Dry Needling: Difference between revisions
Claire Knott (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) m (Kim Jackson moved page Dry needling to Dry Needling) |
||
| (26 intermediate revisions by 8 users not shown) | |||
| Line 8: | Line 8: | ||
== Description == | == Description == | ||
[[Image:Dry Needling.jpg|thumb|right|300x240px]] Trigger-point dry needling is an invasive procedure where a fine needle or [[Acupuncture|acupuncture]] needle is inserted into the skin and [[Muscle|muscle]]. It | [[Image:Dry Needling.jpg|thumb|right|300x240px]] Trigger-point dry needling is an invasive procedure where a fine needle or [[Acupuncture|acupuncture]] needle is inserted into the skin and [[Muscle|muscle]]. It targets myofascial [http://www.physio-pedia.com/Trigger_Points trigger points] (MTrPs) - hyperirritable spots palpable as nodules in the taut bands of skeletal muscles.<ref name="Dommerholt et al">Dommerholt J, Mayoral del Moral O, Gröbli C. [https://www.tandfonline.com/doi/abs/10.1179/jmt.2006.14.4.70E Trigger point dry needling.] Journal of Manual & Manipulative Therapy. 2006 Oct 1;14(4):70E-87E.</ref> Trigger point dry needling can be performed at either superficial or deep tissue levels. <br> | ||
== Pathophysiology of MTrPs == | |||
[[Trigger Points|Trigger points]] are attributed to an excessive release of acetylcholine from specifc motor endplates. They can be categorised into Active and Latent MTrPs<ref>Hong CZ. [https://link.springer.com/article/10.1007/s11916-006-0058-3 Treatment of myofascial pain syndrome]. Current pain and headache reports. 2006 Sep;10:345-9.</ref><ref>Kuan TS. [https://link.springer.com/article/10.1007/s11916-009-0059-0 Current studies on myofascial pain syndrome]. Current pain and headache reports. 2009 Oct;13:365-9.</ref>. | |||
[[Image:Trigger point pain.jpg|300px|alt=|right]] | |||
*Active MTrPs can spontaneously trigger local or referred pain. They cause muscle '''weakness''', '''restricted [[range of motion (ROM)]]''' and '''autonomic phenomena'''. | |||
*Latent MTrPs do not cause pain unless they are stimulated. They may alter muscle activation patterns and restrict ROM. | |||
*Active and latent MTrPs cause '''[[allodynia]]''' at the trigger point site and '''hyperalgesia''' away from the trigger point in response to applied pressure<ref name="Dommerholt">Dommerholt J. [https://www.tandfonline.com/doi/abs/10.1179/106698111X13129729552065 Dry needling—peripheral and central considerations.] Journal of Manual & Manipulative Therapy. 2011 Nov 1;19(4):223-7.</ref>. | |||
*MTrPs form due to the development of a taut band within the muscle. This band is caused by excessive acetylcholine from the motor endplate, combined with the inhibition of acetylcholine esterase and an up-regulation of nicotinic acetylcholine receptors. | |||
* | * Taut bands initially form as a protective physiological response to actual or potential muscle damage. These bands are believed to develop in reaction to unaccustomed eccentric or concentric loading, sustained postures, and repetitive low-load stress. However, their persistence contributes to prolonged pain. | ||
[[ | *Pain associated with MTrPs is due to '''hypoxia''' and '''decreased blood flow.''' This results in decreased pH, activating muscle nociceptors for [[homeostasis|'''homeostasis''']] restoration, leading to [[Peripheral Sensitisation|'''peripheral sensitisation''']]. | ||
*MTrPs also play a role in '''[[Central Sensitisation|central sensitisation]]'''. While the mechanism is not fully understood, MTrPs sustain nociceptive input into the dorsal horn, thereby contributing to central sensitisation. | |||
== Deep VS Superficial Dry Needling == | |||
Superficial dry needling involves inserting the needle up to 10 mm into the subcutaneous tissue, its benefits include ease of administration, decreased risk of significant tissue trauma, reduced risk of nerve and visceral injury and patient comfort. | |||
The | Deep dry needling involves the insertion of the needle beyond the subcutaneous tissue into the muscle to reach MTrPs<ref>Griswold D, Wilhelm M, Donaldson M, Learman K, Cleland J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6598484/ The effectiveness of superficial versus deep dry needling or acupuncture for reducing pain and disability in individuals with spine-related painful conditions: a systematic review with meta-analysis. Journal of Manual & Manipulative Therapy.] 2019 May 27;27(3):128-40.</ref>. | ||
== Mechanisms of Action == | |||
Dry needling has been shown to immediately increase pressure pain threshold and ROM, decrease muscle tone, and decrease pain in patients with musculoskeletal conditions<ref name=":1">Gattie E, Cleland JA, Snodgrass S. The effectiveness of trigger point dry needling for musculoskeletal conditions by physical therapists: a systematic review and meta-analysis. Journal of Orthopaedic & Sports Physical Therapy. 2017 Mar;47(3):133-49.</ref>. The suggested mechanisms of action include: | |||
'''Local Twitch Response:''' Dry needling can elicit a ‘local twitch response’ which is an involuntary spinal reflex resulting in a localised contraction of the affected muscles that are being dry-needled. Local twitch response can lead to alteration in the length and tension of muscle fibres and stimulate mechanoreceptors like A Beta fibres<ref name=":2">Cagnie B, Dewitte V, Barbe T, Timmermans F, Delrue N, Meeus M. [https://link.springer.com/article/10.1007/s11916-013-0348-5 Physiologic effects of dry needling.] Current pain and headache reports. 2013 Aug;17(8):1-8. | |||
</ref>. | |||
'''Effects on Blood Flow:''' Sustained contraction of taut muscle bands in trigger points might cause local ischemia and hypoxia. Dry needling causes vasodilation in the small blood vessels leading to increased muscle blood flow and oxygenation<ref name=":2" />. | |||
= | '''Neurophysiological effects:''' Dry needling can elicit local and central nervous responses, promoting homeostasis at the trigger point site and leading to a decrease in both central and peripheral sensitisation to pain<ref name=":1" />. | ||
'''Remote Effects:''' Dry needling of distal MTrP has been found to have an analgesic effect on proximal MTrP. The literature has conflicting evidence regarding the contralateral effect<ref name=":2" /> | |||
'''[[Placebo Effect]]:''' Expectations regarding dry needling can strongly influence pain perception<ref>Cagnie B, Dewitte V, Barbe T, Timmermans F, Delrue N, Meeus M. Physiologic effects of dry needling. Current pain and headache reports. 2013 Aug;17:1-8.</ref>. | |||
== Indications == | |||
* [[Myofascial Pain|Myofascial pain]] with the presence of [[Trigger Points|trigger points]] | |||
* [[Chronic pain]] | |||
* [https://www.physio-pedia.com/Low_Back_Pain Low back pain] | |||
* [[Muscle Strain|Strains]] | |||
* [[Osteoarthritis]] | |||
* [[Fibromyalgia]] | |||
* [[Tendinopathy|Tendinopathies]].<ref>McAphee D, Bagwell M, Falsone S. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9159711/ Dry Needling: A Clinical Commentary.] International Journal of Sports Physical Therapy. 2022;17(4):551.</ref>{{#ev:youtube|MB4mVDqU1y0|350}}<ref>Tim Trevail. Dry Needling: Trapezius. Available from: https://www.youtube.com/watch?v=MB4mVDqU1y0 </ref> | |||
== Contraindications == | |||
'''Absolute contraindications<ref name="Trigger Point Dry Needling">Dommerholt J., Fernandez-de-las-Penas C. Trigger Point Dry Needling. An Evidenced and Clinical-Based Approach. Edinburgh: Churchill Livingstone-Elsevier, 2013</ref>''' | |||
Dry needling (DN) therapy should be avoided in patients under the following circumstances <ref>Australian Society of Acupunture Physioterapists Inc. Guidelines for safe acupuncture and dry needling practice, 2007.</ref> <ref>White, A., Cummings M., Filshie, J. Evidence of safety of acupuncture. An introduction to Western medical acupuncture. Edinburgh: Churchill Livingstone, 2008.</ref>: | |||
*Unwilling or unable to give consent due to fear, believes, communication, cognitive, age-related factors. | |||
*Medical emergency or acute medical condition. | |||
*Local infection | |||
*Over an area or limb with lymphedema as this may increase the risk of infection/cellulitis and the difficulty of fighting the infection if one should occur. | |||
*Inappropriate for any other reason. | |||
= | '''Relative Contraindications<ref name="Trigger Point Dry Needling" />''' | ||
* | *Abnormal bleeding tendency | ||
* | *Compromised immune system | ||
* | *Vascular disease | ||
* | *[[Diabetes]] | ||
*Pregnancy | |||
*Children | |||
*Frail patients | |||
*Patients with [[epilepsy]] | |||
*Psychological status | |||
*Patient allergies | |||
*Patient medication | |||
*Unsuitable patient for any reason | |||
== Clinical Evidence == | |||
The effectiveness of this treatment depends greatly on the skill of the therapist to accurately palpate myofascial [[Trigger Points|trigger points]] as well as kinaesthetic awareness of the anatomical structures. | |||
A review study concluded that dry needling, particularly in combination with other therapies, has moderate evidence for reducing pain severity in people diagnosed with [[Low Back Pain|low back pain]]. However, it also stated that the follow-up effects of dry needling and its clinical superiority in improving functional disability are ambiguous.<ref>Liu L, Huang QM, Liu QG, Thitham N, Li LH, Ma YT, Zhao JM. [https://www.sciencedirect.com/science/article/abs/pii/S0003999317304525 Evidence for dry needling in the management of myofascial trigger points associated with low back pain: a systematic review and meta-analysis]. Archives of physical medicine and rehabilitation. 2018 Jan 1;99(1):144-52.</ref> | |||
According to a systematic review study of 16 studies, 7 of which were RCTs, the use of DN alone or with other interventions generally resulted in improvement in spasticity level, pain intensity, and ROM in [[stroke]] survivors.<ref>Valencia-Chulian R, Heredia-Rizo AM, Moral-Munoz JA, Lucena-Anton D, Luque-Moreno C. [https://www.sciencedirect.com/science/article/abs/pii/S0965229920305586 Dry needling for the management of spasticity, pain, and range of movement in adults after stroke: A systematic review]. Complementary Therapies in Medicine. 2020 Aug 1;52:102515.</ref> | |||
DN | Another systematic review study concluded that DN reduced the severity of [[Myofascial Pain|myofascial pain]], which is usually associated with trigger points, in patients with temporomandibular joint dysfunction. However, it was also stated that there is a low level of evidence on this subject and that trials with bigger sample sizes and a lower risk of bias are needed.<ref>Vier, C., de Almeida, M.B., Neves, M.L., Dos Santos, A.R.S. and Bracht, M.A., 2019. [https://www.sciencedirect.com/science/article/abs/pii/S1413355518300510 The effectiveness of dry needling for patients with orofacial pain associated with temporomandibular dysfunction: a systematic review and meta-analysis]. ''Brazilian journal of physical therapy'', ''23''(1), pp.3-11.</ref> | ||
A systematic review of 23 trials considering needling therapies for myofascial trigger point pain concluded that direct dry-needling (where MTrPs were directly targeted) was as '''beneficial as wet needling'''.<ref name="cummings and white">Cummings TM, White AR. [https://www.sciencedirect.com/science/article/abs/pii/S0003999301066564 Needling therapies in the management of myofascial trigger point pain: a systematic review.] Archives of physical medicine and rehabilitation. 2001 Jul 1;82(7):986-92.</ref> There is no clear evidence that it is beneficial above placebo. More studies of higher quality with reproducible diagnostic criteria and a valid placebo are needed to draw firm conclusions on this. | |||
A systematic review and meta-analysis with level 1a evidence concluded that:<ref>Gattie E, Cleland JA, Snodgrass S. [https://www.jospt.org/doi/full/10.2519/jospt.2017.7096 The effectiveness of trigger point dry needling for musculoskeletal conditions by physical therapists: a systematic review and meta-analysis.] Journal of orthopaedic & sports physical therapy. 2017 Mar;47(3):133-49.</ref> | |||
* Dry needling applied by a physical therapist has very low to moderate quality evidence for superiority over no treatment or sham dry needling in reducing pain and improving pressure pain threshold in patients with musculoskeletal pain in the immediate to 12-week follow-up period. | |||
* Dry needling in improving functional outcomes has low-level evidence for superiority over no treatment and sham dry needling but no difference with other physical therapy treatments. | |||
* There is insufficient evidence for the long-term benefit of dry needling. | |||
== | == Electrical Dry Needling == | ||
Electrical dry needling (EDN) is a technique in which two needles are inserted as electrodes for passing an electric current. One of the main advantages of using EDN in clinical practice or acupuncture research is its capacity to set stimulation frequency and intensity objectively and quantifiably. | |||
In clinical practice, both low- and high-frequency electrostimulation are used often for diverse conditions. Low-frequency stimulation is specifically recommended for muscular atrophy <ref>Liu G.Techniques of acupuncture and moxibustion. Beijing: Huaxia Publishing House. 1998:177 p.</ref>, whereas high-frequency stimulation is recommended for spinal spasticity<ref>Yuan Y, Yan S, Chen X, Han JS X: The effect and mechanism of electroacupuncture in treating spinal spasticity: a clinical study. Nat Med J Chin, 1992;73:5932.</ref>.On animals for example EDN with 2-Hz stimulation seems to induce acupuncture analgesia by the release of endomorphin, β-endorphin and enkephalin binding to μ and δ opioid receptors. EDN with 100-Hz stimulation, however, enhances the release of dynorphin binding to the opioid receptor in the [[Spinal cord anatomy|spinal cord]] dorsal horn to produce an acupuncture analgesic effect<ref name=":0">Napadow V, Makris N, Liu J, Kettner NW, Kwong KK, Hui KK. [https://onlinelibrary.wiley.com/doi/abs/10.1002/hbm.20081 Effects of electroacupuncture versus manual acupuncture on the human brain as measured by fMRI.] Human brain mapping. 2005 Mar;24(3):193-205.</ref>. | |||
= | Most studies demonstrated a broad neuro matrix response that involved the [[Limbic System|limbic system]] and limbic-related brain structures including the [[amygdala]], [[hippocampus]], [[hypothalamus]], cingulate, prefrontal and insular cortices, [[Basal Ganglia|basal ganglia]], and [[cerebellum]]<ref name=":0" />. On human infact results demonstrated a greater effect on the limbic and limbic-related brain structures with real EDN than with nonspecific or placebo stimulation. Specifically, the hemodynamic response produced a signal increase in notable limbic-related regions such as the [[insula]], [[thalamus]], [[cerebellum]], and the anterior middle cingulate cortex. Interestingly, however, the subgenual anterior cingulate showed a signal decrease<ref>Wu MT, Sheen JM, Chuang KH, Yang P, Chin SL, Tsai CY, Chen CJ, Liao JR, Lai PH, Chu KA, Pan HB. [https://www.sciencedirect.com/science/article/abs/pii/S1053811902911456 Neuronal specificity of acupuncture response: a fMRI study with electroacupuncture]. Neuroimage. 2002 Aug 1;16(4):1028-37.</ref>. | ||
=== Clinical Relevance === | |||
* It has been found that when [[Manual Therapy|manual therapy]] and exercise programmes are combined with dry needling, the improvement in pain, function and disability is bigger in patients with [[Knee Osteoarthritis|knee osteoarthritis]] and [[Plantar Fasciitis|plantar fasciitis]]. <ref>Dunning J, Butts R, Young I, Mourad F, Galante V, Bliton P, Tanner M, Fernández-de-Las-Peñas C. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6250299/ Periosteal electrical dry needling as an adjunct to exercise and manual therapy for knee osteoarthritis: a multicenter randomized clinical trial]. The Clinical journal of pain. 2018 Dec;34(12):1149.</ref><ref>Dunning J, Butts R, Henry N, Mourad F, Brannon A, Rodriguez H, Young I, Arias-Buría JL, Fernández-de-Las-Peñas C. [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0205405 Electrical dry needling as an adjunct to exercise, manual therapy and ultrasound for plantar fasciitis: A multi-center randomized clinical trial]. PLoS One. 2018 Oct 31;13(10):e0205405.</ref> | |||
* EDN and upper cervical and upper thoracic HVLA thrust spinal manipulation were shown to be more effective than non-thrust mobilisation and exercise in patients with chronic headaches, and the effects were maintained at 3 months. <ref>Dunning J, Butts R, Zacharko N, Fandry K, Young I, Wheeler K, Day J, Fernández-de-Las-Peñas C. [https://www.sciencedirect.com/science/article/pii/S1529943020311451 Spinal manipulation and perineural electrical dry needling in patients with cervicogenic headache: a multicenter randomized clinical trial]. Spine J. 2021 Feb;21(2):284-295 | |||
</ref> | |||
* EDN combined with cervicothoracic manipulation c resulted in greater reductions in pain, disability, and medication intake than nonthrust peripheral joint/soft tissue mobilisation, exercise, and interferential current in patients with [[Subacromial Pain Syndrome|subacromial pain syndrome]]. The effects were maintained at 3 months.<ref>Dunning J, Butts R, Fernández-de-Las-Peñas C, Walsh S, Goult C, Gillett B, Arias-Buría JL, Garcia J, Young IA. [https://www.jospt.org/doi/full/10.2519/jospt.2021.9785 Spinal Manipulation and Electrical Dry Needling in Patients With Subacromial Pain Syndrome: A Multicenter Randomized Clinical Trial]. J Orthop Sports Phys Ther. 2021 Feb;51(2):72-81. | |||
</ref> | |||
== References == | == References == | ||
| Line 120: | Line 118: | ||
[[Category:Acupuncture]] | [[Category:Acupuncture]] | ||
{{DEFAULTSORT:Dry_Needling}} | |||
Latest revision as of 13:52, 29 January 2024
Original Editor - Ajay Upadhyay
Top Contributors - Sehriban Ozmen, Gayatri Jadav Upadhyay, Daniele Barilla, Irene Leahy, Kim Jackson, Lilian Ashraf, Redisha Jakibanjar, Admin, WikiSysop, Candace Goh, Claire Knott, Riccardo Ugrin, Rishika Babburu, Bruno Serra and Melissa Coetsee
Description[edit | edit source]
Trigger-point dry needling is an invasive procedure where a fine needle or acupuncture needle is inserted into the skin and muscle. It targets myofascial trigger points (MTrPs) - hyperirritable spots palpable as nodules in the taut bands of skeletal muscles.[1] Trigger point dry needling can be performed at either superficial or deep tissue levels.
Pathophysiology of MTrPs[edit | edit source]
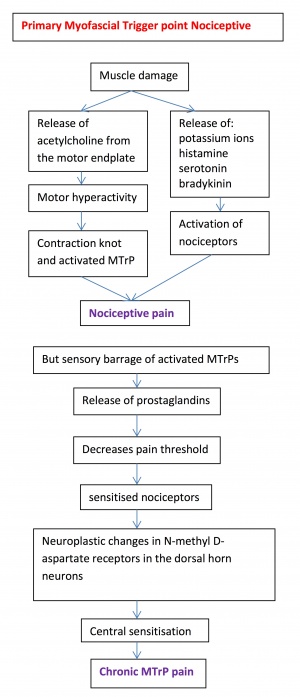
Trigger points are attributed to an excessive release of acetylcholine from specifc motor endplates. They can be categorised into Active and Latent MTrPs[2][3].
- Active MTrPs can spontaneously trigger local or referred pain. They cause muscle weakness, restricted range of motion (ROM) and autonomic phenomena.
- Latent MTrPs do not cause pain unless they are stimulated. They may alter muscle activation patterns and restrict ROM.
- Active and latent MTrPs cause allodynia at the trigger point site and hyperalgesia away from the trigger point in response to applied pressure[4].
- MTrPs form due to the development of a taut band within the muscle. This band is caused by excessive acetylcholine from the motor endplate, combined with the inhibition of acetylcholine esterase and an up-regulation of nicotinic acetylcholine receptors.
- Taut bands initially form as a protective physiological response to actual or potential muscle damage. These bands are believed to develop in reaction to unaccustomed eccentric or concentric loading, sustained postures, and repetitive low-load stress. However, their persistence contributes to prolonged pain.
- Pain associated with MTrPs is due to hypoxia and decreased blood flow. This results in decreased pH, activating muscle nociceptors for homeostasis restoration, leading to peripheral sensitisation.
- MTrPs also play a role in central sensitisation. While the mechanism is not fully understood, MTrPs sustain nociceptive input into the dorsal horn, thereby contributing to central sensitisation.
Deep VS Superficial Dry Needling[edit | edit source]
Superficial dry needling involves inserting the needle up to 10 mm into the subcutaneous tissue, its benefits include ease of administration, decreased risk of significant tissue trauma, reduced risk of nerve and visceral injury and patient comfort.
Deep dry needling involves the insertion of the needle beyond the subcutaneous tissue into the muscle to reach MTrPs[5].
Mechanisms of Action[edit | edit source]
Dry needling has been shown to immediately increase pressure pain threshold and ROM, decrease muscle tone, and decrease pain in patients with musculoskeletal conditions[6]. The suggested mechanisms of action include:
Local Twitch Response: Dry needling can elicit a ‘local twitch response’ which is an involuntary spinal reflex resulting in a localised contraction of the affected muscles that are being dry-needled. Local twitch response can lead to alteration in the length and tension of muscle fibres and stimulate mechanoreceptors like A Beta fibres[7].
Effects on Blood Flow: Sustained contraction of taut muscle bands in trigger points might cause local ischemia and hypoxia. Dry needling causes vasodilation in the small blood vessels leading to increased muscle blood flow and oxygenation[7].
Neurophysiological effects: Dry needling can elicit local and central nervous responses, promoting homeostasis at the trigger point site and leading to a decrease in both central and peripheral sensitisation to pain[6].
Remote Effects: Dry needling of distal MTrP has been found to have an analgesic effect on proximal MTrP. The literature has conflicting evidence regarding the contralateral effect[7]
Placebo Effect: Expectations regarding dry needling can strongly influence pain perception[8].
Indications[edit | edit source]
- Myofascial pain with the presence of trigger points
- Chronic pain
- Low back pain
- Strains
- Osteoarthritis
- Fibromyalgia
- Tendinopathies.[9][10]
Contraindications[edit | edit source]
Absolute contraindications[11]
Dry needling (DN) therapy should be avoided in patients under the following circumstances [12] [13]:
- Unwilling or unable to give consent due to fear, believes, communication, cognitive, age-related factors.
- Medical emergency or acute medical condition.
- Local infection
- Over an area or limb with lymphedema as this may increase the risk of infection/cellulitis and the difficulty of fighting the infection if one should occur.
- Inappropriate for any other reason.
Relative Contraindications[11]
- Abnormal bleeding tendency
- Compromised immune system
- Vascular disease
- Diabetes
- Pregnancy
- Children
- Frail patients
- Patients with epilepsy
- Psychological status
- Patient allergies
- Patient medication
- Unsuitable patient for any reason
Clinical Evidence[edit | edit source]
The effectiveness of this treatment depends greatly on the skill of the therapist to accurately palpate myofascial trigger points as well as kinaesthetic awareness of the anatomical structures.
A review study concluded that dry needling, particularly in combination with other therapies, has moderate evidence for reducing pain severity in people diagnosed with low back pain. However, it also stated that the follow-up effects of dry needling and its clinical superiority in improving functional disability are ambiguous.[14]
According to a systematic review study of 16 studies, 7 of which were RCTs, the use of DN alone or with other interventions generally resulted in improvement in spasticity level, pain intensity, and ROM in stroke survivors.[15]
Another systematic review study concluded that DN reduced the severity of myofascial pain, which is usually associated with trigger points, in patients with temporomandibular joint dysfunction. However, it was also stated that there is a low level of evidence on this subject and that trials with bigger sample sizes and a lower risk of bias are needed.[16]
A systematic review of 23 trials considering needling therapies for myofascial trigger point pain concluded that direct dry-needling (where MTrPs were directly targeted) was as beneficial as wet needling.[17] There is no clear evidence that it is beneficial above placebo. More studies of higher quality with reproducible diagnostic criteria and a valid placebo are needed to draw firm conclusions on this.
A systematic review and meta-analysis with level 1a evidence concluded that:[18]
- Dry needling applied by a physical therapist has very low to moderate quality evidence for superiority over no treatment or sham dry needling in reducing pain and improving pressure pain threshold in patients with musculoskeletal pain in the immediate to 12-week follow-up period.
- Dry needling in improving functional outcomes has low-level evidence for superiority over no treatment and sham dry needling but no difference with other physical therapy treatments.
- There is insufficient evidence for the long-term benefit of dry needling.
Electrical Dry Needling[edit | edit source]
Electrical dry needling (EDN) is a technique in which two needles are inserted as electrodes for passing an electric current. One of the main advantages of using EDN in clinical practice or acupuncture research is its capacity to set stimulation frequency and intensity objectively and quantifiably.
In clinical practice, both low- and high-frequency electrostimulation are used often for diverse conditions. Low-frequency stimulation is specifically recommended for muscular atrophy [19], whereas high-frequency stimulation is recommended for spinal spasticity[20].On animals for example EDN with 2-Hz stimulation seems to induce acupuncture analgesia by the release of endomorphin, β-endorphin and enkephalin binding to μ and δ opioid receptors. EDN with 100-Hz stimulation, however, enhances the release of dynorphin binding to the opioid receptor in the spinal cord dorsal horn to produce an acupuncture analgesic effect[21].
Most studies demonstrated a broad neuro matrix response that involved the limbic system and limbic-related brain structures including the amygdala, hippocampus, hypothalamus, cingulate, prefrontal and insular cortices, basal ganglia, and cerebellum[21]. On human infact results demonstrated a greater effect on the limbic and limbic-related brain structures with real EDN than with nonspecific or placebo stimulation. Specifically, the hemodynamic response produced a signal increase in notable limbic-related regions such as the insula, thalamus, cerebellum, and the anterior middle cingulate cortex. Interestingly, however, the subgenual anterior cingulate showed a signal decrease[22].
Clinical Relevance[edit | edit source]
- It has been found that when manual therapy and exercise programmes are combined with dry needling, the improvement in pain, function and disability is bigger in patients with knee osteoarthritis and plantar fasciitis. [23][24]
- EDN and upper cervical and upper thoracic HVLA thrust spinal manipulation were shown to be more effective than non-thrust mobilisation and exercise in patients with chronic headaches, and the effects were maintained at 3 months. [25]
- EDN combined with cervicothoracic manipulation c resulted in greater reductions in pain, disability, and medication intake than nonthrust peripheral joint/soft tissue mobilisation, exercise, and interferential current in patients with subacromial pain syndrome. The effects were maintained at 3 months.[26]
References[edit | edit source]
- ↑ Dommerholt J, Mayoral del Moral O, Gröbli C. Trigger point dry needling. Journal of Manual & Manipulative Therapy. 2006 Oct 1;14(4):70E-87E.
- ↑ Hong CZ. Treatment of myofascial pain syndrome. Current pain and headache reports. 2006 Sep;10:345-9.
- ↑ Kuan TS. Current studies on myofascial pain syndrome. Current pain and headache reports. 2009 Oct;13:365-9.
- ↑ Dommerholt J. Dry needling—peripheral and central considerations. Journal of Manual & Manipulative Therapy. 2011 Nov 1;19(4):223-7.
- ↑ Griswold D, Wilhelm M, Donaldson M, Learman K, Cleland J. The effectiveness of superficial versus deep dry needling or acupuncture for reducing pain and disability in individuals with spine-related painful conditions: a systematic review with meta-analysis. Journal of Manual & Manipulative Therapy. 2019 May 27;27(3):128-40.
- ↑ 6.0 6.1 Gattie E, Cleland JA, Snodgrass S. The effectiveness of trigger point dry needling for musculoskeletal conditions by physical therapists: a systematic review and meta-analysis. Journal of Orthopaedic & Sports Physical Therapy. 2017 Mar;47(3):133-49.
- ↑ 7.0 7.1 7.2 Cagnie B, Dewitte V, Barbe T, Timmermans F, Delrue N, Meeus M. Physiologic effects of dry needling. Current pain and headache reports. 2013 Aug;17(8):1-8.
- ↑ Cagnie B, Dewitte V, Barbe T, Timmermans F, Delrue N, Meeus M. Physiologic effects of dry needling. Current pain and headache reports. 2013 Aug;17:1-8.
- ↑ McAphee D, Bagwell M, Falsone S. Dry Needling: A Clinical Commentary. International Journal of Sports Physical Therapy. 2022;17(4):551.
- ↑ Tim Trevail. Dry Needling: Trapezius. Available from: https://www.youtube.com/watch?v=MB4mVDqU1y0
- ↑ 11.0 11.1 Dommerholt J., Fernandez-de-las-Penas C. Trigger Point Dry Needling. An Evidenced and Clinical-Based Approach. Edinburgh: Churchill Livingstone-Elsevier, 2013
- ↑ Australian Society of Acupunture Physioterapists Inc. Guidelines for safe acupuncture and dry needling practice, 2007.
- ↑ White, A., Cummings M., Filshie, J. Evidence of safety of acupuncture. An introduction to Western medical acupuncture. Edinburgh: Churchill Livingstone, 2008.
- ↑ Liu L, Huang QM, Liu QG, Thitham N, Li LH, Ma YT, Zhao JM. Evidence for dry needling in the management of myofascial trigger points associated with low back pain: a systematic review and meta-analysis. Archives of physical medicine and rehabilitation. 2018 Jan 1;99(1):144-52.
- ↑ Valencia-Chulian R, Heredia-Rizo AM, Moral-Munoz JA, Lucena-Anton D, Luque-Moreno C. Dry needling for the management of spasticity, pain, and range of movement in adults after stroke: A systematic review. Complementary Therapies in Medicine. 2020 Aug 1;52:102515.
- ↑ Vier, C., de Almeida, M.B., Neves, M.L., Dos Santos, A.R.S. and Bracht, M.A., 2019. The effectiveness of dry needling for patients with orofacial pain associated with temporomandibular dysfunction: a systematic review and meta-analysis. Brazilian journal of physical therapy, 23(1), pp.3-11.
- ↑ Cummings TM, White AR. Needling therapies in the management of myofascial trigger point pain: a systematic review. Archives of physical medicine and rehabilitation. 2001 Jul 1;82(7):986-92.
- ↑ Gattie E, Cleland JA, Snodgrass S. The effectiveness of trigger point dry needling for musculoskeletal conditions by physical therapists: a systematic review and meta-analysis. Journal of orthopaedic & sports physical therapy. 2017 Mar;47(3):133-49.
- ↑ Liu G.Techniques of acupuncture and moxibustion. Beijing: Huaxia Publishing House. 1998:177 p.
- ↑ Yuan Y, Yan S, Chen X, Han JS X: The effect and mechanism of electroacupuncture in treating spinal spasticity: a clinical study. Nat Med J Chin, 1992;73:5932.
- ↑ 21.0 21.1 Napadow V, Makris N, Liu J, Kettner NW, Kwong KK, Hui KK. Effects of electroacupuncture versus manual acupuncture on the human brain as measured by fMRI. Human brain mapping. 2005 Mar;24(3):193-205.
- ↑ Wu MT, Sheen JM, Chuang KH, Yang P, Chin SL, Tsai CY, Chen CJ, Liao JR, Lai PH, Chu KA, Pan HB. Neuronal specificity of acupuncture response: a fMRI study with electroacupuncture. Neuroimage. 2002 Aug 1;16(4):1028-37.
- ↑ Dunning J, Butts R, Young I, Mourad F, Galante V, Bliton P, Tanner M, Fernández-de-Las-Peñas C. Periosteal electrical dry needling as an adjunct to exercise and manual therapy for knee osteoarthritis: a multicenter randomized clinical trial. The Clinical journal of pain. 2018 Dec;34(12):1149.
- ↑ Dunning J, Butts R, Henry N, Mourad F, Brannon A, Rodriguez H, Young I, Arias-Buría JL, Fernández-de-Las-Peñas C. Electrical dry needling as an adjunct to exercise, manual therapy and ultrasound for plantar fasciitis: A multi-center randomized clinical trial. PLoS One. 2018 Oct 31;13(10):e0205405.
- ↑ Dunning J, Butts R, Zacharko N, Fandry K, Young I, Wheeler K, Day J, Fernández-de-Las-Peñas C. Spinal manipulation and perineural electrical dry needling in patients with cervicogenic headache: a multicenter randomized clinical trial. Spine J. 2021 Feb;21(2):284-295
- ↑ Dunning J, Butts R, Fernández-de-Las-Peñas C, Walsh S, Goult C, Gillett B, Arias-Buría JL, Garcia J, Young IA. Spinal Manipulation and Electrical Dry Needling in Patients With Subacromial Pain Syndrome: A Multicenter Randomized Clinical Trial. J Orthop Sports Phys Ther. 2021 Feb;51(2):72-81.