Bankart lesion
Top Contributors - Nikki Rommers, Estelle Hovaere, Lucinda hampton, Kim Jackson, Chrysolite Jyothi Kommu, Julie Schuermans, Admin, WikiSysop, 127.0.0.1, Elodie Baele, Naomi O'Reilly, Fasuba Ayobami, Birgit Schauvliege and Wanda van Niekerk
Introduction[edit | edit source]
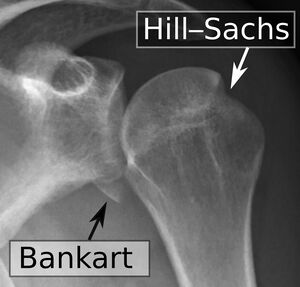
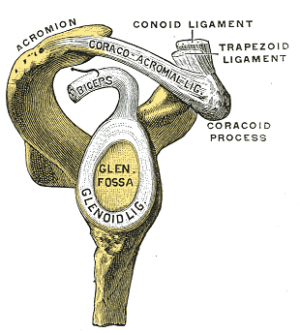
Bankart lesions are injuries of the anteroinferior aspect of the glenoid labral complex and are often found in association with a Hill-Sachs lesion. This injury is a common complication of anterior shoulder dislocation and/or repeated anterior shoulder subluxations. The dislocation of the shoulder joint (anterior) can damage the connective tissue ring around the glenoid labrum. It can also bring damage to the connection between the labrum and capsule. Usually associated with poor construction of the medial glenohumeral ligament. This injury is common for athletes that practice volleyball, tennis, handball, people who do overhead activities.[1][2]
Pathology[edit | edit source]
Bankart lesions occur when the humerus is compressed against the labrum as happens anterior shoulder dislocations or subluxations.. There is detachment of the anteroinferior labrum from the underlying glenoid (possibly with extension further superiorly or posteriorly). Impaction fracture of the anteroinferior glenoid margin frequently occurs simultaneously
Two types of Bankart lesions,
- Soft Bankart lesion: labrum tears from the glenoid, and the injury involves only the soft tissue. Most common
- Bony Bankart lesion: labrum tears and a part of the bony glenoid fractures or breaks off. May lead to notable bone loss in the glenoid, a cause chronic instability.[3]
In many cases of anterior dislocation patients have a Bankart lesion. A reverse Bankart lesion can occurs in case of a posterior dislocation.
Epidemiology /Etiology[edit | edit source]
Anterior Shoulder Instability is the most common traumatic type of instability, representing approximately 95% of all shoulder instabilities. [4] Traumatic shoulder dislocation commonly occur in in collision or contact sports. Abnormal translation of the humeral head during dislocation puts excessive loading on the labrum causing it to stretch along with the capsuloligamentous structures. This excessive stretch causes tearing or avulsion of the labrum with associated capsular injury.[5]
Characteristics/Clinical [edit | edit source]
Bankart lesions usually report a primary or recurrent anterior shoulder dislocation. They present with generalised shoulder pain and the signs and symptoms of recurrent shoulder instability. Some patient present with catching, locking, or popping sensations in the shoulder.[5]
Differential Diagnosis[edit | edit source]
A number of lesions are closely related have similar appearances, including:
- Anterior labroligamentous periosteal sleeve avulsion (ALPSA)
- Rotator Cuff Tears
- SLAP Lesion(Superior Labrum Anterior Posterior)
- Impingement
- Perthes lesion
- Glenolabral articular disruption (GLAD)
- Humeral avulsion of the glenohumeral ligament (HAGL)
- Bony humeral avulsion of the glenohumeral ligament (BHAGL)[6]
Diagnostic Procedures[edit | edit source]
Many patients who sustain a shoulder dislocation will sustain a Bankart lesion. [7] Although Bankart lesions often occur in patients with shoulder dislocation, they are hard to detect in physical examination.
- X-rays are important to obtain to rule out associated fractures and frank bony defects such as bony Bankart, Hill-Sachs, glenoid fractures, coracoid fractures, and greater tuberosity fractures.
- MRI with or without contrast is the gold standard investigation for soft tissue injuries such as glenoid labrum and capsuloligamentous injury. [5]
Outcome Measures[edit | edit source]
See also Category:Shoulder - Outcome Measures
Treatment[edit | edit source]
The patient's expectations, age, and sporting involvement (contact vs. non-contact) are vital factors to assess when treating a Bankart injury. Young patients involved in contact sports (high demand), they will be considered for surgery. In Bankart repairs, the labral fragment is sutured back to the glenoid rim using suture anchors.
Candidates for nonoperative management are patients showing no signs of shoulder instability, preserved normal osseous restrain to instability, and not using shoulder use for sports.[5]
Physical Therapy Management[edit | edit source]
Examination See Shoulder Instability
Interventions include the arthroscopic Bankart repair, an open Bankart repair or conservative management.
- Arthroscopic Bankart repair the muscle strength is regained faster, but the recurrence rates after open Bankart repair are significantly lower.[8]
- Recurrence rate after operative Bankart treatment is significantly reduced compared to a non-operative treatment. [9] After surgery there is of course rehabilitation needed which can be slightly comparable to the non-operative rehabilitation program. [10]
Focus of the rehabilitation program is on maximizing dynamic stability, scapula positioning, proprioception and improving neuromuscular control, as there are no specific exercises to improve the labrum quality. [4][11] For the first six weeks after surgery, emphasis is placed on protected motion. For the second six weeks, emphasis is placed on strengthening exercises so that strong muscles will protect the shoulder as it returns to normal activities. Usually the rehabilitation program is divided in 4 phases. The programs for non-operative treatment and postoperative rehabilitation are very similar.
- Phase 1, 1-6 weeks: consists of sling immobilization with a limited active range of motion for 0 to 4 weeks, this allows 20o of abduction and 40o of internal rotation. [12] This provides an earlier return to functional activity. [4][9][8][13] Immobilization in external rotation reduces the risk of recurrent shoulder dislocations. [10] After the 14 days passive movement is initiated in a pain free zone. Strengthening Exercises are started as isometric contractions to initiate muscle recruitment of the Rotator Cuff muscles, mostly Closed Chain Exercises, such as pushing your underarm against a wall towards exorotation. [11][9][4] The goals are to diminish pain and protect healing soft tissues.[4][13]
- Phase 2, 6 to 12 weeks: progressive passive motion is important, together with active-assisted range of motion exercises. [4]Strengthening of rotator cuff muscles is initiated in balanced exercises. Examples of exercises are movements of the shoulder executed with elastic bands or dumbbells as dynamic open chain strengthening exercises. [13] Rehabilitation should include both closed and open chain exercises. An example of a closed kinetic chain exercise is quadruped position with scapula protraction, progressing to tripod position. A patient can continue to phase three when a normal passive range of motion is achieved.
- Phase 3, 12 weeks to 4 months: Strengthening exercises (see anterior shoulder instability)
- Phase 4, 4 to 6 months: Fully unrestrained activitiesfocused on restoration of a full active range of motion. In this phase a progressively increasing resistance in dynamic exercises is stressed to regain full strength for ADL activities. Most imported in this phase is the return to full active activity of normal life.[5] [9][13]
There are 7 key factors that need to be considered in the rehabilitation of the unstable shoulder. These are:
• Onset of the pathology (traumatic, chronic)
• Degree of instability
• Frequency of dislocation
• Direction of instability (anterior, posterior, multidirectional)
• Concomitant pathologies
• End range neuromuscular control
• Premorbid activity level [4]
References[edit | edit source]
- ↑ Radiopedia Bankart Lesions Available:https://radiopaedia.org/articles/bankart-lesion (accessed 10.1.2023)
- ↑ Widjaja A, Tran A, Bailey M, Proper S (2006). Correlation between Bankart and Hill-Sachs lesions in anterior shoulder dislocation. ANZ J Surg 76 (6): 436–8.
- ↑ Facty Health Bankart Lesions and Shoulder Instability Available:https://facty.com/conditions/joint-pain/bankart-lesions-and-shoulder-instability/ (accessed 10.1.2023)
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 K. E. Wilk, L. C. Macrina, M. Reinold, ‘Non-operative Rehabilitation for traumatic and atraumatic glenohumeral instability’, North American Journal of Sports Fhysical Therapy, 2006, p 16-31 (Level of Evidence 1A)
- ↑ 5.0 5.1 5.2 5.3 5.4 Tupe RN, Tiwari V. Anteroinferior Glenoid Labrum Lesion (Bankart Lesion). Available:https://www.ncbi.nlm.nih.gov/books/NBK587359/ (accessed 10.1.2023)
- ↑ Radiopedia Anterior glenolabral injuries https://radiopaedia.org/articles/anterior-glenolabral-injuries?lang=gb Available:https://radiopaedia.org/articles/anterior-glenolabral-injuries?lang=gb (accessed 10.1.2023)
- ↑ S. Waldt, A. Burkart, A. B. Imhoff, M. Bruegel, E. J. Rummeny, K. Woerler, ‘Anterior Shoulder Instability: Accuracy of MR Arthrography in the Classification of Anteroinferior Labroligamentous Injuries’, Radiology, Volume 237, Number 2, 2005, p 578-583 (Level of Evidence 2B)
- ↑ 8.0 8.1 F. KHIAMI, ET AL. (February 2012), Anterior shoulder instability arthroscopic treatment outcomes measures: The WOSI correlates with the Walch-Duplay score, Revue de chirurgie Orthopédique et Traumatologique, volume 98, pages 48-53fckLRLevel of evidence: 4
- ↑ 9.0 9.1 9.2 9.3 NETTO ET AL ; Treatment of Bankart Lesions in Traumatic Anterior Instability of the Shoulder: A Randomized Controlled Trial Comparing Arthroscopy and Open Techniques; 2012fckLRLevel of evidence: 2
- ↑ 10.0 10.1 VOOS ET AL. Prospective Evaluation of Arthroscopic Bankart Repairs for Anterior Instability;. 2009 fckLRLevel of evidence: 4
- ↑ 11.0 11.1 DOMINIQUE M. ET AL (December 27), Validation of the Instability Shoulder Index Score in a Multicenter Reliability Study in 114 Consecutive cases, Am J Sports Med 2013 41: 278fckLRLevel of evidence: 2B
- ↑ S-H Kim, K-I Ha, M-W Jung, M-S Lim, Y-M Kim, J-H Park, ‘Accelerated Rehabilitation After Arthroscopic Bankart Repair for Selected Cases: A Prospective Randomized Clinical Study’, Arthroscopy, 2003, Volume 19, Number 7 (Level of Evidence 1B)
- ↑ 13.0 13.1 13.2 13.3 T. DUNCAN TENNENT,* FRCS(ORTH), WILLIAM R. BEACH, MD, AND JOHN F. MEYERS, MD, A Review of the Special Tests Associated with Shoulder Examination Part I: The Rotator Cuff Tests. Vol. 31, No. 1, 2003. pag 157-158.fckLRLevel of evidence: 3A