Achilles Tendinopathy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="noeditbox">Welcome to [[Vrije Universiteit Brussel Evidence-based Practice Project|Vrije Universiteit Brussel's Evidence-based Practice | <div class="noeditbox">Welcome to [[Vrije Universiteit Brussel Evidence-based Practice Project|Vrije Universiteit Brussel's Evidence-based Practice Project]]. This space was created by and for the students in the Rehabilitation Sciences and Physiotherapy program of the Vrije Universiteit Brussel, Brussels, Belgium. Please do not edit unless you are involved in this project, but please come back in the near future to check out new information!!</div> <div class="editorbox"> | ||
'''Original | '''Original Editor '''- [[User:Karolyn Conolty|Karolyn Conolty]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Search Strategy | == Search Strategy == | ||
add text here | add text here related to databases searched, keywords, and search timeline <br> | ||
== | == Definition/Description == | ||
add text here | add text here <br> | ||
== | == Epidemiology /Etiology == | ||
add | <span style="font-size: 13px;">add text here</span><span style="font-size: 13px;"> </span> | ||
== | == <span style="font-size: 13px;" />Clinically Relevant Anatomy<br> == | ||
< | |||
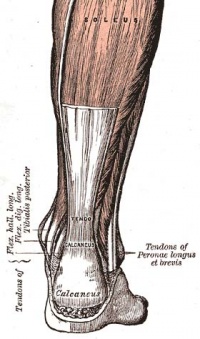
[[Image:Achilles tendon.jpg|thumb|right|200px|Achilles Tendon]] | [[Image:Achilles tendon.jpg|thumb|right|200px|Achilles Tendon]] | ||
| Line 100: | Line 40: | ||
The healing time for tendonitis is generally shorter, and commonly takes several days to 6 weeks. For tendinosis, the expected duration is variable, this can be 6-10 weeks, but it might also take 3-6 months, when the tendinosis has become chronic. <ref>K M Khan, a. p. (2002). Time to abandon the “tendinitis” myth: Painful, overuse tendon conditions have a non-inflammatory pathology . BMJ , 324:626.fckLR Level 2A</ref>, <ref>Evelyn Bass, L. (2012). Tendinopathy: Why the Difference Between Tendinitis and Tendinosis Matters. Int J Ther Massage Bodywork. , 5(1): 14–17.fckLR Level 2C</ref><br> | The healing time for tendonitis is generally shorter, and commonly takes several days to 6 weeks. For tendinosis, the expected duration is variable, this can be 6-10 weeks, but it might also take 3-6 months, when the tendinosis has become chronic. <ref>K M Khan, a. p. (2002). Time to abandon the “tendinitis” myth: Painful, overuse tendon conditions have a non-inflammatory pathology . BMJ , 324:626.fckLR Level 2A</ref>, <ref>Evelyn Bass, L. (2012). Tendinopathy: Why the Difference Between Tendinitis and Tendinosis Matters. Int J Ther Massage Bodywork. , 5(1): 14–17.fckLR Level 2C</ref><br> | ||
== Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Morning pain is a hallmark symptom because the achilles tendon must tolerate full range of movement including stretch immediately on rising in the morning. Symptoms are typically localized to the tendon and immediate surrounding area. Swelling and pain at the attachment are less common. The tendon can appear to have subtle changes in outline, becoming thicker in the A-P and M-L planes.<ref name="Cook et al" /><br> | Morning pain is a hallmark symptom because the achilles tendon must tolerate full range of movement including stretch immediately on rising in the morning. Symptoms are typically localized to the tendon and immediate surrounding area. Swelling and pain at the attachment are less common. The tendon can appear to have subtle changes in outline, becoming thicker in the A-P and M-L planes.<ref name="Cook et al" /><br> | ||
With people who have a tendinopathy of the achilles tendon that has a sensitive zone, combined with intratendinous swelling, that moves along with the tendon and of which sensitivity increases or decreases when the tendon is put under pressure, there will be a high predictive value that in this situation there is a case of tendinosis.<ref>KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.fckLR Level 2C</ref><br> | With people who have a tendinopathy of the achilles tendon that has a sensitive zone, combined with intratendinous swelling, that moves along with the tendon and of which sensitivity increases or decreases when the tendon is put under pressure, there will be a high predictive value that in this situation there is a case of tendinosis.<ref>KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.fckLR Level 2C</ref><br> | ||
== Differential Diagnosis<br> == | |||
[[Ankle Impingement|Posterior Ankle Impingement]], Medial Tendinopathy, [[Retrocalcaneal Bursitis|Retrocalcaneal Bursitis]], [[Sural Nerve|Sural Nerve]], [[Lumbar Radiculopathy|Lumbar Radiculopathy]], [[Ankle Osteoarthritis|Ankle OA]], [[Deep Vein Thrombosis|DVT]], [[Haglund Deformity|Haglund Deformity]], Partial [[Achilles Rupture|Achilles Tendon Rupture]].<ref name="Cook et al" /> | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
| Line 110: | Line 54: | ||
Examination of the achilles tendon is inspection for muscle atrophy, swelling, asymmetry, joint effusions and erythema. Atrophy is an important clue to the duration of the tendinopathy and it is often present with chronic conditions. Swelling, asymmetry and erythema in pathologic tendons are often observed in the examination. Joint effusions are uncommon with tendinopathy and suggest the possibility of intra-articular pathology.<br> | Examination of the achilles tendon is inspection for muscle atrophy, swelling, asymmetry, joint effusions and erythema. Atrophy is an important clue to the duration of the tendinopathy and it is often present with chronic conditions. Swelling, asymmetry and erythema in pathologic tendons are often observed in the examination. Joint effusions are uncommon with tendinopathy and suggest the possibility of intra-articular pathology.<br> | ||
Range of motion testing, strength and flexibility are often limited on the side of the tendinopathy.<ref>. Hammer, W. I. (1999). Functional Soft Tissue Examination and Treatment by Manual Methods. Aspen: Jones &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Bartlett Learning.</ref>, <ref>KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.fckLR Level 2C</ref> | Range of motion testing, strength and flexibility are often limited on the side of the tendinopathy.<ref>. Hammer, W. I. (1999). Functional Soft Tissue Examination and Treatment by Manual Methods. Aspen: Jones &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Bartlett Learning.</ref>, <ref>KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.fckLR Level 2C</ref> | ||
Palpation tends to elicit well-localized tenderness that is similar in quality and location to the pain experienced during activity.<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref><br>Physical examinations of the Achilles tendon often reveals palpable nodules and thickening. Anatomic deformities, such as forefoot and heel varus and excessive pes planus or foot pronation, should receive special attention. These anatomic deformities are often associated with this problem.<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref>, <ref>Shibuya N, T. J. (2012). Is calcaneal inclination higher in patiënts with insertional achilles tendinosis? A case- controlled, cross-sectional study. The journal of foot and ankle surgery , 757-761.fckLR Level 3B</ref> | Palpation tends to elicit well-localized tenderness that is similar in quality and location to the pain experienced during activity.<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref><br>Physical examinations of the Achilles tendon often reveals palpable nodules and thickening. Anatomic deformities, such as forefoot and heel varus and excessive pes planus or foot pronation, should receive special attention. These anatomic deformities are often associated with this problem.<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref>, <ref>Shibuya N, T. J. (2012). Is calcaneal inclination higher in patiënts with insertional achilles tendinosis? A case- controlled, cross-sectional study. The journal of foot and ankle surgery , 757-761.fckLR Level 3B</ref> | ||
| Line 120: | Line 64: | ||
== Outcome Measures == | == Outcome Measures == | ||
Robinson et al recommend the [[VISA-A scale|VISA-A scale]]. This is a subjective rating scale that quantifies the symptoms and dysfunction in the Achilles tendon. It is very useful to rate Achilles tendons and to assess progress of recovery during rehabilitation. <ref name="Cook et al" /><ref name="Robinson et al">Robinson JM, Cook JL, Purdam C et al. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. British J of Sports Med. 2001;35:335-341.</ref> | Robinson et al recommend the [[VISA-A scale|VISA-A scale]]. This is a subjective rating scale that quantifies the symptoms and dysfunction in the Achilles tendon. It is very useful to rate Achilles tendons and to assess progress of recovery during rehabilitation. <ref name="Cook et al" /><ref name="Robinson et al">Robinson JM, Cook JL, Purdam C et al. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. British J of Sports Med. 2001;35:335-341.</ref><br> | ||
== Examination == | |||
add text here related to physical examination and assessment | |||
== Medical Management <br> == | |||
add text here <br> | |||
== Physical Therapy Management / Interventions<br> == | |||
& | <span style="line-height: 1.5em;">The treatment should be conservative, </span><span style="line-height: 1.5em;"> </span><span style="line-height: 1.5em;">including rest, equipment changes, strength and flexibility exercises</span><span style="line-height: 1.5em;">. A popular and effective option is the eccentric strength training. Deep friction massage and stretching of the gastrocnemius and soleus are considered helpful for Achilles tedinopathy.</span><ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref><span style="line-height: 1.5em;"> </span><span style="line-height: 1.5em;">Anatomic deformities can be treated with shoe orthotics. These shoe orthotics correct overpronation or pes planus problems.</span><ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref><span style="line-height: 1.5em;"> </span> | ||
<span style="line-height: 1.5em;">The effects of physical therapy on achilles tendonitis is poorly understood, although musculotendinous strengthening appears essential. </span>[[Eccentric Exercises|Eccentric exercises]]<span style="line-height: 1.5em;"> have been shown to have positive effects of Achilles tendonitis, and remains the gold standard for rehabiliation of this condition.</span><ref name="Cook et al" /><ref name="Roos et al" /><span style="line-height: 1.5em;"> A study by Roos et al concluded that eccentric exercises improve function and reduce pain and effects were apparent after 6 weeks of treatment, lasting for 1 year.</span><ref name="Robinson et al" /> | |||
An inflammation is necessary to start a restoration process in the damaged tissue, but the use of certain medication, such as corticosteroids and quinolones counter the inflammation, and as a result also the restoration process. Even when the patient does not take this medication, tendinosis is also a consequence of a disrupted restoration process.<ref>MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.</ref> | An inflammation is necessary to start a restoration process in the damaged tissue, but the use of certain medication, such as corticosteroids and quinolones counter the inflammation, and as a result also the restoration process. Even when the patient does not take this medication, tendinosis is also a consequence of a disrupted restoration process.<ref>MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.</ref> | ||
| Line 138: | Line 90: | ||
|} | |} | ||
=== Conservative | === Conservative Treatment: <ref>Alex Scott, R. P. (2011). Conservative treatment of chronic Achilles tendinopathy. CMAJ , 183(10): 1159–1165.fckLR Level 1A</ref>,<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref> === | ||
In order to treat the symptoms, antiflogistics or other anti-inflammatory therapy are often used. However these forms of therapy usually cannot prevent the injury to live on. | In order to treat the symptoms, antiflogistics or other anti-inflammatory therapy are often used. However these forms of therapy usually cannot prevent the injury to live on. | ||
| Line 144: | Line 96: | ||
Nevertheless patients will always have to be encouraged to execute less burdening activities, so that the burden on the tendon decreases as well. Complete immobilisation should however be avoided, since it can cause atrophy. | Nevertheless patients will always have to be encouraged to execute less burdening activities, so that the burden on the tendon decreases as well. Complete immobilisation should however be avoided, since it can cause atrophy. | ||
Passive | Passive Rehabilitation: | ||
*Mobilisations can be used for dorsiflexion limitation of the talocrural joint and varus- or valgus limitation of the subtalar joint. | *Mobilisations can be used for dorsiflexion limitation of the talocrural joint and varus- or valgus limitation of the subtalar joint. | ||
*Deep cross frictions (15 min). It’s effectiveness is not scientifically proven and gives limited results. <ref>. Hammer, W. I. (1999). Functional Soft Tissue Examination and Treatment by Manual Methods. Aspen: Jones &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Bartlett Learning.</ref>, <ref>Stasinopoulos D, S. I. (2004). Comparison of effects of exercise programme, pulsed ultrasound and transverse friction in the treatment of chronic patellar tendinopathy. Clin Rehabil , 18(4):347-52.fckLR Level 1B</ref>, <ref>James Henry Cyriax, P. J. (1993). Illustrated manual of orthopaedic medicine. Oxford: Elsevier Health Sciences.</ref>, <ref>Joseph MF, T. K. (2012). Deep friction massage to treat tendinopathy: a systematic review of a classic treatment in the face of a new paradigm of understanding. J Sport Rehabil. , 21(4):343-53.fckLR Level 3A</ref> | *Deep cross frictions (15 min). It’s effectiveness is not scientifically proven and gives limited results. <ref>. Hammer, W. I. (1999). Functional Soft Tissue Examination and Treatment by Manual Methods. Aspen: Jones &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Bartlett Learning.</ref>, <ref>Stasinopoulos D, S. I. (2004). Comparison of effects of exercise programme, pulsed ultrasound and transverse friction in the treatment of chronic patellar tendinopathy. Clin Rehabil , 18(4):347-52.fckLR Level 1B</ref>, <ref>James Henry Cyriax, P. J. (1993). Illustrated manual of orthopaedic medicine. Oxford: Elsevier Health Sciences.</ref>, <ref>Joseph MF, T. K. (2012). Deep friction massage to treat tendinopathy: a systematic review of a classic treatment in the face of a new paradigm of understanding. J Sport Rehabil. , 21(4):343-53.fckLR Level 3A</ref> | ||
*Recently, the use of Extracorporal Shock Wave Therapy was proven.<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref>, <ref>Rompe JD, F. J. (2008). Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy. A randomized, controlled trial. J Bone Joint Surg Am. , (1):52-61.fckLR Level 1B</ref>, <ref>Sten Rasmussen, M. C. (2008). Shockwave therapy for achilles tendinopathy. A double-blind, randomized clinical trail of efficacy. Acta Orthopaedica , 249-256.fckLR Level 1B</ref> | *Recently, the use of Extracorporal Shock Wave Therapy was proven.<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref>, <ref>Rompe JD, F. J. (2008). Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy. A randomized, controlled trial. J Bone Joint Surg Am. , (1):52-61.fckLR Level 1B</ref>, <ref>Sten Rasmussen, M. C. (2008). Shockwave therapy for achilles tendinopathy. A double-blind, randomized clinical trail of efficacy. Acta Orthopaedica , 249-256.fckLR Level 1B</ref> | ||
*Besides that, the application of ice can cause a short decrease in pain and in swelling. Even though cryotherapy 2, 5 was not studied very thoroughly, recent research has shown that for injuries of soft tissue, applications of ice through a wet towel for ten minutes are the most effective measures. <ref>Bleakley C, M. S. (2004). The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med , (1):251-61.fckLR Level 1A</ref>, <ref>Dykstra JH, H. H. (2009). Comparisons of cubed ice, crushed ice, and wetted ice on intramuscular and surface temperature changes. J Athl Train. , (2):136-41.fckLR Level 2A</ref>, <ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref> | *Besides that, the application of ice can cause a short decrease in pain and in swelling. Even though cryotherapy 2, 5 was not studied very thoroughly, recent research has shown that for injuries of soft tissue, applications of ice through a wet towel for ten minutes are the most effective measures. <ref>Bleakley C, M. S. (2004). The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med , (1):251-61.fckLR Level 1A</ref>, <ref>Dykstra JH, H. H. (2009). Comparisons of cubed ice, crushed ice, and wetted ice on intramuscular and surface temperature changes. J Athl Train. , (2):136-41.fckLR Level 2A</ref>, <ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref> | ||
Active | Active Rehabilitation:<br> | ||
*An active exercise program mostly includes eccentric exercises. This can be explained by the fact that eccentric muscle training will lengthen the muscle fibres, which stimulates the collagen production. This form of therapy appears successful for mid-portion tendinosis, but has less effect with insertion tendinopathy. The sensation of pain sets the beginning burdening of the patient and the progression of the exercises.<ref>Bleakley C, M. S. (2004). The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med , (1):251-61.fckLR Level 1A</ref>, <ref>Brett L Woodley, R. J.‐W. (2007). Chronic tendinopathy: effectiveness of eccentric exercise. Br J Sports Med , 41(4): 188–198.fckLR Level 1A</ref>, <ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref> | *An active exercise program mostly includes eccentric exercises. This can be explained by the fact that eccentric muscle training will lengthen the muscle fibres, which stimulates the collagen production. This form of therapy appears successful for mid-portion tendinosis, but has less effect with insertion tendinopathy. The sensation of pain sets the beginning burdening of the patient and the progression of the exercises.<ref>Bleakley C, M. S. (2004). The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med , (1):251-61.fckLR Level 1A</ref>, <ref>Brett L Woodley, R. J.‐W. (2007). Chronic tendinopathy: effectiveness of eccentric exercise. Br J Sports Med , 41(4): 188–198.fckLR Level 1A</ref>, <ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref> | ||
| Line 157: | Line 109: | ||
Thorough management guidelines for achilles tendinopathy is covered in detail in the [[Achilles Tendinopathy Toolkit|Achilles Tendinopathy Toolkit]].<br> | Thorough management guidelines for achilles tendinopathy is covered in detail in the [[Achilles Tendinopathy Toolkit|Achilles Tendinopathy Toolkit]].<br> | ||
== | == Key Research == | ||
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template) | |||
== Clinical Bottom Line == | |||
add text here | |||
== Resources == | == Resources == | ||
<div class="coursebox"> | <div class="coursebox"> | ||
{| width="100%" class="FCK__ShowTableBorders" border="0" cellspacing="4" cellpadding="4" | {| width="100%" class="FCK__ShowTableBorders" border="0" cellspacing="4" cellpadding="4" | ||
Revision as of 19:09, 6 June 2016
Original Editor - Karolyn Conolty
Top Contributors - Aline Tréfois, Admin, Puja Gaikwad, Kim Jackson, Eva Roose1, Rachael Lowe, Lucinda hampton, Laura Ritchie, Shauni Van Overstraeten, Karolyn Conolty, Chi Ngai LO, Christopher, Fasuba Ayobami, Simisola Ajeyalemi, Birgit Schauvliege, Wanda van Niekerk, Naomi O'Reilly, 127.0.0.1, Vidya Acharya, Rucha Gadgil, Eric Robertson, Samuel Adedigba, Jess Bell, Khloud Shreif, David Bayard, Camille Linussio and Olajumoke Ogunleye
Search Strategy [edit | edit source]
add text here related to databases searched, keywords, and search timeline
Definition/Description [edit | edit source]
add text here
Epidemiology /Etiology [edit | edit source]
add text here
Clinically Relevant Anatomy
[edit | edit source]
The Achilles tendon is the single tendon of the soleus and gastrocnemius muscles, inserting into the calcaneus.[1]
Mechanism of Injury / Pathological Process
[edit | edit source]
Tendonitis[edit | edit source]
Tendinitis is the inflammation of the tendon and results from micro-tears that happen when the musculotendinous unit is acutely overloaded with a tensile force that is too heavy and/or too sudden[2].
Achilles tendonitis is commonly seen in athletes who sustain an increase in training load, and is most often due to overuse. Tendons respond poorly to overuse, therefore healing is slow. This can leave a tendon pathologically defective, which decreases tendon strength and leaves it less able to tolerate load, thus vulnerable to further injury[1] or tendinosis. Extrinsic factors contributing to this condition include training errors and inappropriate footwear. Intrinsic factors include inflexibility, weakness and malalignment. [3]
Tendinosis[edit | edit source]
In other situations, there will be clinical inflammation, but objective pathologic evidence for cellular inflammation is lacking, and in these conditions the term tendinosis is more appropriate. Tendinosis is a degeneration of the tendon’s collagen in response to chronic overuse; when overuse is continued without giving the tendon time to heal and rest, such as with repetitive strain injury, tendinosis results. Even tiny movements, such as clicking a mouse, can cause tendinosis, when done repeatedly.
Achilles tendinosis is a degenerative change of the Achilles Tendon associated with pain and often with thickening of the tendon. It is common in athletes, but it also occurs in non athletes. Surgical specimens show a range of degenerative changes of the affected tendon, such as changes in tendon fibre structure and arrangement as well as an increase in glycosaminoglycans, which may explain the swelling of the tendon.[4] The precise cause of tendinosis remains unclear. Even though tendinosis of the achilles tendon is often connected to sport activities, the ailment is also often found with people who do not practice sports. The biggest cause is the excessive overburdening of the tendon. A light degeneration of the achilles tendon can be latently present, but pain only comes into being when the tendon is overburdened. It is also noted that the ailment is usually not preceded by a trauma.[5], [6]
Tendinosis is often confused with tendonitis, but it is important to understand the difference between these two pathologies. Tendonitis is an inflammation of the tendon. This inflammation causes micro-tears in the tendon when the tendon is acutely overloaded. This diagnosis is often mistakenly used when the patiënt actually has tendinosis. Tendinosis is a degeneration process in which no temperature rises occur, as apposed to tendonitis. It is very important to distinguish between these disorders, to discover which treatment is required, and what the expected duration of the treatment will be.
The healing time for tendonitis is generally shorter, and commonly takes several days to 6 weeks. For tendinosis, the expected duration is variable, this can be 6-10 weeks, but it might also take 3-6 months, when the tendinosis has become chronic. [7], [8]
Characteristics/Clinical Presentation[edit | edit source]
Morning pain is a hallmark symptom because the achilles tendon must tolerate full range of movement including stretch immediately on rising in the morning. Symptoms are typically localized to the tendon and immediate surrounding area. Swelling and pain at the attachment are less common. The tendon can appear to have subtle changes in outline, becoming thicker in the A-P and M-L planes.[1]
With people who have a tendinopathy of the achilles tendon that has a sensitive zone, combined with intratendinous swelling, that moves along with the tendon and of which sensitivity increases or decreases when the tendon is put under pressure, there will be a high predictive value that in this situation there is a case of tendinosis.[9]
Differential Diagnosis
[edit | edit source]
Posterior Ankle Impingement, Medial Tendinopathy, Retrocalcaneal Bursitis, Sural Nerve, Lumbar Radiculopathy, Ankle OA, DVT, Haglund Deformity, Partial Achilles Tendon Rupture.[1]
Diagnostic Procedures[edit | edit source]
Examination of the achilles tendon is inspection for muscle atrophy, swelling, asymmetry, joint effusions and erythema. Atrophy is an important clue to the duration of the tendinopathy and it is often present with chronic conditions. Swelling, asymmetry and erythema in pathologic tendons are often observed in the examination. Joint effusions are uncommon with tendinopathy and suggest the possibility of intra-articular pathology.
Range of motion testing, strength and flexibility are often limited on the side of the tendinopathy.[10], [11]
Palpation tends to elicit well-localized tenderness that is similar in quality and location to the pain experienced during activity.[12]
Physical examinations of the Achilles tendon often reveals palpable nodules and thickening. Anatomic deformities, such as forefoot and heel varus and excessive pes planus or foot pronation, should receive special attention. These anatomic deformities are often associated with this problem.[13], [14]
In case extra research is wanted, an echography is the first choice of examination when there is a suspicion of tendinosis.[15]
Imaging studies are not necessary to diagnose achilles tendonitis, but may be useful with differential diagnosis. Ultrasound is the imaging modality of first choice as it provides a clear indication of tendon width, changes of water content within the tendon and collagen integrity, as well as bursal swelling. MRI may be indicated if diagnosis is unclear or symptoms are atypical. MRI may show increased signal within the Achilles.[1]
Outcome Measures[edit | edit source]
Robinson et al recommend the VISA-A scale. This is a subjective rating scale that quantifies the symptoms and dysfunction in the Achilles tendon. It is very useful to rate Achilles tendons and to assess progress of recovery during rehabilitation. [1][16]
Examination[edit | edit source]
add text here related to physical examination and assessment
Medical Management
[edit | edit source]
add text here
Physical Therapy Management / Interventions
[edit | edit source]
The treatment should be conservative, including rest, equipment changes, strength and flexibility exercises. A popular and effective option is the eccentric strength training. Deep friction massage and stretching of the gastrocnemius and soleus are considered helpful for Achilles tedinopathy.[17] Anatomic deformities can be treated with shoe orthotics. These shoe orthotics correct overpronation or pes planus problems.[18]
The effects of physical therapy on achilles tendonitis is poorly understood, although musculotendinous strengthening appears essential. Eccentric exercises have been shown to have positive effects of Achilles tendonitis, and remains the gold standard for rehabiliation of this condition.[1][3] A study by Roos et al concluded that eccentric exercises improve function and reduce pain and effects were apparent after 6 weeks of treatment, lasting for 1 year.[16]
An inflammation is necessary to start a restoration process in the damaged tissue, but the use of certain medication, such as corticosteroids and quinolones counter the inflammation, and as a result also the restoration process. Even when the patient does not take this medication, tendinosis is also a consequence of a disrupted restoration process.[19]
Supportive taping can also help manage symptoms:
| [20] | [21] |
Conservative Treatment: [22],[23][edit | edit source]
In order to treat the symptoms, antiflogistics or other anti-inflammatory therapy are often used. However these forms of therapy usually cannot prevent the injury to live on.
Nevertheless patients will always have to be encouraged to execute less burdening activities, so that the burden on the tendon decreases as well. Complete immobilisation should however be avoided, since it can cause atrophy.
Passive Rehabilitation:
- Mobilisations can be used for dorsiflexion limitation of the talocrural joint and varus- or valgus limitation of the subtalar joint.
- Deep cross frictions (15 min). It’s effectiveness is not scientifically proven and gives limited results. [24], [25], [26], [27]
- Recently, the use of Extracorporal Shock Wave Therapy was proven.[28], [29], [30]
- Besides that, the application of ice can cause a short decrease in pain and in swelling. Even though cryotherapy 2, 5 was not studied very thoroughly, recent research has shown that for injuries of soft tissue, applications of ice through a wet towel for ten minutes are the most effective measures. [31], [32], [33]
Active Rehabilitation:
- An active exercise program mostly includes eccentric exercises. This can be explained by the fact that eccentric muscle training will lengthen the muscle fibres, which stimulates the collagen production. This form of therapy appears successful for mid-portion tendinosis, but has less effect with insertion tendinopathy. The sensation of pain sets the beginning burdening of the patient and the progression of the exercises.[34], [35], [36]
Thorough management guidelines for achilles tendinopathy is covered in detail in the Achilles Tendinopathy Toolkit.
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Clinical Bottom Line[edit | edit source]
add text here
Resources[edit | edit source]
 |
Achilles Tendinopathy Toolkit
The Achilles Tendinopathy Toolkit is a comprehensive evidence based resource to assist practitioners in clinical decision making for Achilles Tendinopathy. |
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1DeUIcPgNLDEQT17PEJLA26uuKLv4fz4eTsAi9nkGXzfWOXsZF|charset=UTF-8|short|max=10: Error parsing XML for RSS
Presentations[edit | edit source]
 |
Achilles Tendonopathy: Intervention
This presentation, created by Shannon Petersen, Clebert LeBlanc, Amy Lavrich, & Kelly Coleman as part of the Regis University OMPT Fellowship, discusses the current best evidence for interventions for Achilles Tendonopathy. |
Read 4 Credit[edit | edit source]
|
Would you like to earn certification to prove your knowledge on this topic? All you need to do is pass the quiz relating to this page in the Physiopedia member area.
|
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Cook JL, Khan KM, Purdam C. Achilles tendinopathy. Manual Therapy 2002;7(3):121-130.
- ↑ Evelyn Bass. Tendinopathy: Why the Difference Between Tendinitis and Tendinosis Matters Int J Ther Massage Bodywork. 2012; 5(1): 14–17.fckLRPublished online Mar 31, 2012.
- ↑ 3.0 3.1 Roos EM, Engstrom M, Lagerquist A, Soderberg B. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy - a randomized trial with 1-year follow-up. Scand J Med Sci Sports. 2004;14:286-295.
- ↑ T E O Schubert, C. W. (2005). Achilles tendinosis is associated with sprouting of substance P positive nerve fibres. Ann Rheum Dis , 1083-1086.fckLR Level 3B
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.
- ↑ K M Khan, a. p. (2002). Time to abandon the “tendinitis” myth: Painful, overuse tendon conditions have a non-inflammatory pathology . BMJ , 324:626.fckLR Level 2A
- ↑ Evelyn Bass, L. (2012). Tendinopathy: Why the Difference Between Tendinitis and Tendinosis Matters. Int J Ther Massage Bodywork. , 5(1): 14–17.fckLR Level 2C
- ↑ KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.fckLR Level 2C
- ↑ . Hammer, W. I. (1999). Functional Soft Tissue Examination and Treatment by Manual Methods. Aspen: Jones &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Bartlett Learning.
- ↑ KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.fckLR Level 2C
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Shibuya N, T. J. (2012). Is calcaneal inclination higher in patiënts with insertional achilles tendinosis? A case- controlled, cross-sectional study. The journal of foot and ankle surgery , 757-761.fckLR Level 3B
- ↑ Healy, N. T. (2010). Ultrasound-guided treatments for chronic Achilles tendinopathy: an update and current status . Skeletal Radiol , 39:425–434.fckLR Level 5
- ↑ 16.0 16.1 Robinson JM, Cook JL, Purdam C et al. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. British J of Sports Med. 2001;35:335-341.
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.
- ↑ Jenna Beaudry. Achilles Tendonitis Tape Job. Available from: http://www.youtube.com/watch?v=xzRhIyw85Xk [last accessed 01/12/12]
- ↑ Aaron Tomlinson. Achilles Tape Application. Available from: http://www.youtube.com/watch?v=fQAwpCToR48 [last accessed 01/12/12]
- ↑ Alex Scott, R. P. (2011). Conservative treatment of chronic Achilles tendinopathy. CMAJ , 183(10): 1159–1165.fckLR Level 1A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ . Hammer, W. I. (1999). Functional Soft Tissue Examination and Treatment by Manual Methods. Aspen: Jones &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp; Bartlett Learning.
- ↑ Stasinopoulos D, S. I. (2004). Comparison of effects of exercise programme, pulsed ultrasound and transverse friction in the treatment of chronic patellar tendinopathy. Clin Rehabil , 18(4):347-52.fckLR Level 1B
- ↑ James Henry Cyriax, P. J. (1993). Illustrated manual of orthopaedic medicine. Oxford: Elsevier Health Sciences.
- ↑ Joseph MF, T. K. (2012). Deep friction massage to treat tendinopathy: a systematic review of a classic treatment in the face of a new paradigm of understanding. J Sport Rehabil. , 21(4):343-53.fckLR Level 3A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Rompe JD, F. J. (2008). Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy. A randomized, controlled trial. J Bone Joint Surg Am. , (1):52-61.fckLR Level 1B
- ↑ Sten Rasmussen, M. C. (2008). Shockwave therapy for achilles tendinopathy. A double-blind, randomized clinical trail of efficacy. Acta Orthopaedica , 249-256.fckLR Level 1B
- ↑ Bleakley C, M. S. (2004). The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med , (1):251-61.fckLR Level 1A
- ↑ Dykstra JH, H. H. (2009). Comparisons of cubed ice, crushed ice, and wetted ice on intramuscular and surface temperature changes. J Athl Train. , (2):136-41.fckLR Level 2A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A
- ↑ Bleakley C, M. S. (2004). The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med , (1):251-61.fckLR Level 1A
- ↑ Brett L Woodley, R. J.‐W. (2007). Chronic tendinopathy: effectiveness of eccentric exercise. Br J Sports Med , 41(4): 188–198.fckLR Level 1A
- ↑ John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A