- Knee disability and Osteoarthritis Outcome score (KOOS)
- The Timed Get Up and Go Test (TUG)
- Visual Analogue Scale (VAS)
- Range of motion (ROM) [8] (evidence leven 1a)
Examination[edit | edit source]
Pre-operative tests[edit | edit source]
First the examiner should ask the patient about the history of complaints and also about expectations from surgery. The examiner should then perform a full objective examination. After this different tests could be carried out to determine whether the patient needs total knee arthroplasty:
- Active ROM
- Passive ROM
- Muscle power
- Functional tasks
Post-operative tests[edit | edit source]
- Inspection: of the wound/scar, redness, adhesion of the skin. When infection of the wound is suspected the patient must be referred to an orthopedist or an emergency doctor.
- Palpation: post-operative swelling, hypertonia (adductors), pain and warmth. [9]
Medical Management[edit | edit source]
The purpose of the surgical procedure is to achieve pain free movement again, with full functionality of the joint, and to recreate a stable joint with a full range of motion.
Total knee arthroplasty is chosen when the patient has serious complaints and functional limitations. Surgery takes some 60-90 minutes and involves putting into place a three-part prosthesis: a part for the femur, a part for the tibia and a part for the patella (not always) and a polyethylene joint. A high comfort insert design is chosen to achieve this. The perfect prosthesis doesn’t exist; every prosthesis must be different and the most appropriate chosen for each patient.
During surgery a tourniquet is sometimes used; this will ensure that that there is less blood loss. However, when a tourniquet is not used, there will be less swelling and less pain.[10] (evidence level: 1b)
Physical Therapy Management[edit | edit source]
Pre-operation[edit | edit source]
The physical therapist can choose to teach the patient the exercises before surgery in order that the patient might understand the procedures and, after surgery, be ready to practice a correct version of the appropriate exercises. In this way recovery can begin very rapidly. It is also important that the functional status of the patient before surgery be as good as possible. This will help recovery after surgery. Furthermore the patient can also start a training program before surgery. The patient has to train his postural control, needs to perform functional exercises and develop the strength of the lower extremities.[11] (evidence level: 1b)
However, there is insufficient quality evidence to support the efficacy of preoperative physiotherapy in adults who undergo total knee arthorplasty. There was minimal to no effect on knee strength, ambulation and pain. (evidence level 1a)
Results show that there is little evidence that pre-operative physiotherapy brings about significant improvements in patient outcome scores, lower limb strength, pain, range of movement and hospital length of stay following total knee arthroplasty.[12] (evidence leven 1a)
Post-operation[edit | edit source]
In several studies the effect of physiotherapy after total knee arthroplasty was examined. Generally these studies have shown that physiotherapy is always beneficial. The reports are not always clear regarding the kind of physiotherapy practiced, but all stress the importance of the patient moving. For example aqua therapy, balance training or cycling were added to the basic therapy, but there was no difference between the results obtained by the various therapies. One study compared a group of patients who didn't receive physiotherapy and a group who did. In this study it was clear that physiotherapy actually has its benefits. (evidence level: 1a)
If you give maximal strength training of 3 training sessions per week for 8 weeks with the supervision of a physiotherapist, muscle strength will increase faster (10 weeks follow up) compared with the standard rehabilitation. (evidence level: 1b)[13]
There is low quality evidence of quadriceps and hamstring weakness following TKA. Therefore strategies that specifically target strengthening of these muscle groups may need to be incorporated in rehabilitation to improve outcomes from TKA. [14] (evidence leven 1a)
The optimal physical therapy protocol should include strengthening and intensive functional exercises given through land-based or aquatic programs, that are progressed as the patient meets clinical and strength milestones. Due to the highly individualized characteristics of these exercises the therapy should be under supervision of of a trained physical therapist. This will give the best long term results. (evidence level 1a)
There are four steps in the revalidation process. The first step is mobilizations, then static strength, followed by dynamic strength, and ending with stabilization. The mobilizations and static strength training can be started at almost the same time. The first day after surgery it is important to stimulate blood circulation. Therefore the patient can be asked to perform a flexion and extension with the feet.
There is also low level evidence that accelerated physiotherapy regimens can reduce acute hospital length of stay.[15] (evidence level 1a)
The most important role of physiotherapists in the management of patientsfollowing TKA isfacilitating mobilisation within 48 hours of surgery, as part of an accelerated pathway. Physiotherapy in the hospital and inpatient rehabilitation settings following TKA should be focused on activity-based interventions. Further research is required to establish the effect of impairment-based interventions in the hospital and inpatient rehabilitation settings following TKA.[15] (evidence level 1a)
The possible beneficial effect of cryotherapy on blood loss is too small to justify it's use.There is evidence that cryotherapy improves knee range of motion and pain in the short-term. With are relatively small sample size of low quality evidence, it was difficult to draw solid conclusions regarding the outcomes measured in a review, and specific recommendations cannot be made about the use of cryotherapy.” [16] LOE 1A
Common bed and chair exercises[edit | edit source]
- Ankle plantarflexion/dorsiflexion
- Isometric knee extension in outer range
- Knee extension/flexion using a pillow behind the knee
- Knee and hip flexion/extension
- Isometric buttock contraction
- Hip abduction/adduction
- Straight leg raise
Key Research[edit | edit source]
Resources[edit | edit source]
Clinical Bottom Line[edit | edit source]
The knee prosthesis is the most commonly placed prosthesis in the human body, the main cause is general wear and degeneration of the joint. There are several risk factors, such as obesity, that we have to keep in mind, and cannot underestimate, in this degeneration process with loss of stability and other structural and functional problems.
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
- ↑ Palmer, Simon H., and M. J. Cross. "Total knee arthroplasty." Available on http://emedicine. medscape. com (ultimo accesso: 15 maggio, 2009) (2014).
- ↑ Kloiber, J., E. Goldenitsch, and P. Ritschl. "Patellar bone deficiency in revision total knee arthroplasty." Der Orthopade (2016).
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedSkou et al. - ↑ 4.0 4.1 Blagojevic, M., et al. "Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis." Osteoarthritis and cartilage 18.1 (2010): 24-33.
- ↑ Etiology and Surgical Interventions for Stiff Total Knee Replacements.
- ↑ Lee, Qunn Jid, Wai Ping Mak, and Yiu Chung Wong. "Risk factors for peri-prosthetic joint infection in total knee arthroplasty." Journal of Orthopaedic Surgery 23.3 (2015).
- ↑ Polat, Ceylan, Sayar, Kucukdurmaz, Erdil and Tuncay. "Effect of body mass index on functional outcomes following arthroplasty procedures." World Journal of Orthopedics. 6.11 (2015). doi:10.5312/wjo.v6.i11.991.
- ↑ Artz, Neil, et al. "Effectiveness of physiotherapy exercise following total knee replacement: systematic review and meta-analysis." BMC musculoskeletal disorders 16.1 (2015): 15. (LOE1a)
- ↑ Jakobsen, Thomas Linding, et al. "Early Progressive Strength Training to Enhance Recovery After Fast‐Track Total Knee Arthroplasty: A Randomized Controlled Trial." Arthritis care; research 66.12 (2014): 1856-1866.
- ↑ Fan Y, Jin J, Sun Z, Li W, Lin J, Weng X, Qiu G. The limited use of a tourniquet during total knee arthroplasty: a randomized controlled trial. Knee. 2014; 21(6): 1263-1268
- ↑ Huber EO, de Bie RA, Roos EM, Bischoff-Ferrari HA. Effect of pre-operative neuromuscular training on functional outcome after total knee replacement: a randomized-controlled trial. BMC Musculoskelet Disord. 2013 May
- ↑ Kwok, Iris HY, Bruce Paton, and Fares S. Haddad. "Does pre-operative physiotherapy improve outcomes in primary total knee arthroplasty?—a systematic review." The Journal of arthroplasty30.9 (2015): 1657-1663. (LOE 1a)
- ↑ 11. Vigdis Schnell H., Olav Andreas F., Otto Schnell H., Siri Bjorgen W. "Randomized controlled trial of maximal strenght training vs standard rehabilitation following total knee arthroplasty." Journal of physical and rehabilitation médicine (2017).
- ↑ Schache, Margaret B., Jodie A. McClelland, and Kate E. Webster. "Lower limb strength following total knee arthroplasty: a systematic review." The Knee 21.1 (2014): 12-20. (LOE1a)
- ↑ 15.0 15.1 Henderson, Kate G., Jason A. Wallis, and David A. Snowdon. "Active physiotherapy interventions following total knee arthroplasty in the hospital and inpatient rehabilitation settings: a systematic review and meta-analysis." Physiotherapy (2017). (LOE1a)
- ↑ Adie, Sam, Justine Naylor, and I. Harris. "Cryotherapy following total knee replacement." Cochrane Database Syst Rev 9 (2009). LOE1
13. Michael J. B., Jennifer E. S. "Early High-Intensity Rehabilitation Following Total Knee Arthroplasty Improves Outcomes." Journal of Orthopaedic & Sports Physical Therapy. (2017). (evidence level: 2b)
14. R.A. Chesham, S. Shanmugam. Does preoperative physiotherapy improve postoperative, patient based outcomes in older adults who have undergone total knee arthroplasty? A systematic review. Physiotherapy Theory Pract (2017). (evidence level: 1a)
15. F. Pozzi, L. Snyder-Mackler, J. Zeni. Physical exercise after knee arthroplasty: a systematic review of controlled trials. EUR J Phys Rehabil Med (2013): 877-892. (evidence level: 1a)