Appendicitis: Difference between revisions
Carolyn Hall (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (200 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original | '''Original Editor '''- [[User:Carolyn Little|Carolyn Little]] and [[User:Genny Tibbs|Genny Tibbs]] [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
Appendicitis is described as the inflammation of the vermiform appendix that | == Introduction == | ||
[[File:Appendicitis depiction.png|thumb|Person suffering from Appendicitis]] | |||
The appendix is a small finger-shaped pouch that projects out from your colon on the lower right side of your abdomen.<ref name="Mayo Clinic">Mayo Clinic. Appendicitis. Available from:http://www.mayoclinic.org/diseases-conditions/appendicitis/basics/definition/CON-20023582. (accessed 18 March 2014).</ref> Appendicitis is described as the inflammation of the vermiform appendix that may result in necrosis and perforation.<ref name="Fuller">Goodman CC, Fuller K. Pathology Implications for the Physical Therapist. 3rd Edition. St. Louis, Missouri: Elsevier Saunders, 2009.</ref> Obstruction, inflammation, or infection can cause the appendix to rupture leading to peritonitis.<ref name="Goodman Synder">Goodman CC, Snyder TK. Differential Diagnosis for Physical Therapists: Screening for Referral. 5th Edition. St. Louis, Missouri: Elsevier Saunders, 2013.</ref> This condition usually requires surgery as medical management due to the fact that acute appendicitis can often be life threatening. Appendicitis is the leading cause of emergency abdominal surgeries.<ref name="Spirt">Spirt MJ. [https://www.tandfonline.com/doi/abs/10.3810/pgm.2010.01.2098 Complicated intra-abdominal infections: a focus on appendicitis and diverticulitis.] Postgraduate Medicine 2010;122(1):39–51.</ref> Upon histological review, acute appendicitis can be divided into simple, gangrenous, or perforated categories.<ref name="Fuller" /> | |||
== Etiology == | |||
The cause of appendicitis is usually an obstruction of the appendiceal lumen. Obstructions can be from eg an appendicolith (stone of the appendix); appendiceal tumors; intestinal parasites; hypertrophied lymphatic tissue. However often the exact etiology of acute appendicitis is unknown. When the appendiceal lumen gets obstructed, bacteria build up in the appendix and cause acute inflammation with perforation and abscess formation<ref>Jones MW, Lopez RA, Deppen JG. Appendicitis. InStatPearls [Internet] 2021 Sep 9. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK493193/ (accessed 11.5.2022)</ref>. | |||
== | == Epidemiology == | ||
Appendicitis is a global disease. The incidence of appendicitis is stable in most Western countries. Data from newly industrialized countries is sparse, but suggests that appendicitis is rising rapidly<ref>Ferris M, Quan S, Kaplan BS, Molodecky N, Ball CG, Chernoff GW, Bhala N, Ghosh S, Dixon E, Ng S, Kaplan GG. The global incidence of appendicitis: a systematic review of population-based studies. Annals of surgery. 2017 Aug 1;266(2):237-41.Available: https://pubmed.ncbi.nlm.nih.gov/28288060/<nowiki/>(accessed 11.5.2022)</ref> | |||
The | |||
The lifetime risk of appendicitis in the United States is 9% for males and 7% for females. It is most commonly diagnosed in adolescents and younger adults. Overall incidence of this condition is declining for reasons not well known. It is suggested that increased dietary fiber intake and improved hygiene could be contributing factors to the decrease in appendicitis cases.<ref name="Fuller" /> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Symptoms of appendicitis include: | |||
* dull pain centred around the navel, which progresses to a sharp pain in the lower right side of the abdomen | |||
* pain in the lower back, hamstring or rectum (less commonly) | |||
* | * fever | ||
* vomiting | |||
* diarrhoea or constipation | |||
* loss of appetite<ref name=":0">Better health channel Appendicitis Available:https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/appendicitis (accessed 11.5.2022)</ref> | |||
* | |||
* | |||
* | |||
* | |||
< | |||
= | |||
== | == Perforated appendix == | ||
If pus builds up in the appendix it eventually bursts, flooding the abdominal cavity with infected matter. Bursting, or perforation, can occur 36 hours or so from the onset of infection. The signs of a perforated appendix include a severe worsening of symptoms and collapse. | |||
This can cause peritonitis which is inflammation of the peritoneum that lines the inner wall of the abdomen and covers most of the abdominal organs. This is a life-threatening complication and requires immediate emergency treatment.<ref name=":0" /> | |||
== Diagnosis == | |||
Diagnostic testing is often indicated for individuals suspected of having appendicitis. Medical imaging such as [[CT Scans|CT scans]], [[Ultrasound Scans|sonograms]], or abdominal [[X-Rays|X-rays]] are used to help confirm possible appendicitis. Additional laboratory tests utilized are urine analyses, to make sure that a urinary tract infection or a kidney stone isn't causing the pain, or complete blood counts. Patients who present with typical appendicitis will have an elevated WBC count >20,000 mm<sup>3</sup>. Physicians will also perform a histological examination of the resected appendix for further confirmation of the condition. Iliopsoas and obturator muscle tests are administered to rule out potential abscesses or insults to [[muscle]] integrity.<ref name="Fuller" /> | |||
== Medical Management == | |||
[[Image:Laparoscopic Appendectomy.jpg|Laparoscopic surgery uses smaller incisions and special surgical tools. Image From: http://www.zadehsurgical.com/general-surgery-services-encino/appendicitis/|alt=|right|frameless|387x387px]] | |||
Appendicitis is a medical emergency that requires immediate care.<ref name="NDDIC II">National Digestive Diseases Information Clearinghouse (NDDIC). Appendicitis. Available from: http://digestive.niddk.nih.gov/ddiseases/pubs/appendicitis/index.aspx (accessed 18 March 2014).</ref> The most common treatment for appendicitis is an appendectomy with some patients receiving antibiotics pre-operatively. Early surgical removal decreases the risk of mortality and morbidity to < 1%.<ref name="Fuller" /> Prognosis for these patients who undergo surgery is typically good unless accurate diagnosis is delayed and perforation occurs. Poor prognostic indicators for this condition include hypovolemia, peritonitis, and septic shock. <ref name="Fuller" />An appendectomy can be performed using a Laparotomy or Laparoscopic surgery. Laparoscopic surgery leads to fewer complications, such as hospital-related infections, and has a shorter recovery time with less scaring. | |||
If the appendix has ruptured and infection has spread beyond the appendix or if an abscess is present, immediate surgery through laparotomy may be required to clean the abdominal cavity and remove the appendix. If the infection is not treated peritonitis can develop. If the infection spreads to the blood it can lead to sepsis.<ref name="NDDIC II" /> <ref>Zadeh Surgical, Inc. Appendicitis. Available from: http://www.zadehsurgical.com/general-surgery-services-encino/appendicitis/ (accessed 22 March 2014).</ref> | |||
One or two days is usually spent in the hospital after an appendectomy.<ref name="Mayo Clinic" /> | |||
An alternative to surgery is antibiotic therapy. Studies that have compared the outcome of surgery to the outcome of antibiotics show that about 70 per cent of cases may resolve with antibiotic therapy and not require surgery. However, the factors leading to failure of antibiotic therapy are not known, so antibiotic therapy alone is usually reserved for patients too frail to undergo surgery.<ref name=":0" /> | |||
== Physiotherapy == | |||
Physical therapist may see patients post appendectomy. Therapist should be aware of the incision site between the anterior superior iliac spine and umbilicus. Patient education would include avoiding strenuous activity, supporting the abdomen when coughing, and breathing exercises. | |||
== Viewing == | |||
Watch this 4 minute video on Appendicitis {{#ev:youtube|JHWUs4lHxgc|300}}<ref>Los Angeles Colonoscopy. Appendicitis: An Overview | Modified Thomas Test. Available from https://www.youtube.com/watch?v=JHWUs4lHxgc (accessed 28/11/2020).</ref> | |||
== | |||
</ | |||
<references /> | == References== | ||
<references /> | |||
[[Category: | [[Category:Bellarmine Student Project]] | ||
Latest revision as of 10:04, 11 May 2022
Original Editor - Carolyn Little and Genny Tibbs from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Genevieve Tibbs, Carolyn Hall, Leana Louw, Elaine Lonnemann, Wendy Walker, Kim Jackson, Lucinda hampton and WikiSysop
Introduction [edit | edit source]
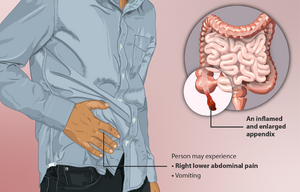
The appendix is a small finger-shaped pouch that projects out from your colon on the lower right side of your abdomen.[1] Appendicitis is described as the inflammation of the vermiform appendix that may result in necrosis and perforation.[2] Obstruction, inflammation, or infection can cause the appendix to rupture leading to peritonitis.[3] This condition usually requires surgery as medical management due to the fact that acute appendicitis can often be life threatening. Appendicitis is the leading cause of emergency abdominal surgeries.[4] Upon histological review, acute appendicitis can be divided into simple, gangrenous, or perforated categories.[2]
Etiology[edit | edit source]
The cause of appendicitis is usually an obstruction of the appendiceal lumen. Obstructions can be from eg an appendicolith (stone of the appendix); appendiceal tumors; intestinal parasites; hypertrophied lymphatic tissue. However often the exact etiology of acute appendicitis is unknown. When the appendiceal lumen gets obstructed, bacteria build up in the appendix and cause acute inflammation with perforation and abscess formation[5].
Epidemiology[edit | edit source]
Appendicitis is a global disease. The incidence of appendicitis is stable in most Western countries. Data from newly industrialized countries is sparse, but suggests that appendicitis is rising rapidly[6]
The lifetime risk of appendicitis in the United States is 9% for males and 7% for females. It is most commonly diagnosed in adolescents and younger adults. Overall incidence of this condition is declining for reasons not well known. It is suggested that increased dietary fiber intake and improved hygiene could be contributing factors to the decrease in appendicitis cases.[2]
Characteristics/Clinical Presentation[edit | edit source]
Symptoms of appendicitis include:
- dull pain centred around the navel, which progresses to a sharp pain in the lower right side of the abdomen
- pain in the lower back, hamstring or rectum (less commonly)
- fever
- vomiting
- diarrhoea or constipation
- loss of appetite[7]
Perforated appendix[edit | edit source]
If pus builds up in the appendix it eventually bursts, flooding the abdominal cavity with infected matter. Bursting, or perforation, can occur 36 hours or so from the onset of infection. The signs of a perforated appendix include a severe worsening of symptoms and collapse.
This can cause peritonitis which is inflammation of the peritoneum that lines the inner wall of the abdomen and covers most of the abdominal organs. This is a life-threatening complication and requires immediate emergency treatment.[7]
Diagnosis[edit | edit source]
Diagnostic testing is often indicated for individuals suspected of having appendicitis. Medical imaging such as CT scans, sonograms, or abdominal X-rays are used to help confirm possible appendicitis. Additional laboratory tests utilized are urine analyses, to make sure that a urinary tract infection or a kidney stone isn't causing the pain, or complete blood counts. Patients who present with typical appendicitis will have an elevated WBC count >20,000 mm3. Physicians will also perform a histological examination of the resected appendix for further confirmation of the condition. Iliopsoas and obturator muscle tests are administered to rule out potential abscesses or insults to muscle integrity.[2]
Medical Management[edit | edit source]
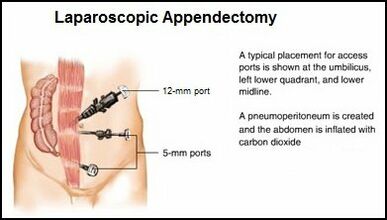
Appendicitis is a medical emergency that requires immediate care.[8] The most common treatment for appendicitis is an appendectomy with some patients receiving antibiotics pre-operatively. Early surgical removal decreases the risk of mortality and morbidity to < 1%.[2] Prognosis for these patients who undergo surgery is typically good unless accurate diagnosis is delayed and perforation occurs. Poor prognostic indicators for this condition include hypovolemia, peritonitis, and septic shock. [2]An appendectomy can be performed using a Laparotomy or Laparoscopic surgery. Laparoscopic surgery leads to fewer complications, such as hospital-related infections, and has a shorter recovery time with less scaring.
If the appendix has ruptured and infection has spread beyond the appendix or if an abscess is present, immediate surgery through laparotomy may be required to clean the abdominal cavity and remove the appendix. If the infection is not treated peritonitis can develop. If the infection spreads to the blood it can lead to sepsis.[8] [9]
One or two days is usually spent in the hospital after an appendectomy.[1]
An alternative to surgery is antibiotic therapy. Studies that have compared the outcome of surgery to the outcome of antibiotics show that about 70 per cent of cases may resolve with antibiotic therapy and not require surgery. However, the factors leading to failure of antibiotic therapy are not known, so antibiotic therapy alone is usually reserved for patients too frail to undergo surgery.[7]
Physiotherapy[edit | edit source]
Physical therapist may see patients post appendectomy. Therapist should be aware of the incision site between the anterior superior iliac spine and umbilicus. Patient education would include avoiding strenuous activity, supporting the abdomen when coughing, and breathing exercises.
Viewing[edit | edit source]
Watch this 4 minute video on Appendicitis
References[edit | edit source]
- ↑ 1.0 1.1 Mayo Clinic. Appendicitis. Available from:http://www.mayoclinic.org/diseases-conditions/appendicitis/basics/definition/CON-20023582. (accessed 18 March 2014).
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Goodman CC, Fuller K. Pathology Implications for the Physical Therapist. 3rd Edition. St. Louis, Missouri: Elsevier Saunders, 2009.
- ↑ Goodman CC, Snyder TK. Differential Diagnosis for Physical Therapists: Screening for Referral. 5th Edition. St. Louis, Missouri: Elsevier Saunders, 2013.
- ↑ Spirt MJ. Complicated intra-abdominal infections: a focus on appendicitis and diverticulitis. Postgraduate Medicine 2010;122(1):39–51.
- ↑ Jones MW, Lopez RA, Deppen JG. Appendicitis. InStatPearls [Internet] 2021 Sep 9. StatPearls Publishing.Available:https://www.ncbi.nlm.nih.gov/books/NBK493193/ (accessed 11.5.2022)
- ↑ Ferris M, Quan S, Kaplan BS, Molodecky N, Ball CG, Chernoff GW, Bhala N, Ghosh S, Dixon E, Ng S, Kaplan GG. The global incidence of appendicitis: a systematic review of population-based studies. Annals of surgery. 2017 Aug 1;266(2):237-41.Available: https://pubmed.ncbi.nlm.nih.gov/28288060/(accessed 11.5.2022)
- ↑ 7.0 7.1 7.2 Better health channel Appendicitis Available:https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/appendicitis (accessed 11.5.2022)
- ↑ 8.0 8.1 National Digestive Diseases Information Clearinghouse (NDDIC). Appendicitis. Available from: http://digestive.niddk.nih.gov/ddiseases/pubs/appendicitis/index.aspx (accessed 18 March 2014).
- ↑ Zadeh Surgical, Inc. Appendicitis. Available from: http://www.zadehsurgical.com/general-surgery-services-encino/appendicitis/ (accessed 22 March 2014).
- ↑ Los Angeles Colonoscopy. Appendicitis: An Overview | Modified Thomas Test. Available from https://www.youtube.com/watch?v=JHWUs4lHxgc (accessed 28/11/2020).