Hypotonia: Difference between revisions
Romy Hageman (talk | contribs) No edit summary |
Romy Hageman (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Romy Hageman|Romy Hageman]] <br> | <div class="editorbox"> '''Original Editor '''- [[User:Romy Hageman|Romy Hageman]] <br> | ||
Latest revision as of 16:50, 17 June 2024
Introduction[edit | edit source]
Hypotonia, commonly known as low muscle tone, is a condition characterized by decreased muscle tension and reduced resistance to passive movement[1][2]. It is often identified in infants and young children but can affect individuals of any age[3].
Hypotonia can occur in a wide range of populations, from newborns to adults, though it is most commonly diagnosed in infancy[3]. The prevalence varies depending on the underlying cause, but it is a relatively common symptom in many neuromuscular and genetic disorders[3][4].
Understanding hypotonia is crucial for physiotherapists and healthcare professionals because it affects motor development, functional abilities, and overall quality of life[5]. Early recognition and intervention can significantly improve outcomes for individuals with hypotonia[6]. It is important to closely monitor potential muscle tone changes within the first two years[6].
Etiology[edit | edit source]
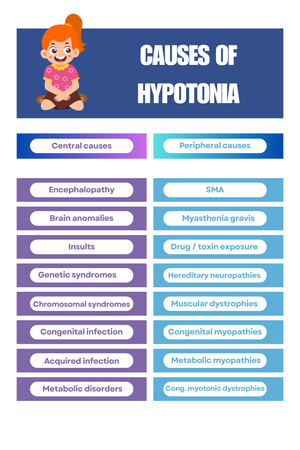
Hypotonia can result from a variety of causes, including genetic disorders (e.g., Down syndrome, Prader-Willi syndrome), neurological conditions (e.g., Cerebral Palsy, Spinal Muscular Atrophy), and metabolic diseases. It can also be idiopathic, with no identifiable cause. Around 80% of 'floppy infants' have a central nervous system origin, such as genetic or chromosomal syndromes, or due to hypoxic-ischemic encephalopathy[7][8].
The myotatic reflex, regulated by the peripheral nervous system, is the primary component of muscle tone[1]. However, the influence of central nervous system structures is also significant: the basal ganglia and red nucleus inhibit muscle tone, and damage to these areas results in hypertonia[1]. Conversely, the cerebellum and striatum facilitate muscle tone, and their damage leads to hypotonia[1].
In approximately 50% of hypotonia cases, the cause can be identified through a thorough history and physical examination[4].
Most cases of hypotonia are congenital and due to central pathology, often involving hypoxic-ischemic encephalopathy or genetic abnormalities[3]. Central hypotonia is present in 60-80% of cases. Down syndrome is the leading genetic cause, followed by Prader-Willi syndrome[3]. Peripheral and unknown causes make up the remainder. Common peripheral causes include spinal muscular atrophy, congenital muscular dystrophy, and congenital myopathies[3]. Spinal muscular atrophy occurs in about 1 in 6,000 to 1 in 10,000 live births[9]. Acquired hypotonia can result from toxins or infections, such as infant botulism.
| Central causes[3] | Peripheral causes[3] |
|---|---|
| Hypoxic encephalopathy | Spinal muscular athrophy |
| Brain anomalies / insults | Myasthenia gravis |
| Genetic / chromosomal syndromes | Drug / toxin exposure |
| Congenital or acquired infections | Hereditary neuropathies |
| Metabolic disorders | Muscular dystrophies |
| Congenital / metabolic myopathies | |
| Congenital myotonic dystrophies |
Associated conditions: common conditions associated with hypotonia include:
- Down syndrome[3]: a genetic disorder caused by the presence of an extra chromosome 21.
- Prader-Willi syndrome[3]: a genetic disorder caused by the loss of function of specific genes on chromosome 15. It is characterized by a constant feeling of hunger, leading to obesity, intellectual disabilities, low muscle tone (hypotonia), and short stature.
- Congestive heart failure[3]: an infant born with a congenital heart defect is a frequent case of hypotonia. Because most of the energy is used for breathing and circulating blood, these infants exhibit significant hypotonia and weakness. Assessing strength is challenging due to the lack of voluntary effort from an acutely ill infant.
- Metabolic disorders[3]: conditions that occurs when the body's normal metabolic processes are disrupted. This can result from enzyme deficiencies or abnormalities, leading to problems in the body's ability to convert food into energy and to manage waste products.
- Peroxisomal disorders[3]: a group of genetic conditions caused by defects in peroxisomes, which are cellular structures involved in breaking down fatty acids and detoxifying harmful substances. These disorders can lead to a range of symptoms, including developmental delays, neurological problems, and liver dysfunction. Examples include Zellweger syndrome and Adrenoleukodystrophy.
- Benign congenital hypotonia[3]: a condition present at birth characterized by hypotonia without an identifiable underlying neurological or muscular disease. It typically results in delayed motor development and muscle weakness, but many children improve over time and do not experience significant long-term complications.
- Pompe disease[3]: a rare genetic disorder caused by mutations in the GAA gene, leading to a deficiency of the enzyme acid alpha-glucosidase. This enzyme deficiency results in the build-up of glycogen in cells, particularly affecting muscles and the heart. Symptoms can include muscle weakness, respiratory issues, and cardiomyopathie. The severity and onset of symptoms can vary widely, with infantile-onset being more severe than late-onset forms.
- Spinal muscular atrophy (SMA)[3]: a genetic disorder characterized by the loss of motor neurons in the spinal cord, leading to muscle weakness and atrophy. It is caused by mutations in the SMN1 gene, which is essential for the survival of motor neurons. SMA affects physical strength and motor development, with severity ranging from early infantile onset, which is the most severe, to later-onset forms that are milder.
- Congenital myasthenic syndromes[3]: a group of genetic disorders impairing the transmission of signals between nerves and muscles, leading to muscle weakness and fatigue. These syndromes are caused by mutations affecting proteins at the neuromuscular junction. Symptoms often appear in infancy or early childhood and can include drooping eyelids, difficulty swallowing, and respiratory issues. The severity and specific features can vary widely among individuals.
- Drug toxicity - magnesium[3]: in neonates, a magnesium level above 1.15 mmol/l is considered hypermagnesemia. This condition often occurs in infants born to mothers treated with magnesium sulfate for eclampsia. Symptoms include hypotonia, reduced or absent reflexes, respiratory depression, poor feeding, slow heart rate (bradycardia) and ileus. Monitoring magnesium levels and providing supportive care are typically sufficient for management[4].
- Congenital muscular dystrophy type 1A - Laminin-A2[3]: clinical features include peripheral hypotonia, joint contractures, delayed motor milestone achievement, kyphoscoliosis, and respiratory problems. The condition typically starts in infancy or early childhood. Most patients have normal intelligence.
- Ullrich congenital muscular dystrophy[3]: a frequent cause of congenital muscular dystrophy. It is characterized by torticollis, kyphoscoliosis, distal joint hyperelasticity, and proximal joint contractures.
Pathophysiology[edit | edit source]
The underlying mechanisms of hypotonia involve disruptions in the central or peripheral nervous system, affecting muscle tone regulation[1]. This can include abnormalities in the brain, spinal cord, nerves or muscles. Central hypotonia is characterized by normal strength or mild to moderate weakness, with antigravity movements being present but often weaker[1]. In contrast, peripheral hypotonia is associated with significant muscle weakness and the absence of antigravity movements[1].
Clinical presentation: individuals with hypotonia often present with[1][10]:
- Floppy or rag-doll-like limbs:
- Scarf sign
- Diminished resistance to passive movement
- Hypermobile joints: exaggerated hip abduction, ankle dorsiflexion and hyperpronation of the feet, hyperextension of the knees
- Hip dysplasia
[11]In this video, you can see an example of the Scarf Sign on a baby with hypotonia.
- Delayed motor milestones:
- Such as rolling over, sitting, crawling, or walking
- Decreased activity tolerance
- Decreased / slow movements
- Posture:
- Leaning on things for support
- Poor antigravity posture
- Rounded shoulders
- Lack of posture regulation
- Froglike posture: full abduction and external rotation of legs
- W sitting
- Abnormal postures
- Winging of the scapula posture
- Fisted hands
- Asymmetry or postural fixations
- Head drop while sitting
- Decreased strength:
- Weakness
- Weakness in the muscles of the face, resulting in difficulties with feeding and speech, but also excessive drooling
- Problems with balance:
- Other:
- Poor attention or motivation
- Poor state of alertness
- Slow responses
- Constipation
- Irregular breathing patterns
- Weak cry
- Plagiocephaly
Diagnostic Procedures[edit | edit source]
Diagnosing hypotonia involves a comprehensive evaluation, including:
- History / interview[12]:
- Prenatal history
- Neonatal history:
- Hypotonia at birth with poor Apgar score may indicate hypoxic-ischemic encephalopathy[3].
- Poor muscle tone developing 12-24 hours after birth may indicate metabolic disorder[3].
- Past medical history
- Developmental history
- Family / Parent history
- School history
- Physical examination[13]: assessing muscle tone, reflexes, and motor skills
- Posture[12]:
- W or M sitting
- Frog-like posture
- Rag doll posture
- Winging of the scapula
- Postural fixation
- Postural alignment
- Protruding abdomen
- Kypho-lordosis
- Dysmorphic features and drooling (observation)[12]:
- Myopathic facies
- Oral-motor dysfunction
- Antigravity positions[12]
- Resistance to passive movement (palpation)[12]
- Flexibility and joint hypermobility (Range of Motion)[12]
- Motor skills (developmental assessments)[12]
- Muscle Strength (manual muscle testing)[12]
- Endurance and activity tolerance (functional assessment)[12]
- Reflexes (reflex testing)[12]: are there any abnormal reflexes?
- Posture[12]:
- Genetic testing[14][15]: identifying underlying genetic causes
- Imaging studies[13][15]: MRI or CT scan to examine brain and spinal cord abnormalities
- Electromyography (EMG)[16]: evaluating the electrical activity of muscles
Tests relevant for the physiotherapist:
- Pull-to-sit test[17][18]: also known as the traction response test, is a clinical assessment used to evaluate muscle tone and the development of motor control in infants. The infant is in a supine position. The physiotherapist grasps the infant's hands and slowly pulls the infant up towards a sitting position. If the child's head lags significantly behind the trunk or flops backward, this may indicate hypotonia.
- Scarf sign[17][18]: this is a clinical assessment used to evaluate muscle tone in infants. The infant is in a supine position. The physiotherapist moves one of the infant's arms across the chest towards the opposite shoulder. The outcome is the observation of the movement and the resistance of the arm.
- Vertical suspension[17][18]: during this clinical assessment, an infant is held under the arms. A hypotonic infant would slip through the examiner's hands. This test primarily evaluates appendicular muscle tone[17][19].
- Horizontal suspension[17][18]: this is a clinical assessment. It involves lifting the infant in a prone position with a hand supporting the chest and abdomen. Normally, an alert, full-term infant will show some flexion of the arms and legs and can hold the head above the horizontal for a short period. An infant with hypotonia will assume an inverted ''U'' shape[17][19].
- The Bayley Scales of Infant and Toddler Development (BSID) may be used to assess motor, cognitive, language, and social-emotional domains of development[3]. The assessment of the BSID may be difficult when the infant has a profound weakness[19].
- The Alberta Infant Motor Scale (AIMS): this is a standardized assessment tool used to evaluate the motor development of infants from birth to 18 months in four positions: prone, supine, sitting, and standing. This tool can be used to track the motor development in children with hypotonia[2].
- The Morgan Paleg Hypotonia Scale (MPH-10)[20]: this scale provides cut-off scores for detecting mild/moderate or severe hypotonia.
- Hammersmith Infant Neurological Examination (HINE)[21]: this examination is designed for children aged 2 months to 2 years and offers a simple and quantifiable assessment[6].
- Testing reflexes[2]: reduced or absent deep tendon reflexes suggest a peripheral or lower motor unit disorder. Although measuring these reflexes does not directly quantify hypotonia in children, it should be assessed in children with severe hypotonia and weakness. These cases warrant appropriate medical evaluation and referral.
Management and treatment[edit | edit source]
Physical therapy interventions are central to managing hypotonia. Interventions may include:
- Strengthening exercises: building muscle strength to support posture and movement[22].
- Developmental exercises: supporting the achievement of motor milestones in children[22].
Multidisciplinary approach: effective management often requires a team approach, involving[3]:
- Occupational therapists: assisting with fine motor skills and daily activities.
- Speech therapists: addressing feeding and speech difficulties.
- Medical specialists: providing medical management and monitoring of underlying conditions.
Home exercises and parental involvement: engaging parents and caregivers in home exercise programs is vital[3]. They can help reinforce therapy goals and support the child's development in a familiar environment. It is also important to make the parents aware of contraindications[4].
Prognosis[edit | edit source]
The prognosis for individuals with hypotonia varies depending on the underlying cause[3]. Effective management can greatly enhance the quality of life for those with hypotonia, enabling greater independence and participation in daily activities[3].
Conclusion[edit | edit source]
Hypotonia, characterized by low muscle tone, can have significant impacts on motor development and overall function. Early diagnosis and interventions are crucial for improving outcomes[3][4].
Clinical implications: Healthcare professionals must be aware of the signs and symptoms of hypotonia and adopt a multidisciplinary approach to manage this condition effectively. Early and consistent intervention can greatly enhance the quality of life for individuals with hypotonia.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Guadalupe De Santos-Moreno M, Velandrino-Nicolás AP, Gómez-Conesa A. Hypotonia: Is It a Clear Term and an Objective Diagnosis? An Exploratory Systematic Review. Pediatric Neurology. 2023; 138: 107-117
- ↑ 2.0 2.1 2.2 Robles AH, Paleg GS, Livingstone RW. Identifying and Evaluating Young Children with Developmental Central Hypotonia: An Overview of Systematic Reviews and Tools. Healthcare. 2024; 12(4): 493
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 3.22 3.23 3.24 3.25 3.26 3.27 Madhok SS, Shabbir N. Hypotonia. StatPearls Publishing, Treasure Island. 2020
- ↑ 4.0 4.1 4.2 4.3 4.4 Kaler J, Hussain A, Patel S, Majhi S. Neuromuscular Junction Disorders and Floppy Infant Syndrome: A Comprehensive Review. Cureus. 2020; 12(2): e6922
- ↑ Segal I, Peylan T, Sucre J, Levi L, Bassan H. Relationship between central hypotonia and motor development in infants attending a high-risk neonatal neurology clinic. Pediatric Physical Therapy. 2016; 28: 322-336
- ↑ 6.0 6.1 6.2 Goo M, Tucker K, Johnston LM. Muscle tone assessments for children aged 0 to 12 years: a systematic review. Developmental Medicine & Child Neurology. 2018; 60(7): 660-671
- ↑ Richer LP, Shevell MI, Miller SP. Diagnostic profile of neonatal hypotonia: an 11-year study. Pediatric Neurology. 2001; 25(1): 32-37
- ↑ Veneruso M, Fiorillo C, Broda P, Baratto S, Traverso M, Donati A, Savasta S, Falsaperla R, Mancardi MM, Pedemonte M, Panicucci C, Piatelli G, Pacetti M, Moscatelli A, Ramenghi LA, Nobili L, Minetti C, Bruno C. The Role of Muscle Biopsy in Diagnostic Process of Infant Hypotonia: From Clinical Classification to the Genetic Outcome. Frontiers in Neurology. 2021; 12: 735488
- ↑ D'Amico A, Mercuri E, Tiziano FD, Bertini E. Spinal muscular atrophy. Orphanet J Rare Dis. 2011; 6(71)
- ↑ Lawerman TF, Brandsma R, Maurits NM, Martinez-Manzanera O, Verschuuren-Bemelmans CC, Lunsing RJ, Brouwer OF, Kremer HPH, Sival Da. Paediatric motor phenotypes in early-onset ataxia, developmental coordination disorder, and central hypotonia. Developmental Medicine & Child Neurology. 2020; 62(1): 75-82
- ↑ onlinemedicalvideo Neurology exam: newborn-abnormal: Tone - Scarf Sign. Available from: https://www.youtube.com/watch?v=57MNEM6cmrc [last accessed 17/-6/2024]
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 12.6 12.7 12.8 12.9 Govender P, Joubert RWE. Evidence-Based Clinical Algorithm for Hypotonia Assessment: To Pardon the Errs. Occupational Therapy International. 2018; 8967572
- ↑ 13.0 13.1 Albanji MH, Alsaad AN, AlAnazi RF, Aleisa ZA, Alam DS, Alhashim AH. Utility of Hypotonia Diagnostic Investigations: A 12-year Single Center Study. Molecular Genetics and Metabolism Reports. 2020; 25: 100665
- ↑ Sharma S, Repnikova E, Noel-MacDonnell JR, LePichon J-B. Diagnostic yield of genetic testing in 324 infants with hypotonia. Clinical Genetics. 2021; 100(6): 752-757
- ↑ 15.0 15.1 Morton SU, Christodoulou J, Costain G, Muntoni F, Wakeling E, Wojcik MH, French CE, Szuto A, Dowling JJ, Cohn RD, Raymond FL, Darras BT, Williams DA, Lunke S, Stark Z, Rowitch DH, Agrawal PB. Multicenter Consensus Approach to Evaluation of Neonatal Hypotonia in the Genomic Era: A Review. JAMA Neurology. 2022; 79(4): 405-413
- ↑ Ganguly J, Kulshreshtha D, Almotiri M, Jog M. Muscle tone physiology and abnormalities. Toxins (Basel). 2021; 3: 1-20
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 Peredo DE, Hannibal MC. The floppy infant: evaluation of hypotonia. Pediatrics in Review. 2009; 30(9): e66-76
- ↑ 18.0 18.1 18.2 18.3 Bodensteiner JB. The evaluation of the hypotonic infant. Seminars in Pediatric Neurology. 2008; 15(1): 10-20
- ↑ 19.0 19.1 19.2 Harris SR. Congenital hypotonia: clinical and developmental assessment. Developmental Medicine and Child Neurology. 2008; 50(12): 889-892
- ↑ Paleg G, Morgan A. The Morgan Paleg Hypotonia Scale. In Proceedings of the International Cerebal Palsy Conference, Pisa, Italy. 2012; 45.
- ↑ Romeo DM, Ricci D, Brogna C, Mercuri E. Use of the Hammersmith Infant Neurological Examination in infants with cerebral palsy: A critical review of the literature. Developmental Medicine & Child Neurology. 2015; 58(3): 240-245
- ↑ 22.0 22.1 Paleg G, Romness M, Livingstone R. Interventions to improve sensory and motor outcomes for young children with central hypotonia: A systematic review. Journal of Pediatric Rehabilitation Medicine. 2018; 11(1): 57-70