Anterior Knee Pain: Difference between revisions
mNo edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Prepatellar bursitis" to "[[Prepatellar Bursitis") |
||
| (39 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editors ''' - [[User:Maxime Tuerlinckx|Maxime Tuerlinckx]] | '''Original Editors ''' - [[User:Maxime Tuerlinckx|Maxime Tuerlinckx]], Ineza Roger Noel ,Ismael El Habouchi ,Faryan Bouzapar and Tom Flachet as part of the [[Vrije Universiteit Brussel Evidence-based Practice Project]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description == | == Definition/Description == | ||
| Line 8: | Line 8: | ||
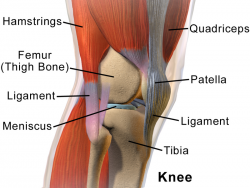
[[Image:Knee Anatomy Side View.png|thumb|right|250px|Knee - Side View]] | [[Image:Knee Anatomy Side View.png|thumb|right|250px|Knee - Side View]] | ||
<br> Anterior knee pain is | <br> Anterior knee pain is [[Pain-Modulation|pain]] that occurs in the anterior and central aspect of the [[knee]]. Its cause can be due to a number of conditions: <ref>Sala D, Silvestre A, Gomar-Sancho F. Intraosseous hyperpressure of the patella as a cause of anterior knee pain. Medscape Orth Sports Med. 1999;3:1–8.</ref> | ||
*[[Patellofemoral Pain Syndrome|Patellofemoral pain syndrome]] | *[[Patellofemoral Pain Syndrome|Patellofemoral pain syndrome]] | ||
*[[Chondromalacia Patellae|Chondromalacia Patellae]] | *[[Chondromalacia Patellae|Chondromalacia Patellae]] | ||
*[[Osgood-Schlatter | *[[Osgood-Schlatter Disease|Osgood-Schlatter’s disease]] | ||
*[[Sinding Larsen Johansson Syndrome|Sinding Larsen Johansson syndrome]] | *[[Sinding Larsen Johansson Syndrome|Sinding Larsen Johansson syndrome]] | ||
*[[Plica Syndrome|Plica synovialis syndrome]] | *[[Plica Syndrome|Plica synovialis syndrome]] | ||
*[[Knee Bursitis|Knee bursitis/Hoffa’s disease]] | *[[Knee Bursitis|Knee bursitis/Hoffa’s disease]] | ||
*[[Articular Cartilage Lesions|Articular cartilage injury]] | *[[Articular Cartilage Lesions|Articular cartilage injury]] | ||
* | *Bone tumours: Most patients will experience [[Pain Behaviours|pain]] in the area of the tumour. Pain can become worse during [[Physical Activity|physical activity]] and often awakens patients during the night. Bone mass around the tumour becomes weaker and the [[bone]] may [[fracture]] as a result. <ref>OrthoInfo. Diseases and conditions. Available from: | ||
http://orthoinfo.aaos.org/topic.cfm?topic=A00074 (accessed 27 May 2020) | |||
</ref> | |||
*[[Osteochondritis Dissecans of the Knee|Osteochondritis dissecans]] | *[[Osteochondritis Dissecans of the Knee|Osteochondritis dissecans]] | ||
*[[Patellofemoral Instability|Patellafemoral instability/subluxation]] | *[[Patellofemoral Instability|Patellafemoral instability/subluxation]] | ||
*Patellar stress fracture: A stress fracture in the patella is caused either by fatigue as a result of submaximal stress loads or insufficiency where the bone has been previously weakened due to physiological stress. It reduces shock absorption such that high repetitions of load may lead to a stress fracture. <ref>Crowther MA, Mandal A, Sarangi PP. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1725122/pdf/v039p000e6.pdf Propagation of stress fracture of the patella]. Br J Sports Med. 2005;39(2):e6. </ref> | |||
* | |||
*[[Patellar Tendinitis|Patellar tendinitis]] | *[[Patellar Tendinitis|Patellar tendinitis]] | ||
*[[Knee Osteoarthritis|Patellofemoral osteoarthritis]] | *[[Knee Osteoarthritis|Patellofemoral osteoarthritis]] | ||
* | *[[Pes Anserinus Bursitis|Pes anserine bursitis]]: The anserine bursa is one of 13 bursae found around the knee, located just below the pes anserinus. Patients with pes anserine bursitis often complain of spontaneous knee pain with tenderness in the inferomedial aspect of the knee joint. <ref>Helfenstein M Jr, Kuromoto J. Anserine syndrome. Rev Bras Reumatol. 2010;50(3):313-327.</ref> | ||
*[[Patellar Tendinitis|Quadriceps tendinopathy]] | *[[Patellar Tendinitis|Quadriceps tendinopathy]] | ||
*[[Prepatellar | *[[Prepatellar Bursitis|Prepatellar Bursitis]] | ||
*[[Iliotibial Band Syndrome|Iliotibial band syndrome]] <ref> Dixit S, DiFiori JP, Burton M, Mines B. Management of patellofemoral pain syndrome. Am Fam Physician. 2007;75(2):194-202. | *[[Iliotibial Band Syndrome|Iliotibial band syndrome]] <ref>Dixit S, DiFiori JP, Burton M, Mines B. Management of patellofemoral pain syndrome. Am Fam Physician. 2007;75(2):194-202. </ref> | ||
== Epidemiology / | == Epidemiology /Aetiology == | ||
The | The aetiology of anterior knee pain is multifactorial and not well defined due to the variety of symptoms, pain location and pain level experienced by the patient. Underlying factors could be patella abnormalities, muscular imbalances or weakness leading to patella malalignment on flexion and extension. The can cause include overuse injuries such as; [[tendinopathy]], insertional tendinopathy, [[Patellar malalignment|patellar instability]], chondral and osteochondral damage <ref name=":1">Suzanne Werner, Anterior knee pain: an update of physical therapy, Knee Surg Sports Traumatol Artrosc (2014) 22:2286-2294.</ref>. | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
There is no clear definition of anterior knee pain <ref name=":0">Witvrouw E, Werner S, Mikkelsen C, Van Tiggelen D, Berghe Vanden L, Cerulli G. Clinical classification of patellofemoral pain syndrome: guidelines for non-operative treatment. Knee Surg Sports Traumatol Arthrosc. 2005, 13 (2): 122-130.</ref>as patients can present with various symptoms. There may be functional deficit, crepitus and/or instability. With activities of daily living pain often occurs or get worse when walking downstairs, squatting, depressing the clutch pedal in a car, wearing high-heeled shoes, or sitting for long periods with the knees in a flexed position, known as 'movie sign'. Patients can also experience a degree of instability, especially on walking up and down stairs or over ramps <ref>Vincente Sanchis-Alfonso, Holistic approach to understand anterior knee pain. Clinical implications, Knee Surg Sports Traumatol Artrosc (2014) 22:2257-2285</ref>. Individuals with overuse injuries may report a feeling of instability or giving way, although this may not be a true giving way (which is associated with internal injury to the knee), but a neuromuscular inhibition as a result of pain, muscle weakness, patellar or joint instability <ref>Houghton KM. Review for the generalist: evaluation of anterior knee pain. Pediatric Rheumatology Online Journal. 2007;5:8. doi:10.1186/1546-0096-5-8.</ref> | |||
== Differential Diagnosis == | |||
* Referred pain from [[Hip Anatomy|hip joint]] pathology such as capital femoral epiphysis | |||
* Referred pain from the Saphenous nerve <ref name=":0" /> | |||
== | == Diagnostic Procedures == | ||
Evaluation of anterior pain is challenging as it can be non-specific and differential diagnosis is extensive. It requires a thorough examination, symptom history, in-depth knowledge of the associated structures and typical injury patterns. In younger individuals, an assessment of their general growth and development is also essential to determine a diagnosis. | |||
'''Knee-spine syndrome-''' In older individuals with anterior knee discomfort, Tsuji et al. [66] investigated the relationship between patellofemoral joint pain, lumbar lordosis, and sacral inclination. Those with and without anterior knee discomfort had a significantly different sacral inclination. Patients with patellofemoral discomfort had a reduced sacral inclination (by approximately 5°). The "knee-spine syndrome" was the name given to this pathological condition.<ref>Petersen W, Ellermann A, Gösele-Koppenburg A, Best R, Rembitzki IV, Brüggemann GP, Liebau C. [https://link.springer.com/article/10.1007/s00167-013-2759-6 Patellofemoral pain syndrome.] Knee surgery, sports traumatology, arthroscopy. 2014 Oct;22:2264-74.</ref> | |||
Some key factors in obtainin an accurate diagnosis are; the pain characteristics, i.e. its location, character, onset, duration, change with activity or rest, aggravating and alleviating factors and any night pain; trauma (acute macrotrauma, repetitive microtrauma, recent/remote); mechanical symptoms (locking or extension block, instability, worse during or after activity); inflammatory symptoms such as morning stiffness, swelling; effects of previous treatments and the current level of function of the patient: if there is any history of [[gout]], pseudogout, [[Rheumatoid Arthritis|rheumatoid arthritis]], or other degenerative joint diseases. Selective use of appropriate imaging, such as [[Ultrasound Scans|Ultrasound]] and [[MRI Scans|MRI]] are excellent tools for differential diagnosis and for ruling out sources of intra-articular derangements <ref>Llopis E, Padron M. Anterior knee pain, European journal of radiology. 2017; 62(1): 27–43</ref> | |||
Diagnosing and thus selecting an individual specific, non-operative treatment protocol can be vexing. The European Rehabilitation Panel have devised a guideline which should lead to improved treatment choice and outcomes. They suggest the following assessment parameters: | |||
* '''Symptoms''': Pain (location and type) or instability problems? | |||
* Alignment of the entire lower extremity: Squinting [[patella]]? High Q-angle? Genu valgus? Genu recurvatum? Pronation of the subtalar joint? | |||
* '''Patellar position''': [[Patella alta]]? Patella baja? Patellar glide? Patellar tilt? Patellar rotation? | |||
* Muscles and soft tissues: Hypotrophy of VMO? An imbalance between VM and VL? Weakness of knee extensors, hip flexors and/or hip abductors? Tightness of the medial retinaculum? Tightness of lateral muscle structures, hamstrings and/or rectus femoris? | |||
* Knee function (pain and/or maltracking of the patella): During different dynamic activities, e.g. stair walking, step-up/step-down exercises and one-leg squat? | |||
The 13 item screening Kujala Anterior Knee Pain Scale (AKPS)<ref>Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–63.</ref> can also be used to identify patellofemoral pain in adolescents and young adults<ref>Foss KD, Myer GD, Chen SS, Hewett TE. Expected Prevalence From the Differential Diagnosis of Anterior Knee Pain in Adolescent Female Athletes During Preparticipation Screening. Journal of Athletic Training. 2012; 47(5): 519-524 </ref>. ''Ittenbach et all'' suggest that is highly reliable, but not without its limitations and further research is needed for its use outside of a clinical environment and application to the general population<ref>Ittenbach RF, Huang G, Barber Foss KD, Hewett TE, Myer GD. Reliability and Validity of the Anterior Knee Pain Scale: Applications for Use as an Epidemiologic Screener. Rudan J, ed. ''PLoS ONE''. 2016;11(7):e0159204. doi:10.1371/journal.pone.0159204.</ref>. The AKPS has shown to have good test-retest reliability. | |||
The [http://www.physio-pedia.com/Lower_Extremity_Functional_Scale_(LEFS) Lower Extremity Functional Scale (LEFS)] is a further self-report test, to assess difficulties that the patient has with activities. This questionnaire is less specific for anterior knee pain patient than the anterior knee pain scale. The LEFS also demonstrates a high test-retest reliability and its reliability and responsiveness is slightly higher than that of the AKPS <ref>Watson CJ, Propps M, Ratner J, Zeigler DL, Horton P, Smith SS. Reliability and Responsiveness of the Lower Extremity Functional Scale and the Anterior Knee Pain Scale in Patients With Anterior Knee Pain. Journal of Orthopaedic and Sport Physical Therapy 2005; 35(3):136‐146. doi:10.2519/jospt.2005.35.3.136</ref> | |||
== Outcome Measures == | == Outcome Measures == | ||
The | The Kujala anterior knee pain scale and the [[Lower Extremity Functional Scale (LEFS)|Lower extremity functional scale]] can be used for both an initial screening tool as well as to detect changes with treatment and as outcome measures. | ||
The [[Single Leg Squat Test|single leg squat]] is also used to assess anterior knee pain. | |||
== Medical Management == | == Medical Management == | ||
Where there is a bony abnormality or retinaculum dysfunction, non-operative treatment may be less successful, but operative treatment should be reserved for those with correctable anatomical abnormalities that have failed conservative therapy<ref>Smith TO, McNamara I, Donell ST. The contemporary management of anterior knee pain and patellofemoral instability. Knee. 2013;20 Suppl 1:S3‐S15. doi:10.1016/S0968-0160(13)70003-6 | |||
</ref> | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
For | For long term non-operative results, any postural mal-alignment or altered movement patterns should be addressed initially before introducing a strengthening programme. When assessing functional abnormality and compensatory patterns the whole lower limb should be observed, not restricting assessment to the knee area<ref>McClinton SM, Cobian DG, Heiderscheit BC. Physical therapist management of anterior knee pain. Current reviews in musculoskeletal medicine. 2020 Dec;13(6):776-87.</ref>. Any significant leg length discrepancy should be addressed as well any intrinsic imbalances in the [[Foot Anatomy|foot]] where these are contributing factors. ''Eng et all'' suggest that orthotics alongside exercise can result in more effective outcomes for sufferers of anterior knee pain compared to exercise alone <ref>Eng JJ, Pierrynowski MR. Evaluation of soft foot orthotics in the treatment of patellofemoral pain syndrome [published correction appears in Phys Ther 1993;73(5):330]. ''Phys Ther''. 1993;73(2):62‐70. doi:10.1093/ptj/73.2.62</ref>, but any exercise and/or stretching programme needs to be individualised relative to the presenting symptoms and the [[Movement Dysfunction|movement dysfunction]]. | ||
<div class="row"> | |||
<div class="col-md-6"> {{#ev:youtube|-u4HH8q3tyA|300}} <div class="text-right"><ref>Ask Doctor Jo. Physical Therapy for Knee Pain Relief - Ask Doctor Jo. Available from: http://www.youtube.com/watch?v=-u4HH8q3tyA [last accessed 27/5/2020]</ref></div></div> | |||
<div class="col-md-6"> {{#ev:youtube|yQKxITLikiE|300}} <div class="text-right"><ref>Ask Doctor Jo. 10 Best Knee Pain Strengthening Exercises – Ask Doctor Jo. Available from: http://www.youtube.com/watch?v=yQKxITLikiE [last accessed 27/5/2020]</ref></div></div> | |||
Where the retinaculum is tight, affecting the [[Patellofemoral Joint|patellofemoral joint]], manual stretching or McConnell taping may improve symptoms. But taping alone does not significantly reduce pain. However, there is evidence that knee taping, including placebo-taping, combined with exercise provides a superior reduction in pain compared with [[Therapeutic Exercise|exercise]] alone. Therapies such as proprioceptive training, shoe inserts and taping may be best utilized as a complement to traditional exercise therapy; however, they have not been effective when implemented alone.<ref>Logan CA, Bhashyam AR, Tisosky AJ, Haber DB, Provencher MT. Systematic Review of the effect of Taping Techniques on Patellofemoral Pain Syndrome. Sports Health. 2017;9(5):456-461.https://doi.org/10.1177/1941738117710938</ref> | |||
== | With an exercise programme, improving the eccentric muscular control is more effective than concentric exercises, with closed chain exercises being more functional and minimising stress on the patellofemoral joint.<ref name=":0" /> Reduced knee extensor strength is commonly seen in anterior knee pain patients, as well as weakness in the [[Vastus Medialis Oblique|vastus medialis obliquus (VMO)]], although Witvrouw et al concluded that the VMO can not be worked in isolation<ref name=":0" />, VMO designed exercises activating both VM and VL. A neuromuscular dysfunction is thought to be the cause of a VMO deficit. | ||
Muscle length in the hamstrings, gastrocnemius and Rectus femoris all effect patellofemoral mechanics. Tight hamstrings can generate an increased reaction force over the patellofemoral joint as a greater force is required by the quadriceps for movement, so regular stretching is advised. But according to ''Mason et al,'' who compared the effectiveness of quadriceps stretching, quadriceps strengthening and taping in isolation and in combination, quadriceps stretching and quadriceps strengthening resulted in isolation in more improvements than taping. They also concluded that combining these treatments is recommended as the initial approach to treating patellofemoral pain but further individualized more functional, global treatment is essential. <sup><ref>Mason M, Keays SL, Newcombe PA. The effect of taping, quadriceps strengthening and stretching prescribed separately or combined on patellofemoral pain. Physiother Res Int. 2011; 16(2):109-19</ref></sup> | |||
== Presentations == | == Presentations == | ||
<div class="coursebox"> | <div class="coursebox"> | ||
{| cellspacing="4" cellpadding="4" width="100%" border="0 | {| class="FCK__ShowTableBorders" cellspacing="4" cellpadding="4" width="100%" border="0" | ||
|- | |- | ||
| align="center" | <imagemap> | | align="center" | <imagemap> | ||
| Line 85: | Line 100: | ||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Anterior knee pain is a symptom, not a diagnosis. Any diagnosis for the pain is, essentially, via exclusion due to the numerous possible conditions, where patella abnormality or muscular imbalances are important factors, determined by a thorough history and patient examination. There is also a high correlation between AKP and faulty hip mechanics, so any assessment needs to involve the entire kinetic chain. Treatment is highly individualised and the European Rehabilitation Panel's guideline is a useful tool for choosing a non-operative treatment protocol. | |||
== References == | |||
<references /> | |||
<references /> | |||
[[Category:Vrije_Universiteit_Brussel_Project]] [[Category: | [[Category:Vrije_Universiteit_Brussel_Project]] | ||
[[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | |||
[[Category:Presentations]] | |||
[[Category:Knee]] | |||
[[Category:Knee - Conditions]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Sports Injuries]] | |||
Latest revision as of 15:34, 19 October 2023
Original Editors - Maxime Tuerlinckx, Ineza Roger Noel ,Ismael El Habouchi ,Faryan Bouzapar and Tom Flachet as part of the Vrije Universiteit Brussel Evidence-based Practice Project
Top Contributors - Laura Ritchie, Scott Cornish, Admin, Kim Jackson, Maxime Tuerlinckx, Uchechukwu Chukwuemeka, Blessed Denzel Vhudzijena, Roger Ineza, Hanne Vanrysselberghe, Shaimaa Eldib, Michelle Lee, WikiSysop, Mudra Shah, Wanda van Niekerk, Lucinda hampton and Sai Kripa
Definition/Description[edit | edit source]
Anterior knee pain is pain that occurs in the anterior and central aspect of the knee. Its cause can be due to a number of conditions: [1]
- Patellofemoral pain syndrome
- Chondromalacia Patellae
- Osgood-Schlatter’s disease
- Sinding Larsen Johansson syndrome
- Plica synovialis syndrome
- Knee bursitis/Hoffa’s disease
- Articular cartilage injury
- Bone tumours: Most patients will experience pain in the area of the tumour. Pain can become worse during physical activity and often awakens patients during the night. Bone mass around the tumour becomes weaker and the bone may fracture as a result. [2]
- Osteochondritis dissecans
- Patellafemoral instability/subluxation
- Patellar stress fracture: A stress fracture in the patella is caused either by fatigue as a result of submaximal stress loads or insufficiency where the bone has been previously weakened due to physiological stress. It reduces shock absorption such that high repetitions of load may lead to a stress fracture. [3]
- Patellar tendinitis
- Patellofemoral osteoarthritis
- Pes anserine bursitis: The anserine bursa is one of 13 bursae found around the knee, located just below the pes anserinus. Patients with pes anserine bursitis often complain of spontaneous knee pain with tenderness in the inferomedial aspect of the knee joint. [4]
- Quadriceps tendinopathy
- Prepatellar Bursitis
- Iliotibial band syndrome [5]
Epidemiology /Aetiology[edit | edit source]
The aetiology of anterior knee pain is multifactorial and not well defined due to the variety of symptoms, pain location and pain level experienced by the patient. Underlying factors could be patella abnormalities, muscular imbalances or weakness leading to patella malalignment on flexion and extension. The can cause include overuse injuries such as; tendinopathy, insertional tendinopathy, patellar instability, chondral and osteochondral damage [6].
Characteristics/Clinical Presentation[edit | edit source]
There is no clear definition of anterior knee pain [7]as patients can present with various symptoms. There may be functional deficit, crepitus and/or instability. With activities of daily living pain often occurs or get worse when walking downstairs, squatting, depressing the clutch pedal in a car, wearing high-heeled shoes, or sitting for long periods with the knees in a flexed position, known as 'movie sign'. Patients can also experience a degree of instability, especially on walking up and down stairs or over ramps [8]. Individuals with overuse injuries may report a feeling of instability or giving way, although this may not be a true giving way (which is associated with internal injury to the knee), but a neuromuscular inhibition as a result of pain, muscle weakness, patellar or joint instability [9]
Differential Diagnosis[edit | edit source]
- Referred pain from hip joint pathology such as capital femoral epiphysis
- Referred pain from the Saphenous nerve [7]
Diagnostic Procedures[edit | edit source]
Evaluation of anterior pain is challenging as it can be non-specific and differential diagnosis is extensive. It requires a thorough examination, symptom history, in-depth knowledge of the associated structures and typical injury patterns. In younger individuals, an assessment of their general growth and development is also essential to determine a diagnosis.
Knee-spine syndrome- In older individuals with anterior knee discomfort, Tsuji et al. [66] investigated the relationship between patellofemoral joint pain, lumbar lordosis, and sacral inclination. Those with and without anterior knee discomfort had a significantly different sacral inclination. Patients with patellofemoral discomfort had a reduced sacral inclination (by approximately 5°). The "knee-spine syndrome" was the name given to this pathological condition.[10]
Some key factors in obtainin an accurate diagnosis are; the pain characteristics, i.e. its location, character, onset, duration, change with activity or rest, aggravating and alleviating factors and any night pain; trauma (acute macrotrauma, repetitive microtrauma, recent/remote); mechanical symptoms (locking or extension block, instability, worse during or after activity); inflammatory symptoms such as morning stiffness, swelling; effects of previous treatments and the current level of function of the patient: if there is any history of gout, pseudogout, rheumatoid arthritis, or other degenerative joint diseases. Selective use of appropriate imaging, such as Ultrasound and MRI are excellent tools for differential diagnosis and for ruling out sources of intra-articular derangements [11]
Diagnosing and thus selecting an individual specific, non-operative treatment protocol can be vexing. The European Rehabilitation Panel have devised a guideline which should lead to improved treatment choice and outcomes. They suggest the following assessment parameters:
- Symptoms: Pain (location and type) or instability problems?
- Alignment of the entire lower extremity: Squinting patella? High Q-angle? Genu valgus? Genu recurvatum? Pronation of the subtalar joint?
- Patellar position: Patella alta? Patella baja? Patellar glide? Patellar tilt? Patellar rotation?
- Muscles and soft tissues: Hypotrophy of VMO? An imbalance between VM and VL? Weakness of knee extensors, hip flexors and/or hip abductors? Tightness of the medial retinaculum? Tightness of lateral muscle structures, hamstrings and/or rectus femoris?
- Knee function (pain and/or maltracking of the patella): During different dynamic activities, e.g. stair walking, step-up/step-down exercises and one-leg squat?
The 13 item screening Kujala Anterior Knee Pain Scale (AKPS)[12] can also be used to identify patellofemoral pain in adolescents and young adults[13]. Ittenbach et all suggest that is highly reliable, but not without its limitations and further research is needed for its use outside of a clinical environment and application to the general population[14]. The AKPS has shown to have good test-retest reliability.
The Lower Extremity Functional Scale (LEFS) is a further self-report test, to assess difficulties that the patient has with activities. This questionnaire is less specific for anterior knee pain patient than the anterior knee pain scale. The LEFS also demonstrates a high test-retest reliability and its reliability and responsiveness is slightly higher than that of the AKPS [15]
Outcome Measures[edit | edit source]
The Kujala anterior knee pain scale and the Lower extremity functional scale can be used for both an initial screening tool as well as to detect changes with treatment and as outcome measures.
The single leg squat is also used to assess anterior knee pain.
Medical Management[edit | edit source]
Where there is a bony abnormality or retinaculum dysfunction, non-operative treatment may be less successful, but operative treatment should be reserved for those with correctable anatomical abnormalities that have failed conservative therapy[16]
Physical Therapy Management[edit | edit source]
For long term non-operative results, any postural mal-alignment or altered movement patterns should be addressed initially before introducing a strengthening programme. When assessing functional abnormality and compensatory patterns the whole lower limb should be observed, not restricting assessment to the knee area[17]. Any significant leg length discrepancy should be addressed as well any intrinsic imbalances in the foot where these are contributing factors. Eng et all suggest that orthotics alongside exercise can result in more effective outcomes for sufferers of anterior knee pain compared to exercise alone [18], but any exercise and/or stretching programme needs to be individualised relative to the presenting symptoms and the movement dysfunction.
Where the retinaculum is tight, affecting the patellofemoral joint, manual stretching or McConnell taping may improve symptoms. But taping alone does not significantly reduce pain. However, there is evidence that knee taping, including placebo-taping, combined with exercise provides a superior reduction in pain compared with exercise alone. Therapies such as proprioceptive training, shoe inserts and taping may be best utilized as a complement to traditional exercise therapy; however, they have not been effective when implemented alone.[21]
With an exercise programme, improving the eccentric muscular control is more effective than concentric exercises, with closed chain exercises being more functional and minimising stress on the patellofemoral joint.[7] Reduced knee extensor strength is commonly seen in anterior knee pain patients, as well as weakness in the vastus medialis obliquus (VMO), although Witvrouw et al concluded that the VMO can not be worked in isolation[7], VMO designed exercises activating both VM and VL. A neuromuscular dysfunction is thought to be the cause of a VMO deficit.
Muscle length in the hamstrings, gastrocnemius and Rectus femoris all effect patellofemoral mechanics. Tight hamstrings can generate an increased reaction force over the patellofemoral joint as a greater force is required by the quadriceps for movement, so regular stretching is advised. But according to Mason et al, who compared the effectiveness of quadriceps stretching, quadriceps strengthening and taping in isolation and in combination, quadriceps stretching and quadriceps strengthening resulted in isolation in more improvements than taping. They also concluded that combining these treatments is recommended as the initial approach to treating patellofemoral pain but further individualized more functional, global treatment is essential. [22]
Presentations[edit | edit source]
 |
Case Study: Adolescent Anterior Knee Pain
This presentation was created by Omolara Ajayi in collaboration with: EIM Clinical Excellence Network and Physical Therapy Central. |
Clinical Bottom Line[edit | edit source]
Anterior knee pain is a symptom, not a diagnosis. Any diagnosis for the pain is, essentially, via exclusion due to the numerous possible conditions, where patella abnormality or muscular imbalances are important factors, determined by a thorough history and patient examination. There is also a high correlation between AKP and faulty hip mechanics, so any assessment needs to involve the entire kinetic chain. Treatment is highly individualised and the European Rehabilitation Panel's guideline is a useful tool for choosing a non-operative treatment protocol.
References[edit | edit source]
- ↑ Sala D, Silvestre A, Gomar-Sancho F. Intraosseous hyperpressure of the patella as a cause of anterior knee pain. Medscape Orth Sports Med. 1999;3:1–8.
- ↑ OrthoInfo. Diseases and conditions. Available from: http://orthoinfo.aaos.org/topic.cfm?topic=A00074 (accessed 27 May 2020)
- ↑ Crowther MA, Mandal A, Sarangi PP. Propagation of stress fracture of the patella. Br J Sports Med. 2005;39(2):e6.
- ↑ Helfenstein M Jr, Kuromoto J. Anserine syndrome. Rev Bras Reumatol. 2010;50(3):313-327.
- ↑ Dixit S, DiFiori JP, Burton M, Mines B. Management of patellofemoral pain syndrome. Am Fam Physician. 2007;75(2):194-202.
- ↑ Suzanne Werner, Anterior knee pain: an update of physical therapy, Knee Surg Sports Traumatol Artrosc (2014) 22:2286-2294.
- ↑ 7.0 7.1 7.2 7.3 Witvrouw E, Werner S, Mikkelsen C, Van Tiggelen D, Berghe Vanden L, Cerulli G. Clinical classification of patellofemoral pain syndrome: guidelines for non-operative treatment. Knee Surg Sports Traumatol Arthrosc. 2005, 13 (2): 122-130.
- ↑ Vincente Sanchis-Alfonso, Holistic approach to understand anterior knee pain. Clinical implications, Knee Surg Sports Traumatol Artrosc (2014) 22:2257-2285
- ↑ Houghton KM. Review for the generalist: evaluation of anterior knee pain. Pediatric Rheumatology Online Journal. 2007;5:8. doi:10.1186/1546-0096-5-8.
- ↑ Petersen W, Ellermann A, Gösele-Koppenburg A, Best R, Rembitzki IV, Brüggemann GP, Liebau C. Patellofemoral pain syndrome. Knee surgery, sports traumatology, arthroscopy. 2014 Oct;22:2264-74.
- ↑ Llopis E, Padron M. Anterior knee pain, European journal of radiology. 2017; 62(1): 27–43
- ↑ Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–63.
- ↑ Foss KD, Myer GD, Chen SS, Hewett TE. Expected Prevalence From the Differential Diagnosis of Anterior Knee Pain in Adolescent Female Athletes During Preparticipation Screening. Journal of Athletic Training. 2012; 47(5): 519-524
- ↑ Ittenbach RF, Huang G, Barber Foss KD, Hewett TE, Myer GD. Reliability and Validity of the Anterior Knee Pain Scale: Applications for Use as an Epidemiologic Screener. Rudan J, ed. PLoS ONE. 2016;11(7):e0159204. doi:10.1371/journal.pone.0159204.
- ↑ Watson CJ, Propps M, Ratner J, Zeigler DL, Horton P, Smith SS. Reliability and Responsiveness of the Lower Extremity Functional Scale and the Anterior Knee Pain Scale in Patients With Anterior Knee Pain. Journal of Orthopaedic and Sport Physical Therapy 2005; 35(3):136‐146. doi:10.2519/jospt.2005.35.3.136
- ↑ Smith TO, McNamara I, Donell ST. The contemporary management of anterior knee pain and patellofemoral instability. Knee. 2013;20 Suppl 1:S3‐S15. doi:10.1016/S0968-0160(13)70003-6
- ↑ McClinton SM, Cobian DG, Heiderscheit BC. Physical therapist management of anterior knee pain. Current reviews in musculoskeletal medicine. 2020 Dec;13(6):776-87.
- ↑ Eng JJ, Pierrynowski MR. Evaluation of soft foot orthotics in the treatment of patellofemoral pain syndrome [published correction appears in Phys Ther 1993;73(5):330]. Phys Ther. 1993;73(2):62‐70. doi:10.1093/ptj/73.2.62
- ↑ Ask Doctor Jo. Physical Therapy for Knee Pain Relief - Ask Doctor Jo. Available from: http://www.youtube.com/watch?v=-u4HH8q3tyA [last accessed 27/5/2020]
- ↑ Ask Doctor Jo. 10 Best Knee Pain Strengthening Exercises – Ask Doctor Jo. Available from: http://www.youtube.com/watch?v=yQKxITLikiE [last accessed 27/5/2020]
- ↑ Logan CA, Bhashyam AR, Tisosky AJ, Haber DB, Provencher MT. Systematic Review of the effect of Taping Techniques on Patellofemoral Pain Syndrome. Sports Health. 2017;9(5):456-461.https://doi.org/10.1177/1941738117710938
- ↑ Mason M, Keays SL, Newcombe PA. The effect of taping, quadriceps strengthening and stretching prescribed separately or combined on patellofemoral pain. Physiother Res Int. 2011; 16(2):109-19